![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
461 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
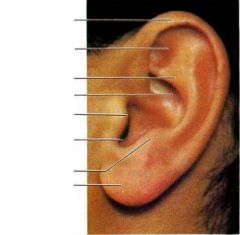
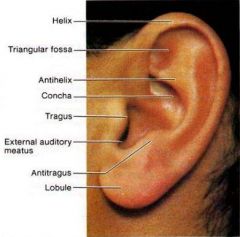
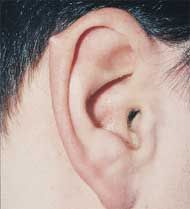
What is the pinna AKA auricle?
|
visible part of the ear
|
|
|
|
|
|
|
|
|
|
|
|
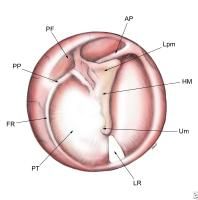
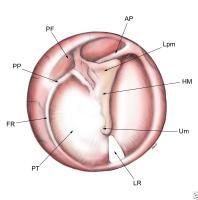
LPM = short/lateral process of malleus
HM = handle of malleus UM = umbo FR = annulus fibrosus PF = pars flaccida PT = pars tensa LR = light reflex |
|
|

|

Lp = short (lateral) process of malleus
Hm = handle of malleus (manubrium) Um = umbo Lpi = long process of incus An = annulus fibrosus At = pars flaccida Lr = light reflex |
|
|
|
Where does cerumen come from?
|
secreted by sebaceous glands in outer third of external auditory canal
|
|
|
|
What is the function of cerumen?
|
lubrication and protection of external auditory canal
|
|
|
|
How do you distinguish the tympanic membrane of the right ear from the TM of the left ear?
|
remember that the short process of the malleus is anterior to the umbo
|
|
|

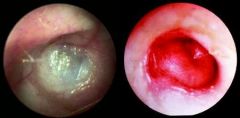
Is this the tympanic membrane of the left ear or right ear?
|
left ear
|
|
|
|
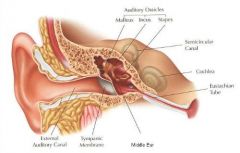
What is the function of the cochlea of the inner ear?
|
hearing
|
|
|
|
What is the function of the vestibule of the inner ear?
|
balance
|
|
|
|
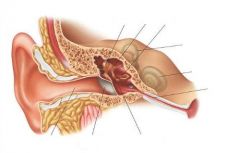
Describe the physiology of hearing.
|
sound waves travel through external ear → causing TM to vibrate → vibrations travel through middle ear causing ossicles to vibrate → causing vibrations to pass into inner ear via oval window → vibrations travel via endolymph of cochlea to round window → vibrations cause hair cells of organ of corti to strike membrane of corti → causing vestibulocochlear nerve to transmit info to temporal lobe
|
Mosbys p319
|
|
|
Describe an ear exam.
|
1. whisper test - icecream, baseball
2. inspect auricle - landmarks, size, shape, symmetry, color, lesions, deformities, discharge 2. palpate auricle (should be firm and mobile) - tenderness, swelling, nodules 3. perform otoscope exam (should be minimal cerumen, uniformly pink) -inspect ear canal for foreign bodies, cerumen, discharge, erythema, swelling, scaling, lesions -inspect TM for landmarks, contour (bulging, retraction), color, perforation |
Mosbys p329
|
|
|
Darwin's tubercle
(normal variant) |
|
|

|
preauricular pit (normal variant)
|
|
|

|
cauliflower ear
|
|
|
|
What is the etiology of cauliflower ear?
|
blunt trauma → necrosis of underlying cartilage
|
Mosbys p329
|
|

|
sebaceous cyst
|
|
|

|
tophi → gout
|
|
|
|
Head trauma + bloody/serous otorrhea may indicate?
|
skull fracture
|
Mosbys p329
|
|
|
What is the ddx for purulent foul-smelling otorrhea?
|
foreign body
otitis |
Mosbys p329
|
|
|
Pain when pulling on lobule of ear may indicate?
|
inflammation of external auditory canal
|
Mosbys p331
|
|
|
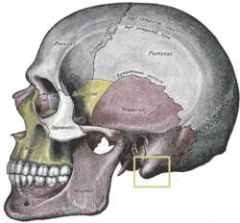
Tenderness and swelling in mastoid area may indicate?
|
mastoiditis
|
Mosbys p331
|
|
|
mastoid process of temporal bone
|
|
|
|
Define otorrhea.
|
ear discharge
|
|
|
|
What are the 2 types of cerumen?
|
wet - dark, sticky
dry - light brown to gray, flaky, sparse |
Mosbys p331
|
|
|
What patient populations are wet and dry cerumen most commonly seen?
|
wet → whites and blacks
dry → asians and native americans |
Mosbys p331
|
|

What type of cerumen is this?
|
dry; seen primarily in Asians and Native Americans
|
|
|
|
What is the management for cerumen impaction?
|
removal via curette or warm water irrigation
|
|
|
|
What are the contraindications for removing cerumen impaction via warm water irrigation?
|
otitis externa
perforated TM myringotomy or tympanotomy tubes mastoid cavity |
Mosbys p332
|
|
|
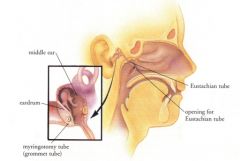
What are myringotomy tubes?
|
ear tubes; incision created in TM to place tubes in order to relieve pressure and drain fluid; treatment for otitis media
|
|
|
|
What is the umbo?
|
end of handle of malleus; center of tympanic membrane
|
|
|
|
Describe a normal tympanic membrane.
|
pearly gray, translucent, slightly convex
|
|
|
|
Bulging tympanic membrane may indicate?
|
increased middle ear pressure or fluid in middle ear
|
|
|

|
exostoses
|
|
|
|
What is another name for serous otitis media?
|
glue ear
|
|
|

|
normal tympanic membrane
|
|
|

|
erythema + retraction → serous otitis media
|
|
|
|
What are 3 broad reasons for abnormal color of tympanic membrane?
|
1. thickening of TM
2. increase in blood vessels of TM 3. fluid in middle ear (blood, pus) |
|
|
|
Define hemotympanum.
|
presence of blood in tympanic cavity of middle ear
|
|
|

|
tympanic membrane perforation
|
|
|

|
tympanosclerosis
|
|
|

|
otitis externa
|
|
|
|
What is tympanosclerosis?
|
deposition of calcium into tympanic membrane due to trauma or infection
|
|
|

|
hemotympanum
|
|
|
|
Describe a bulging tympanic membrane.
|
more convex, loss of bony landmarks, distorted light reflex
|
Mosbys p332
|
|
|
Describe a retracted tympanic membrane.
|

more concave, accentuated bony landmarks, distorted light reflex
|
Mosbys p332
|
|
|
What are tophi of the ear?
|
small white uric acid crystals along peripheral margins of auricle
|
|
|
|
What is the purpose of pneumoscopy?
|
to determine if the tympanic membrane is mobile or not
|
Mosbys p333
|
|
|
What is the ddx if the tympanic membrane does not move upon pneumoscopy?
|
no mobility → TM perforation or myringtomy/tympanotomy tubes present
bulging + no mobility → fluid in middle ear retraction + no mobility → obstruction of eustachian tube w/ or w/out effusion mobility only with negative pressure → obstruction of eustachian tube w/ or w/out effusion *improper pneumoscopy technique may produce misleading results |
Mosbys p333
|
|
|
What is the ddx for excess mobility in small areas of the tympanic membrane upon pneumoscopy?
|
atrophic tympanic membrane
healed perforation |
Mosbys p333
|
|
|
A yellow or amber colored tympanic membrane indicates?
|

serous fluid in middle ear → serous otitis media
|
Mosbys p333
|
|
|
A deep red or blue colored tympanic membrane indicates?
|

blood in middle ear → hemotympanum
|
Mosbys p333
|
|
|
Air bubbles behind the tympanic membrane indicate?
|
serous fluid in middle ear → resolving middle ear effusion
|
Mosbys p333
|
|
|
A white or red colored tympanic membrane indicates?
|
infection in middle ear → acute otitis media
|
Mosbys p333
|
|
|
A dull tympanic membrane indicates?
|
fibrosis
|
Mosbys p333
|
|
|
White flecks or plaques on the tympanic membrane indicate?
|
healed inflammation
|
Mosbys p333
|
|
|
How do you perform the weber test?
|
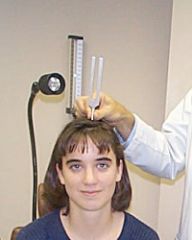
-hold base of tuning fork and tap tines
-place vibrating tuning fork on midline of patient's head -ask patient if sound is heard -ask patient if it is heard equally in both ears or better in one ear -sound should be heard equally in both ears -if conductive hearing loss, sound will lateralize to affected ear -if sensorineural hearing loss, sound will lateralize to non-affected ear |
|
|
|
How do you perform the rinne test?
|

