![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
102 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is gout?
|
metabolic disorder/arthritis characterized by uric acid crystals in joints, synovium of tendons, and kidneys
|
Orthopedics p292, 510
|
|
|
What is the etiology of gout?
|
excess uric acid → hyperuricemia → formation of crystals:
1. too much uric acid synthesized 2. too little uric acid eliminated by kidneys |
Orthopedics p292, 510
|
|
|
What are the risk factors of gout?
|
men >40y/o
unusual in women until menopause hypertension obesity abnormal kidney function FH of gout purine-rich diet excessive alcohol intake aspirin thiazide diuretics lead poisoning hemolytic anemia, leukemia, other blood disorders |
Orthopedics p292
|
|
|
What is the clinical presentation of gout?
|
rapid onset
pain, inflammation, erythema, edema, warmth of joint monoarticular usually MTP joint of great toe or lower extremity (foot, ankle, knee) sometimes wrist or elbow |
Orthopedics p510
|
|
|
What is the diagnostic work-up of gout?
|
1. aspirate joint → order cell count, crystals, gram, culture (to R/O infectious arthritis)
2. crystals → urate crystals, needle-shaped, negatively birefringent (shine brightly under polarized light) 3. uric acid → hyperuricemia 4. WBC → mild leukocytosis 5. ESR → elevated 6. radiographs intially normal, may progress to bone erosion |
|
|
|
Define tophi.
|
nodules under skin formed by uric acid deposits
|
Orthopedics p510
|
|
|
What are the complications of gout?
|
kidney stones
tophi bone erosion |
Orthopedics p510
|
|
|
What is the treatment for acute gout?
|
1. NSAIDs → ibuprofen, indomethacin (if younger patient)
2. colchicine 3. if NSAIDs not tolerated → prednisone 4. if oral medications cannot be given → intraarticular cortisone injection 5. rest, elevation, moist heat |
Orthopedics p510
|
|
|
What is the prevention for gout?
|
1. decrease seafood, meat, alcohol
2. increase low-fat dairy 3. change gout-inducing medications if necessary 4. prescribe allopurinol or probenecid |
Orthopedics p510
|
|
|
Is gout monoarticular or polyarticular?
|
monoarticular
*unless uncommon presentation |
Orthopedics p510
|
|
|
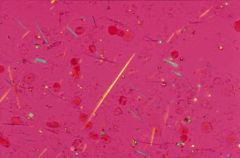
What are the characteristics of urate crystals associated with gout?
|
needle-shaped
negatively birefringent |
Orthopedics p293
|
|

|
gout at MTP joint of great toe
|
|
|
|
needle-shaped negatively birefringent uric acid crystals → gout
|
|
|
|
What is the name for gout affecting the MTP joint of the great toe?
|
podagra
|
|
|
|
What must be R/O in suspected gout?
|
infectious arthritis
cellulitis |
Orthopedics p292
|
|
|
Uric acid may be normal during acute attack of gout, true or false?
|
true
*check uric acid when attack is over |
Orthopedics p293
|
|
|
What is the dosing for colchicine?
|
2 0.5mg tablets initially followed by 1 tablet every hour, up to 12, until symptoms reside or diarrhea ensues
|
Orthopedics p294
|
|
|
What are the cons of colchicine?
|
inconvenient dosing
GI side effects → diarrhea |
Orthopedics p294
|
|
|
How do you determine whether to prescribe allopurinol or probenecid?
|
order uric acid 24-hour urine collection:
>800mg/d indicates overproducer → prescribe allopurinol <800mg/d indicates underexcreter → prescribe probenecid (only if normal renal function, otherwise prescribe allopurinol) |
Orthopedics p294
|
|
|
What is another name for pseudogout?
|
chondrocalcinosis
|
|
|
|
What is pseudogout?
|
arthritis characterized by calcium pyrophosphate dihydrate (salt) crystals in joints
|
|
|
|
What is the etiology of pseudogout?
|
unknown
|
|
|
|
A majority of people with hyperuricemia never develop gout, true or false?
|
true
|
|
|
|
List types of seronegative spondyloarthropathy.
|
ankylosing spondylitis
psoriatic arthritis Reiter's syndrome and other forms of reactive arthritis IBD-associated arthritis |
Orthopedics p164
|
|
|
What are the characteristics of seronegative spondyloarthropathies?
|
1. affect axial skeleton
2. negative for RF |
|
|
|
What is the triad that characterizes Reiter's syndrome?
|
arthritis
conjunctivitis nongonococcal urethritis |
Orthopedics p167
|
|
|
What is the etiology of Reiter's syndrome?
|
unknown
possibly induced by enteric (Salmonella) or sexually transmitted infections (Chlamydia) |
Orthopedics p167
|
|
|
What is Reiter's syndrome?
