Reading...
![]()
Play button
![]()
Play button
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
45 Cards in this Set
- Front
- Back
|
Traumatic Brain Injury (TBI)
|
- Damage to brain tissue caused by external mechanical force
- Evidenced by 1) Loss of consciousness due to brain trauma 2) Posttraumatic amnesia 3) Skull fracture 4a) Objective neurological findings attributed to TBI or 4b) Mental status examination |
|
|
Severity of TBI
|
- severity on continuum
-> From mild to moderate to severe - Considerable variation across groups concerning a) Treatment b) Course of recovery c) General outcome - Initial presentation of TBI becomes one of most important predictors for immediate and long-term outcome |
|
|
Moderate to severe TBI
|
- Often persisting impairment that affect ability to return to previous level of functioning
- More likely to require inpatient or post-acute rehabilitation than patients with mild TBI -> consequently, also more likely to require outpatient care - Limited awareness of cognitive and psychosocial problems -> additional stress for family and friends |
|
|
Incidence/prevalence of traumatic brain injury
|
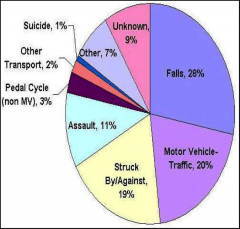
- USA
- About 160 cases (mild, moderate and severe) per 100,000 persons - Determination of incidence difficult, however, because 1) many people with mild TBI do not seek treatment or are not hospitalised 2) Methodological differences between studies - Methodological differences between studies might also explain variation between countries |
|
|
Risk factors for TBI
|
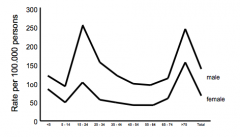
- Age
-> Highest rates of TBI in 14-24 year-old persons and persons > 64 years - Gender -> The average female to male ratio is 1 : 1.6 to 2.8 - Alcohol consumption -> Correlation between TBI and blood alcohol consumption -> 56 % of adults with TBI had a positive blood alcohol level - Previous brain injury -> average “Non TBI” to “previously TBI” ratio is 1 : 2.9 -> Further increase of rates for third TBI (given already two prior injuries) - Socioeconomic status -> Highest numbers of TBI in families at lowest income level |
|
|
Measurement of injury severity: The Glasgow Coma Scale (GCS)
|
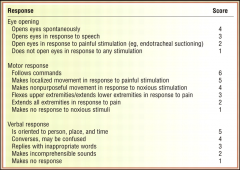
- measures depth of coma by patients patient’s responsiveness level
1) Eye opening 2) Motor movement 3) Verbal communication - Glasgow Coma Scale Score -> 15-13: Mild -> 12-9: Moderate -> 8-3: Severe - Differentiation depending on presence or absence of findings on initial CT/MRI: Complicated versus Uncomplicated - Advantages a) Scores can be determined within first 24 hours b) Predictive for early important outcomes (e.g. survival) c) Predictive for later functional outcomes (e.g. employment) |
|
|
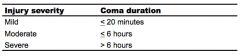
Measurement of injury severity: length of coma
|
|
|
|
Measurement of injury severity: Time to follow commands
|
- Predictive for
a) Global outcome b) Neuropsychological functioning c) Personal independence d) Employment after TBI - Advantage: Can be obtained in early stages - Disadvantage: a) Can be affected by sedative drugs b) Close monitoring of patient for extended time period c) Affected by fluctuations in patient’s mental status d) Not immediately available for early prediction of outcome |
|
|
Measurement of injury severity: Posttraumatic amnesia
|
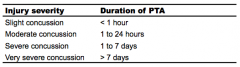
- Posttraumatic amnesia: Phase of recovery during which patient is responsive but confused, disoriented and unable to form and retain new memories
- Retrospectively by waiting until patient is no longer confused and asking about first memory patient can recall following TBI - Prospectively by repeated measurement of patient’s disorientation with standardised scales - Most commonly used criteria for classification of injury severity on basis of post traumatic amnesia Russel & Smith (1961): See picture - Predictive for a) Neuropsychological outcome b) Independent living c) Return to work - Disadvantages a) Close monitoring of patient for extended time period b) Affected by fluctuations preventing ceffective communication (e.g. Aphasia, intubation) |
|
|
Comparison of measurements of injury severity
|
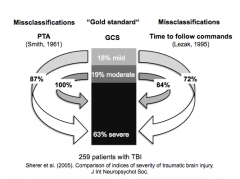
- Classification on basis of different indices does not always correspond to same injury severity, so that there may be different severity levels of an individual patient’s injury based on which measurement is used
|
|
|
Categorisation of traumatic brain injury
|
- Focal injuries
- Diffuse injuries |
|
|
Diffuse traumatic brain injury
|
- Affecting brain in widespread pattern
