![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
215 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are the characteristics of nephrotic vs. nephritic syndrome?
|
NEPHRITIC SYNDROME:
HTN edema → periorbital, scrotal ↓ GFR hematuria proteinuria NEPHROTIC SYNDROME: peripheral edema hypoalbuminemia hyperlipidemia heavy proteinuria >3.5g/24h |
Current ch22
|
|
|
List nephrotic syndromes.
|
primary:
minimal change disease focal glomerular sclerosis membranous nephropathy membranoproliferative glomerulonephritis secondary associated with DM, SLE, amyloidosis |
|
|
|
What is the etiology of minimal change disease?
|
idiopathic
associated with: hypersensitivity (bee stings, NSAIDs) viral URTI tumors (Hodgkin disease) drugs (lithium, gold) |
|
|
|
What are the USPSTF screening recommendations for renal cell carcinoma?
|
no recommendations
|
USPSTF Handbook 2009
|
|
|
What is the clinical presentation of minimal change disease?
|
nephrotic syndrome changes
-protein malnutrion -hyperlipidemia -more susceptible to infection and thromboembolic events -rarely acute kidney injury |
|
|
|
What is the diagnostic workup of minimal change disease?
|
hypoalbuminemia
proteinemia hyperlipidemia proteinuria histology |
|
|
|
What are the USPSTF screening recommendations for Wilms' tumor?
|
no recommendations
|
USPSTF Handbook 2009
|
|
|
What is the management of minimal change disease?
|
1. prednisone 1mg/kg/d
2. continue treatment several weeks following remission of proteinuria |
|
|
|
What is the prognosis of minimal change disease?
|
children often recover quickly
adults may requires 16 weeks of prednisone treatment most complications due to corticosteroids ESRD rare |
|
|
|
What patient population is most commonly affected by minimal change disease?
|
children
|
|
|
|
Nephritic syndrome.
|
HTN → due to volume overload
edema → first seen in low pressure areas → periorbital, scrotal hematuria +/- dysmorphic RBCs or RBC casts proteinuria |
|
|
|
What is the etiology of post-streptococcal glomerulonephritis?
|
group A beta-hemolytic streptococci (especially type 12)
commonly occurs following pharyngitis or impetigo |
|
|
|
What is the clinical presentation of post-streptococcal glomerulonephritis?
|
strep throat or impetigo 1-3 weeks prior
HTN edema cola-colored urine oliguria |
|
|
|
What is the diagnostic workup of post-streptococcal glomerulonephritis?
|
high ASO titer (unless given antibiotics)
hematuria → RBC casts proteinuria → <3.5g/24h |
|
|
|
What is the management of post-streptococcal glomerulonephritis?
|
1. antibiotics
2. antihypertensives 3. diuretics 4. salt restriction |
|
|
|
What is the prognosis of post-streptococcal glomerulonephritis?
|
children → outcome favorable
adults → more prone to chronic kidney disease |
|
|
|
What is the prevention of post-streptococcal glomerulonephritis?
|
treat strep throat appropriately
|
|
|
|
Colo-colored urine may indicate?
|
post-streptococcal glomerulonephritis (1-3 weeks following infection)
IgA nephropathy (few days following infection) |
|
|
|
What is another name for IgA nephropathy?
|
Berger disease
|
|
|
|
What is the etiology of IgA nephropathy?
|
unknown
associated with: HIV CMV hepatic cirrhosis celiac disease most common nephritic syndrome in U.S. commonly occurs in adolescent males |
|
|
|
What are the risk factors for renal cell carcinoma?
|
smoking
familial and genetic factors dialysis |
|
|
|
What is the clinical presentation of IgA nephropathy?
|
gross hematuria
URTI (50%) flu-like illness (15%) GI symptoms (10%) red or cola-colored urine 1-2 days following onset |
|
|
|
What is the clinical presentation of renal cell carcinoma?
|
fever, weight loss
hematuria flank pain palpable mass in abdomen |
|
|
|
What is the diagnostic workup of IgA nephropathy?
|
↑ IgA (50%)
hematuria proteinuria renal biopsy → positive IgA staining |
|
|
|
What is the diagnosic workup of renal cell carcinoma?
|
erythrocytosis 5% though anemia more common
hypercalcemia 10% UA → hematuria 60% KUB or CT → renal masses |
|
|
|
What is the management of IgA nephropathy?
|
1. if significant proteinuria (>1g/24h) → ACE inhibitor or ARB, corticosteroids, fish oil
2. if ESRD → kidney transplant |
|
|
|
What is the management of renal cell carcinoma?
|
1. if localized → partial or complete nephrectomy
2. no effective chemotherapy |
|
|
|
What is the prognosis of IgA nephropathy?
|
33% → remission
40-50% → chronic kidney disease remainder → stable CREAT + chronic hematuria |
|
|
|
What is the pattern of metastasis for renal cell carcinoma?
|
◦Lung (75%)
◦Soft tissues (36%) ◦Bone (20%) ◦Liver (18%) ◦Cutaneous sites (8%) ◦Central nervous system (8%) |
|
|
|
What is Goodpasture syndrome?
|
nephritic syndrome characterized by glomerulonephritis + pulmonary hemorrhage
|
|
|
|
What is the etiology of Goodpasture syndrome?