|
type of seronegative spondyloarthropathy
type of reactive arthritis characterized by triad of arthritis, conjunctivitis, and nongonococcal urethritis |
Orthopedics p167
|
|
|
What is the clinical presentation of Reiter's syndrome?
|
triad of arthritis, conjunctivitis, and nongonoccoal urethritis
usually affects young joints symptoms follow infection 3-4 weeks later lower extremeties affected sacroiliitis heel pain from achilles tendonitis or plantar fasciitis |
Orthopedics p167
|
|
|
What is reactive arthritis?
|
sterile arthritis that develops at a joint as a result of infection distant to the joint
|
Orthopedics p167
|
|
|
What is the management of Rieter's syndrome?
|
1. arthritis is self-limiting and resolves in few months
2. symptomatic treatment → NSAIDs 3. if urethritis → tetracycline x 10-14 days |
Orthopedics p167
|
|
|
What are the indications for arthrocentesis (joint aspiration)?
|
to determine if:
inflammatory vs. non-inflammatory crystal-induced → gout, pseudogout infectious → infectious arthritis diagnosis uncertain |
|
|
|
What are the contraindications forarthrocentesis (joint aspiration)?
|
overlying infection (cellulitis, psoriatic plaque) or bacteremia → may introduce infection into joint
severe coagulopathy or warfarin therapy (INR >3.0) → may cause bleeding |
Current p729
|
|
|
List types of monarticular inflammatory arthritis.
|
gout
pseudogout septic arthritis |
|
|
|
List types of oligoarticular inflammatory arthritis.
|
spondyloarthropathies:
ankylosing spondylitis psoriatic arthritis reactive arthritis → Reiter's syndrome IBD-related arthritis |
|
|
|
What is the most common polyarticular inflammatory arthritis?
|
RA
|
|
|
|
What disorder does a negative ANA rule out?
|
SLE
|
|
|
|
RF and ANA are non-specific tests, true or false?
|
true
|
|
|
|
What is psoriatic arthritis?
|
psoriasis + oligoarticular inflammatory arthritis
|
Orthopedics p167
|
|
|
What is the etiology of psoriatic arthritis?
|
complication of psoriasis
occurs in 5-10% of psoriasis |
Orthopedics p167
|
|
|
What is the clinical presentation of psoriatic arthritis?
|
psoriatic lesions preceding arthritis by few years
arthritis involving axial skeleton (sacroiliitis) and peripheral joints (small joints of hands and feet) oligoarticular sausage finger nail pitting and ridging |
Orthopedics p167
|
|
|
What is the diagnostic workup of psoriatic arthritis?
|
HLA-B27 positive if axial involvement
|
Orthopedics p167
|
|
|
List types of infectious arthropathy.
|
gonococcal arthritis
nongonococcal bacterial (septic) arthritis viral arthritis Lyme disease |
|
|
|
What disorder is "bamboo spine" associated with?
|
ankylosing spondylitis
|
|
|
|
What is the criteria for prescribing allopurinol for prevention of gout?
|
serum uric acid >5mg/dL
24 hour urine uric acid >800mg/dL (overproducer) or <800mg/dL (underexcreter) + impaired renal function |
|
|
|
What is the criteria for prescribing probenecid for prevention of gout?
|
serum uric acid >5mg/dL
24 hour urine uric acid <800mg/d (underexcreter) + normal renal function |
|
|
|
Describe the process of purine metabolism (which leads to uric acid formation).
|
purine → guanosine → guanine→ xanthine → uric acid
xanthine converted to uric acid via xanthine oxidase *allopurinol acts as xanthine oxidase inhibitor |
|
|
|
What is the brand name of allopurinol?
|
zyloprim
|
|
|
|
What 2 types of arthritis affect DIP joints?
|
OA
psoriatic arthritis |
Current p729
|
|
|
What 2 types of arthritis may present with nodules?
|
RA
gout |
Current p729
|
|
|
Should glucose and protein be ordered on synovial fluid?
|
no
|
Current p729
|
|
|
What are the most common causes of bloody synovial fluid?
|
trauma
bleeding disorder iatrogenic → traumatic tap |
Current p729
|
|
|
*What are the synovial fluid results for normal, noninflammatory, inflammatory, purulent, and hemorrhagic disorders?
|

|
|
|
|
What is the viscosity of normal synovial fluid?
|
high
|
|
|
|
Describe the mucin clot test and its interpretation.
|
1. acetic acid added to synovial fluid
2. if normal, non-inflammatory, or hemorrhagic synovial fluid → clot formation 3. if inflammatory or purulent synovial fluid → poor clot formation → cloudy appearance → may indicate RA, gout, septic arthritis, etc. |
|
|
|
What is required for diagnosis of gout, pseudogout, and infectious arthrits?