1. hold base of tuning fork and tap tines
2. place vibrating tuning fork on mastoid bone 3. ask patient if sound is heard 4. ask patient to tell you when it stops 5. when it stops, move vibrating tuning fork in front of ear 6. ask patient if sound is heard 7. if no, stop test 8. if yes, ask patient to tell you when it stops 9. normally air conduction is heard longer than bone conduction (2:1 ratio) -conductive hearing loss if BC heard longer than AC -sensorineural hearing loss if AC heard longer than BC but air <2:1 ratio |
|
|
|
What tuning fork is used to perform the weber test and rinne test?
|
512hz
|
|
|
|
What is the ddx for clear, watery otorrhea?
|
CSF leakage
|
|
|
|
What is the ddx for bloody otorrhea?
|
trauma
chronic bacterial otitis externa |
|
|

|
small white or black conidiophores on white hyphae → Aspergillus (fungal) associated otitis externa
|
|
|
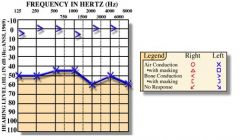
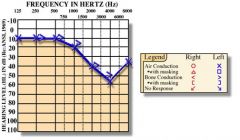
Explain the results of this audiogram.
|
normal bone conduction + diminished air conduction → conductive hearing loss in left ear
|
|
|
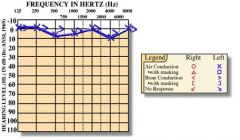
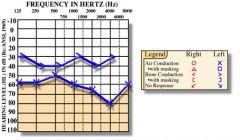
Explain the results of this audiogram.
|
normal hearing
|
|
|
Explain the results of this audiogram.
|
equally diminished air conduction and bone conduction → sensorineural hearing loss in left ear
|
|
|
Explain the results of this audiogram.
|
diminished bone conduction + even more diminished air conduction → mixed hearing loss in left ear
|
|
|
|
What is conductive hearing loss?
|
dysfunction of external ear, middle ear, or tympanic membrane; impairing passage of sound vibrations to inner ear
|
|
|
|
What is the etiology of conductive hearing loss?
|
1. obstruction → foreign body, cerumen impaction, exostosis
2. inflammation/infection → otitis externa, otitis media, serous otitis media, mastoiditis 3. stiffness → otosclerosis 4. discontinuity → ossicular disruption |
|
|
|
What is the most common cause of conductive hearing loss?
|
cerumen impaction
|
|
|
|
What is sensorineural hearing loss?
|
dysfunction of inner ear (most often caused by cochlea deterioration due to loss of hair cells in organ of corti), vestibulocochlear nerve, or auditory parts of brain; impairing passage of nerve impulses to brain
|
|
|
|
What is the ddx for sensorineural hearing loss?
|
presbyacusis
noise trauma head trauma infection tumor vascular ischemia ototoxic drugs meniere's disease |
|
|
|
What is otosclerosis?
|
abnormal bone growth in middle ear; may cause conductive hearing loss
|
|
|
|
What is exostosis commonly known as?
|
surfer's ear
|
|
|
|
What patient population is most affected by exostosis?
|
surfers
|
|
|
|
What is presbyacusis?
|
age-related sensorineural hearing loss
|
|
|
|
List 6 disorders of the external auditory canal.
|
1. foreign body
2. cerumen impaction 3. pruritus 4. otitis externa 5. malignant otitis externa 6. exostoses |
|
|
|
List 8 disorders of the middle ear.
|
1. perforated tympanic membrane
2. hemotympanum 3. acute otitis media 4. chronic otitis media 5. serous otitis media 6. cholesteatoma 7. otosclerosis 8. mastoiditis |
|
|
|
What physical exam should you do for a hearing complaint?
|
1. whisper test
2. weber test 3. rinne test 4. inspect auricle and neck 5. palpate auricle and neck 6. otoscopy - inspect external auditory canal and tympanic membrane |
|
|
|
When should you order audiometry evaluation?
|
when hearing loss not easily remedied
*cerumen impaction and otitis media easily remedied |
|
|
|
Define otalgia.
|
ear pain
|
|
|
|
Define tinnitus.
|
ringing in ears
|
|
|
|
Define vertigo.
|
imaginary sense of motion (spinning, tilting, falling) while still or exagerrated sense of motion while moving
|
|
|
|
What is the common name for otitis externa?
|
swimmer's ear
|
|
|
|
What is otitis externa?
|
infection of external auditory canal
|
|
|
|
What is the etiology of otitis externa?
|
when trauma or moist environment favors bacterial or fungal growth
|
|
|
|
Define dizziness.
|
lightheadedness or faintness
|
|
|
|
What is a common cause of referred otalgia?
|
TMJ dysfunction
|
|
|
|
What are the characteristics of presbyacusis?
|
age-related sensorineural hearing loss (predominantly high frequency), manifests as reduced ability to perceive or discriminate sounds (people sound like they are mumbling), bilateral, progressive
|
Current p186
|
|
|
What is the epidemiology of presbyacusis?
|
present in 25% of 65-75y/o
present in 50% of >75y/o |
|
|
|
What is the management for presbyacusis?
|
1. hearing aids
2. telephone amplifiers 3. advise family and friends on measures to improve communication - minimize background noise, face person, talk clearly |
|
|
|
Sounds of what decibel are potentially injurious?
|
>85 dB
|
Current p186
|
|
|
What is etiology of noise trauma?
|
industrial machinery, discharged weapons, loud music
|
|
|
|
What is the patient education for noise trauma?
|
1. wear earplugs when exposed to moderately loud noises
2. wear specially designed ear muffs when exposed to explosive noises |
Current p187
|
|
|
What types of head trauma may cause hearing loss?
|
concussion
skull fracture air bag deployment |
Current p187
|
|
|
List ototoxic drugs.
|
1. salicylates → aspirin at high doses (>12 325mg tablets daily)
2. antibiotics → aminoglycosides (neomycin, gentamicin, streptomycin, tobramycin, kenamycin), vancomycin 3. antimalarials → quinine 4. loop diuretics → furosemide, ethacrynic acid 5. chemotherapeutic drugs containing platinum → cisplatin, carboplatin 6. ear drops → neomycin, gentamicin |
http://tiny.cc/ototoxicdrugs
|
|
|
In what patient populations are ototoxic drugs contraindicated?
|
pregnancy
elderly pre-existing hearing loss renal insufficiency ototoxic ears drops + tympanic membrane perforation |
Current p187
|
|
|
What measures should be taken to reduce risk of ototoxicity when prescribing ototoxic drugs?
|
1. before treatment, evaluate hearing
2. during treatment, prescribe lowest effective dose, monitor drugs levels (serum peak and trough), and monitor hearing (serial audiometry) |
Current p187
|
|
|
It is possible for topical agents that enter middle ear to be absorbed into inner ear via round window, true or false?
|
true
*avoid prescribing ototoxic ear drops if tympanic membrane perforated |
Current p187
|
|
|
What are the 2 most common causes of sensorineural hearing loss?
|
1. presbyacusis
2. noise trauma |
|
|
|
What is the treatment for sudden sensorineural hearing loss?
|
1. order audiometry immediately
2. prescribe corticosteroids to prevent permanent hearing loss (prednisone 80mg PO daily, tapered over 10 days) *hearing loss may be permanent if not treated within 6 weeks |
Current 187
|
|
|
Vertigo is often accompanied by what sign?
|
nystagmus
|
|
|
|
What is the cardinal symptom of vestibular disease?
|
vertigo
|
Current p188
|
|
|
Describe the characteristics of vestibular dysfunction originating in ear.
|
sudden onset vertigo, nausea, vomting, tinnitus, hearing loss, horizontal nystagmus
|
Current p188
|
|
|
Define nystagmus.
|
involuntary eye movements
|
Stedmans
|
|
|
What is the dix-hallpike test?
|
diagnostic maneuver used to identify benign paroxysmal positional vertigo (BPPV)
|
|
|
|
Describe the characteristics of vestibular dysfunction originating in CNS.
|
gradual onset vertigo, +/- vertical nystagmus without delay and not inhibited by visual fixation
|
|
|
|
What is the ddx for vertigo?
|
1. peripheral vestibulopathy - acute vertigo
-benign paroxysmal positioning vertigo - minutes -labrynthitis - days to week -meniere's disease 2. central vestibulopathy - gradual vertigo 3. systemic disorders 4. drugs → alcohol, analgesics, hypnotics, tranquilizers, antibiotics, anticonvulsants |
Current p189
|
|
|
What is electronystagmography (ENG)?
|
group of eye movement tests that measure nystagmus if suspected vestibular or neurological disorder
|
|
|
|
What is labyrinthitis?
|
inflammation of the inner ear
|
|
|
|
What is the etiology of labryinthitis?
|
ear infection
upper respiratory tract infection allergy cholesteatoma ototoxic drugs |
Current p189
|
|
|
What are the characteristics of labyrinthitis?
|
severe vertigo that continuously lasts for days to weeks, nausea, vomiting, tinnitus, unilateral hearing loss
|
Current p189
|
|
|
What are the complications of labrynthitis?
|
permanent hearing loss (rare)
spread of inflammation (rare) |
Current p189
|
|
|
What is the treatment for labyrinthitis?
|
1. antibiotics if associated with fever or symptoms of bacterial infection
2. supportive care -antihistamines -relief for nausea, vomiting, dizziness - diazepam, meclizine |
|
|
|
What is the patient education for vertigo-related disorders?
|
1. when symptoms occur, remain still and rest, do not read
2. avoid bright lights 3. avoid sudden position changes 4. avoid hazardous activities like driving or operating machinery until 1 week after symptoms have cleared 5. resume activity gradually |
|
|
|
What are the indications for prescribing meclizine?
|
nausea, vomiting, and dizziness related to motion sickness
|
|
|
|
What is the trade name for diazepam?
|
valium
|
|
|
|
Describe the characteristics of benign paroxysmal positioning vertigo.
|
vertigo associated with changes in head position, 10-15sec delayed onset, 10-60sec duration, recurrent over days, positive dix-hallpike test
|
Current p189
|
|
|
What is the treatment for benign paroxysmal positioning vertigo?
|
epley maneuver
|
Current p189
|
|
|
What is the procedure for the dix-hallpike test?
|
1. patient sits upright with legs extended
2. turn patients head 45 degrees 3. help patient lay down quickly with head extended 20 degrees (i.e. head hanging off end of table) 4. observe eyes for nystagmus 5. have patient sit up and observe eyes for nystagmus reversal |
|
|
|
What are the indications for a positive dix-hallpike test?
|
Nystagmus characterized by:
1. 10-15sec delayed onset 2. rotational 3. fatiguable (repetition of test will result in less nystagmus) 4. reversal (direction of nystagmus reverses upon sitting up) |
|
|
|
What is the etiology of Meniere's disease?
|
idiopathic, but related to distension of endolymphatic compartment of inner ear
|
Current p189
|
|
|
What are the characteristics of Meniere's disease?
|
episodic vertigo, 20 minutes to several hours in duration, fluctuating low-frequency sensorineural hearing loss, tinnitus (low-tone, blowing), aural fullness, symptoms wax and wane
|
Current p189
|
|
|
What is the management for Meniere's disease?
|
1. low salt diet (1-2 grams per day)
2. diuretic (acetazolamide) 3. avoid caffeine, alcohol, tobacco |
Current p189
|
|
|
Describe the steps of the ear exam.
|
1. ask about use of hearing devices
2. inspect auricle and mastoid 3. palpate auricle 4. pull helix and lobule 5. switch ears 6. perform gross whisper test 7. perform otoscopy (use finger strut) → external auditory canal, tympanic membrane, bony landmarks 8. perform insufflation |
|
|
|
What is the eustachian tube?
|
cartilaginous and bony passageway between middle ear and nasopharnyx
|
|
|
|
What are the functions of the eustachian tube?
|
1. equalize middle ear pressure with atmospheric pressure, allowing TM to vibrate freely
2. clear small amount of mucus produced by middle ear |
|
|
|
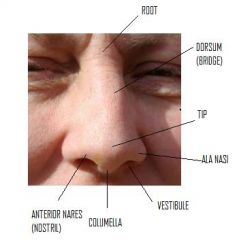
What are the functions of the nose and nasopharynx?
|
1. smell
2. air passage 3. warmth, humidification, and filtration of inspired air 4. resonance of laryngeal sound |
Mosbys p319
|
|
|
|
|
|
|
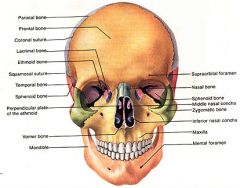
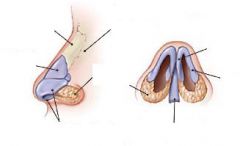
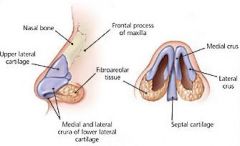
What bones form the nasal bridge?
|
frontal bone, nasal bone, and frontal process of maxillary bone
|
|
|
|
What forms the floor of the nose?
|
hard and soft palate
|
|
|
|
Where are the adenoids (pharyngeal tonsils) located?
|
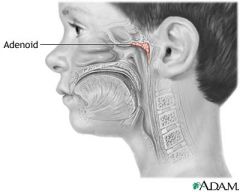
posterior wall of nasopharnyx
|
|
|
|
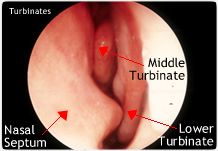
What is the function of the superior, middle, and inferior turbinates?
|
warm, humidify, and filter inspired air
|
Mosbys p321
|
|
|
Describe the nose exam.
|
1. inspect nose - landmarks, size, shape, color, flaring/narrowing, discharge (unilateral, bilateral, amount, color, watery, mucoid, purulent, bloody, crusting)
2. palpate nose - tenderness, masses, displaced cartilage/bone 3. assess patency of nares 4. perform nasoscopy -keep head level to view inferior turbinate -tilt head back to view middle turbinate -angle speculum toward midline to view septum -inspect nasal mucosa (should be deep pink, glistening) - color, swelling, lesions, masses, discharge -inspect nasal septum (should be midline, straight, thicker anteriorly) - alignment, perforation, bleeding, crusting |
Mosbys p334
|
|
|
Bilateral watery rhinorrhea + nasal congestion + sneezing is indicative of?
|
allergic rhinitis
|
Mosbys p335
|
|
|
Define rhinorrhea.
|
nasal discharge
|
|
|
|
Unilateral watery rhinorrhea + head trauma is indicative of?
|
CSF → cribiform plate fracture
|
Mosbys p335
|
|
|
What are the characteristics of rhinorrhea in presence of foreign body?
|
unilateral, thick, greenish, purulent, malodorous
|
Mosbys p335
|
|
|
What is the ddx for mucoid rhinorrhea?
|
rhinitis
|
Mosbys p335
|
|
|
What is the ddx for purulent rhinorrhea?
|
1. if unilateral → foreign body
2. if bilateral → upper respiratory tract infection |
Mosbys p335
|
|
|
Nasal flaring is indicative of?
|
respiratory distress
|
Mosbys p335
|
|
|
Which turbinates are visible upon nasoscopy examination?
|
middle and inferior
|
|
|
|
What are the characteristics of turbinates indicative of allergies?
|
pale pink or bluish gray, swollen boggy constistency
|
Mosbys p335
|
|