|
anti-GBM antibodies
associated with: influenza A hydrocarbon solvent exposure HLA-DR2 and HLA-B7 antigens 6x more common in males more common in 20-40y/o |
|
|
|
What does anti-GBM antibodies stand for?
|
anti-glomerular basement membrane antibodies
|
|
|
|
What is the clinical presentation of Goodpasture syndrome?
|
URTI (20-60%)
HTN edema dyspnea hemoptysis respiratory failure |
|
|
|
What is the diagnostic workup of Goodpasture syndrome?
|
CBC → iron deficiency anemia
anti-GBM antibodies → positive (90%) sputum → hemosiderin-laden macrophages CXR → shifting pulmonary infiltrates due to pulmonary hemorrhage |
|
|
|
What is the management of Goodpasture syndrome?
|
1. plasma exchange to remove anti-GBM antibodies x daily for <2 weeks
2. immunosuppressive therapy to prevent formation of anti-GBM antibodies and control inflammation 3. corticosteroids 4. cyclophosphamide |
|
|
|
What is the etiology of polycystic kidney disease?
|
genetic → autosomal dominant disorder
common |
|
|
|
What is the clinical presentation of polycystic kidney disease?
|
FH of polycystic kidney disease
hx of UTI or nephrolithiasis abdominal or flank pain HTN abdominal mass large palpable kidneys +/- hepatic, splenic, and pancreatic cysts |
|
|
|
What is the diagnostic workup of polycystic kidney disease?
|
UA → hematuria, mild proteinuria
US → bilateral kidney cysts |
|
|
|
What is the management of polycystic kidney disease?
|
1. for pain → bed rest, analgesics
2. hydration if kidney stones 3. antibiotics if renal infection 4. anti-hypertensives for HTN 5. eat low-protein diet; avoid caffeine |
|
|
|
What is the prognosis of polycystic kidney disease?
|
50% → ESRD by 60y/o
|
|
|
|
What is the etiology of acute tubular necrosis?
|
1. ischemia → due to prolonged hypotension or hypoxia → due to volume depletion, sepsis, shock, surgery
2. nephrotoxins → aminoglycosides, cyclosporine, contrast dye, myoglobinuria (due to rhabdomyolitis), hemolysis, hyperuricemia, multiple myeloma |
|
|
|
What is the clinical presentation of acute tubular necrosis?
|
symptoms of acute kidney injury
urine → brown |
|
|
|
What is the diagnostic workup of acute tubular necrosis?
|
hyperkalemia
hyperphosphatemia BUN:CREAT <20:1 UA → pigmented (muddy brown) granular casts, renal tubular epithelial cells, epithelial casts ↑ urine sodium |
|
|
|
What is the management of acute tubular necrosis?
|
1. avoid volume overload and hyperkalemia → loop diuretics
2. treatment dependent on cause 3. dialysis indicated if life-threatening electrolyte disturbances, volume overload unresponsive to diuretic therapy, worsening metabolic acidosis, uremic complications |
|
|
|
What is the prognosis of acute tubular necrosis?
|
mortality 20-50% in hospital settings, 70% if comorbidities, higher if elderly, severe disease, and multisystem organ failure
|
|
|
|
What is acute tubular necrosis?
|
acute kidney injury due to tubular damage
|
|
|
|
Muddy brown casts may indicate?
|
acute tubular necrosis
|
|
|
|
What is acute renal failure (acute kidney injury)
|
sudden decrease in kidney function → inability to maintain fluid, electrolyte, and acid-base balances or excrete nitrogenous wastes
3 LEVELS: 1. risk → 1.5-fold ↑ serum CREAT 2. injury → 2-3-fold ↑ serum CREAT 3. failure → decreased urine output <0.5mg/kg/h over 6,12, or 24 hours |
|
|
|
What is the clinical presentation of acute renal failure?
|
malaise
nausea vomiting altered sensation altered fluid homeostatsis HTN pericardial effusion (manifesting as pericardial friction rub) → cardiac tamponade arrhythmias due to hyperkalemia rales due to hypervolemia diffuse abdominal pain bleeding and clotting disorders encephalopathy → confusion, asterixis, seizures |
|
|
|
What is the diagnostic workup of acute renal failure?
|
sudden ↑ BUN and CREAT
hyperkalemia hyperphosphatemia metabolic acidosis hypocalcemia anemia over weeks |
|
|
|
What is the etiology of acute renal failure?
|
1. prerenal
2. intrinsic 3. postrenal |
|
|
|
What is prerenal azotemia?
|
renal hypoperfusion → decreased GFR → increased BUN and serum CREAT
|
|
|
|
What is postrenal azotemia?
|
obstructive uropathy → decreased GFR → increased BUN and seum CREAT
|
|
|
|
What is the etiology of prerenal azotemia?
|
renal hypoperfusion can be caused by:
volume depletion ∆ vascular resistance ↓ cardiac output |
|
|
|
Why is a decreased FeNa seen in prerenal acute kidney injury?
|
decreased GFR → decrease Na+ to INTACT tubules → increased fraction of filtered Na+ absorped → decrased fraction of Na+ excreted
|
|
|
|
Decreased FeNa may indicate?
