![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
462 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is rheumatic fever?
|
complication of strep throat or scarlet fever
|
|
|
|
What type of disease is mumps?
|
parotitis
|
|
|
|
What is the etiology of rheumatic fever?
|
strep throat
scarlet fever uncommon in United States |
|
|
|
Define exanthem?
|
generalized skin rash; caused by infectious disease, autoimmune disease, or drugs/toxins
|
|
|
|
What is the clinical presentation of rheumatic fever?
|

recent infection
fatigue fever erythema marginatum → erythematous rings mostly on trunk that disappear and reappear over weeks to months subcutaneous nodules → small painless nodules on extensor surfaces chorea → abrupt nonrhythmic involuntary movements and muscular weakness carditis polyarthritis |
|
|
|
What is the etiology of mumps?
|
caused by a paramyxovirus; spread via respiratory droplets; usually affects unimmunized children
|
Current p1250
|
|
|
What is the diagnostic workup of rheumatic fever?
|
↑ ESR
↑ CRP ↑ ASO → repeat in 10-14 days if normal ↑ PR interval on EKG → repeat in 2 weeks and 2 months if abnormal also order: CBC BC if febrile throat culture CXR echocardiogram → repeat in 1 month if negative |
Current
Harrisons |
|
|
Define enathem?
|
mucosal membrane rash; often accompanying an exanthem
|
|
|
|
What is the diagnostic (Jones) criteria of rheumatic fever?
|
recent strep throat + 2 major criteria or 1 major and 2 minor criteria
Major: erythema marginatum subcutaneous nodules pericarditis, myocarditis, or endocarditis polyarthritis chorea Minor: hx of rheumatic fever or rheumatic heart disease fever arthralgias ↑ ESR ↑ CRP ↑ ASO ↑ PR interval on EKG |
Current EMED ch19
|
|
|
What is the clinical presentation of mumps?
|

incubation 2-3 weeks before onset
fatigue and fever → variable parotid gland enlargement → unilateral or bilateral, usually one enlarges before the other stenson's duct → erythematous, edematous with yellow secretions parotid tenderness facial edema +/- trismus +/- submaxillary and sublingual gland involvement |
Current p1250
|
|
|
What is the most common symptom of rheumatic fever?
|
arthritis
|
|
|
|
What is pericarditis?
|
inflammation of the pericardium
|
|
|
|
What is the diagnostic work-up of mumps?
|
usually diagnosed clinically; swab parotid duct for confirmation via NAAT (more sensitive), viral culture or serum IgM
|
Current p1250
|
|
|
What is the etiology of pericarditis?
|
infection → cocksackieviruses, echoviruses
inflammation in lung or myocardium post MI post cardiac surgery hemopericardium uremia autoimmune disease → RA, SLE neoplasm → lung, breast, renal cell carcinoma, Hodgkin disease, lymphoma drug toxicity → penicillins, clozapine, minoxidil radiation |
Current ch10
|
|
|
List 8 diseases caused by protoza.
|
giardiasis
amoebiasis trichomoniasis toxoplasmosis malaria cryptosporidiosis leishmaniasis sleeping sickness |
|
|
|
What is the diagnostic workup of pericarditis?
|
↑ elevated ESR
EKG → diffuse ST segment elevation, often PR depression, sometimes T wave inversion CXR → often normal, possible cardiac enlargement if fluid present, R/O extracardiac disease |
Current ch10
|
|
|
What are the complications of mumps?
|
pancreatitis →affects children; upper abdominal pain, nausea, vomiting
orchitis → affects 25-40% postpubertal men, high fever, testicular swelling and tenderness oophoritis → affects 5% of postpubertal women, lower abdominal pain, ovarian enlargement meningitis → high fever, headache, stiff neck, lethargy rarely nerve deafness, myocarditis, facial paralysis, transvere myelitis, hydrocephalus, aquaductal stenosis |
Current p1250
Current Peds |
|
|
What is the most common cause of pericarditis?
|
viral infection
usually cocksackieviruses and echoviruses sometimes influenza, varicella, mumps, EBV, hepatitis, or HIV rarely TB or bacterial → pneumococci from lung infection or borrelia burgdorferi from lyme disease |
Current ch10
|
|
|
Define bacteremia.
|
bacteria in blood
|
|
|
|
Describe the EKG often found in pericarditis.
|
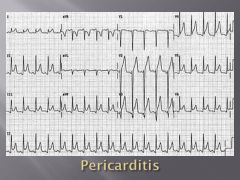
diffuse ST segment elevation
possible PR segment depression |
Current ch10
|
|
|
Mumps is the most common cause of what disease in children?
|
pancreatitis
|
Current p1250
|
|