|

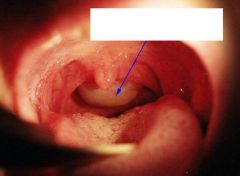
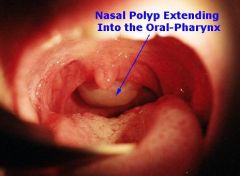
nasal polyp → allergic rhinitis or chronic nasal obstruction
|
|
|
|
What are the characteristics of a nasal polyp?
|

pale, gelatenous, edematous, mucosally-covered masses
|
Mosbys p335
|
|

|
|
|
|

|

allergic salute → transverse nasal crease → chronic allergic rhinitis
|
|
|
|
|
|
|
|
What are the physical exam findings for sinusitis?
|
1. dull or opaque sinus transillumination
2. purulent, colored rhinorrhea 3. maxillary toothache 4. poor response to decongestants |
Mosbys p355
|
|
|
What are signs of chronic cocaine insufflation?
|
1. scabs on nasal mucosa
2. perforation of nasal septa where chronic irritation results in ischemic necrosis of septal cartilage 3. ↓ smell and taste |
Mosbys p355
|
|
|
Define hyperemia.
|
increased blood flow to an area
|
|
|
|
What are signs of recent cocaine insufflation?
|
1. rhinorrhea
2. hyperemia and edema of nasal mucosa 3. white powder residue |
Mosbys p355
|
|
|
What are common symptoms of cocaine insufflation?
|
nasal congestion, rhinorrhea, recurrent epistaxis, sinus problems
|
Mosbys p355
|
|
|
Pain on palpation or percussion of the frontal or maxillary sinus indicates?
|
sinusitis
|
|
|
|
How do you perform transillumination of the maxillary sinus?
|
1. dim lights
2. place lighted otoscope on infraorbital rim 3. ask patient to open mouth 4. look for light in mouth 5. if transillumination → normal sinus 6. if no transillumination → sinusitus |
|
|

|

transillumination → normal maxillary sinus
|
|
|
|
What is septal deviation?
|
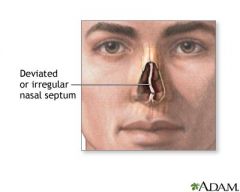
displacement of nasal septum
|
|
|
|
What is ddx for septal deviation?
|
congenital
trauma |
|
|

|

deviated septum
|
|
|
|
What is the most frequently fractured bone in the body?
|
nasal bone
|
|
|
|
What are the physical exam findings of nasal bone fracture?
|
pain, soft tissue hematoma (black eye), epistaxis, crepitance, palpable mobile bony segments
|
Current p199
|
|
|
What is important to R/O with nasal fracture?
|
1. septal hematoma
2. additional fractures/trauma |
Current p199
|
|
|
What is closed reduction?
|
restoration of dislocation or fracture to correct alignment without surgical exposure of the fragments
|
|
|
|
What is the treatment for nasal bone fracture?
|
1. if marked nasal swelling, wait 3-5 days to perform reduction
2. prescribe pain medication 3. counsel patient to rest, maintain head elevation, apply ice, and return within 3-5 days for reduction 4. perform closed reduction using topical 4% cocaine and locally injected 1% lidocaine 2. refer to otorhinolaryngologist 3-5 days following reduction |
Current p199
http://tiny.cc/aafp-nasalfracture |
|
|
What is a septal hematoma?
|
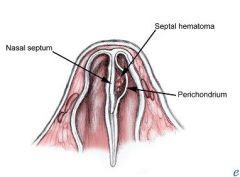
blood filled cavity between septum and perichondrium
|
|
|
|
What are the complications of an untreated septal hematoma?
|
loss of nasal cartilage → saddle nose deformity
|
Current p199
|
|
|
What organism commonly causes infection of a septal hematoma?
|
S. aureus
|
Current 199
|
|
|
|
|
|

