![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
245 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Describe the procedure for performing a breast exam.
|
1. introduce self
2. explain purpose of exam 3. wash hands 4. ask patient to lower gown 5. inspect breasts, nipples, and areolae -arms hanging loosely at sides -hands behind head -hands on hips 6. palpate supraclavicular, infraclavicular, and axillary lymph nodes bilaterally 7. have patient regown on one side 8. have patient lie down and place arm above head on side that is ungowned 9. palpate breast with light, medium, and deep pressure in strips, moving fingers in circles without lifting them 10. repeat with other breast 11. review results 12. ask about self-breast exams |
|
|
|
During inspection of the breasts, what are you examining?
|
size
shape/contour symmetry texture color venous patterns lesions |
|
|
|
During inspection of the nipples and areolae, what are you examining?
|
size
shape symmetry texture eversion/inversion/retraction color discharge |
Mosbys p514
|
|
|
List the breast quadrants.
|
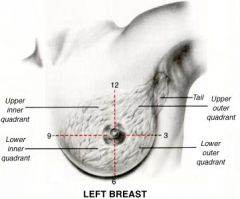
1. UIQ (upper inner quadrant)
2. LIQ (lower inner quadrant) 3. LOQ (lower outer quadrant) 4. UOQ (upper outer quadrant) 5. Tail of Spence |
|
|
|
What should you include when documenting a breast mass?
|
1. location – breast, quadrant, o'clock location from nipple, distance from nipple, document with illustration
2. size – length, width, thickness, document in cm 3. shape – round, oval, lobular, irregular 4. margins – circumscribed, microlobulated, spiculated, ill-defined, obscured 5. consistency – soft, firm, hard 6. mobility – fixed, mobile, direction of mobility 7. retractions – altered contour, dimpling 8. tenderness |
Mosbys p508
|
|

|
supernumerary nipple
|
|
|

What does this breast most likely indicate?
|
peau d'orange → inflammatory or advanced breast cancer
|
|
|
|
What is peau d'orange and what does it indicate?
|
edema of the breast due to blocked lymphatic drainage → indicative of inflammatory or advanced breast cancer
|
Mosbys p502
|
|
|
Describe the location of the breasts.
|
1. between sternal border and midaxillary line
2. superior to pectoralis major m. and serratus anterior m. 3. between 2-3rd rib to 6-7th rib |
Mosbys p492
|
|
|
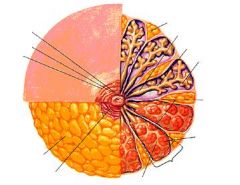
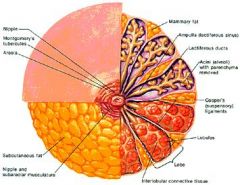
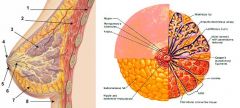
Describe the anatomy of glandular tissue of the breast.
|
each breast consists of 15-20 lobes
each lobe consists of 20-40 lobules each lobule contains acini cells acini cells produce milk that drains into laciferous ducts that drain to nipple |
Mosbys p492
|
|
|
What are Cooper ligaments?
|
suspensory ligaments that support the breasts
|
Mosbys p492
|
|
|
What arteries supply the breasts?
|
1. superificial tissue → intercostal aa.
2. deep tissue and nipples → branches of internal mammary a. and lateral thoracic a. |
Mosbys p492
|
|
|
What are Montgomery tubercles?
|

sebaceous glands in areola which secrete oil for lubrication and protection of nipples and areolae
|
|
|
|
|
|
|
|
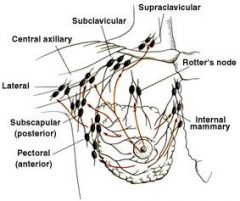
List the lymph nodes that drain the breasts.
|
supraclavicular
infraclavicular axillary internal mammary interpectoral (rotter) subscapular |
|
|
|
Define thelarche.
|
breast development
|
|
|
|
What HPI questions should you ask for breast discomfort/pain?
|
-onset - sudden or gradual
-duration - start, constant, intermittent -severity -character - aching, throbbing, stinging, burning, stabbing, pulling -location - localization, unilateral, bilateral, radiation -associated symptoms - nipple discharge, mass -other - irritation from skin-to-skin contact or bra, strenous activity, recent trauma -relationship to menses |
Mosbys p496
|
|
|
What HPI questions should you ask for nipple discharge?
|
-onset - sudden, gradual
-duration - start, constant, intermittent, spontaneous, provoked -character - amount, color, constistency, odor -location - unilateral, bilateral -associated symptoms - breast pain, nipple retraction, mass -other - recent trauma -relationship to menses |
Mosbys p496
|
|
|
What HPI questions should you ask for breast mass?
|
-onset - when first noticed
-duration - constant, intermittent -character changes - size, consistency, mobility -location - localization -associated symptoms - breast pain, nipple discharge, nipple retraction, breast dimpling, tender lymph nodes -relationship to menses |
Mosbys p496
|
|
|
What PMH questions should you ask for breast complaints?
|
-history of breast disease - fibrocystic changes, fibroadenomas, cancer
-history of cancer - endometrial, ovarian, colorectal -surgeries - breast aspirations, biopsies, implants, reductions, plasties; oophorectomy -mammography history - last mammogram, frequency, results -menstrual history; breast changes during menstruation -pregnancy history -lactation history -menopause -hormonal meds -other meds |
Mosbys p496
|
|
|
Define oophorectomy.
|
surgical removal of ovary/ovaries
|
Stedmans
|
|
|
List risk factors for breast cancer.
|
1. non-modifiable
age - increases with age gender - increases if female genetics - increases if BRCA1 or BRCA2 gene mutations present history of breast cancer family history of breast cancer 2. modifiable childbirth - increased if nulliparity or late age at birth of first child hormone therapy - increased if estrogen and progesterone homrone therapy after menopause obesity alcohol |
Mosbys p497
|
|
|
What is the ddx for unilateral bloody nipple discharge?
|
intraductal papilloma (most common)
mammary duct ectasia breast cancer |
|
|
|
What is the ddx for nipple discharge?
|
pregnancy
lactation nipple stimulation nipple/areola/breast infection/abscess intraductal papilloma (most common) mammary duct ectasia fibrocystic changes breast cancer paget's disease hyperprolactinemia |
|
|
|
When is the best time to perform a self-breast examination?
|
2-3 days following menstruation when breasts are least likely to be tender or swollen
|
Mosbys p498
|
|
|
Define hyperprolactinemia.
|
↑ prolactin in blood
normal during pregnancy and lactation |
|
|
|
How often should self-breast exams be performed?
|
once a month
|
Mosbys p498
|
|
|
Describe a self-breast examination.
|
1. stand in front of mirror and look for anything unusual (size, shape, symmetry, nipple discharge, puckering, dimpling)
-arms at sides -hands behind head -hands on hips 2. move fingers in circle, feeling for any lumps -check entire breast -check armpit |
Mosbys p499
|
|
|
What are the recommendations for breast cancer screening?
|
1. clinical breast exam
-if <40y/o, every 1-3 years if >40y/o, every year 2. mammogram -if average risk, start at 40y/o, every year -if increased risk, consider more frequent CBE, earlier mammogram, additional tests 3. self breast examination -optional -if >20, monthly |
Mosbys p500
|
|
|
Describe peau d'orange.
|
skin of breast resembles orange peel due to thickened skin, enlarged pores, and accentuated skin markings
|
Mosbys p502
|
|
|
What is the ddx for visible venous patterns in breasts?
|
normal, bilateral
-obesity -pregnancy abnormal, unilateral -dilated veins due to ↑ blood flow to malignancy |
Mosbys p502
|
|
|
Which part of the breast is peau d'orange often first visible?
|
areola
|
Mosbys p502
|
|
|
What is the ddx for nipple inversion?
|
-if lifetime inversion → normal
-if recent inversion → cancer |
Mosbys p502
|
|
|
When should nipple compression be performed?
|
only if complaint of spontaneous nipple discharge
|
Mosbys p509
|
|
|
Define galactorrhea.
|
milk production in non-pregnant or non-lactating woman
|
|
|
|
Define gynecomastia.
|
abnormally large mammary glands in males
|
|
|
|
Define amastia.
|
absence of breast, aveola, and nipple
may be congenital or iatrogenic |
|
|
|
Define polymastia.
|
extra breast(s)
|
|
|
|
Define mastalgia.
|
breast pain
|
|
|