|
prerenal acute kidney disease
|
|
|
|
What does a FeNa <1% mean? What does a FeNa >1-2% mean?
|
<1% means tubular function intact → prerenal
>1-2% means tubular function NOT intact → acute tubular necrosis |
|
|
|
BUN rising out of proportion of CREAT suggests?
|
prerenal
↓ GFR → increased BUN and CREAT → with enhanced water and salt absorption in prerenal states → urea passively absorbed with Na+ but CREAT secreted → BUN rises out of proportion to CREAT |
|
|
|
What are the most common causes of acute kidney injury?
|
70-75% caused by:
1. prerenal 2. instrinsic → acute tubular necrosis |
|
|
|
Compare the BUN:CREAT, Urine Na+, FeNa, and Urine Osm in prerenal and acute tubular necrosis.
|
PRERENAL (tubules intact):
BUN:CREAT ratio → >20:1 (urea reabsorped with Na+ but not creatinine) Urine Na+ → <10 (Na+ reabsorped) FeNa → <1% (Na+ reabsorped) Urine Osm → >500 (urine concentrated b/c tubules intact) ACUTE TUBULAR NECROSIS (tubules not intact): BUN:CREAT ratio → 10:1 Urine Na+ → >20 (decreased Na+ reabsorption) FeNa → >2% (decreased Na+ reabsorption) Urine Osm → 300-350 (less concentrated b/c tubules NOT intact) |
|
|
|
What is the ddx for acute kidney injury?
|
1. prerenal
2. instrinsic → acute tubular necrosis, interstitial nephritis, acute glomerulonephritis 3. postrenal |
|
|
|
What is the etiology of postrenal azotemia?
|
renal pelvis obstruction
urethral obstruction bladder obstruction ureteral stones urethral stones blood clots neurogenic bladder BPH bladder, prostate, or cervical cancer most common cause in men = BPH |
|
|
|
What is the etiology of acute interstitial nephritis?
|
1. drug reaction (70%) → NSAIDs, penicillins, cephalosporins, sulfonamides, rifampin (TB), sulfa-containing diuretics, , PPIs (GERD), allopurinol (gout), phenytoin (seizures)
2. infection → strep, CMV, rocky mountain spotted, fever, histoplasmosis, leptospirosis 3. autoimmune → SLE, sjogren's, sarcoidosis, cryoglobulinemia 4. idiopathic |
Current ch22
|
|
|
What is the clinical presentation of acute interstitial nephritis?
|
fever (>80%)
transient maculopapular rash (25-50%) arthralgias acute or chronic kidney injury |
Current ch22
|
|
|
What is the diagnostic workup of acute interstitial nephritis?
|
CBC → eosinophilia (80%)
UA → hematuria (95%), RBCs, pyuria (including eosinophiluria), WBCs, WBC casts, modest proteinuria especially if due to NSAIDs |
Current ch22
|
|
|
What is the management of acute interstitial nephritis?
|
1. discontinue causitive agent
2. supportive measures 3. if kidney injury persists → short-course corticosteroids → prednisone or methylpredinisone |
Current ch22
|
|
|
What is the prognosis of acute interstitial nephritis?
|
good
recovery over weeks to months rarely progress to ESRD |
Current ch22
|
|
|
RBC casts indicate?
|
glomerulonephritis
|
|
|
|
What is acute kidney disease (AKA acute renal failure)?
|
worsening of kidney function over hours to days → retention of BUN and CREAT
|
|
|
|
What is chronic kidney disease?
|
worsening of kidney function over months to years
|
|
|
|
Oliguria is unusual in chronic kidney disease, true or false?
|
true
|
|
|
|
Compare acute vs. chronic renal disease.
|
ACUTE:
worsening over hours to days oliguria or not anemia rare small kidneys rare CHRONIC: worsening over months to years oliguria rare anemia common small kidneys common (except polycystic kidney disease, HIV nephropathy, diabetic nephropathy, scleroderma, amyloidosis, leukocytic infiltration) |
|
|
|
Anemia, abnormally small kidneys, and no oliguria often indicates?
|
chronic kidney disease
|
|
|
|
What is vesicoureteral reflux?
|
type of chronic interstitial nephritis
characterized by retrograde flow of urine from bladder to kidneys during voiding caused by incompetent vesicoureteral spincter → urine enters interstitium of kidney → inflammation → fibrosis disorder of childhood (most damage occurs before 5y/o) HTN, hx of UTIs, chronic kidney disease, focal glomerulosclerosis substantial proteinuria (unusually in most tubular diseases) US or IVP → renal sclerosis or hydronephrosis if mild → antibiotic prophylaxis if sever → surgery can progress to ESRD |
|
|
|
What is hydronephrosis?
|
distension and dilation of renal pelvic calyces due to vesicoureteral reflux (retrograde flow of urine from bladder to kidney)
|
|
|
|
What is ESRD?
|
when kidneys function is <10% of normal, requiring dialysis or kidney transplant to sustain life
|
|
|
|
What is uremia?
|
caused by kidney failure (more commonly chronic but sometimes acute)
characterized by fluid, electrolyte, acid-base, metabolic, and hormone imbalances |
|
|
|
What are the indications for kidney transplant?
|
1. chronic kidney failure → DM, HTN, glomerulonephritis, polycystic kidney disease, etc.