- Reflects 2. principle mechanism: Acceleration / deceleration injuries resulting from unrestricted movement of head, which results in shear, tensile and compressive strain on brain tissue - Pathology 1: Tearing of bridging veins, subdural haematoma, diffuse axional and vascular injury - Pathology 2: Contre-coup injury more sever than coup injury - Injury from contact forces often occurs in two places 1. Site of initial impact of brain with skull (coup) 2. Site diametrically opposite of initial impact (contre-coup) |
|
|
Focal traumatic brain injury
|
- Affecting circumscribed region(s) of brain
- Reflects 1. principle mechanism: an object strikes head or brain comes into contact with skull - Pathology: injury to scalp, skull fracture, surface contusions, intracerebral haematomas |
|
|
Contusion
|
= "bruise“ that may cause tissue damage and bleeding
- Injury of brain tissue after traumatic brain injury - Characteristic distribution of contusions after TBI: a) Cerebellum b) Frontal and temporal lobes c) Frontal and temporal poles |
|
|
Diffuse Axonal Injury
|
- In acceleration/deceleration injuries: particular risk for diffuse axonal injury
- Serious traumatic lesion - Brain goes into back and forth or side to side gliding motion - Axons are stretched and twisted but do not snap immediately - Sudden deformation causes changes in the axonal cytoskeleton - Some axons with mild lesions probably recover but many eventually rupture (several hours after trauma) - Disruption of communication between neurons and can lead to cognitive, behaviourial and emotional changes - Clinical effects are difficult to separate from other concurrent TBI pathology - Predictive of later outcome: a) Edema b) Hypoxia / ischemia c) Increased intracranial pressure d) Associated vascular changes (e.g. hypotension) e) Meningitis f) Abscess |
|
|
Acute treatment of moderate to severe traumatic brain injury
|
= Stabilisation of patient immediately after injury
- Unblocking of airways - Assisting breathing - Keeping blood circulating - Monitoring for edema - Relieving from increased intracranial pressure (surgery, e.g. removal of blood clot) - Prevention of seizure by anticonvulsive medication - Prevention of other medical problems (e.g. infections, pneumonia) |
|
|
Subacute treatment of moderate to severe traumatic brain injury
|
= Rehabilitation and return of patient to community
- Usually: Admission to acute rehabilitation hospital (most patients still in post traumatic amnesia) - Three main goals 1. Early detection of complications (e.g. Muscle contractions, infections, Fluid accumulation) 2. Facilitation of neurological and functional recovery - Improvement of function often incomplete - Supported by rehab professionals (E.g. clinical neuropsychologists, physical, occupational and speech therapists, neurologists) - Training of functions, compensation strategies, learning new ways to do routine tasks, etc. 3. Prevention of injury - During post traumatic amnesia, various problems may lead to further injury: Poor balance, Incoordination, Weakness, Cognitive impairments, Unaware of limitations, Agitation and restlessness |
|
|
Chronic treatment of moderate to severe traumatic brain injury
|
- Continuation of rehabilitation and treatment long-term impairments, which are common after TBI
- More complex function recover more slowly (e.g. problem solving) Examples: - Cognitive and functional training (neuropsychology) - Counseling and/or psychotherapy - Medications - Physical therapy - Speech therapy - Assistive technologies - Changes in personality (childish, dependent, short-tempered) - Impaired perception |
|
|
Course of recovery after moderate to severe traumatic brain injury
|
- Predictable stages of recovery
-> Progression through stages fairly constant -> Variability with specific stages and length of time spent in each 1. Coma - Non-responsive state - Patient has closed eyes - No following of instructions - No following of instructions - No purposeful movements 2. Vegetative state - Non-responsive state - No self- or environmental awareness - Return of sleep/wake cycles - Periods of eye opening 3. Minimally conscious state - Minimal but definitive evidence of awareness of self- or environment (e.g. Motor response to noxious stimuli or sounds or smiling) - Indication of resolution of this state: Consistent following to commands, Verbal/gestural responding, Consistent purposeful behaviour 4. Confused state - Posttraumatic amnesia - impairments of orientation, memory, attention, language, behaviour, mood, perception 5. Recovery - Progressive resolution of physical, cognitive, motor, behavioural impairments |
|
|
Neuropsychological functioning after moderate to severe traumatic brain injury