|
amastia
|
|
|
|
Define supernumerary nipple.
|
congenital accessory nipple(s) located in milk line
|
|
|

|
polymastia
|
|
|

|
Left: asymmetric gynecomastia
Right: normal |
|
|
|
List possible signs/symptoms of breast cancer.
|
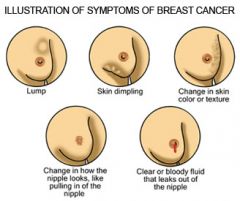
nipple discharge
nipple retraction breast dimpling breast mass peau d'orange |
|
|
|
List lifestyle changes that can reduce risk of breast cancer.
|
1. reduce alcohol intake to ≤ 1 drink per day
2. exercise regularly to maintain healthy weight 3. avoid postmenopausal combination hormone therapy |
Mosbys p510
|
|
|
How do you differentiate between nipple inversion and nipple retraction?
|
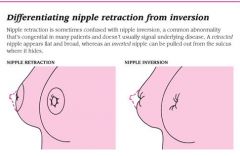
|
|
|

|
nipple retraction due to breast cancer
|
|
|

|
paget's disease of the breast
|
|
|

|
dimpling due to breast cancer
|
|
|
|
What are the indications for performing a breast exam?
|
routine health maintenance
mastalgia nipple discharge changes in breast appearance breast mass |
|
|
|
Define mastitis.
|
inflammation of breast tissue
|
|
|
|
Who is most commonly affected by mastitis?
|
lactating women where blocked lactiferous ducts (due to inadequate emptying or tight bra) cause engorgement and subsequent mastitis
|
|
|

|
mastitis
|
|
|
|
*notes on breast exam
|
1. don't peer, stand up straight
2. have patient press down on hips 3. do 3 complete circles 4. include notation of tattoos if in area |
|
|
|
What is the ddx for gynecomastia?
|
puberty
hormonal imbalance pituitary or testicular tumor steroid or estrogen-containing medications |
|
|
|
Ovaries can be found at the level of what surface landmark?
|
ASIS
|
Mosbys p582
|
|
|
What is the function of the bartholin glands?
|
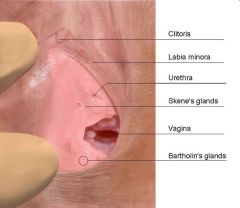
secrete mucus for vaginal lubrication during sexual excitation
|
Mosbys p579
|
|
|
Why might a pelvic exam be performed?
|
1. general health check-up - important to detect infections, STIs, cancer in early stages, other reproductive problems
2. suspected vaginal infections (candidiasis, bacterial vaginosis) 3. suspected STIs (trichomonasis, gonorrhea, chlamydia, herpes, HPV) 4. screen for cervical abnormalities (PAP) 5. evaluate abdominal/pelvic pain 6. evaluate abnormal uterine bleeding 7. evaluate pelvic organ abnormalities (uterine fibroids, ovarian cysts, uterine prolapse) 7. required before prescribing certain contraception (IUD, diaphragm) 7. collect evidence for sexual assault |
|
|
|
What is the ddx for cervical motion tenderness?
|
PID
ovarian cyst ectopic pregnancy |
|
|
|
What is anteversion?
|
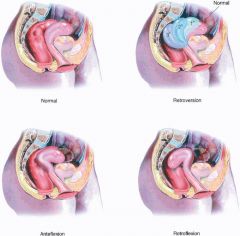
uterus tipped anteriorly (normal)
|
|
|
|
What is retroversion?
|
uterus tipped posteriorly
|
|
|
|
What is anteflexion?
|
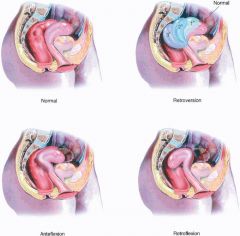
fundus of uterus anterior to cervix; anterior of uterus is concave
|
|
|
|
What is retroflexion?
|
fundus of uterus posterior to cervix; anterior of uterus is convex
|
|
|
|
What is the position of the uterus found in most women?
|
anteverted and anteflexed
|
|
|
|
What are the 3 layers of the uterus?
|
endometrium
myometrium perimetrium |
|
|
|
List the parts of the uterus.
|
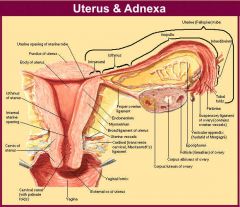
1. corpus
-fundus -body -isthmus 2. cervix -internal os -cervical canal -external os |
|
|
|
What is the etiology of a bartholin cyst?
|
blockage of bartholin gland due to trauma, inflammation, or infection, resulting in fluid-filled cyst
|
|
|
|
What are the complications of a bartholin cyst?
|
may progress to bartholin abscess (i.e. infected bartholin cyst)
*abscess likely if pain present |
|
|

|
bartholin cyst/abscess
|
|
|

|
bartholin cyst/abscess
|
|
|
|
What is the function of the skene glands?
|
associated with female ejaculation (homologous to male prostate)
|
|
|
|
What is dispareunia?
|
painful sexual intercourse
|
|
|
|
What is the etiology of a skene duct cyst?
|
blockage of skene gland usually due to infection
|
|
|
|
What are the complications of a skene duct cyst?
|
skene duct abscess
urethral obstruction recurrent UTIs |
|
|
|
Describe vaginal discharge due to candida.
|
white curd-like discharge
|
|
|
|
What is the ddx for vaginal discharge?
|
normal discharge
bacterial vaginosis (BV) vulvovaginal candidiasis (candidal vaginitis) trichomoniasis (trichomonal vaginitis) gonorrhea chlamydia atrophic vaginitis allergic vaginitis pelvic inflammatory disease (PID) cervicitis foreign body infected IUD |
|
|
|
What organism causes bacterial vaginosis most commonly?
|
gardnerella vaginalis
|
|
|

|
cystocele
|
|
|

|
cystocele
|
|
|

|
uterine prolapse
|
|
|

|
rectocele
|
|
|
|
What is vaginitis?
|
non-infectious or infectious inflammation of the vaginal mucosa (and sometimes inflammation of the vulva)
|
|
|
|
What is pelvic inflammatory disease (PID)?
|
infection of the upper female genital tract (i.e. cervix, uterus, fallopian tubes, or ovaries)
|
|
|
|
Define cystocele.
|
prolapse/herniation of urinary bladder into vagina
|
|
|
|
Define rectocele.
|
prolapse/herniation of rectum into vagina
|
|
|
|
What are the adnexa of the uterus?
|
appendages of the uterus (i.e. fallopian tubes, ovaries, and associated ligaments)
|
|
|
|
During pregnancy, when should you order hct and 1 hour glucose?
|
28 weeks
|
|
|
|
During pregnancy, when should you order GBSDNA probe?
|
36 weeks
|
|
|
|
Define urethrocele.
|
prolapse/herniation of urethra into vagina
|
|
|
|
List 7 broad pelvic complaints.
|
1. pain
2. urinary symptoms 3. premenstrual symptoms 4. menopausal symptoms 5. vaginal dischage 6. abnormal uterine bleeding 7. infertility |
|
|
|
Describe the normal appearance of the cervix in a nulliparous patient.
|

pink uniform squamous epithelium; os appears small and round
|
Mosbys p601
|
|
|
Describe the normal appearance of the cervix in a parous patient.
|

pink uniform squamous epithelium; os appears as horizontal slit
|
Mosbys p601
|
|
|
Candida albicans is part of normal flora, true or false?
|
true
found in oropharynx, large intestine, and vagina |
|
|
|
List red flags for sexual abuse.
|
1. medical
-general neglect or physical abuse -trauma or scarring of genital or anal areas -ususual skin color in genital or anal areas -STI -genitourinary symptoms (pruritus, pain, rash, lesions, odor, bleeding, discharge, dysuria, hematuria, UTI, enuresis) -anorectal symptoms (pruritus, pain, bleeding, fecal incontinence, poor anal sphincter tone, bowel habit dysfunction) 2. behavior -school problems -dramatic weight change/eating habits -depression -sleep problems -sudden personality/behavior changes -sudden avoidance of certain people/places 3. sexual behavior -excessive masturbation or sexual behavior -repeated object insertion -sexually provacative mannerisums -age-inappropriate sexual knowledge -sex play between children with >4 years age difference -sex play involving force, threats, bribes -child asking to be touched/kissed in genital area |
Mosbys p611
|
|
|
What are clue cells?
|
epithelial cells coated by Gardnerella vaginalis
indicative of bacterial vaginosis |
|
|