2. kidney tumor → Wilm's tumor, renal cell carcinoma |
|
|
|
What is the approach to continuing care following a kidney transplant?
|
1. immunosuppressive therapy
-induction therapy at time of transplant -maintenance therpay post-transplant 2. hemodialysis within 48 hours of transplant 3. monitor potassium to prevent hyperkalemia 4. recovery within 3-6 weeks |
|
|
|
What is the appropriate next step when pyelonephritis is unresolving despite appropriate antibiotics?
|
treatment failure warrants US or CT
|
|
|
|
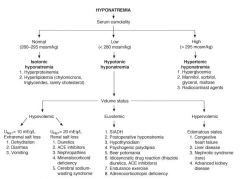
What is the diagnostic workup of hyponatremia?
|
order serum sodium → if <135 mEq/L → hyponatremia → order serum osmolality → if <280 mEq/L → hypotonic hyponatremia → evaluate volume status → urine sodium
BMP +/- thyroid or adrenal function tests |
Current ch21
|
|
|
Hyponatremia is usually due to a sodium deficiency, true or false?
|
false, hyponatremia is usually due to excess water relative to sodium
|
Current ch21
|
|
|
Define hyponatremia.
|
serum sodium <135 mEg/L
|
Current ch21
|
|
|
What is the most common electrolye disoder in hospitalized patients?
|
hyponatremia
|
Current ch21
|
|
|
What are the complications of hyponatremia?
|
iatrogenic cerebral osmotic demyelination due to overly rapid sodium correction
|
Current ch21
|
|
|
Total body water and sodium can be low, normal, or high in presence of hyponatremia, true or false?
|
true
|
Current ch21
|
|
|
What is the etiology of hyponatremia + normal osmolality (AKA isotonic hyponatremia)?
|
pseudohyponatremia caused by:
hyperproteinemia → paraproteinemias, IV immunoglobulin therapy hyperlipidemia → usually chylomicrons or triglycerides (rarely cholesterol) |
Curent ch21
|
|
|
What is the etiology of hyponatremia + high osmolality (AKA hypertonic hyponatremia)?
|
translocational hyponatremia caused by:
hyperglycemia mannitol therapy for ↑ ICP radiocontrast agents *glucose and mannitol cause osmosis of water from intracellular space to extracellular space → decreasing plasma sodium concentraiton |
Current ch21
|
|
|
What is the normal range for serum osmolality?
|
280-295 mOsm/kg
|
Ch21
|
|
|
What is the etiolgy for hyponatremia + low serum osmolality (AKA hypotonic hyponatremia)?
|
|
|
|
|
What is the clinical presentation of hyponatremia?
|
dependent on acuity and severity
if severe (<110) and chronic → may be asymptomatic due to adaptation if mild (130-135) and acute → often asymptomatic fatigue, nausea → HA, lethargy, disorientation → respiratory arrest, seizure, brainstem herniation, brain damage, coma → death |
|
|
|
What is the evaluation of a electrolyte disorder?
|
fluid intake
fluid outake medications |
|
|
|
What does SIADH stand for?
|
syndrome of inappropriate ADH secretion
|
|
|
|
What are the diagnostic criteria for SIADH?
|
1. hyponatremia <135 mEq/L
2. low osmolality <280 mOsm/kg 3. euvolemia 4. urine sodium >20 mEq/L 5. normal thyroid and adrenal function 6. absence of heart, liver, or kidney diseae 7. may also see low BUN <10mg/dL or hypouricemia <4 mg/dL |
|
|
|
SIADH is ruled out by?
|
azotemia
azotemia is associated with hypovolemia SIADH is associated with euvolemia |
|
|
|
What is the diagnostic workup of hypocalcemia?
|
ionized calcium
PTH vitamin D magnesium |
|
|
|
Low total serum calcium + normal ionized calcium usually indicates?
|
normal calcium metabolism
|
Current ch21
|
|
|
What is the most common cause of low total serum calcium vs low ionized caclium (true hypocalcemia)?
|
low total serum calcemia → hypoalbuminemia
low ionized calcium → CKD |
Current ch21
|
|
|
What is the most accurate measurement of serum calcium?
|
ionized calcium
|
Current ch21
|
|
|
What are the clinical symptoms of hyponatremia?
|
lethargy
agitation disorientation nausea anorexia muscle cramps hypothermia cheyne-stokes respiration hyporeflexia (decreased DTRs) seizures |
Interpreting Laboratory Data p122
|
|
|
What are the clinical symptoms of hypernatremia?
|
thirst
lethargy restlessness irritability muscle spasms hyperreflexia (increased DTRs) seizures coma death |
Interpreting Laboratory Data p124
|
|
|
What are the clinical symptoms of hypokalemia?
|
fatigue
muscle weakness muscle cramps hypotension arrhythmias areflexia |
|
|
|
What are the clinical symptoms of hyperkalemia?
|
muscle weakness
hypotension bradycardia arrhythmias cardiac arrest |
|
|
|
hypophosphatemia
|
tissue hypoxia
rhabdomyolysis parasthesias encephalopathy |
|
|
|
What is the diagnostic workup of metabolic acidosis?