|
- Risk for persistent cognitive impairment is related to initial injury severity
- Extent and pattern depend to great extent on time of assessment relative to onset of injury, since there is a substantial recovery across majority of cognitive functions Overall: - Motor impairments after traumatic brain injury - Impaired orientation - Impaired attention / Reduced information processing speed - Memory impairment - Impaired language and communication skills - Disturbances of executive functions - Deficits in social functioning and self-regulation |
|
|
Motor impairments after moderate to severe traumatic brain injury
|
- Fine motor movements
- Dysphagia (impaired swallowing) - Spasticity (stiffness because of contraction of muscles) - Dysarthria (poor articulation) - Balance disturbances - Hemiparesis |
|
|
Impaired attention / Reduced information processing speed after moderate to severe traumatic brain injury
|
- Prevalent across all levels of injury severity
- Persistent deficits, even in patients with a supposed good recovery |
|
|
Memory impairment after moderate to severe traumatic brain injury
|
- Very common (also in post-acute phase)
- Persists even after recovery of other cognitive functions - Occurs across different aspects of memory processing, including encoding, consolidation and retrieval - Improvement of memory in most patients with TBI -> However, Lack of improvement or even decline in some patients because of a) Injury related factors (e.g. hypoxia) b) Patient related factors (e.g. depression) |
|
|
Impaired language and communication skills after moderate to severe traumatic brain injury
|
- Including deficits of word-finding (anomia, anomic aphasia), verbal fluency and comprehension of complex commands
- Problems initiating conversations and interpreting indirect communication - Contribute to impairments in psychosocial functioning |
|
|
Disturbances of executive functions after moderate to severe traumatic brain injury
|
- very common
- Often prevent independent functioning and return to occupational life - Commin problems: -> Verbal and design fluency -> Conceptual reasoning / flexibility -> Application of strategies (e.g. clustering in memory tests) -> Working memory -> Planning / problem solving |
|
|
Deficits in social functioning and self-regulation after moderate to severe traumatic brain injury
|
- often not captured by neuropsychological assessment
- Irritability - Anxiety - OCD - Restlessness or agitation - Depression - Fatigue (sometimes even narcoleptic syndromes) |
|
|
Narcolepsy after moderate to severe traumatic brain injury
|
- Neurological disorder characterised by sleep at inappropriate times or some of its components such as REM sleep
- Sleep attacks - Cataplexy: sudden attack of extreme muscle weakness while the person remains awake, often triggered by strong emotions or sudden physical effort - Sleep paralysis: inability to move while falling asleep or waking up - Hypnagogic hallucination: dreamlike experiences that occur just before a person falls asleep, accompanied by sleep paralysis - Currently, the most common treatment is stimulant drugs, e.g., modafinil |
|
|
1 month after moderate to severe traumatic brain injury
|
- Patients with less severe injuries: More selective impairments, including memory, cognitive flexibility, psychomotor speed
- Patients with most severe injuries: Impairments on most measures, including motor speed, attention, cognitive flexibility, memory, processing speed, reasoning skills |
|
|
6 year after moderate to severe traumatic brain injury
|
- 70% suffer from cognitive impairment
- Impairments of learning and memory = Most frequent |
|
|
Neuropsychological assessment in moderate to severe traumatic brain injury
|
- WHEN to administer neuropsychological tests?
a) early assessment - Patients are still in post traumatic amnesia, which leads to useful data that may predict later functional status b) Delayed assessment - Confusion and diorientation in patients leads to porrf performance and yields limited information regarding strengths and weaknesses - Survey of neuropsychologists suggests broad guidelines: a) For all levels of TBI severity, preliminary testing at resolution of post traumatic amnesia b) For mild TBI, first testing between 1st week and 1st month post-injury and follow–up after 1year c) For moderate to severe TBI, first testing not within first 3 months and subsequent repeat assessment after 6, 12 and 24 months (as needed) |
|
|
Neuropsychological test battery for traumatic brain injury
|
- Comprehensive: measures of attention, memory, executive functions, motor functioning, etc.