|
pericardial effusion
|
Current ch10
|
|
|
Define cellulitis.
|
diffuse inflammation of connective tissue
|
|
|
|
What are the characteristics of a pericardial friction rub?
|
high frequency → use diaphragm
scratching, grating, squeaking sound 3 components → 1 systolic sound between S1 and S2 + 1 diastolic sound during early diastole + 1 diastolic sound during late diastole loudest at lower left sternal border, during inspiration sometimes better detected during forced expiration while leaning forward |
|
|
|
What is the management of mumps?
|
Symptomatic:
1. analgesics 2. fluids 3. topical compresses 4. bed rest until afebrile 5. isolation until swelling subsides infectious 1-2 days prior to onset of symptoms and 5 days afterward |
Current p1250
|
|
|
Blank
|
pericardial friction rub
|
|
|
|
What is the diagnostic-workup for bacteremia?
|
BC x 2
|
|
|
|
What is the management for pericarditis?
|
1. if viral → symptomatic treatment
-aspirin 650mg every 3-4 hours or indomethacin -if unresponsive → corticosteroids x 2 weeks -may recur or be complicated by cardiac tamponade 2. if post-MI or cardiac surgery → symptomatic treatment -aspirin 650mg every 3-4 hours x 2-4 weeks -if severe → corticosteroids -to prevent recurrences → colchicine x few months |
Current ch10
|
|
|
What is the prevention of rubeola, mumps, rubella, and varicella?
|
MMRV vaccine at 12-15 months and 4-6 years
|
Current 1249
|
|
|
What is rheumatic heart disease?
|
condition characterized by damaged heart valves due to rheumatic fever
|
|
|
|
Define myositis.
|
inflammation of muscle
|
|
|
|
What is the management of rheumatic fever?
|
1. for strep throat → benzathine penicillin G 1.2 million units IM single dose
2. if penicillin allegy → erythromycin 40mg/kg daily 3. for fever and arthritis → aspirin 4. if refractory to aspirin → corticosteroids 4. bed rest until afebrile and resting HR, ESR, and EKG normal 5. to prevent recurrence → benzanthine penicillin G 1.2 million units IM every 4 weeks -if no carditis → continue until 21 y/p -if carditis + no valvular damage → continue for 10 years -if carditis + valvular damge → continue for 10 years or until 40y/o if high risk for reexsposure of strep throat (parent, teacher, medical professional, military personnel) If chorea: 1. provide calming environment 2. medications only control symptoms but do not alter duration or outcome 3. carbamazepine → may not see effect for 2 weeks, continue for 2 weeks after symptoms subside If HF: see HF management |
Current ch10
|
|
|
What is the prevention of rubeola, mumps, rubella, and varicella?
|
MMRV vaccine at 12-15 months and 4-6 years
|
Current 1249
|
|
|
Who is most commonly affected by rheumatic fever?
|
children 5-15y/o
|
Current ch10
|
|
|
Define fasciitis.
|
inflammation of fascia
|
|
|
|
What is the clinical presentation of rheumatic heart disease?
|
history of rheumatic fever → may be single attack or repeated attacks
damage to valve cusps, commissures, and chordae tendineae → stenosis and/or insufficiency 50-60% → mitral valve 20% → mitral and aortic valves 10% → mitral and/or aortic + tricupsid valves |
Current ch10
|
|
|
What is herpangina?
|
viral infection of the mouth
|
|
|
|
What are the complications of rheumatic fever?
|
1. CHF
2. rheumatic heart disease 3. myocardial involvement 4. arrhythmia 5. pericardial effusion 6. rheumatic pneumonitis |
Current ch10
|
|
|
What are characteristics of anaerobic infections?
|
polymicrobial
malodorous infected tissue and pus abscess formation |
Current p1321
|
|
|
What valve is most commonly affected in rheumatic heart disease?
|
mitral valve
|
Current ch10
|
|
|
What is the etiology of herpangina?
|
caused by coxsackieviruses; spread via respiratory droplets or fecal-oral; usually affects infants and young children in summer
|
|
|
|
What are the complications of rheumatic heart disease?
|
endocarditis
|
|
|
|
Animal membrane condoms do not protect against?
|
HIV
|
|
|
|
What is the clinical presentation of pericarditis?
|
fever
dyspnea anterior pleuritic chest pain → worse when supine, relieved when upright may radiate to neck, shoulders, back, or epigastrium pericardial friction rub |
|
|
|
What is the clinical presentation of herpangina?
|