|
synovial fluid confirmation
|
|
|
|
What are the indications for prescribing medication for the prevention of gout? What are the goals?
|
Indications:
1. frequent attacks 2. tophi 3. kidney stones Goals: 1. reduce uric acid <6mg/dL 2. prevent attacks 3. encourage mobilization of tophi |
Orthopedics p510
|
|
|
Is OA inflammatory or non-inflammatory?
|
non-inflammatory
|
Current p729
|
|
|
What is OA?
|
degenerative non-inflammatory arthritis characterized by degeneration of cartilage and hypertrophy of bone at articular margins
|
Current p730
|
|
|
What is the etiology of osteoarthritis?
|
primary → aging
secondary → trauma, overuse, arthritis, metabolic disease, neurologic disease hereditary and mechanical factors risk increased with obesity, competitive contact sports, frequent bending and carrying |
Current p730
|
|
|
What is the clinical presentation of OA?
|
insidious onset
minimal morning stiffness and inflammation pain with motion, relieved by rest may affect cervical and lumbar spine, carpometacarpal joint of thumb, PIP, DIP, hip, knee, MTP joint of big toe no systemic symptoms crepitus limited ROM heberden or bouchard nodes |
Current p729
|
|
|
What is the diagnostic workup of OA?
|
ESR → normal
radiograph → narrowed joint space, osteophytes, dense subchondral bone, bony cysts |
Current p729
|
|
|
What is the management of OA?
|
1. if mild → acetominophen 2.6-4g/d
2. if no response to acetominophen or severe → NSAIDs 3. corticosteroid injections up to 4x per year 4. capsaicin cream 0.025-0.075% 3-4x daily for knee OA 5. if functional impairment (restricts walking or pain at rest) or refractory to treatment → refer to orthopedic specialist → hip or knee replacement surgery |
Current p731
|
|
|
What is the prevention of OA?
|
1. maintain normal vitamin D levels
2. lose weight → decreases risk of OA in weight-bearing joints |
Current p731
|
|
|
Does recreational running increase the risk of OA?
|
no
|
Current p730
|
|
|
Define Heberden node.
|
bony enlargement of DIP joint; caused by formation of osteophytes; associated with OA
|
Current p730
|
|
|
Define Bouchard node.
|
bony enlargement of PIP joint; caused by formation of osteophytes; associated with OA
|
Current p730
|
|

|
Heberden node of RT index finger
|
|
|
|
What disorder are Heberden and Bouchard nodes associated with?
|
OA
|
|
|
|
What medications may increase risk of hyperuricemia and gout?
|
lose dose aspirin
niacin (vitamin B3) thiazide and loop diuretics allopurinol → if taken within 2 weeks of attack |
Current p734
|
|
|
What is scleroderma?
|
chronic disorder characterized by diffuse fibrosis of the skin and internal organs
|
Current p758
|
|
|
Where does gout most commonly occur on initial presentation?
|
MTP joint of great toe
|
Orthopedics p510
|
|
|
When should patients start allopurinol or probenecid therapy following acute attack of gout?
|
2 weeks following attack
*if started earlier, therapy may prolong attack or cause a new one |
Orthopedics p294
|
|
|
Which of the following are NSAIDs → aspirin, acetaminophen, ibuprofen?
|
aspirin and ibuprofen
*acetaminophen is not an anti-inflammatory, but an analgesic and antipyretic |
|
|
|
When evaluating suspected arthritis, what should you consider?
|
1. inflammatory vs noninflammatory
2. number of joints involved 3. specific joints involved 4. extra-articular manifestations → fever (gout), rash (psoriatic arthritis, SLE), nodules (RA, gout), neuropathy (polyarteritis nodosa) |
Current p729
|
|
|
What tests should be ordered on synovial fluid?
|
cell count
crystals if suspected gout or pseudogout culture if suspected infectious arthritis |
|
|
|
Who is most commonly affected by scleroderma?
|
although the condition is rare, women are 2-3 x more affected than men, presenting in 3rd-5th decade
|
Curren tp758
|
|
|
What is the etiology of lyme disease?
|
caused by bacteria Borrelia burgdorferi
transmitted via tick bite tick carried by mice and deer found in mid-atlantic, NE, north central regions of united states |
Current p1342
|
|
|
What is the clinical manifestation of lyme disease?
|

history of tick bite with tick present >72 hours
stage 1 → after 1 week → target lesion + flu-like symptoms stage 2 → weeks to months later → fatigue, HA, stiff neck, skin lesions, neurologic (meningitis, Bell palsy), cardiac stage 3 → months to years later → arthritis, myalgias *stages overlap and vary |
Current p1342
|
|
|
What is the diagnostic workup of lyme disease?