-> Change sensitivity -> Be carful, however, some patients may consciously or unconsciously exaggerate symptoms in follow up assessments |
|
|
Outcome of moderate to severe traumatic brain injury
|
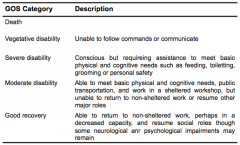
- commonly determined with Glasgow Outcome Scale
-> at 6 months reliable predictor of ultimate outcome - Global outcome depends on time, with an expected trend to better outcome with passing time |
|
|
Return to work following moderate to severe traumatic brain injury
|
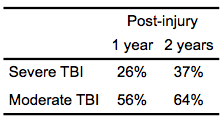
- Drop of employment rate from 86% before injury to 29% after injury
- 1 year post injury: 42% unimployment rate - Risk for unemployment higher in: a) Males b) People with higer education c) People with more severe injuries d) people with greater impairment on early neuropsychological functioning (at 1 month) - Return to work more likely in younger patients or patients with technical/managerial jobs than in patients over 45 years of age or in unskilled occupations - Premorbid characteristics, e.g. pre-injury employment status, and cognitive and functional status are better predictors than injury severity variables |
|
|
Annual incidence of mild traumatic brain injury
|
- 5 cases per 1000 persons
|
|
|
Effect of age in mild traumatic brain injury
|
- Older people (>60 years) 4 times more likely than younger (around 30 years)
|
|
|
Cognitive deficits after mild traumatic brain injury
|
- effects are cumulative
-Typical deficits after mild traumatic brain injury a) Memory impairment b) Reduced cognitive processing c) Reduced attention span d) Impaired cognitive flexibility - Unsually resolve within 3 months - Exaggeration or malingering of cognitive deficits should routinely taken into consideration, as 40% of mild TBI claims probably involve malingering or symptom exaggeration |
|
|
Postconcussional syndrome
|
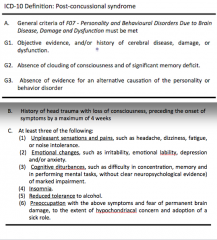
- Most common psychological disturbance following mild TBI
- Common symptoms: fatigue, nausea, changes in sleep and eating patterns, periods of dizziness, hypersensitivity to noise, lessened tolerance to alcohol, irritability, anxiety and depression - There are cross-cultural issues |
|
|
Rivermead Post-Concussion Symptoms Questionnaire
|
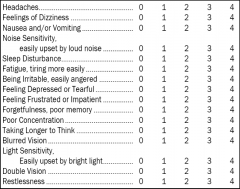
- used to determine the presence and severity of post-concussion syndrome
- Recognition of syndrome: "Compared with before the accident, do you now (i.e., over the last 24 hours) suffer from: ..." 0 = not experienced at all 1 = no more of a problem 2 = mild problem 3 = moderate problem 4 = severe problem |
|
|
Standard assessment of concussion
|
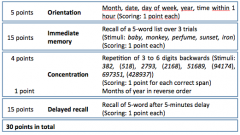
- Appropriate for assessment of the acute status
|
|
|
Why are rehabilitation units for traumatic brain injury so difficult to establish and maintain?
|
- head-injured population is often viewed as burden on society
- rehab is far from straightforward, that is there is no "right" way but many "wrong" way -> commonly need for physical therapy, speech therapy, occupational therapy, cognitive rehabilitation and individual and family-centered psychotherapy and psychoeducation |
|
|
Closed head injuries
|
- most common (90%)
- sudden acceleration, deceleration or rotation - Diffuse damage to nerve fibres because of stretching, shearing, vibration and rotation on axis of brain - damage most severe at brainstem, especially reticular formation, resulting in lowered arousal of cortex - arteries and veins may be torn, leaking blood into brain and causing diffuse disruption or focal damage - focal damage can also be caused by brain rubbing on skull -> mostly inferior frontal lobes and inferior anterior temporal lobe - Coup injuries: damage at site of impact - Contre-coup injuries: damage brain region directly opposite the site of impact - First injury in first few seconds - Second injury, if victim is trapped and can't breath - Third injury include swelling blood from torn vessels increasing pressure, blood clots, chronic subdural hematomas, hydrocephalus |
|
|
Ischemia
|
- restriction in blood supply to tissues
|
|
|
Psychiatric and psychosocial disorders following traumatic brain injury
|
- personality change
-> often result of frontal-lobe damage - emotional lability - irritability - inability to inhibit aggressive and violent reactions - poor control of the expression of (often inappropriate) emotions - Years after TBI depression suicidal thoughts may occur, when patient realises plateaued status |
|
|
Mild traumatic brain injury
|
- combination of:
a) period of unconsciousness of 20min or less b) Glasgow Coma Score of 13-15 on regaining consciousness, usually corresponding to spontaneous eye opening, ability to obey commands, and verbal response may be incoherent or confused c) hospitalisation not greater than 48h d) period of post traumatic amnesia of less than 24h - acute symptoms: headache, nausea, sleepiness, confusion and disorientation |
|
|
Rehabilitation from mild traumatic brain injury
|
- rest
- increase activity and working hours gradually |