|
ABG:
pH decreased PCO2 decreased HCO3- decreased anion gap normal or increased |
|
|
|
What are the two type of metabolic acidosis?
|
anion gap acidosis → increased unmeasured anions
normal anion gap acidosis |
|
|
|
What is the anion gap?
|
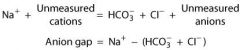
difference between readily measured anions and cations
|
|
|
|
What is the etiology of metabolic acidosis? Distinguish between anion gap acidosis and normal anion gap acidosis.
|
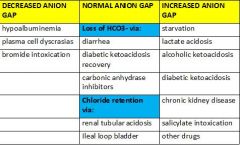
|
|
|
|
What is the managment of metabolic acidosis?
|
treat underlying disorder
|
|
|
|
What is the clinical presentation of metabolic acidosis?
|
dependent on underlying cause
compensatory hyperventilation kussmaul breathing if severe |
|
|
|
What is the diagnostic workup of metabolic alkalosis?
|
ABG:
pH increased HCO3- increased PCO2 increased due to compensation urine Cl- to differentiated between saline-responsive (<25mEg/L) and saline-unresponsive (>40 mEq/L) |
|
|
|
*What is the etiology of metabolic alkalosis?
|
initiation factors: generation of HCO3-
maintenance factors: renal conservation of HCO3- |
|
|
|
What is the clinical presentation of metabolic alkalosis?
|
no characteristics symptoms or signs
hypotension concomitant hypokalemia may cause weakness and hyporeflexia |
|
|
|
What is the management of metabolic alkalosis?
|
1. if mild → well tolerated
2. if severe (>7.40) or symptomatic → urgent treatment 3. if saline responsive → correct extracellular volume deficit with saline 4. if non-saline responsive → dependent on cause |
|
|
|
Compare acid-base disorders.
|
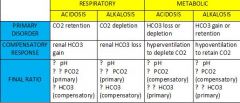
|
|
|
|
What is respiratory acidosis?
|
when lungs fail to adequately excrete CO2 → increasing [CO2]
|
Lab p179
|
|
|
What is respiratory alkalosis?
|
when lungs excessively excrete CO2 → decreasing [CO2]
|
Lab p179
|
|
|
What is metabolic acidosis?
|
deficiency in HCO3-
|
Lab p179
|
|
|
What is metabolic alkalosis?
|
excess of HCO3-
|
Lab p179
|
|
|
What is the ddx for respiratory acidosis?
|
results from hypoventilation
COPD kidney failure → decreased HCO3- causes increased H+ severe diarrhea → loss of HCO3- diabetic ketoacidosis drug overdose → aspirin, narcotics |
|
|
|
What is the clinical presentation of respiratory acidosis?
|
if acute → drowsiness, confusion, change in mental status, asterixis, myoclonus, increased ICP, papilledema
|
|
|
|
What is the diagnostic workup of respiratory acidosis?
|
ABG:
pH → low (acidemia) pCO2 → high serum: if chronic → hypochloremia |
|
|
|
What is the management of respiratory acidosis?
|
1. treat underlying disorder
2. if opioid overdose or no other obvious cause for hypoventilation → prescribe nalaxone |
|
|
|
What is the ddx for respiratory alkalosis?
|
results from hyperventilation
hyperventilation syndrome (anxiety) pulmonary → interstitial lung disease, pneumonia, PE, pulmonary edema hypoxia → hypotension, V/Q mismatch, anemia, high altitude CNS → trauma, infection, CVA, tumor, neurologic disease cirrhosis septicemia drugs → pregnancy (progesterone), corticosteroids, salicylates, nicotine, hypovolemia vomiting hypochloremia |
|
|
|
What is the clinical presentation of respiratory alkalosis?
|
if acute → lightheadedness, perioral numbness, parasthesias, anxiety
|
|
|
|
What is the diagnostic workup of respiratory alkalosis?
|
ABG:
pH → high (alkalemia) pCO2 → low |
|
|
|
What is the managment for respiratory alkalosis?
|
1. treat underlying cause
2. if due to hyperventilation syndrome (anxiety) → discourage breathing into paper bag → does not correct PCO2 and may decrease PO2 → instead provide reassurance or sedation → often self-limited → muscle weakness will suppress ventilation |
|
|
|
What is SpO2?
|
oxygen saturation → amount of oxygen bound to hemoglobin
|
|
|
|
What is normal SpO2?
|
95-98%
|
|
|
|
What is normal PaO2?
|
80-100 mmHg (at sea level)
|
|
|
|
How many O2 binding sites does a hemoglobin molecule have?
|
4
|
|
|
|
What PaO2 results indicate mild, moderate, and severe hypoxemia?
|
normal → 80-100 mmHg
mild → 60-80 mmHg moderate → 40-60 mmHg severe → <40 mmHg |
|
|
|
What is the normal range for PaCO2?
|
35-45 torr
|
|
|
|
What is the normal range for pH?
|
7.35-7.45
|
|
|
|
Interpret the following ABG results:
pH → 7.25 PO2 → 80 PCO2 → 70 HCO3- → 24 FiO2 → 21% |
pH → 7.25 → acidosis
PO2 → 80 → normal PCO2 → 70 → high = hypoventilation HCO3- → 24 → normal uncompensated respiratory acidosis |
|
|
|
What is FiO2?