|

nasal bone fracture
|
|
|
|
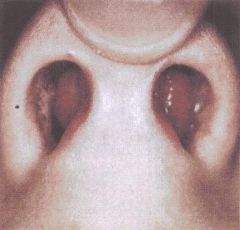
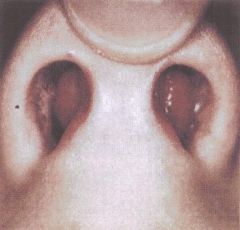
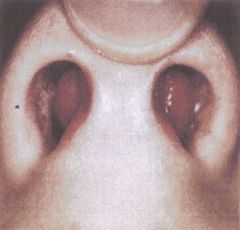
bilateral septal hematoma
|
|
|
|
Which is more common, anterior or posterior epistaxis?
|
anterior
|
|
|
|
Define epistaxis.
|
nosebleed
|
|
|
|
What are the signs of anterior epistaxis?
|
nosebleed
|
|
|
|
What are possible signs of posterior epistaxis?
|
asymptomatic, nausea, hemoptysis, hematemesis, melena, anemia, or sudden massive nosebleed
|
|
|
|
Define epistaxis digitorum.
|
nose picking
|
|
|
|
What is the ddx for epistaxis?
|
Local:
foreign body epistaxis digitorum forceful nose blowing trauma septal deviation septal perforation rhinitis chronic sinusitus nasal polyps intranasal neoplasm vascular malformation medications - topical corticosteroid alcohol cocaine or other drug use low humidity → drying of nasal mucosa environmental irritants Systemic: HTN (think posterior epistaxis) athersclerotic disease (think posterior epistaxis) liver disease hemophilia thrombocytopenia platelet dysfunction leukemia medications - NSAIDs, aspirin, anticoagulants |
http://tiny.cc/aafp-epistaxis
|
|
|
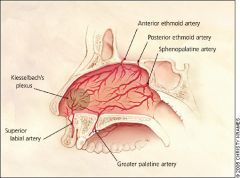
What 5 arteries supply the nasal septum?
|
superior labial a.
greater palatine a. anterior ethmoid a. posterior ethmoid a. sphenopalatine a. |
http://tiny.cc/aafp-epistaxis
|
|
|
If nasal polyps are unilateral, what do you need to R/O?
|
cancer
|
|
|
|
|
|
|

|

foreign body (plastic toy wheel)
|
|
|
|
What is Kiesselbach's plexus?
|
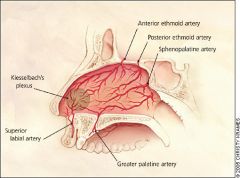
region in anterior septum where superior labial, anterior ethmoid, sphenopalatine, and greater palatine arteries anastomose to form a vascular plexus
|
|
|

|
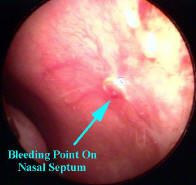
anterior epistaxis
|
|
|

|

Kiesselbach's plexus → normal nasal septum
|
|
|
|
What is the management of epistaxis?
|

1. perform Trotter's method
-manually compress nostrils for 5-20 minutes -sit upright to reduce BP -tilt head forward to prevent blood from pooling in posterior pharnyx, avoiding nausea and airway obstruction 2. during manual compression, assess airway and blood loss 3. if bleeding stops, discharge 4. if bleeding continues, locate source 5. apply anaesthetic + vasoconstrictor via spray or swab -leave for 10 minutes 6. locate source 6. perform chemical or electrocautery -if chemical cautery, apply silver nitrate stick to source in decreasing concentric circles |
http://tiny.cc/bmj-epistaxis
http://tiny.cc/aafp-epistaxis |
|

|

robin egg blue necrosis → narcotic abuse
|
|
|

|

perforated septum
|
|
|
|
What is the ddx for nasal septum perforation?
|
nasal trauma/surgery
autoimmune disease topical nasal decogestants chronic nasal steroids cocaine |
|
|
|
Why is a septal hematoma concerning?
|
septal cartilage has no blood supply, but receives all its nutrients from the perichondrium; if untreated, the septal cartilage can die within 24 hours and result in a saddle nose deformity
|
|
|

|

mild saddle nose deformity due to septal hematoma
|
|
|

|

Trotter's method → manual compression of nasal septum for epistaxis
|
|
|
|
What is a neti pot?
|

device used for irrigating the nasal passages
|
|
|
|
What are the indications for use of a neti pot?
|
allergies
common cold minor sinus infections |
|
|
|
How do you use a neti pot?
|

1. make saline solution (16 ounces water, 1 tsp salt)
2. fill neti pot 3. tilt head at 45 degree angle over sink 4. place spout in top nostril and pour 5. repeat for other nostril 6. use daily when symptomatic and 3x per week when asymptomatic 7. side effects may include nasal irritation or rarely epistaxis 8. combat side effects by adjusting water temperature, reducing salt, or reducing frequency |
http://tiny.cc/webmd-netipot
|
|
|
What is Samter's triad (AKA triad asthma)?
|
condition consisting of asthma, nasal polyposis, and aspirin sensitivity where aspirin may cause severe bronchospasm
|
|
|
|
What are the effects of aspirin on a patient with asthma and nasal polyposis?
|
aspirin (and other NSAIDS) may induce severe brochospasm (asthma attack), anaphylaxis, and uticaria
*other NSAIDS includes ibuprofen but not acetominophen |
|
|
|
What is the management for Samter's triad?
|
1. avoid aspirin and other NSAIDS, replace with acetominophen
2. if aspirin necessary, undergo aspirin desensitization 3. indications for desensitization include significant corticosteroid side effects, refractory to treatment, severe polyposis, CHD, RA, OA |
http://tiny.cc/wao-samterstriad
|
|
|
What is the etiology of septal hematoma?
|
trauma - soft tissue injury or nasal fracture
|
|
|
|
What is the management of a septal hematoma?
|
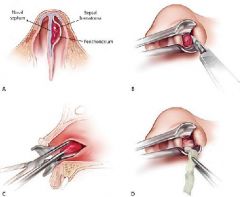
1. anesthesia, incision using hemostat, drainage, insertion of gauze packing
2. send for culture 3. prescribe antibiotics for S. aureus |
http://tiny.cc/aafp-nasalfracture
|
|
|
What are the physical exam findings of a septal hematoma?
|
nasal congestion
widening of anterior septum |
|
|
|
What is hay fever?
|
allergic rhinitis due to outdoor triggers like pollen
|
|
|
|
What is allergic rhinitis?
|
inflammation of the nasal passages due to allergens
|
|
|
|
What is the etiology of allergic rhinitis?
|
sensitivity + allergen (dust, pet dander, mites, mold, pollen, ragweed, air pollution, and other inhaled allergens) → antibody production → antibodies bind to mast cells → mast cells release histamine → inflammation, rash, mucous production, pruritus
|
|
|
|
What is the clinical presentation of allergic rhinitis?
|
1. eyes - pruritus, red, watery
2. nose - sneezing, pruritus, nasal congestion, clear watery rhinorrhea 3. throat - pruritus, postnasal drip, cough, sore throat |
|
|
|
What is the diagnostic workup for allergic rhinitis?
|
If symptoms are extemely bothersome, determine offending allergen with either:
1. serum RAST → allergen specific IgE antibody 2. skin testing |
Current p197
|
|
|
What is the management of allergic rhinitis?
|
1. antihistamines
2. intranasal corticosteroids 3. irrigate nasal passages with neti pot 4. avoid/reduce allergen exposure |
|
|
|
90% of epistaxis cases originate at what site?
|
Kiesselbach's plexus
|
|
|
|
What are 3 broad categories of rhinitis?
|
1. vasomotor rhinitis
2. allergic rhinitis - seasonal, perennial 3. infective rhinitis |
|
|
|
What is hereditary hemorrhagic telangiectasia (HHT)?
|
genetic disorder characterized by abnormal blood vessel formation
|
|
|
|
What are the diagnostic criteria for hereditary hemorrhagic telangiectasia?
|
1. spontaneous recurrent epistaxis
2. multiple telangiectasias 3. arteriovenous malformations 4. first-degree family member with HHT *possible HHT if 2 of the above, while definite HHT if 3 of the above |
|
|
|
What is the patient education for epistaxis?
|
1. lubricate septum with petroleum jelly to prevent drying
2. use a humidifier at night to prevent drying 3. avoid nose rubbing, blowing, and picking 4. avoid hot/spicy food and tobacoo to prevent nasal vasodilation 5. avoid straining and vigorous exercise |
Current p199
http://www.aafp.org/afp/2005/0115/p312.html |
|
|
What percentage of Americans are affected by allergic rhinitis?
|
14-40%
|
Current p196
|
|
|
What is the etiolgy of vasomotor rhinitis?
|
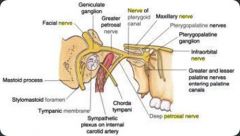
increased sensitivity of the vidian nerve (AKA nerve of pterygoid canal)
|
|
|
|
Define xerostomia.
|
dry mouth
|
|
|
|
When should you prescribe nasal spray antihistamines for allergic rhinitis?
|
when patients complain of side effects (sedation, xerostomia) with oral antihistamines
|
Current p196
|
|
|
List high-sedating (1st generation) antihistamines.
|
diphenhydramine (Benadryl)
hydroxyzine (Allegra) chlorpheneramine (Chlor-Trimetron) |
|
|
|
List low-sedating (2nd generation) antihistamines, whether Rx or OTC, and dosing?
|
cetirizine (Zyrtec) → OTC, 10mg PO daily
loratadine (Claritin) → OTC, 10mg PO daily desloratadine (Clarinex) → Rx, 5mg PO daily fexofenadine (Allegra) → Rx, 60mg PO 2x daily or 120mg PO daily |
Current p196
|
|
|
Which are more effective for treatment of allergic rhinitis, non-sedating antihistamines or intranasal corticosteroids?
|
intranasal corticosteroids
|
Current p196
|
|
|
What is the patient education for use of intranasal corticosteroids for allergic rhinitis?
|
1. ≥ 2 week delay in onset of relief
2. tilt head forward, hold bottle straight up, spray toward ipsilateral ear to deliver to middle meatus 3. side effects include epistaxis possibly due to incorrect delivery |
Current p197
|
|
|
What are indications for prescribing intranasal corticosteroids for allergic rhinitis?
|
recurrent acute bacterial rhinosinusitis
chronic rhinosinusitus |
Current p196
|
|
|
What is nasal vestibulitis?
|
bacterial infection of nasal vestibule
|
Current p195
|
|
|
What is the etiology of nasal vestibulitis?
|
nasal manipulation (excessive nose blowing, nose picking, hair trimming) → S. aureus folliculitis
|
Current p195
|
|
|
What are the complications of nasal vestibulitis?
|
furuncles
cellulitis cavernous sinus thrombosis |
http://tiny.cc/merck-nasalvestibulitis
|
|
|
What is the clinical presentation of nasal vestibulitis?
|
nasal vestibule inflammation
crusting bleeding when crusts slough |
|
|
|
What is the management of nasal vestibulitis?
|
1. prescribe systemic antibiotic for S. aureus → dicloxacillin 250mg PO 4x daily x 7-10 days
2. apply topical bacitracin or mupirocin 2-3x daily 3. if recurrent, prescribe rifampin 10mg/kg PO 2x daily for last 4 days of treatment |
Current p195
|
|