What does this vaginal discharge indicate?
|
thin milky white discharge → bacterial vaginosis
|
|
|
|
VULVOVAGINAL CANDIDIASIS
|
ETIOLOGY:
caused by candida albicans (90%) may be associated with pregnancy, obesity, systemic disorder (DM, HIV), medication (antibiotics, corticosteroids, oral contraceptives), chronic debilitation occurs in 75% of women CLINICAL PRESENTATION: severe vulvar pruritis vulvar erythema white cottage-cheesy vaginal discharge +/- burning following urination +/- labia minora erythema, excoriation, edema if affecting skin adjacent to labia, think DM or other systemic illness DIAGNOSTIC WORKUP pH normal (≤4.5) wet mount (KOH) → pseudohyphae fungal culture MANAGEMENT: 1. treat only if symptomatic 2. d/c antibiotics if possible 3. control underlying disease 4. avoid nonabsorbent undergarments 5. avoid douching |
|
|
|
Describe vaginal discharge due to bacterial vaginosis.
|
thin milky white discharge
|
|
|
|
BACTERIAL VAGINOSIS
|
ETIOLOGY:
altered vaginal flora (decreased lactobacilli + overgrowth of Gardnerella vaginalis, Mobiluncus, Prevotella, Porphyromonas, Bacteroides, Peptostreptococcus) CLINICAL PRESENTATION: grayish-white vaginal discharge fishy odor (more noticeable following unprotected intercourse) non-irritating DIAGNOSTIC WORKUP: pH 5.0-5.5 whiff test positive (fishy odor following application of KOH) wet mount → clue cells, ↓ lactobacilli, few WBCs gram stain → lots of small gram-negative bacteria, few lactobacilli *gram stain more sensitive (93%) and specific (70%) than wet mount MANAGEMENT: treat symptomatic patients and consider treating asymptomatic patients IF NON-PREGNANT: Options include: 1. metonidazole 2g PO single dose 2. metronidazole 500 mg PO twice daily x 5 days 3. clindamycin 300 mg PO 2x daily x 7 days 4. metronidazole gel 0.75% (1 full applicator, 5g) intravaginally once or twice daily x 5 days 5. clindamycin cream 2% (1 full applicator, 5g) intravaginally at bedtime x 7 days 6. clindamycin ovules 100g intravaginally at bedtime x 3 days 7. inform patients that condoms or diaphragms may be weakened during treatment with clindamycin cream since it is oil-based IF PREGNANT: Options include: 1. metronidazole 250mg PO 3x daily x 7 days 2. clindamycin 300 mg PO 2x daily x 7 days 3. do not use topical agents COMPLICATIONS: PID, post-abortion infection, post-hysterectomy vaginal cuff cellulitus PREVENTION: condoms hydrogen peroxide douches oral or vaginal application of yogurt containing lactobacillus acidophilus intravaginal planting of exogenous lactobacilli prophylaxis longer treatment periods *treatment of male does not help prevent recurrence in female MATERNAL-FETAL TRANSMISSION: BV may increase risk of preterm delivery, though treatment of asymptomatic pregnant women does not necessarily reduce risk of preterm delivery or adverse outcomes |
|
|
|
GONORRHEA
|
ETIOLOGY:
sexually transmitted infection caused by Neisseria Gonorrhoeae infects glandular structures of vulva, perineum, anus, urethra, and cervix CLINICAL PRESENTATION: symptoms range from asymptomatic (85%) to severe copious mucopurulent discharge DIAGNOSTIC WORKUP: gram stain → gram-negative diplococcic within WBCs NAAT or GCCHDNA MANAGEMENT: IF UNCOMPLICATED, options include: 1. ceftriaxone 125 mg IM single dose (3rd gen cephalosporin) 2. cefixime 400 mg PO single dose (3rd gen cephalosporin) 3. ciprofloxacin 500 mg PO single dose (2nd gen quinolone) 4. ofloxacin 400 mg PO single dose (2nd gen quinolone) 5. levofloxacin 250 mg PO single dose (3rd gen quinolone) 6. If infection acquired while in California, Asia, or the Pacific (including Hawaii) → spectinomycin 2g IM single dose (d/t cephalosporin or quinolone resistance) 7. treat for chlamydia COMPLICATIONS: salpingitis, tubo-ovarian abscess, peritonitis ectopic pregnancy, infertility PREVENTION: safe sex practices including condoms MATERNAL-FETAL TRANSMISSION: if active infection present during delivery, newborn may develop conjunctivitis |
|
|
|
What organism is considered normal flora of the vagina?
|
lactobacilli
|
|
|
|
CHLAMYDIA
|
ETIOLOGY:
sexually transmitted infection caused by Chlamydia Trachomatis CLINICAL PRESENTATION: may be asymptomatic dysuria post-coital bleeding mucopurulent cervicitis may present as lymphogranuloma venereum (LGV) → initially a painless, vesicular, transient lesion or shallow ulcer of vulva; retroperitoneal lymphadenopathy; may progress to genital or anal fistulas, strictures, or rectal stenosis; uncommon in U.S. but common in SE Asia and Africa DIAGNOSTIC WORKUP: NAAT or GCCHDNA MANAGEMENT: 1. treat patient and partner 2. azithromycin 1 g PO single dose 3. other options include doxycycline, erythromycin, ofloxacin, levofloxacin 4. avoid sex for 7 days 5. repeat screening 3-4 months following treatment 6. if persistent symptoms, recurrence, or pregnancy → test for cure 7. if LGV → doxycycline 100mg 2x daily x 21 days 8. treat gonorrhea COMPLICATIONS: salpingitis, tubual occlusion, ectopic pregnancy, infertility PREVENTION: screen all sexually active women safe sex practices including use of condoms MATERNAL-FETAL TRANSMISSION: neonatal conjunctivitis |
|
|
|
What equipment is needed for the pelvic exam?
|
gown
drape stirups light gloves speculum pap broom/vial gc/chlam dna probe cotton swab and saline solution lubrication fecal occult card |
|
|
|
TRICHOMONIASIS
|
ETIOLOGY:
sexually transmitted infection caused by Trichomonas vaginalis (unicellular flagellate protozoan) infects lower urinary tract of women and men most prevalent non-viral STI in U.S. CLINICAL PRESENTATION: copious greenish-white frothy vaginal discharge vaginal wall erythema strawberry cervix +/- malodor, urinary symptoms, vulvar pruritis, labia minora edema and tenderness DIAGNOSTIC WORKUP: pH > 5.0 wet mount → motile trichomonads, ↑ PMNs *Trichomonas vaginalis are larger than PMNs but smaller than epithelial cells MANAGEMENT: 1. treat patient and partner 2. metronidazole 2g PO single dose 3. metronidazole 500mg PO 2x daily x 7 days 4. avoid alcohol to prevent severe nausea and vomiting 5. avoid sex or use condoms until treatment completed 6. if persistent symptoms → repeat metronidazole after 4-6 weeks if presence of trichomonads confirmed and WBC normal 7. if resistance → 2-4g daily x 10-14 days, consult CDC 8. evaluate for gonorrhea, chlamydia, syphilis, and HIV COMPLICATIONS: PREVENTION: safe sex practices including use of condoms use of spermicidal agents (Nonoxynol 9) MATERNAL-FETAL TRANSMISSION: increased transmission of HIV |
|
|
|
The cervix feels similar to cartilage of the nose, true or false?
|
true
|
|
|
|
*pelvic exam notes
|
1. angle speculum downward
2. do wet mount before pap/gc/chlam 3. cervix should feel like cartilage |
|
|
|
Define vestibule.
|
area enclosed by labia minora
|
|
|
|
What is the function of the ovaries?
|
secrete estrogen and progesterone which control menstrual cycle and support pregnancy
|
|
|
|
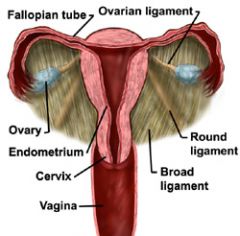
What are the 3 parts of the broad ligament of the uterus?
|
mesosalpinx
mesoovarium mesometrium |
|
|
|
List 5 ligaments that support the uterus.
|
ovarian ligament
broad ligament round ligament cardinal ligament uterosacral ligament |
|
|
|
What is a urethrocele?
|
prolapse of female urethra into vagina
|
|
|
|
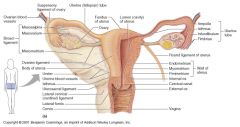
Describe breast anatomy.
|
|
|
|
|
Describe breast lymph nodes.
|
|
|
|
|
How do you differentiate nipple retraction vs. inversion?
|
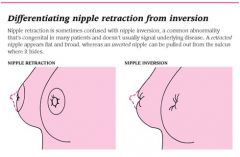
|
|
|
|
Define mastalgia.
|
breast pain
|
|
|
|
Define polymastia.
|
extra breast(s)
|
|
|
|
Define galactorrhea.
|
milk production in absence of lactation or pregnancy
|
|
|
|
Define supernumerary nipple.
|
extra nipple(s)
|
|
|
|
Define amastia.
|
absence of breast, areola, and nipple; congenital or iatrogenic
|
|
|
|
Describe the documentation for a breast mass.
|