|
fraction of inspired O2
FiO2 of normal room air = 21% |
|
|
|
Interpret the following ABG results:
pH = 7.26 PO2 = 70 PCO2 = 40 HCO3 = 17 |
pH = 7.26 → low → acidosis
PO2 = 70 → low → hypoxemia PCO2 = 40 → normal HCO3 = 17 → low → metabolic uncompensated metabolic acidosis with mild hypoxemia |
|
|
|
Interpret the following ABG results:
pH = 7.55 PO2 = 80 PCO2 = 25 HCO3 = 21 |
pH = 7.55 → high → alkalosis
PO2 = 80 → normal PCO2 = 25 → low → respiratory HCO3 = 21 → normal uncompensated respiratory alkalosis |
|
|
|
What is the normal range for serum HCO3-?
|
21-27
|
Interpreting Laboratory Data p182
|
|
|
Interpret the following ABG results:
pH = 7.30 PO2 = 50 PCO2 = 80 HCO3 = 37 |
pH = 7.30 → low → acidosis
PO2 = 50 → low → moderate hypoxemia PCO2 = 80 → high → respiratory HCO3 = 37 → high → compensating partially compensated (pH not normal) respiratory acidosis with moderate hypoxemia |
|
|
|
COPD can result in respiratory acidosis because?
|
COPD associated with chronic CO2 retention
|
|
|
|
What are the steps for interpreting a ABG?
|
acidosis or alkalosis?
respiratory or metabolic? if metabolic acidosis → anion gap or normal anion gap? uncompensated, partially compensated, or compensated (mixed)? mild, moderate, or severe hypoxemia? |
|
|
|
Describe diabetic nephropathy.
|
history of DM → typically 10 years
albuminuria followed by decreased GFR renal biopsy other end-organ damage → diabetic retinopathy |
|
|
|
What is the pathophysiology of diabetic nephropathy?
|
normally all glucose reabsorped by kidney
if uncontrolled DM → hyperglycemia → more glucose filtered than can be reabsorbed (glucose is dependent on secondary active tranport which is limited by saturation) → glycosuria diffuse or nodular glomerulosclerosis |
|
|
|
What is the risk of diabetic nephrophathy?
|
if type I DM → 30-40% after 20 years
if type II DM → 15-20% after 20 years |
|
|
|
What is amyloidosis?
|
disorder characterized by abnormal deposition of amyloid protein into various tissues or organs
|
|
|
|
Discuss the renal involvement in amylodisis.
|
amyloid proteins deposited into kidneys
can be primary renal amyloidosis or secondary amyloidosis primary occurs in older age groups, has benign urinary sediment, and degree of proteinuria not associated with extent of renal lesions enlarged kidneys biopsy primary progresses to ESRD in 2-3 years few treatment options → prednisone, melphalan, stem cell transplant, kidney transplant |
|
|
|
diabetic nephropathy, SLE, amyloidosis: nephrotic or nephritic?
|
NEPHROTIC:
diabetic nephropathy amyloidosis NEPHROTIC & NEPHRITIC: SLE |
|
|
|
Discuss renal involvement in SLE.
|
presents as glomerular syndromes (nephritic, nephrotic, or asymptomatic kidney disease) or non-glomerular (intestial nephritis, vasculitis)
if SLE → monitor UA for hematuria and proteinuria if hematuria or proteinuria present → perform kidney biopsy treatment varies based on severity → none, immunosuppressants |
|
|
|
What are the most common pharmacologic agents associated with nephrotoxicity?
|
acetaminophen
NSAIDS → high dose ASA antibiotics → penicillins, cephalosporins, sulfonamides, vancomycin antivirals → acyclovir antifungals → amphotericin B antituberculosis → rifampin antineoplastics → cisplatin, carboplatin diuretics ACE inhibitors and ARBs allopurinol lithium contrast dye gold ethylene glycol (found in radiator fluid) |
|
|
|
What does KUB stand for?
|
kidneys ureters bladder xray
|
|
|
|
What is another name for a plain abdominal xray?
|
KUB
|
|
|
|
What does IVP stand for?
|
intravenous pyelogram
|
|
|
|
What are the contraindications for IVP?
|
increased risk of acute kidney injury → DM with serum creatinine <2 mg/dL, prerenal azotemia, severe volume contraction
chronic kidney disease multiple myeloma |
|
|
|
What is the normal range for sodium?
What are the critical values for sodium? |
normal range = 136-145 mEg/L
critical values = <125 or >155 |
Interpreting Laboratory Data p120
|
|
|
What is the normal range for potassium?
What are the critical values for potassium? |
normal range = 3.5-5.0 mEq/L
critical values = <3.0 or >6.0 |
Interpreting Laboratory Data p120
|
|
|
What is the normal range for chloride?
What are the critical values for chloride? |
normal range = 96-106 mEg/L
critical values = none |
Interpreting Laboratory Data p120
|
|
|
What is the normal range for venous total CO2 (AKA serum bicarbonate)?