|
LYME via ELISA for screening
western blot for confirmation *though diagnosis clinical (i.e. exposure in endemic area + target lesion) in early stage since LYME often negative |
Current p1344
|
|
|
What is the management of lyme disease?
|
doxycycline
|
Current p1345
|
|
|
What is the prevention of lyme disease?
|
avoid endemic areas
cover exposed skin use repellants inspect for ticks 200mg doxycycline prophylaxis following tick bite |
Current p1345
|
|
|
What do deer ticks look like?
|
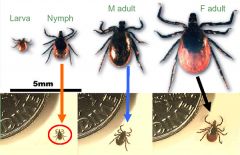
|
|
|

|
target lesion → lyme disease
|
|
|
|
What viruses are most commonly associated with arthritis?
|
parvovirus B19
hepB hepC |
Current p779
|
|
|
What is the etiology of viral arthritis?
|
parvovirus B19
hepB hepC |
Current p779
|
|
|
What is the clinical presentation of viral arthritis?
|
parvovirus B19 → acute polyarthritis in adults (slapped cheek fever in children); mimics RA
hepB → polyarthritis, jaundice, urticaria hepC → chronic polyarthritis, mimics RA |
Current p779
|
|
|
What is the diagnostic workup of viral arthritis?
|
parvovirus B19 → positive IgM antibodies
hepB → positive antigen, elevated serum transaminases hepC → positive antigen, non-erosive radiographs |
Current p779
|
|
|
What is the management of viral arthritis?
|
if parvovirus B19 → self limiting within several weeks
|
Current p779
|
|
|
What is the etiology of gonococcal arthritis?
|
secondary to gonorrhea infection
caused by bacteria neisseria gonorrhea transmitted via sex |
|
|
|
What is the clinical presentation of gonococcal arthritis?
|

initially → migratory polyarthralgias x 1-4 days involving elbow, wrist, knee or ankle
skin lesions → small necrotic pustules over extremities especially palms/soles Pattern 1 → tenosynovitis involving wrists, fingers, ankles or toes (60%) Pattern 2 → purulent monoarthritis involving elbow, wrist, knee or ankle (40%) |
Current p778
|
|
|
Who is most commonly affected by gonococcal arthritis?
|
1. young women → especially during menses or pregnancy
2. homosexual men |
Current p778
|
|
|
What is the diagnostic workup of gonococcal arthritis?
|
CBC
BC synovial fluid: cell count 30,000-60,000 cells/mcL positive gram stain in 25% cases positive culture in <50% cases GC/chlam culture → cervical, urethral, rectal, pharyngeal |
Current p778
|
|
|
What is the management of gonococcal arthritis?
|
1. admit to hospital to confirm diagnosis, exclude endocarditis, and start tx
2. 3rd generation cephalosporin → cefriaxone IV x 1-2 days 3. then cefixime PO x 7-10 days |
Current p778
|
|
|
What is the etiology of nongonococcal (septic) arthrits)?
|
Staph aureus (50%)
MRSA group B strep gram-negatives (10%) → E. coli and pseudomonas aeruginosa associated with: loss of skin integrity → psoriasis, ulcers infection → endocarditis damaged or prosthetic joints → RA immunocompromise → DM, alcoholism, cirrhosis, kidney disease, immunosuppressant therapy) IV drug use |
Current p777
|
|
|
What is the most common cause of septic arthritis?
|
staph aureus
|
Current p777
|
|
|
What is the clinical presentation of septic arthritis?
|
inflammatory monoarticular arthritis
commonly affects knee, hip, wrist, shoulder, or ankle acute pain, swelling, warmth worsens over hours joint effusion |
Current p777
|
|
|
What is the diagnostic workup of septic arthritis?
|
synovial fluid:
cell count >50,000 cells/mcL differentail >90% PMNs gram stain culture BC positive in 50% of cases |
Current p777
|
|
|
What is the management of septic arthritis?
|
1. hospitalization
2. broad-spectrum antibiotics until culture results (vancomycin if suspected MRSA) 3. narrow-spectrum antibiotics x 6 weeks 4. early orthopedic consult for joint drainage |
Current p777
|
|
|
Sausage fingers may indicate?
|
psoriatic arthritis
reactive arthritis |
|
|
|
What are the signs and symptoms of joint inflammation?
|
morning stiffness ≥30min, erythema, swelling, warmth
|
Current p729
|
|
|
What percentage of people >40 y/o display radiographic features of OA in weight-bearing joints?
|
90%
|
Current p730
|