1. location – breast, quadrant, o’clock position from nipple, distance from nipple (document with illustration)
2. size – length, width, thickness (document in cm) 3. shape – round, oval, lobular, irregular 4. margins – circumscribed, microlobulated, spiculated, ill-defined, obscured 5. consistency – soft, firm, hard 6. mobility – fixed, mobile, direction of mobility 7. retractions – altered contour, dimpling 8. tenderness |
|
|
|
Describe how to collect and perform a wet mount.
|
1. swab vagina
2. place swab in saline (NaCl) 3. add drop of discharge/saline to one side of slide a. place cover slip over it b. examine slide using microscope at 40X c. look for RBCs, WBCs, clue cells, trichomonas 4. add drop of discharge/saline to other side of slide d. add drop of KOH e. place cover slip over it f. examine slide g. look for yeast |
|
|
|
What are the indications for a wet mount?
|
vaginal discharge
|
|
|
|
What is a wet mount?
|
suspension of vaginal discharge in saline
|
|
|
|
What are the components of a back office wet mount?
|
a. RBCs
b. WBCs c. KOH → yeast – budding yeast or pseudohyphae d. trichomonas e. clue cells f. whiff test → odor after adding KOH? |
|
|
|
Define amenorrhea.
|
absence of menses
|
|
|
|
Define menorrhagia (AKA hypermenorrhea).
|
abnormally heavy or prolonged menses
|
|
|
|
Define thelarche.
|
onset of breast development
|
|
|
|
Define menarche.
|
onset of menstruation
|
|
|
|
Define pubarche.
|
first appearance of pubic hair
|
|
|
|
Define polymenorrhea.
|
abnormally frequent menses
|
|
|
|
Define oligomenorrhea.
|
abnormally light or infrequent menses
|
|
|
|
Define metrorrhagia.
|
menstrual bleeding at irregular intervals, particularly in between expected menstrual periods
|
|
|
|
Define menometrorrhagia.
|
abnormally heavy and prolonged menses that occurs at irregular intervals
|
|
|
|
Define post-coital bleeding.
|
vaginal bleeding following intercourse
|
|
|
|
Define hypomenorrhea.
|
abnormally light and shortened menses
|
|
|
|
Define cryptomenorrhea.
|
condition characterized by the occurence of menstruation without visible blood due to obstruction of the outflow tract
|
|
|
|
Define prenatal.
|
before birth
|
|
|
|
Define perinatal.
|
interval from 28 weeks gestations to 7 days of life
|
|
|
|
Define postnatal.
|
after birth
|
|
|
|
Define mittelschmerz.
|
pain due to ovulation
mittelschemerz means "middle pain" presents as unilateral lower abdominal pain |
|
|
|
Define puberty.
|
process of physical changes by which a child's body becomes an adult body capable of reproduction
|
|
|
|
Define infertility.
|
the state of being unable to produce offspring
|
|
|
|
Define gravida/gravity.
|
women who is or has been pregnant; number of pregnancies regardless of outcome
*include current pregnancy |
|
|
|
Define nulligravida, primigravida, and multigravida.
|
nulligravida = women who has never been pregnant
primigravida = women who is pregnant for the first time or has been pregnant once multigravida - women who has been pregnant 2 or more times |
|
|
|
Define para/parity.
|
women who has given birth; number of viable births (>20 weeks) regardless of outcome
*count multiple births as 1 |
|
|
|
Define nulliparous, parous, and multiparous.
|
nulliparous = women who has never given birth or completed a pregnancy beyond 20 weeks
parous = women who has given birth once multiparous = women who has given birth 2 or more times |
|
|
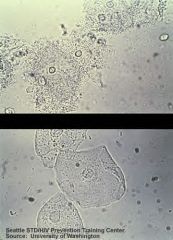
What do these wet mount slides indicate?
|
Top: clue cells → bacterial vaginosis
Bottom: epithelial cells → normal wet mount |
|
|
|
How is gravity/parity documented?
|
GP, GPA, or G/TPAL, where:
G = number of pregnancies P = number of viable births (>24 weeks) T = number of term births (≥37 weeks) P = number of preterm births (>24 weeks or <37 weeks) A = number of abortions (<24 weeks) (spontaneous or induced) L = number of living children *count multiple births as 1 1. 2 pregnancies resulting in 2 live births = G₂P₂ 2. 2 pregnancies resulting in 1 live birth and 1 miscarriage = G₂P₁A₁ 3. 4 pregnancies resulting in 2 term births, 1 preterm birth, 1 miscarriage, and 3 living children = G4T2P1A1L3 |
|
|
|
How is the last menstrual period (LMP) documented?
|
first day of last menstrual period
|
|
|
|
What happens to the maternal blood volume during pregnancy?
|
↑ 40-50%
mainly due to ↑ plasma volume begins during 1st trimester and peaks after 30th week returns to normal 3-4 weeks post-delivery |
Mosby's p422
|
|
|
Define colostrum.
|
first milk secreted at termination of pregnancy
contains more protein and minerals than mature milk also contains antibodies and host resistance factors |
Stedmans
|
|
|
What changes occur in the breast as a result of pregnancy?
|
1. nipples darken, become more prominent and erect
2. areolae darken and enlarge 3. montgomery tubercles appear due to sebaceous gland hypertrophy 4. breasts enlarge (sometimes 2-3 times normal size) due to increased glandular tissue 5. veins become visible due to increased vascularization |
Mosbys p495
|
|
|
Breasts rarely return to pre-lactation size, true or false?
|
true
|
Mosbys p495
|
|
|
Following colostrum production, when does milk production occur?
|
2-4 days following delivery
|
Mosbys p495
|
|
|
What causes lactation to occur?
|
↑ prolactin
↓ estrogen sucking stimulation |
Mosbys p495
|
|
|
Discuss the initial presentation of sexual assault.
|
often present to emergency department complaining of being mugged or concerned about STIs/HIV and do not admit to being raped
may present with psychiatric symptoms (depression, anxiety, suicide attempt) |
|
|
|
Discuss the long-term sequelae of sexual assault.
|
PTSD characterized by intense pyschological distress, psychic numbing, re-experiencing of trauma, and avoidance of stimuli associated with trauma
difficulty in reestablishing sexual and emotional relationships (50%) suicidal ideation (33-50%) suicide attempts (20%) |
|
|
|
What is sexual assault?
|
any sexual act performed by one person on another without the person's consent
includes genital, oral, or anal penetration by the assaulter or by an object may result from force, the threat of force either on the victim or another person, or the victim's inability to give appropriate consent |
|
|
|
List sexual assault statistics.
|
700,000 to 1,000,000 American women are sexually assaulted every year
only 30% reported to the police 50% of rape victims tell no one 20% of adult women, 15% of college-age women, and 12% of adolescent girls have experienced sexual abuse and assault during their lifetime incidence may be higher for African American women and for adolescent females adolescents, elderly, and physically/developmentally disabled are particularly vulnerable |
|
|
|
List date rape drugs.
|
flunitrazepam (Rohypnol)
gamma-hydroxybutyrate (GHB) |
|
|
|
Discuss initial assessment of sexual assault.
|
obtain informed consent prior to examining sexual assault victim
obtain history and physical exam in presence of chaperone ask patient to describe attacker and course of events history → LMP, contraceptive, pre-existing pregnancy, pre-existing infection, last consensual sex before assault, activities between assault and examination (eating, drinking, urination, defecation, bathing, douching) physical exam → inspect skin, oropharynx, and breasts for trauma (take photos), perform pelvic/rectal exam (moisten speculum only with saline, inspect for trauma or foreign objects) rape kit saliva TRIC GCCHDNA probe PAP smear HEPB RPR HIV collect samples of attacker (pubic hair, fingernail scrapings, blood, semen) inform victim she will likely experience rape-trauma syndrome and advise to seek help if and when these symptoms occur FUV in 2 weeks for repeat physical exam,TRIC, and GCCHDNA refer for counseling monitor for alcohol and drug abuse monitor for pysch symptoms (depression, suicidal ideation) repeat HEPB and RPR in 12 weeks repeat HIV in 6 months |
|
|
|
"Rape" and "physical assault" are legal terms that should not be used in the medical record, true or false?
|
true
instead report findings as "consistent with use of force" |
|
|
|
Describe the rape-trauma syndrome.
|
ACUTE PHASE:
may last for hours or days characterized by a distortion or paralysis of the individual's coping mechanisms responses vary from complete loss of emotional control (crying, uncontrolled anger) to an unnatural calm and detachment DELAYED PHASE: may occur months or years after the sexual assault characterized by chronic anxiety, feelings of vulnerability, loss of control, self-blame, anxiety, nightmares, flashbacks, catastrophic fantasies, feelings of alienation and isolation, sexual dysfunction, psychological distress, mistrust of others, phobias, depression, hostility, and somatic symptoms (fatigue, HAs, nausea, myaglias, eating disturbances, sleep disturbances, intense startle reactions) |
|
|
|
When does ovulation occur?
|
day 14 of menstrual cycle (i.e. 14 days after 1st day of period)
|
|
|
|
What are the phases of the menstrual cycle and the major hormone associated with each?
|
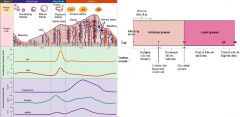
PROLIFERATIVE PHASE (AKA follicular phase):
day 1-14 menstruation d/t no fertilization follicular development major hormone = estrogen OVULATION: day 14 ovum released from follicle major hormones = surge in LH and FSH, slight surge in estrogen SECRETORY PHASE (AKA luteal phase): day 14-28 corpus luteum development corpus luteum degeneration if no fertilization occurs major hormone = progesterone |
|
|
|
List questions for a sexual history.
|
Now I am going to take a few minutes to ask you some direct questions about your