What are the critical values for CO2? |
24-30 mEq/L
<15 or >40 mEq/L *this is not the same as PCO2 or aterial serum bicarbonate!!! PCO2 = 36-44 mmHg aterial serum bicarbonate = 21-27 mEq/L |
Interpreting Laboratory Data p120
Access Medicine |
|
|
How many liters of fluid do the kidneys filter per day?
How many liters of urine is excreted per day? |
180L filtered
1.5 L excreted as urine 99% of fluid reabsorped!!! |
Interpreting Laboratory Data p162
|
|
|
What is the normal range of serum creatinine?
|
0.7-1.5 mg/dL
|
Interpreting Laboratory Data p162
|
|
|
What is creatinine?
|
breakdown product of creatine phosphate in muscle
|
|
|
|
What is the significance of abnormal serum creatinine?
|
1. if elevated → indicates decreased GFR (if normal muscle mass + no recent meat ingestion)
2. if normal → kidney function may still be abnormal!!! 3. if decreased → cirrhosis (liver producing less creatine) → order 24-hour creatinine clearance |
Interpreting Laboratory Data p163
|
|
|
What may cause a false elevation in serum creatinine?
|
unusually large amounts of uric acid, glucose, fructose, acetone, acetoacetate, pyruvic acid, or ascorbic acid
|
Interpreting Laboratory Data p163
|
|
|
What is the patient education for collecting a clean-catch urine specimen?
|
1. wash hands
2. do not touch inside of lid or cup 3. clean self with towelette by wiping inner labia front to back if female or tip of penis if male 4. urinate into toilet then stop 5. urinate into cup until full then stop 6. finish urinating in toilet 7. place lid on tight 8. deliver to lab immediately or refrigerate |
|
|
|
What are the results for a normal urine dip?
|
specific gravity → 1.005-1.030
pH → 4.5-8.0 glucose → 0 protein → 0 to trace bilirubin → 0 urobilinogen → 0-1.0 ketones → 0 hemoglobin → 0 to trace nitrites → 0 leukocyte esterase → 0 to trace |
|
|
|
What does specific gravity measure?
|
ability of kidney to concentrate urine
results depend on hydration and kidney function |
|
|
|
What are ketones?
|
products of fatty acid and fat metabolism
|
|
|
|
Positive ketones on a urine dip may indicate?
|
starvation
diabetic ketoacidosis |
|
|
|
Abnormal urobilinogen on a urine dip may indicate?
|
INCREASED:
any condition causing increased hemolysis or bilirubin DECREASED: bile duct obstruction |
|
|
|
What is urobilinogen?
|
liver excretes conjucated bilirubin into intestinal tract where it is converted to urobilinogen
most excreted via feces some excreted via urine |
|
|
|
What happens to a urine sample that sits out too long before being tested?
|
bacteria multiply and use glucose (if present)
glucose decrease due to bacteria ketones decrease due to evaporation bilirubin and urobilinogen are oxidized due to light exposure formed elements decompose within 2 hours |
Interpreting Laboratory Data p169
|
|
|
How a urine dip performed?
|
dipstick dipped into a urine sample → chemically impregnated squares react with substances in urine → producing color-coded results
*timing is critical |
|
|
|
Positive hemoglobin on a urine dip may indicate?
|
presence of hemoglobin, RBCs, or myoglobin
|
|
|
|
What is leukocyte esterase?
|
enzyme found in certain types of WBCs → primarily PMNs
|
|
|
|
Positive leukocyte esterase on a urine dip may indicate?
|
UTI
|
|
|
|
Positive nitrite on a urine dip may indicate?
|
UTI
|
|
|
|
What may cause a false positive or a false negative nitrite on a urine dip?
|
false positive → strip exposed to air
false negative → infection with non-nitrite producing organisms (Enterococcus, Streptococcus faecalis) |
|
|
|
What organisms convert nitrate to nitrite?
|
E. coli
Klebsiella Enterobacter Proteus Staphylococcus Pseudomonas |
|
|
|
List the collection requirements for a UA.
|
1. collect midstream or via catheter
2. examine within 1 hour of collection to avoid destruction of formed elements |
|
|
|
If a urine dip is positive, what should be ordered?
|
microscopy
|
|
|
|
What is included in a urine dip?
|
specific gravity
pH hemoglobin glucose protein bilirubin ketones nitrites leukocyte esterase |
|
|
|
What is included in a urine microscopy?
|
RBCs
WBCs epithelial cells casts → RBC, WBC, granular, hyaline, waxy crystals → calcium oxalate, calcium phosphate, uric acid, struvite, cystine microorganisms |
|
|
|
UA revealing heavy proteinuria and lipiduria indicates?
|
nephrotic syndrome
|
|
|
|
What is found in a UA associated with glomerulonephritis?
|
hematuria
dysmorphic RBCs RBC casts proteinuria |
Current ch
|
|
|
What is found in a UA associated with acute tubular necrosis?
|
pigmented (muddy brown) granular casts
renal tubular epithelial cells and casts |
|
|
|
What is found in a UA associated with interstitial nephritis or pyelonephritis?
|
RBCs
WBCs WBC casts small proteinuria |
|
|
|
What is the ddx for proteinuria?