|
unilateral nasal vestibulitis
|
|
|
|
Nasal polyps in children might indicate?
|
cystic fibrosis
|
Current p199
|
|
|
What is the etiology of nasal polyps?
|
allergic rhinitis
chronic nasal obstruction |
|
|
|
What is the management for nasal polyps?
|
1. if small → topical nasal corticosteroids x 1-3 months
2. oral corticosteroids → prednisone, prescribe 21-5mg tablets, take 30mg on day 1, taper 5mg each day for 6 days 3. if large or refractory → surgical removal 4. continue intranasal corticosteroids following removal to prevent recurrence 5. determine offending allergen to prevent recurrence |
Current p199
|
|
|
What organism causes nasal vestibulitis?
|
S. aureus
|
|
|
|
What is a upper respiratory tract infection (URTI)?
|
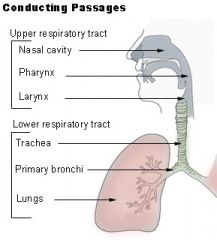
acute infection involving the upper respiratory tract: sinuses, nose, larynx, pharnyx
|
|
|
|
What are examples of URTIs?
|
common cold (viral rhinitis), influenza, sinusitus, tonsillitis, pharyngitis, laryngitis, epiglottitis
|
|
|
|
What is viral rhinitis?
|
common cold
|
Current p192
|
|
|
What is the etiology of viral rhinitis?
|
rhinoviruses (30-50%)
coronaviruses (10-15%) influenza human parainfluenza viruses human respiratory syncytial virus adenoviruses enteroviruses metapneumovirus |
|
|
|
What is the presentation of viral rhinitis?
|
malaise, headache, hyposmia, sneezing, nasal congestion, WATERY rhinorrhea, throat discomfort, cough, erythematous edematous nasal mucosa
|
Current p192
|
|
|
What is the management for viral rhinitis?
|
supportive measures:
1. rest 2. fluids 3. decongestants → pseudoepedrine 30-60mg every 4-6 hours or 120mg 2x daily |
Current p192
|
|
|
What is the patient education for viral rhinitis?
|
antibiotics are not helpful!!!
|
|
|
|
What are the complications of viral rhinitis?
|
eustachian tube dysfunction
transient middle ear effusion 2° bacterial rhinosinusitis |
Current p192
|
|
|
What are the indications that viral rhinitis has been complicated by bacterial rhinosinusitis?
|
persistence of symptoms beyond 1 week + unilateral facial or tooth pain + purulent yellow/green rhinorrhea
|
Current p192
|
|
|
Define hyposmia.
|
↓ sense of smell
|
|
|
|
How many viruses cause the common cold?
|
>200
|
|
|
|
What is the prevention for viral rhinitis?
|
1. support immune system → get enough sleep, drink water, avoid secondhand smoke, avoid unecessary antibiotics
2. avoid germs → sanitize/wash hands, disinfect surfaces |
|
|
|
What is rhinitis medicamentosa?
|
rebound nasal congestion caused by extended use of topical decogestants
|
|
|
|
What is the management of rhinitis medicamentosa?
|
1. cessation of topical decongestants
2. supportive care during withdrawal with topical intranasal corticosteroids or oral prednisone |
|
|
|
What is the etiology of acute bacterial rhinosinusitis (sinusitis)?
|
impaired mucociliary clearance → obstruction of sinus pore → accumulation of mucus in sinus cavity → 2° bacterial infection (S. pneumoniae, H. influenzae, S. aureus, M. catarrhalis)
|
Current p193
|
|
|
What is the presentation of acute bacterial rhinosinusitis?
|
persistence of symptoms >10 days or worsening symptoms within 10 days after initial improvement, facial pain over sinus, purulent yellow/green rhinorrhea, malaise, fever, headache, hyposmia, halitosis, cough
|
Current p193
|
|
|
What is the most commonly affected sinus in acute bacterial rhinosinusitis?
|
maxillary
|
Current p193
|
|
|
What is the treatment for acute bacterial rhinosinusitis?
|
1. NSAIDs
2. nasal decongestants → oxymetazoline 0.05% or xylometazoline 0.05-0.1% 1-2 sprays in each nostril every 6-8 hours for ≤3 days 2. oral decongestants → pseudoephedrine 30-120mg PO per dose up to 240mg per day 3. antibiotics if symptoms last ≥10-14 days or symptoms severe (fever, facial swelling) -amoxicillin (first line agent if not allergic to penicillin) x 10 days -macrolide (first-line agent if allergic to penicillin) |
Current p193
|
|
|
What are the complications of acute bacterial rhinosinusitis?
|
Local:
orbital cellulitis → vision change facial cellulitis → facial erythema/edema cavernous sinus thrombosis → ophthalmoplegia, chemosis, vision loss intracranial extension → mental status change osteomyelitis *any changes in ocular examination warrants immediate CT |
|
|
|
What is osteomyelitis?
|
bone infection
|
|
|
|
What is cavernosus sinus thrombosis?
|
blood clot in cavernous sinus
|
|
|
|
What is the etiology of cavernosus sinus thrombosis?
|
complication of bacterial infection, usually of paranasal sinuses, usually S. aureus
|
|
|
|
What is the presentation of cavernosus sinus thrombosis?
|
ophthalmoplegia
chemosis visual loss |
|
|
|
Define chemosis.
|
conjuctival edema
|
|
|
|
Define ophthalmoplegia.
|
paralysis of one or more extraocular muscles
|
|
|
|
What is the diagnostic workup for suspected cavernosus sinus thrombosis?
|
MRI
|
|
|
|
What is the management for cavernosus sinus thrombosis?
|
IV antibiotics
|
|
|

|
chemosis
|
|
|
|
What is rhinocerebral mucormycosis?
|
invasive fungal sinusitis
|
|
|
|
What is the etiology of rhinocerebral mucormycosis?
|
immunocompromise (DM, renal failure, AIDs, long-term corticosteroid therapy, therapy for hematologic malignancies) + fungal infection (Mucor, Absidia, Rhizopus) → spread of fungus through vascular channels
|
|
|
|
What is the presentation of rhinocerebral mucormycosis?
|
symptoms initially similar to bacterial rhinosinusitus, but more severe facial pain, clear/straw rhinorrhea, visual symptoms, black eschar on middle turbinate
|
|
|
|
What is pathognomic for rhinocerebral mucormycosis?
|
black eschar on middle turbinate
not universal may not be apparent if infection deep/high within nasal bones |
|
|
|
What is the diagnostic workup of rhinocerebral mucormycosis?
|
nasal biopsy with silver stains → broad nonseptate hyphae within tissues + necrosis with vascular occlusion
|
|
|
|
What is the treatment for rhinocerebral mucormycosis?
|
medical and surgical emergency
1. wide surgical debridement 2. amphotericin B via IV |
|
|
|
What are the complications for rhinocerebral mucormycosis?
|
often loss of at least one eye
20% mortality if DM 50% mortality if renal failure nearly 100% mortality if AIDs or hematologic malignancy |
|
|
|
When is diagnostic imaging of the paranasal sinuses appropriate?
|
uncertain or recurrent cases
order Water view xray |
|
|
|
Describe the steps of the nose exam.
|
1. inspect nose
2. palpate nose 3. assess nostril patency 4. perform nasoscopy → vestibule, inferior and middle turbinates, septum |
|
|

|
orbital cellulitis
|
|
|
|
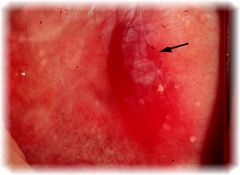
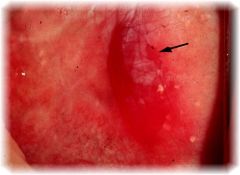
What is leukoplakia?
|

white patch found on buccal mucosa or tongue; non-removable; premalignant
*occasionally found on female external genitals |
|
|
|
|
|
|
|
What is the etiology of oral leukoplakia?
|
chronic irritation resulting in hyperkeratosis (thickening of stratum corneum)
*irritation may be caused by dental problems, alcohol, tobacco |
Current p201
|
|

|
oral candadiasis
|
|
|
|
What is the clinical presentation of oral leukoplakia?
|

white patch on buccal mucosa or tongue; thick, slightly raised, indurated, non-removable; premalignant
|
|
|
|
|
|
|
|
What is the diagnostic work-up of oral leukoplakia?
|
if leukoplakia is enlarging → incisional biopsy or exfoliative cytology
|
|
|
|
What is the common name for oral candadiasis?
|
thrush
|
|
|
|
What is the management of oral leukoplakia?
|
1. remove source of irritation → treat dental problems, stop drinking alcohol, stop smoking (should disappear within few weeks or months)
2. surgical removal |
Current p201
|
|
|
|
|
|
|
What is the diagnostic work-up of erythroplakia?
|
if cannot be attributed to trauma, inflammation, or vascular cause → incisional biospy or exfoliative cytology
|
Current p201
|
|

|
cheilitis
|
|
|

|
tonsillolithiasis
|
|
|

|
oral candidiasis
|
|
|

|
angular cheilitis
|
|
|

|
actinic cheilitis
|
|
|
|
What are the functions of the mouth and oropharnyx?
|
1. breathing
2. vocalization 3. taste 4. initial digestion by mastication and salivary enzymes 5. passage of food |
Mosbys 322
|
|