sexual health. These questions are very personal, but it is important for me to know so I can help you be healthy. I ask these questions to all of my patients regardless of age or marital status and they are just as important as other questions about your physical and mental health. Like the rest of this visit, this information is strictly confidential. Are you currently sexually active? Do you have sex with men, women, or both? How many partners do you currently have? How many partners have you had in the last 2 months? The last year? Do you use any substances or devices to enhance your sexual experience? Are you trying to get pregnant? Are you concerned about getting pregnant or getting a partner pregnant? What are you doing to prevent pregnancy? Oral contraceptives? Patch? Injection? IUD? Have you ever been tested for HIV? Do you want to be? Have you ever had any STIs? How about your partners? If so, what was it and when did it occur? Have you or any of your partners used injected drugs? Have you or any of your partners had sex with a prostitute? Have you gotten your hepB vaccines? What are you doing to protect yourself against sexually transmitted infections and HIV? Condoms? What type of sex do you have? Vaginal, oral, or anal? Do you use condoms? If not, why not? In what situations do you use condoms? Are there any changes with your or your partner's sexual desire? In frequency of sex? Do you have difficulty getting or maintaining an erection? Do you have difficulty getting an orgasm? Do you have any pain with sex? |
|
|
|
What are the breast cancer screening recommendations from American Cancer Society, American College of Gynecologists, and USPSTF?
|
American Cancer Society:
1. yearly mammogram starting at age 40 2. CBE every 3 years if 20-39 and yearly starting at age 40 3. optional SBE starting at age 20 4. MRI if risk factors (FH) American College of Gynecologists: 1. mammogram every 1-2 years if 40-49 2. mammogram yearly if ≥50 3. optional SBE USPSTF: 1. mammography every 2 years if 50-74 (grade B) 2. mammography before age 50 depends on risk factors and patient values (grade C) 3. insufficient evidence to recommend mammography after age 74 (grade I) 4. SBE is not recommended (grade D) 5. insufficient evidence to recommend CBE (grade I) 6. insufficient evidence to recommend digital mammography or MRI (grade I) |
|
|
|
Describe the role of vaginal estrogen pre-menopause.
|
premenopausal → estrogen thickens vaginal epithelium and results in presence of intraepithelial glycogen → glycogen results in production of lactic acid → lactic acid promotes growth of normal vaginal flora (lactobacilli and acidogenic corynebacteria)
|
Current OB/Gyn
|
|
|
Describe the role of vaginal estrogen post-menopause.
|
postmenopausal → endogenous estrogen production declines → vaginal epithelium loses glycogen → vaginal acidity declines → lactobacilli replaced by mixed flora (pathogenic cocci) → vagina becomes atrophic and more prone to trauma and infection
|
Current OB/Gyn
|
|
|
What does normal physiologic vaginal discharge look like?
|
white and milky
|
|
|
|
Define leukorrhea.
|
vaginal discharge
|
|
|
|
What questions should be asked about vaginal discharge?
|
amount
color odor consistency associated pruritus associated dyspareunia |
|
|
|
What is the w/u for vaginal discharge?
|
1. history → vulvar or vaginal pain, pruritis, discharge, sexual activity, feminine hygiene products (douching, soaps, perfumes), overlying garments, medications (OCP, abx), previous infections, underlying medical conditions (diabetes)
2. physical examination → vulva, vaginal walls, and cervix 3. labs → pH, whiff test, wet mount |
|
|
|
A mixed vaginal bacterial flora is expected when?
|
premenarche
postmenopause |
|
|
|
Lactobacilli (vaginal flora) produce?
|
hydrogen peroxide
|
|
|
|
NABOTHIAN CYSTS:
|
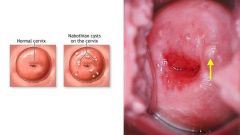
tunnel or cleft of tall columnar endocervical epithelium becomes covered by squamous metaplasia
few mm to 3 cm translucent or yellow |
|
|
|
LEIOMYOMA OF UTERUS:
|
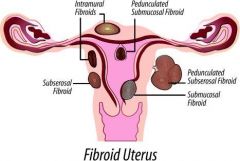
AKA uterine fibroid
benign smooth muscle neoplasm originate in myometrium of uterus associated with abnormal uterine bleeding |
|
|
|
POLYCYSTIC OVARIAN SYNDROME (POS):
|
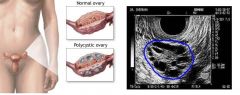
characterized by persistent anovulation
related to hypothalamic pituitary dysfunction and insulin resistance. enlarged polycystic ovaries, secondary amenorrhea or oligomenorrhea, infertility, obesity, hirsutism diagnosed if 2 of the following are present: 1. oligomenorrhea or amenorrhea 2. hyperandrogenism 3. polycystic ovaries on ultrasound – “oyster ovaries,” enlarged, sclerocystic with smooth pearl-white surfaces without indentations diagnostic w/u: elevated androgens, high LH, low FSH (increased LH/FSH ratio), low day-21 progesterone (anovulation), lipid abnormalities, insulin resistance |
|
|
|
ENDOMETRIOSIS:
|
endometrial-like cells grow in areas other than endometrium
reproductive age constant pelvic pain premenstrual low sacral backache which subsides following onset of menses dyspareunia especially with deep penetration dysmenorrhea, infertility tender nodules in the posterior vaginal fornix uterine motion tenderness |
|
|
|
ADENOMYOSIS:
|
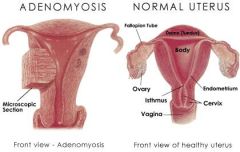
growth of endometrium into myometrium
may be distinct nodules (adenomyomas) or diffuse etiology unknown classic presentation – parous, middle-aged, menorrhagia, dysmenorrheal, symmetrically enlarged uterus menorrhagia premenstrual or comentrual dysmenorrheal menorrhagia uterus uniformly enlarged, globular, boggy hysterectomy curative |
|
|
|
TERATOMA:
|
AKA dermoid cyst
benign ovarian neoplasm derived from any of the 3 germ cell layers reproductive-age asymptomatic unless torsion or rupture transvaginal ultrasound laparoscopic removal |
|
|
|
CERVICAL POLYPS:
|
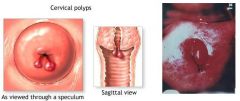
benign cervical neoplasm
common in multigravidas >20y/o rare before menarche often asymptomatic intermenstrual or post-coital bleeding menorrhagia leukorrhea if endocervical → red, smooth, narrow pedicle, soft, protrusion from cervical canal at external os if ectocervical → pale, flesh-colored, smooth, rounded or elongated, broad pedicle hysterosalpingogram or hysteroscopy if polyp high in endocervical canal remove and biopsy b/c malignant change may occur |
|
|
|
List ddx for cervicitis.
|
INFECTIOUS:
chlamydia gonorrhea trichomoniasis genital herpes HPV BV irritation from diaphragm, cervical cap allergy to latex of condoms, spermicides |
|
|
|
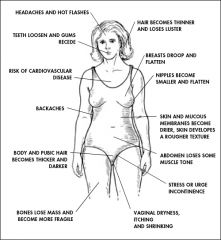
What is menopause?
|
cessation of menses due to aging or bilateral oophorectomy
no menstruation for 1 year |
|
|
|
What is the etiology of menopause?
|
aging
bilateral oophorectomy premature menopause: ovarian failure and menstrual cessaton <40y/o often d/t genetic or autoimmune |
|
|
|
What is the clinical presentation of menopause?
|
~51y/o if d/t aging
hot flashes night sweats vaginal dryness dyspareunia mood changes → anxiety, depression etc. thinned vaginal mucosa → pale smooth vaginal mucosa small cervix and uterus ovaries non-palpable |
|
|
|
What is the diagnostic workup of menopause?
|
elevated FSH and LH
|
|
|
|
What is the management of menopause?
|
1. for hot flashes → consider estrogen/progestin therapy or SSRIs
2. for vaginal atrophy → lubrications, vaginal creams, estradiol vaginal ring 3. calcium and vitamin D supplements 4. monitor for osteoporosis and treat accordingly 5. if vaginal bleeding occurs following menopause → R/O endometrial cancer 5. provide education and support and referral to midlife discussion groups 6. if surgical menopause → immediate estrogen therapy that is then tapered |
|
|
|
How long does menopause last?
|
menstruation diminishes until absent usually over 1-3 year period
|
|
|
|
What are hot flashes?
|
feeling of intense heat over face and trunk
flushing sweating worse following oophorectomy may occur at night and cause insomnia and fatigue |
|
|
|
What is the controversy behind menopause-associated hormone replacement therapy?
|
estrogen-progestin therapy increased risk of cardiovascular disease, cerebrovascular disease and breast cancer
can consider prescribing if early menopause + severe hot flashes but d/c after 3-4 years |
|
|
|
How long do hot flashes typically last?
|
2-3 years
|
|
|
|
List most common types of gestational trophoblastic disease.
|
hydatidiform mole
choriocarcinoma |
|
|
|
HYDATIFORM MOLE:
|
over-production of tissue supposed to develop into placenta
2 types: 1. Partial – abnormal placenta + some fetal development 2. Complete – abnormal placenta + no fetal development Etiology unknown but may be associated with diet low in protein, animal fat, and vitamin A Usually benign but may develop into cancer ( hyperemesis vaginal bleeding in 1st trimester preeclampsia before 24 weeks abnormally large uterus gestational age absent fetal heart tones serial HCG higher than expected ultrasound with absent fetus D & C or hysterectomy may develop into choriocarcinoma |
|
|
|
CHORIOCARCINOMA:
|
type of gestational trophoblastic disease
may result from hydatidiform mole, abortion, ectopic pregnancy usually late vaginal bleed in postpartum enlarged uterus, ovaries vaginal lesions serial HCG chemotherapy |
|
|
|
What is the normal pH of the vagina?
|
3.5-4.0
|
Current OB/Gyn
|
|
|
List the 4 criteria for diagnosis of bacterial vaginosis.
|
1. thin white/yellow homogenous discharge
2. pH > 4.5 3. clue cells 4. fishy odor (after adding KOH) *3 of 4 must be present for diagnosis |
|
|
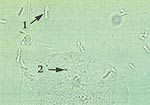
What does this wet mount slide indicate?
|
lactobacilli (1) and epithelial cells (2) → normal wet mount
|
|
|
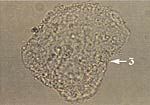
What does this wet mount slide indicate?
|
clue cell (3) → bacterial vaginosis
|
|
|
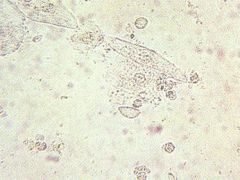
What does this wet mount slide indicate?
|