|
1. functional → benign
exercise acute illness orthostatic proteinuria 2. overload → overproduction of circulating filterable plasma proteins hemoglobinuria → hemolysis myoglobinuria → rhabdomyolysis Bence Jones proteins → multiple myeloma 3. glomerular → desctruction of epithelial cell foot processes → abnormal glomerular permeability → increased filtration of normal plasma proteins → urine protein electrophoresis reveals large increase in albumin 4. tubular → decreased reabsorption of normal plasma proteins at proximal tubule acute tubular necrosis acute interstitial nephritis aminoglycoside toxicity lead toxicity hereditary metabolic disease → Wilson, Fanconi |
|
|
|
What type of protein is detected via a urine dip?
|
albumin
*add sulfosalicyclic acid to detect positively charged light chain immunoglobulins → if precipitation occurs they are present |
|
|
|
What 24 hour urine protein result is indicative of glomerular proteinuria?
|
>1g
|
|
|
|
What 24 hours urine protein result is indicative of proteinura in adults?
|
150-160mg
|
|
|
|
What is the initial approach to evaluating proteinuria?
|
1. urine dip
2. random urine protein-creatinine ratio or 24-hour urine protein (random urine easier with less chance of patient collection error) 3. possible kidney biopsy (more likely if acute) |
|
|
|
What are the results for a normal 24-hours urine protein?
|
<150-160mL
|
|
|
|
What are the results for a normal random urine protein-creatine ratio?
|
<0.2mL
*which corresponds to 200mL/24 hours |
|
|
|
When is hematuria significant?
|
>3 RBCs per high power field on at least 2 occasions
|
|
|
|
False-positive hematuria on a urine dip can be caused by?
|
myoglobin
HCL beets rhubard oxidizing agents bacteria so always follow abnormal dip with micrcospy! |
|
|
|
Transient hematuria common, true or false?
|
true
more concerning in >40y/o due to increased risk of malignancy |
|
|
|
What is the ddx for hematuria?
|
RENAL:
glomerular → IgA nephropathy, thin GBM disease, membranoproliferative glomerulonephritis, systemic nephritis syndromes extraglomerular → cysts, calculi, intestitial nephritis, renal neoplasia EXTRARENAL: urologic cancer |
|
|
|
What is the ddx for bland urinary sediment?
|
prerenal
postrenal chronic kidney disease |
|
|
|
What is the ddx for casts?
|
RBC casts → glomerulonephritis
WBCs casts → pyelonephritis, interstitial nephritis tubular epithelial casts → acute tubular necrosis, interstitial nephritis granular casts → acute tubular necrosis waxy casts → chronic kidney disease hyaline casts → concentrated urine, post-exericse, febrile disease, diuretic therapy |
|
|

RBC casts indicate?
|
glomerulonephritis
vasculitis → wegener's, polyarteritis nodosa autoimmune → SLE endocarditis renal infarction sickle cell anemia |
|
|
|
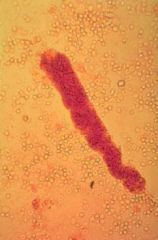
RBC cast → glomerulonephritis
|
|
|

|
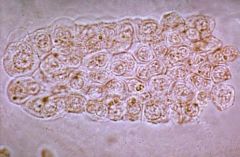
pigmented (muddy brown) granular cast → acute tubular necrosis
|
|
|

Pigmented (muddy brown) granular casts indicate?
|
acute tubular necrosis
|
|
|
|
Hyaline casts indicate kidney disease, true or false?
|
false
ddx includes concentrated urine, post-exericse, febrile disease, diuretic therapy |
|
|
|
Waxy casts indicate?
|
chronic kidney disease → indicates stasis in enlarged collecting tubules
|
|
|
|
renal tubular epithelial cell cast → acute tubular necrosis, interstitial nephritis
|
|
|
|
What is cystourethroscopy (AKA cystoscopy)?
|
cystoscope inserted into into urethra in order to view inside of urethra and bladder
takes 10-40 minutes must urinate before procedure local anesthesia given urine sample taken bladder inflated with sterile water stones removed biopsy taken low risk adverse effects following procedure include burning on urinination, hematuria |
|
|
|
Describe broad casts.
|
granular or waxy
wider than other types of casts form in large nephron tubules with little flow indicative of advanced renal failure |
|
|
|
What do broad casts indicate?
|
renal failure
|
|
|
|
What is PSA?
|
tumor marker for prostate cancer
|
Interpreting Laboratory Data p42
|
|
|
What produces PSA?
|
glandular epithelial cells of the prostate
|
Interpreting Laboratory Data p42
|
|
|
What are the normals for PSA?
|
<4 ng/mL
|
Interpreting Laboratory Data p42
|
|
|
What are the side effects of treating prostate cancer with leuprolide?
|
leuprolide is a LH-releasing hormone analog where persistent use down-regulates LHRH receptors, causing less LH secretion, causing less testosterone synthesis, causing decreased libido and ED
|
Interpreting Laboratory Data p42
|
|
|
What does CFU stand for?
|
colony forming unit
|
|
|
|
What are the 6 functions of the kidneys?
|
1. regulation of water and eletrolyte balance
2. excretion of metabolic waste, hormones, drugs 3. regulation of BP 4. regulation of RBC synthesis 5. regulation of vitamin D synthesis 6. gluconeogenesis |
|