|
bluish-gray macules → peutz-jeghers syndrome
|
|
|

|
angioedema
|
|
|
|
What is Stenson's duct?
|
parotid duct; drains saliva from from parotid gland to oropharynx; found in buccal mucosa adjacent to maxillary 2nd molar
|
|
|
|
What is Wharton's duct?
|
submandibular duct; drains saliva from submandibular gland to sublingual caruncle; found at sublingual fold adjacent to both sides lingual frenulum
|
|
|
|
What is sialolithiasis?
|
salivary duct stones
|
|
|

|
oral cancer → squamous cell carcinoma on lower lip
|
|
|
|
Where does Stenson's duct exit in the oropharnyx?
|
buccal mucosa adjacent to maxillary 2nd molar
|
|
|
|
Where does Wharton's duct exit in the oropharynx?
|
sublingual fold adjacent to lingual frenulum
|
|
|

|
sialolithiasis of Stenson's duct
|
|
|

|
enlarged tonsils
|
|
|

|
sialolithiasis of Wharton's duct
|
|
|
|
List the salivary glands.
|
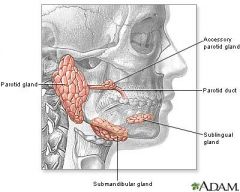
parotid
submandibular sublingual |
|
|
|
Where do the sublingual glands drain into the oropharynx?
|
multiple ducts along sublingual fold
|
|
|
|
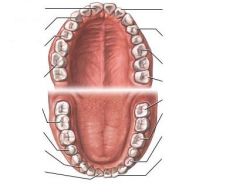
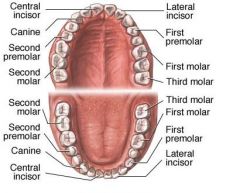
List the number and type of teeth found in each jaw.
|
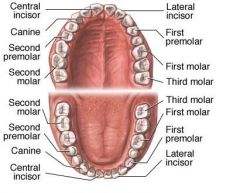
4 incisors
2 canines 4 premolars 6 molars (including wisdom teeth) 32 teeth total |
Mosbys p322
|
|
|
What is another name for the palatotonsillar arch?
|
anterior tonsillar pillar
|
|
|
|
What is another name for the palatopharyngeal arch?
|
posterior tonsillar pillar
|
|
|
|
What are the risk factors for oral cancer?
|
>40y/o
male> female 2:1 black ill-fitting dentures iron deficiency anemia, pernicious anemia, lichen planus, HPV, HIV oral lesions → leukoplakia, erythroplakia, oral lichen planus history of malignancy alcohol tobacco textile or leather manufacturing |
Mosbys p327
|
|
|
What equipment is needed for the oral exam?
|
gloves
penlight tongue blade gauze |
|
|
|
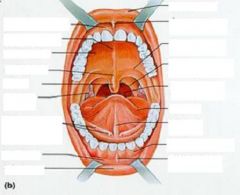
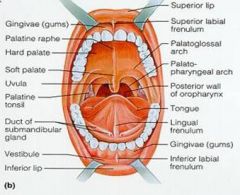
Describe the oral exam.
|
1. inspect and palpate lips (should be smooth, symmetrical, pink) → symmetry, color, edema, lesions
2. inspect buccal mucosa (should be smooth, moist, pinkish red) → color, edema, lesions -stenson's duct (should appear as yellow or whitish pink protrusion) → swelling, exudate, stones (milk duct if swelling present) 3. inspect gingiva (should appear stippled, pink, clear margins at tooth) → inflammation, swelling, bleeding 4. palpate gums → thickening, induration, lesions, masses, tenderness 5. inspect teeth → number, missing teeth, wear, notches, caries 6. palpate teeth → loose teeth 7. ask patient to stick out tongue (should not be atrophied, should be midline) → testing hypoglossal nerve, deviation, tremor, limitation of movement inspect dorsum of tongue (should be dull red, moist, glistening, papillae) → size, color, coating, swelling, ulcerations, atrophy 8. ask patient to touch tip of tongue to roof of mouth inspect ventral surface of tongue (should be smooth, pink, with large veins between frenulum and fimbriated folds, wharton's ducts) → swelling, varicosities 9. wrap tongue with gauze and inspect lateral sides of tongue, wipe tongue with gauze 10. palpate tongue and floor of mouth → nodules, masses, ulcerations 11. inspect uvula, tonsillar pillars, tonsils, and posterior wall of oropharynx → -tonsils should be pink and within confines of tonsillar pillars -posterior wall should be smooth, glistening, pink 12. ask patient to say ah → testing hypoglossal nerve 13. elicit gag reflex → testing glossopharyngeal and vagus nerves |
|
|
|
Define cheilitis.
|

dry cracked lips
|
|
|
|
What is the ddx for cheilitis?
|
Dehydration via:
excessive lip licking wind chapping braces dentures |
Mosbys p336
|
|
|
Define angular cheilitis AKA cheilosis.
|

red unilateral or bilateral fissures at labial commissures
|
Mosbys p336, p342
|
|
|
What is the ddx for angular cheilitis?
|
overclosure of mouth allowing saliva to macerate tissue
iron deficiency anemia riboflavin (vitamin B2) deficiency niacin (vitamin B3) deficiency sprue HIV |
Mosbys p336
|
|

|
angioedema
|
|
|
|
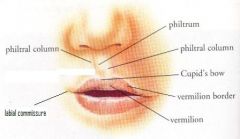
What is actinic cheilitis?
|

whitish discoloration at vermillion border; premalignant; caused by chronic sun exposure
|
|
|
|
Lip pallor indicates?
|
anemia
|
|
|
|
Circumoral pallor indicates?
|

scarlet fever
|
|
|
|
Bluish purple lips indicate?
|

cyanosis
|
|
|
|
Cherry red lips may indicate?
|
acidosis
carbon monoxide poisoning (though cherry red discoloration is thought to be of little use because "cherry red means dead") |
|
|
|
Describe the lips/buccal mucosa in peutz-jeghers syndrome.
|

blue-gray macules
|
|
|

|
circumoral pallor → scarlet fever
|
|
|

|
cyanosis
|
|
|
|
What are fordyce spots?
|
ectopic sebaceous glands on lips and buccal mucosa characterized by small white-yellow raised lesions; normal variation
|
Mosbys p339
|
|
|
What is parotitis?
|
inflammation of the parotid gland(s)
|
|
|
|
What is the most common viral cause of parotitis?
|
mumps virus
|
|
|
|
What is oral hairy leukoplakia?
|

irregular white lesions with "hairy" projections located on lateral tongue
|
Mosbys p342
|
|

|
oral leukoplakia
|
|
|
|
What is gingivitis?
|

inflammation of the gums
|
|
|
|
Deeply pigmented buccal mucosa may indicate?
|
endocrine condition
|
Mosbys p339
|
|
|
Whitish or pinkish scars on buccal mucosa may indicate?
|
trauma from poor tooth alignment
|
Mosbys p339
|
|
|
What is the ddx for gingival hypertrophy?
|
puberty
pregnancy leukemia phenytoin (Dilantin) therapy |
Mosbys p339
|
|
|
Blue-black line along gum margin may indicate?
|

chronic lead or bismuth poisoning
|
Mosbys p339
|
|
|
What is aphthous stomatitis?
|

canker sore
|
Mosbys p339
|
|

|
gingivitis
|
|
|

|
dental caries
|
|
|

|
blue-black line along gum margin → chronic lead or bismuth poisoning
|
|
|

|
aphthous stomatitis
|
|
|

|
glossitis
|
|
|
|
What is the clinical presentation of carbon monoxide poisoning?
|
fatigue, headache, nausea, loss of consciousness, rapid pulse
|
|
|
|
What is the etiology of glossitis?
|
2° to:
dehydration irritant → hot foods, spicy foods, alcohol, tobacco trauma → teeth, dental applicances, burns allergy → mouthwash, toothpaste, mints nutritional deficiency → iron, riboflavin (B2), niacin (B2), cobalamin (B12), vitamin E infection autoimmune disease drug reaction |
Mosbys p340
Current p202 |
|
|
What is the ddx for hairy tongue?
|
reduced flow of saliva
soft diet mouth breathing poor dental hygiene coffee or tea alcohol tobacco oxidizing mouthwashes bismuth-containing antidiarrheals → Peptol-Bismol broad-spectrum antibiotics radiation to head and neck |
|
|
|
What is hairy tongue?
|

abnormally elongated filiform papillae on dorsum of tongue causing hairy appearance and discoloration; usually black, but may be any color depending on source causing discoloration (bacterial overgrowth, food, product, medication)
|
Mosbys p340
|
|
|
How do you differentiate white hairy tongue and oral hairy leukoplakia?
|
mucosal bunch biospy with immunostaining for presence of EBV
if positive for EBV → oral hairy leukoplakia |
|
|

|
black hairy tongue
|
|
|

|
geographic tongue (normal variant)
|
|
|
|
Define stomatitis.
|
inflammation of oral mucosa; may involve lips, buccal mucosa, gums, tongue, or roof/floor of mouth
|
|
|
|
Define gingivostomatitis.
|
gingivitis + stomatitis (inflammation of the gums + inflammation of the oral mucosa)
|
|
|
|
What is torus palatinus?
|

bony protuberance in midline of hard palate; normal variant but may cause denture fitting problems
|
Mosbys p342
|
|

|
torus palatinus (normal variant)
|
|
|
|
What is torus mandibularis?
|

bony protuberance on lingual surface of mandible; normal variant but may cause denture fitting problems
|
|
|