trichomonas and WBCs → trichomoniasis
|
|
|
|
For suspected ovarian cancer, which tumor marker would you order?
|
CA 125
|
|
|
|
Do yeast form hyphae or pseudohyphae?
|
pseudohyphae
*yeast are unicellular and therefore cannot form hyphae, but yeast can form pseudohyphae if incomplete budding occurs and cells remain intact after division |
|
|
|
A wet mount with a fishy odor (positive whiff test) is indicative of?
|
bacterial vaginosis or trichomoniasis
|
|
|
|
What are clue cells and what are they indicative of?
|
epithelial cells coated in bacteria that are indicative of bacterial vaginosis
|
|
|
|
What is the normal range for vaginal pH?
|
3.8-4.2
|
|
|
|
How long are pap specimens kept in pathology?
|
21 days
|
|
|
|
The presence of intermediate or basal cells on wet mount indicates?
|
inflammation of vaginal epithelium
|
|
|
|
What are the FDA pregnancy categories and their significance?
|

|
|
|
|
What are the recommendations for calcium for women?
|
age 14-18 1300mg/day
age 19-49 1000mg/day age >50 1200mg/day pregnant or lactating 1300mg/day |
|
|
|
List methods of non-hormonal contraception.
|
TRADITIONAL METHODS:
1. abstinence 2. natural family planning 3. coitus interruptus (withdrawal method) BARRIER METHODS: 1. male condom 2. female condom 3. vaginal diaphragm 4. cervical cap 5. spermicides 6. copper IUD STERILIZATION: 1. vasectomy 2. tubal ligation |
|
|
|
COITUS INTERRUPTUS (AKA withdrawal method):
|
withdrawal of penis before ejaculation
disadvantages → requires sufficient male self-control, failure may occur if semen escapes before orgasm or semen deposited on external genitalia near vagina no contraindications no reliable theoretical or actual user effectiveness rates no adverse effects or risks except pregnancy |
|
|
|
MALE CONDOM:
|
contraceptive sheath which covers penis during coitus and prevents deposition of semen in vagina
made from latex, polyurethane or lamb ceca (latex and polyurethane are impervious to organisms causing STIs while lamb ceca is not) advantages → highly effective against pregnancy and STIs, inexpensive indications → prevents pregnancy and STIs, recommend for all non-monogamous couples theoretical user effectiveness rate → 99.7% (failure in 3/1000) failure d/t sheath defect actual user effectiveness rates → 70-90% in 1st year of use (10-30% failure in 1st year of use) failure d/t applying condom late or not withdrawing penis before detumescence |
|
|
|
FEMALE CONDOM:
|

contraceptive sheath which is inserted into vagina with 1 ring near cervix and the other ring outside vagina near introitus and prevents ejaculation of sperm in vagina
made of polyurethane advantages → under control of female partner, some STI protection, perfect use reduces annual risk of HIV by >90% disadvantages → bulky, expensive theoretical user effectiveness rate → 2.6% failure during 1st 6 months, effectiveness comparable to diaphragm and cervical cap |
|
|
|
VAGINAL DIAPHRAGM:
|

contraceptive barrier which is inserted into the vaginal cul-de-sac and covers the cervix
circular ring ranging from 50-105mm in diameter (must be fitted) apply jelly or cream on cervical side before insertion (otherwise ineffective), then apply more jelly on and around diaphragm after insertion may insert 6 hours prior to intercourse leave in place for 6-24 hours following intercourse advantages → some STI protection disadvantages → requires fiiting (and yearly refitting), must anticipate need for contraception, vaginal diameter altered by weight fluctuations or deliveries contraindications → significant pelvic relaxation, shortened vagina, sharply retroverted or anteverted uterus theoretical user effectiveness rate → 94% (6 pregnancies per 100 women per year of exposure) actual user effectiveness rate → 80-85% (15-20 pregnancies per 100 women per year of exposure) failure d/t improper placement or dislodgement, early removal side effects → vaginal wall irritation, increased risk of UTIs |
|
|
|
CERVICAL CAP:
|
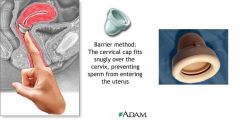
small cuplike diaphragm which is placed over cervix and held in place by suction
must be fitted (though tailoring to fit each individual cervix is difficult) little advantage over diaphragm confirm proper placement following intercourse do not remove for 8-48 hours following intercourse disadvantages → fitting difficult, must be able to feel cervix side effects → foul discharge after 1 day of use theoretical user effectiveness → similar to diaphragm failure d/t dislodgement |
|
|
|
List most to least effective forms of non-hormonal contraception.
|
abstinence
vasectomy tubal ligation male condom vaginal diaphragm coitus interruptus family planning method female condom spermicides cervical cap |
|
|
|
SPERMICIDES:
|
kill sperm and act as mechanical barrier which prevents sperm from entering cervical canal
types include jellies, creams, gels, foam tablets, suppositories, or vaginal sponge (contain nonoxynol 9) disadvantages → foam tablets or suppositories may require few minutes for adequate dispersion, not effective against chlamydia, gonorrhea, or HIV theoretical user effectiveness rate → 15% failure rate if used alone actual user effectiveness rate → 30% failure rate if used alone side effects → external genitalia and vaginal mucosa irritation, frequent use associated with genital lesions (which increases risk of HIV transmission) |
|
|
|
Categorize hormonal contraceptives based on the hormones present.
|
ESTROGEN & PROGESTIN combo:
oral contraceptives injection (Lunelle) patch (Ortho Evra) vaginal ring (Nuvaring) PROGESTIN only: progestin only pill injection (Devo Provera) contraceptive implant (Implanon) IUD (Mirena) |
|
|
|
Define monophasic, biphasic, triphasic, and extended cycle oral contraceptives.
|
MONOPHASIC:
constant dose of estrogen and progestin BIPHASIC: |
|
|
|
ORAL CONTRACEPTIVE PILLS:
|
combination of estrogen (ethinyl estradiol) and progestin (norethindrone, norethindrone acetate, levonorgestrel, desogestrel, norgestimate, or drospirenone)
INDICATIONS: MOA: RELATIVE EFFECTIVENESS: ABSOLUTE CONTRAINDICATIONS: >35y/o smoker pregnant breastfeeding <6 weeks postpartum BP >160/100 thrombogenic mutation (factor V leiden) current or hx of VTE, MI, CVA ↑ risk for CVD (HTN, uncontrolled DM, active SLE) valvular heart disease liver disease migraines with aura breast cancer major surgery with prolonged immobilization RELATIVE CONTRAINDICATIONS: <35y/o + smoker Undiagnosed vaginal bleeding DRUG INTERACTIONS: ADVERSE EFFECTS: breakthrough bleeding, spotting, nausea, HA, weight gain RISKS: VTE (increased if stasis, factor V leiden, leg trauma, pelvic surgery) MI (increased if smoker, dyslipidemia, uncontrolled HTN, or longstanding DM) CVA (increased if age, smoking, HTN, migraine HA with neurologic symptoms) no protection against STIs BENEFITS: ↓ acne ↓ menstrual blood flow (preventing anemia) and dysmenorrhea ↓ risk of benign fibrocystic breast disease (30-50%), menstrual disorders, PID, salpingitis, endometrial (50%), ovarian (40-80%), and colorectal cancer, ectopic pregnancy (90%), RA progression, bone mineral density loss PATIENT EDUCATION: taken for 21 days followed by 7 days of placebo (in which menstruation occurs) COST: |
|
|
|
PROGESTIN-ONLY ORAL CONTRACEPTIVE:
|
progestin only (usually norethindrone or levonorgestrel)
INDICATIONS: unable to take OCP d/t contraindications (>35y/o smoker, breastfeeding, sickle cell anemia, HTN, SLE, migraine HA, mental retardation), estrogen contraindicated MOA: unknown cervical mucus thickens → cervix less permeable to sperm endometrial activity is out-of-phase → prevents implantation even if fertilization occurs does not suppress ovulation RELATIVE EFFECTIVENESS: BENEFITS: ABSOLUTE CONTRAINDICATIONS: RELATIVE CONTRAINDICATIONS: ADVERSE EFFECTS: irregular bleeding DRUG INTERACTIONS: RISKS: PATIENT EDUCATION: take at same time every day (2-3 hours late can reduce effectiveness for 48 hours) COST: |
|
|
|
What are the types of emergency contraception?
|
contraception to prevent unwanted pregnancy if:
1. unprotected intercourse 2. error in contraceptive use 3. sexual assault types include: 1. Preven – estrogen and progesterone combination, delays or inhibits ovulation or disrupts corpus luteum, 100g ethinyl estradiol and 500-600g levonorgestrel, take 1st dose within 3 days, take 2nd dose 12 hours later, side effects include nausea (50%) and vomiting (20%), take meclizine (antiemetic) 1 hour before 1st dose 2. Plan B – progestin only, thickens cervical mucus which inhibits sperm survival and passage through uterus, inhibits GnRH which inhibits FSH/LH secretion which inhibitions ovulation, inhibits implantation, 750g levonorgestrel, take 1st dose within 3-5 days, take 2nd dose 12 hours later (may also take single dose of 1500g), nausea and vomiting less severe than in Preven 3. Copper IUD – no hormone, interferes with sperm function or inhibits implantation, insert within 7 days, effective for 10 years |
|
|
|
Describe ACHES in regards to oral contraceptive use?
|
A → abdominal pain → blood clot in liver or pelvis, gallbladder or benign liver tumor
C → chest pain → angina, MI, PE H → headache → migraine with focal neurologic symptoms, HTN, CVA E → eye problems → vision changes, CVA S → severe leg pain → DVT Contact provider immediately if experience any of these symptoms! |