|
torus mandibularis (normal variant)
|
|
|

|
cleft uvula
*benign *subclinical manifestation of cleft palate |
|
|
|
What does saying "ah" test for?
|
1. movement of soft palate → observe soft palate rise symmetrically with uvula remaining in midline
2. glossopharyngeal nerve (CN IX) 3. vagus nerve (CN X) |
Mosbys p343
|
|
|
Failure of soft palate to rise bilaterally while saying "ah" may indicate?
|
vagus nerve paralysis
*uvula will deviate to unaffected side |
Mosbys p343
|
|
|
What is Kaposi's sarcoma?
|
tumor caused by HHV8; can affect skin, oral cavity (usually hard palate or gingiva), respiratory tract, or GI tract
|
|
|
|
Describe the appearance of infected tonsils?
|
enlarged, erythematous, covered in exudate
|
|
|

|
pharyngitis
|
|
|

|
tonsillitis
|
|
|

|
palatal petichiae → GABHS pharyngitis
|
|
|
|
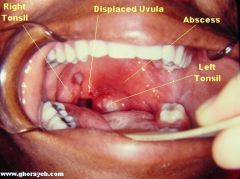
What may a red bulge adjacent to tonsil and extending beyond midline indicate?
|
peritonsillar abscess
|
Mosbys p343
|
|
|
Yellowish mucoid film in pharnyx indictes?
|
postnasal drip
|
Mosbys p343
|
|

|
peritonsillar abscess
*displacing uvula, anterior pillar, and palatine tonsil medially |
|
|
|
What is the presentation of tonsillitis?
|
fatigue, fever, referred ear pain, sore throat, dysphagia, fetid breath, enlarged erythematous tonsils, tonsillar exudates, cervical lymphadenopathy
|
Mosbys p356
|
|
|
What is a peritonsillar abscess?
|
infection of tissue between tonsillar pillar and tonsil; complication of tonsillitis
|
Mosbys p356
|
|
|
What is the presentation of a peritonsillar abscess?
|
fatigue, fever, referred ear pain, sore throat, dysphagia, drooling, muffled voice, enlarge and erythematous tonsil/tonsillar pillar/adjacent soft palate, possible displacement of uvula/tonsil, cervical lymphadenopathy
|
Mosbys p356
|
|
|
What is the clinical presentation of oral cancer?
|
white or red patch (leukoplakia, erythroplakia); non-healing ulceration; induration or mass in buccal mucosa; bleeding; commonly located on vermillion border of lower lip, tongue, or floor of mouth; painless initially but more painful with tissue erosion; cervical lymphadenopathy
|
Mosbys p357
|
|
|
Define xerostomia.
|
dry mouth
|
Mosbys p359
|
|
|
What is the ddx for xerostomia?
|
RA
scleroderma polymyositis Sjogren syndrome smoking anticholinergic or antidepressant drugs radiation therapy |
Mosbys p359
|
|
|
Describe the steps of the oral exam.
|
1. ask about use of dental prostheses
2. inspect lips 3. inspect oral cavity with penlight and tongue blade -inspect buccal mucosa, stenson's duct -inspect gingiva and teeth -inspect palate -inspect tonsillar pillars, tonsils, and posterior wall of pharynx -inspect tongue 4. palpate sublingual area while grasping tongue with gauze → wharton's duct 5. note breath odor |
|
|
|
What is sialadenitis?
|
inflammation of a salivary gland
|
|
|
|
What is the etiology of aphthous stomatitis?
|
unknown; possible association with HHV6
|
Current p203
|
|
|
What is the clinical presentation of aphthous stomatitis?
|

small round ulceration with yellow-gray fibroid center surrounded by red halo; single or multiple; found on labial or buccal mucosa; painful; recurrent
|
Current p203
|
|
|
What is the management of aphthous stomatitis?
|
for symptomatic relief, prescribe topical corticosteroids, either triamcinolone acetonide or fluocinonide
|
Current p203
|
|
|
What are other names for aphthous stomatitis?
|
aphthous ulcer
ulcerative stomatitis canker sore |
Current p203
|
|
|
How long does pain last and how long does healing take for aphthous stomatitis?
|
painful for 7-10 days, healing takes 1-3 weeks
|
Current p203
|
|
|
What is the ddx for aphthous stomatitis?
|
if large or persistent, consider:
erythema multiforme drug allergies herpes simplex pemphigus pemphigoid epidermolysis bullosa acquisita bullous lichen planus Behcet disease inflammatory bowel disease squamous cell carcinoma |
Current p203
|
|
|
What is glossodynia?
|
burning and pain of the tongue +/- glossitis
|
Current p202
|
|
|
Name oral lesions considered to be premalignant.
|
actinic cheilitis
leukoplakia erythroplakia oral lichen planus |
|
|

|
erythroplakia
|
|
|
|
peritonsillar abscess
|
|
|
|
What type of cancer accounts for 90% of oral cancer?
|
squamous cell carcinoma
|
Current p201
|
|
|
2-6% of cases of leukoplakia and 90% of cases of erythroplakia are either ... or .... ?
|
dysplasia
carcinoma |
Current p201
|
|
|
What are the major risk factors for oral leukoplakia and erythroplakia?
|
alcohol
tobacco (especially pipes and chewing tobacco) |
Current p201
|
|
|
erythroplakia
|
|
|
|
What is the clinical presentation of erythroplakia?
|
red patch on buccal mucosa, tongue, or palate; soft, velvety; premalignant
|
|
|
|
What is the treatment for erythroplakia?
|
1. if indicated by biopsy → surgical excision
2. long-term monitoring since recurrence common |
|
|
|
What is erythroplakia?
|
red patch on buccal mucosa, tongue, or palate that can't be attributed to any other pathology; premalignant
|
|
|
|
What is the etiology of erythroplakia?
|
unknown; possibly similar to squamous cell carcinoma
|
|
|

|
white, lacy, reticular pattern on buccal mucosa → oral lichen planus
|
|
|
|
What is the clinical presentation of oral lichen planus?
|
1. white, lacy reticular lesions on buccal mucosa (may mimic candidiaisis, leukoplakia)
2. erosive lesions (may mimic SCC) |
|
|
|
What is oral lichen planus?
|
chronic inflammatory autoimmune disease
|
|
|
|
What is the management of oral hairy leukoplakia?
|
zidovudine or acyclovir
|
Current p202
|
|
|
What is the management for suspected oral cancer?
|
1. if unclassifiable white or red lesion that persists >2 weeks → refer to ENT for evaluation, biopsy, and treatment
2. treatment dependent on staging 3. if small → surgical excision 4. if large → surgical excision, neck dissection, radiation |
Current p202
|
|
|
What is the cause for 75% of oral cancer?
|
alcohol
tobacco |
|
|

|
oral cancer → squamous cell carcinoma on ventrolateral tongue
|
|
|

|
oral cancer → squamous cell carcinoma on floor of mouth
|
|
|

|
oral cancer → squamous cell carcinoma on ventrolateral tongue
|
|
|
|
What are filiform papillae?
|
1 of 4 types of lingual papillae; small white prominences on surface of tongue; v-shaped cones with filamentous processes; abrasive coating; do not contain taste buds
|
|
|
|
What sign occurs with defective desquamation of filiform papillae?
|
hairy tongue →
white hairy tongue (papillae naturally white) black hairy tongue (papillae discolored by overgrowth of bacteria or food/product/medication) |
|
|
|
What is the clinical presentation of glossitis?
|

inflammation of the tongue with loss of filiform papillae resulting in smooth tongue; rarely painful
|
Current p202
|
|
|
What is the management of glossitis?
|
1. treat primary cause
2. if primary cause not found → consider empiric nutritional therapy |
Current p202
|
|
|
What is "burning mouth syndrome"?
|
glossodynia in absence of any clinical findings; most common in postmenopausal women; no associated risk factors; benign; may be treated with alpha-lipoic acid or clonazepam
|
Current p203
|
|
|
What is the etiology of glossodynia?
|
associated with:
causes of glossitis xerostomia candidiasis DM drugs → diuretics tobacco |
Current p203
|
|
|
What is the management of glossodynia?
|
1. treat primary cause
2. choose alternative medications 3. encourage smoking cessation 4. reassure patient that glossodynia is benign |
Current p203
|
|
|
What are other names for necrotizing ulcerative gingivitis?
|
vincent's infection
trench mouth |
Current p203
|
|
|
What is the etiology of necrotizing ulcerative gingivitis?
|
stress (common in young adults at examination time) or predisposing factors (systemic diseases) → bacterial infection characterized by fusiform bacilli (gram-pos) and spirochetes (gram-neg)
|
Current p203
|
|
|
What is the clinical presentation of necrotizing ulcerative gingivitis?
|
acute gingival inflammation and necrosis; painful; possible fever, halitosis, bleeding, cervical lymphadenopathy
|
Current p203
|
|
|
What is the management of necrotizing ulcerative gingivitis?
|
1. penicillin 250mg PO 3x daily x 10 days
2. warm half-strength peroxide rinses |
Current p203
|
|
|
What is herpetic stomatitis?
|
viral infection of the mouth
|
|
|
|
What is the etiology of herpetic stomatitis?
|
HSV
|
|
|
|
What is the clinical presentation of herpetic stomatitis?
|
initial burning
small vesicles → rupture → scab usually on gingiva or mucocutaneous border of lip sometimes on soft palate, buccal mucosa or tongue |
|
|
|
What is the management for herpetic stomatitis?
|
1. if immunocompetent → mild, short-lived (10 days)
2. if immunocompromised → prescribe acyclovir 200-800mg 5x daily x 7-14 days |
|
|
|
What is the prevention for herpetic stomatitis?
|
1. avoid contact with infected people (cold sores or herpetic stomatitis)
2. avoid sharing food, drinks, utensils |
|
|
|
What % of the population carries HSV?
|
~90%
|
|
|

|
herpetic stomatitis
|
|
|
|
What is the management of hairy tongue?
|
1. benign and self-limited
2. brush tongue daily 3. improve oral hygiene 3. refrain from drinking tea, coffee, or alcohol; refrain from smoking; change mouthwash |
|
|
|
What are the types of gingivitis?
|
1. plaque-associated gingivitis
2. necrotizing ulcerative gingivitis 3. hormone-induced gingival hyperplasia → puberty, pregnancy 4. drug-induced gingival hyperplasia → dilantin, cyclosporin, procardia 5. bacterial, viral, or fungal infection → herpetic stomatitis, oral candidiasis 6. mucocutaenous diseases → oral lichen planus, pemphigus vulgaris 7. blood disorders → acute leukemia |
|
|
|
What is herpangina?
|
viral infection of the mouth
|
|
|
|
What is the etiology of herpangina?
|
caused by coxsackieviruses; spread via respiratory droplets or fecal-oral; usually affects infants and young children in summer
|
|
|
|
What is the clinical presentation of herpangina?
|

high fever; sore throat, dysphagia, and loss of appetite; red macules → vesicles → ulcerations with white-grey base and red border, located on soft palate or tonsillar pillars
|
|
|
|
What is the management and patient eduction for herpangina?
|
1. self-limiting → usually resoves in 1 week
2. take acetominophen or ibuprofen for fever and discomfort (avoid aspirin) 3. increase fluids 4. eat cold non-irritating diet → milk, icecream, popsicles 5. avoid citrus, fried, spicy, and hot food |
|
|
|
What is the prevention for herpangina?
|
handwashing
|
|
|

|
herpangina
|
|
|
|
In children <12y/o with a viral illness, what medication should not be used?
|
aspirin
|
|
|
|
What is hand, foot, and mouth disease?
|
viral infection of the hands, feet, and mouth
|
|
|
|
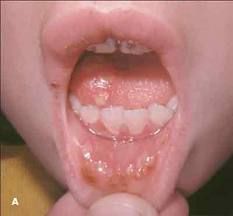
What is the etiology of hand, foot, and mouth disease?
|
caused by coxsackievirus; transmitted via rhinorrhea, saliva, sputum, stool, blister fluid; commonly occurs in young children during summer and early fall
|
|
|
|
What is the clinical presentation of hand, foot, and mouth disease?
|

fatigue; fever; sore throat; non-pruritic blistering rash on hands, feet, and buttocks; ulcers in mouth
|
|
|
|
What is the management and patient education of hand, foot, and mouth disease?
|
1. self-limiting → resolves in 7-10 days
2. take acetominophen or ibuprofen for fever and pain 3. rinse with salt water → 1/2 tsp salt, 1 glass of warm water 4. increase fluids to prevent dehydration |
|
|
|
What is the prevention of hand, foot, and mouth disease?
|
avoid contact with infected people; handwashing; cleaning objects
|
|
|
|
What is cellulitis?
|
diffuse inflammation of connective tissue of skin (dermis and hypodermis)
|
|
|
|
What is the etiology of bacterial sialadenitis?
|
usually caused by S. aureus; associated with ductal obstruction, dehydration, chronic illness, sjogren's syndrome
*viral parotitis usually caused by mumps virus |
Current p206
|
|
|
What is the clinical presentation of bacterial sialadenitis?
|
acute swelling of parotid or submandibular gland; increased pain and swelling with meals; tenderness, erythema, and pus at ductal opening
*viral sialadenitis is non-painful |
Current p206
|
|
|
What is the management of sialadenitis?
|
1. IV antibiotics → nafcillin 1g IV q4-6hr
2. increase salivary flow → hydration, sialogogues (lemon drops), warm compresses, massage of gland 3. rinse mouth with salt water → 1 tsp salt + 1 cup water 3. practice good oral hygiene |
Current p206
|
|

|
sialadenitis → parotitis
|
|
|
|
What is the etiology of sialolithiasis?
|
crystallization of saliva → blockage of duct; associated with stricture or infection
|
|
|
|
What is the clinical presentation of sialolithiasis?
|
local pain and swelling
|
|
|
|
What is the management of sialolithiasis?
|
remove stone manually or surgically
|
|
|
|
Which is more common, sialolithiasis of Stenson's duct or Wharton's duct?
|
Wharton's duct
|
Current p206
|
|
|
What is the etiology of GABHS pharyngitis?
|
group A beta-hemolytic streptococcus
|
|
|
|
What is the presentation of GABHS pharyngitis?
|
Centor Criteria:
sore throat + 1. fever >100.4°F 2. pharyngotonsillar exudates 3. anterior cervical lymphadenopathy 4. no cough *if 1 criteria present → unlikely *if 2 criteria present → possible *if 3 criteria present → likely *if 4 criteria present → treat regardless of rapid strep odynophagia, scarlatiniform rash; no rhinorrhea or hoarseness |
|
|
|
What is the diagnostic work-up of GABHS pharyngitis?
|
rapid strep; throat culture if negative
|
|
|
|
What is the etiology of mononucleosis?
|
epstein barr virus (EBV); transmitted via saliva or genital secretions; common in young adults
|
Current p204
|
|
|
What is the presentation of mononucleosis?
|
fatigue, fever, sore throat, myalgia; cervical lymphadenopathy; hepatosplenomegaly; possible palatal petichiae, tonsillar exudates, or maculopapular rash
*1/3 of mono also presents with GABHS |
Current p204
|
|
|
What is the diagnostic work-up of mononucleosis?
|
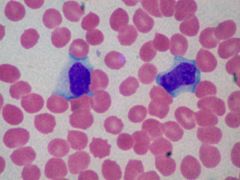
CBCDP → lymphocytosis (>35%)
blood smear → atypical large lymphocytes monospot EBV titers if monospot negative |
Current p204
|
|
|
What is the presentation of viral pharyngitis?
|
sore throat, rhinorrhea, no pharyngotonsillar exudate
|
Current p204
|
|
|
What are the indications for tonsillectomy?
|
1. airway obstruction → sleep apnea, cor pulmonale
2. recurrent streptococcal tonsillitis 3. recurrent peritonsillar abscess 4. chronic tonsillitis 5. if persistent tonsillar asymmetry → excisional biopsy to R/O lymphoma |
Current p207
|
|
|
What are the cons of tonsillectomy?
|
1. pain, especially if adult
2. protracted fever and emesis 3. post-operative bleeding, may lead to laryngospasm or airway obstruction |
Current p207
|
|
|
What are the complications of GABHS pharyngitis?
|
scarlet fever
rheumatic fever glomerulonephritis local abscess formation |
Current p205
|
|
|
What is the treatment for GABHS pharyngitis?
|
1. prescribe antibiotics to prevent sequelae
|
|
|
|
What is the diagnostic work-up of viral pharyngitis?
|
rapid strep to R/O GABHS
|
|
|
|
What is the management of viral pharyngitis?
|
1. self-limiting → resolves within 7-10 days
2. acetominophen for fever 3. salt water gargle → 1tsp salt, 1 cup water several times per day 4. NO ANTIBIOTICS!!! |
|
|
|
What are the complications of viral pharyngitis?
|
complications rare
|
|
|
|
How long before a person infected with mononucleosis would test positive with a monospot?
|
4 weeks after onset
|
Current p1243
|
|
|
Interpret the results of an EBV titer for mononucleosis.
|
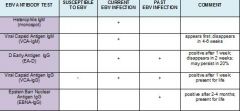
1. if VCA-IgM positive → current infection
2. if VCA-IgG positive → recent or past infection 3. if VCA-IgM negative but others positive → past infection 4. if VCA-IgG negative → susceptible to infection |
|
|
|
What is the management of mononucleosis?
|
1. acetominophen or ibuprofen for pain and fever
2. warm salt water gargle 3-4x daily for sore throat 3. increase fluids 4. rest 5. avoid contact sports >4 weeks 6. if GABHS → penicillin or erythromycin 7. if impending airway obstruction, hemolytic anemia, or severe thrombocytopenia → corticosteroids |
|
|
|
Define trismus.
|
inability to open mouth fully
|
|
|

|
bilateral submandibular lymphadenopathy
|
|
|

|
submental lymphadenopathy
|
|
|
|
What is ludwig's angina?
|
cellulitis of the sublingual and submaxillary spaces; ENT emergency due to potential airway obstruction
|
Current p206
|
|
|
What is the etiology of ludwig's angina?
|
polymicrobial infection caused by staphylococci, streptococci, and bacteroides
usually dental infection → infected or recently extracted lower molar tongue piercing foreign body or laceration in floor of mouth oral infection mandible fracture oral malignancy |
|
|
|
What is the clinical presentation of ludwig's angina?
|

dental pain or recent dental procedure; dysphonia, hot potato voice, dysphagia, odynophagia, sore throat, neck swelling, restricted neck movement; erythema and edema of submandibular area; often erythema and edema of floor of mouth; possible displacement of tongue superior and posterior
|
Current p206
|
|
|
What is the management of ludwig's angina?
|
1. determine state of airway → tracheotomy, intubation
2. prescribe empiric antibiotics → penicillin + clindamycin or metronidazole 3. order C&S to refine antibiotic treatment 4. if refractory to treatment → surgical drainage |
|
|
|
Define dysphagia.
|
difficulty swallowing
|
|
|
|
Define odynophagia.
|
painful swallowing
|
|
|
|
Define dysphonia.
|
difficulty speaking
|
|
|
|
List conditions characterized by "hot potato voice."
|
peritonsillar abscess
ludwig's angina |
|
|
|
What is the clinical presentation of cerumen impaction?
|
hearing loss
pruritus pain tinnitus cough |
|