|
|
|
What is the appropriate history and physical exam for prescribing oral contraceptive pills?
|
MENSTRUAL HISTORY:
age of menarche LMP duration of menses length and regularity of menstrual cycle occurence of spotting and breakthrough bleeding CONTRACEPTIVE HISTORY: type response adverse effects compliance RISK FACTORS: smoking clotting disorder HTN DM migraine HAs MI CVA VTE liver disease cholestasis breast cancer surgery with immobilization within 1 month PHYSICAL EXAM: BP breast exam pelvic exam - abnormal vaginal bleeding PAP smear |
|
|
|
What is the MOA of progestins?
|
thickens cervical mucus → preventing migration of sperm
inhibits GnRH secretion → inhibiting FSH/LH secretion → preventing ovulation thins endometrium → preventing implantation |
|
|
|
DEPO PREVERA:
|
DEPO PREVERA: injection, depot medroxyprogesterone acetate (DMPA) 150mg IM (deltoid or gluteus maximus) every 3 months (effective for 4 months)
BENEFITS: ↓ risk of ectopic pregnancy, endometrial cancer; ↓ sickle cell crisis, seizures; improved symptoms associated with endometriosis; no ↑ risk for arterial or venous disease RISKS: ↓ bone mineral density (encourage adequate calcium intake), irregular bleeding or prolonged menstrual flow during 1st 6 months, amenorrhea after 1st year, +/- weight gain, return to baseline fertility requires 10 months after stopping injections WHEN TO PRESCRIBE: want intermediate or long-term contraception, need to avoid estrogen, not intending to become pregnant in near future, breast feeding >6 weeks postpartum, menstrual bleeding is problem or nuisance, sickle cell disease or seizures, prefers injections, prefers contraceptive use to be unknown to partner |
|
|
|
If patient has secondary amenorrhea + negative pregnancy test, what is the treatment to stimulate withdrawal bleeding?
|
trial of progesterone
medroxyprogesterone acetate10 mg PO daily x 10–13 days per month (or every other month) |
|
|
|
What are risks of UTI in women?
|
young or >65 y/o
sexually active use of diaphragm or spermicide cream |
|
|
|
List sulfonamides used to treat UTIs.
|
sulfamethoxazole
trimethoprim |
|
|
|
Sulfamethoxazole + Trimethoprim (Bactrim): MOA, indications, contraindications, adverse effects, dosing parameters, patient education
|
MOA:
inhibits folate synthesis INDICATIONS: UTIs acute otitis media in children acute exacerbations of chronic bronchitis in adults due to H. flu or S. pneumo prophylaxis and treatment of pneumocystic jiroveci pneumonitis (PCP) traveler's diarrhea due to entertoxigenic E. coli enteritis due to Shigella flexneri or Shigella sonnei CONTRAINDICATIONS: hypersensitivitiy to any sulfa drug infants <2 m/o pregnancy breast feeding megaloblastic anemia due to folate deficiency severe hepatic or renal disease ADVERSE EFFECTS: rash, urticaria nausea, vomiting, anorexia DOSING PARAMETERS FOR UTI: 1 double-strength tablet PO q12 hours x 3-5 days if uncomplicated x 7-10 days if complicated x 14 days if pyelonephritis x 2 weeks if acute prostatitis x 2-3 months if chronic prostatitis PATIENT EDUCATION: take with 8oz of water wear sunscreen and avoid prolonged sun exposure to prevent photosensitivity |
Lexi-Comp p1407
|
|
|
List quinolones used to treat UTIs.
|
ciprofloxacin
norfloxacin |
|
|
|
List cephalosporins used to treat UTIs.
|
cephalexin
|
|
|
|
List penicillins used to treat UTIs.
|
procaine penicillin G
ampicillin amoxicillin + clavulanic acid (Augmentin) |
|
|
|
Ciprofloxacin: MOA, indications, contraindications, adverse effects, dosing parameters, patient education
|
MOA:
inhibits bacterial DNA synthesis and reproduction INDICATIONS: systemic infections CONTRAINDICATIONS: ADVERSE EFFECTS: DOSING PARAMETERS: PATIENT EDUCATION: |
|
|
|
Norfloxacin: MOA, indications, contraindications, adverse effects, dosing parameters, patient education
|
MOA:
inhibits bacterial DNA synthesis and reproduction INDICATIONS: effective against gram-neg and gram pos in treating: uncomplicated UTIs complicated UTIs prostatitis CONTRAINDICATIONS: ADVERSE EFFECTS: DOSING PARAMETERS: PATIENT EDUCATION: |
|
|
|
Leuprolide: MOA, indications, contraindications, adverse effects, dosing parameters, patient education
|
MOA:
agonist of luteinizing hormone-releasing hormone → inhibiting gonadotropin secretion → decreasing testosterone INDICATIONS: palliative treatment of advanced prostate cancer endometriosis anemia caused by uterine fibroids central precocious puberty CONTRAINDICATIONS: hypersensitivity abonormal vaginal bleeding pregnancy breast feeding ADVERSE EFFECTS: altered mood, depression, memory HA, weakness, pain, depression, insomnia, fatigue, dizziness, vertigo skin reaction edema nausea, vomiting, weight change hot flashes, testicular atrophy, hyperlipidemia, decreased libido vaginitis, urinary disorder flu-like syndrome DOSING PARAMETERS: PATIENT EDUCATION: if treating for prostate cancer, initial rise in serum testosterone may cause worsening of symptoms |
|
|
|
When should a 3 day regimen vs a 7 day regimen be used for acute uncomplicated UTI?
|
3 day regimen if:
uncomplicated cystitis 7 day regimen if cystits + diphragm use >65 y/o DM symptoms >7 days recurrent infection |
|
|
|
What is the clinical use of pyridium in acute UTI?
|
symptomatic relief of urinary itching, burning, urgency, or frequency
|
|
|
|
Nitrofurantoin: MOA, indications, contraindications,
adverse effects, dosing, patient education |
MOA:
inhibits several bacterial enzymes → interfering with metabolism and cell wall synthesis INDICATIONS: prevention and treatment of UTI caused by E. coli, klebsiella, enterobacter, S. aureus, enterococcus CONTRAINDICATIONS: hypersensitivity pregnancy at term breastfeeding renal impairment DOSING: 7 day regimen PATIENT EDUCATION: take with food requires monitoring of LFTs if for prophylaxis, take at bedtime |
|
|
|
Discuss the use of nitrofurantoin in the use of UTIs.
|
rarely used due to narrow-spectrum and toxicity
useful against E. coli and gram-pos cocci other organisms may be resistant causes GI upset, acute pneumonitis, neurologic problems |
|
|
|
What are the adverse effects of nitrofurantoin?
|
GI disturbances
acute pneumonitis neurologic problems |
|
|
|
What does HCG stand for?
|
human chorionic gonadotropin
|
|
|
|
What are the indications for ordering an HCG?
|
HCGP → pregnancy confirmation, suspected ectopic pregnancy, suspected miscarriage
BHCG → suspected trophoblastic disease or germ cell tumors of ovaries or testes |
|
|
|
What is an HCG test?
|
tumor marker
measures human chorionic gonadotropin in blood normally undetectable produced by placenta to maintain function of corpeus luteum also produced by some germ cell tumors |
|
|
|
Compare and contrast types of vaginal discharge.
|
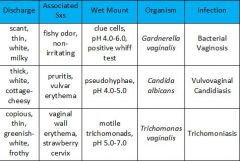
|
|