high fever; sore throat, dysphagia, and loss of appetite; red macules → vesicles → ulcerations with white-grey base and red border, located on soft palate or tonsillar pillars
|
|
|
|
What makes up the lymphatic system?
|
lymph fluid, lymph collecting ducts, lymph nodes, adenoids, tonsils, thymus, lung mucosa, stomach mucosa, peyers patches, spleen, bone marrow
|
|
|
|
What is the management and patient eduction for herpangina?
|
1. self-limiting → usually resoves in 1 week
2. take acetominophen or ibuprofen for fever and discomfort (avoid aspirin) 3. increase fluids 4. eat cold non-irritating diet → milk, icecream, popsicles 5. avoid citrus, fried, spicy, and hot food |
|
|

|

|
|
|
|
What is the prevention for herpangina?
|
handwashing
|
|
|
|
What lymph nodes should be examined during the lymphatic exam?
|
preauricular
postauricular suboccipital tonsillar submandibular submental anterior cervical chain posterior cervical chain supraclavicular infraclavicular axillary epitrochlear inguinal femoral |
|
|
|
How do you differentiate oral candidiasis from oral leukoplakia?
|
candidiasis will wipe off (and bleed when scraped) while leukoplakia will not
|
|
|
|
Define lymphadenopathy.
|
enlarged lymph node(s)
|
|
|
|
What is oral candidiasis?
|
yeast infection of the mouth
|
|
|
|
Define lymphadenitis.
|
inflammation of lymph nodes
|
|
|
|
What is the etiology of oral candidiasis?
|
caused by yeast Candida albicans; commonly associated with dentures, dibilitation, anemia, DM, HIV, broad-spectrum antibiotics, corticosteroids, chemotherapy, radiation therapy
|
|
|
|
Define lymphangitis.
|
inflammation of lymph vessels
|
|
|
|
What is the clinical presentation of oral candidiasis?
|

white curd-like patches overlying erythematous mucosa; painful; removable
*angular cheilitis is another manifestation of candidiasis |
|
|
|
Define lymphedema.
|
swelling due to obstruction of lymph nodes/vessels resulting in accumulation of lymph fluid
|
|
|
|
What is the diagnostic workup of oral candidiasis?
|

1. KOH → reveals pseudohyphae
2. HIV if no other explainable cause |
|
|
|
What is giardiasis?
|
protozoal infection of upper small intestine
|
Current p1371
|
|
|
What is the management of oral candidiasis?
|
1. prescribe antifungal, either fluconazole 100mg/d x 7-14 days, ketoconazole 200-400mg/d x 7-14 days (take with breakfast), clotrimazole troches, nystatin vaginal troches, or mouth rinses
2. for local relief, half-strength hydrogen peroxide mouth rinses or 0.12% chlorhexidine 3. if dentures, prescribe nystatin powder applied to dentures 3-4x daily x several weeks 4. if HIV, prescribe longer course of antifungal 3. if refractory, prescribe itraconazole 200mg PO daily |
|
|
|
What is the etiology of giardiasis?
|
caused by parasite protozoa giardia lamblia; spread via fecal-oral route (contaminated water), person-to-person contact, or anal-oral sexual contact
|
Current p1371
|
|
|
What is the clinical presentation of giardiasis?
|
acute diarrhea → profuse, watery
chronic diarrhea → greasy, malodorous no blood, mucus, or pus fatigue, nausea, abdominal cramps, bloating, flatulence, anorexia no fever or vomiting |
Current p1371
|
|
|
What is the diagnostic work-up of giardiasis?
|
O&P
giardia antigen |
Current p1372
|
|
|
What are the complications of giardiasis?
|
vitamin deficiencies due to malabsorption
anorexia |
Current p1372
|
|
|
What is the management of giardiasis?
|
1. metronidazole or tinidazole
2. testing and treatment of household and daycare contacts |
Current p1372
|
|
|
What is the prevention for giardiasis?
|
1. if daycare → frequent handwashing, proper diaper disposal
2. if traveling → boil water for 1 minute or filter water with pore <1 micrometer |
Current p1372
|
|
|
What is the etiology of typhoid fever?
|
usually caused by bacteria salmonella typhi; spread via ingestion of contaminated water or food
|
Current p1312
|
|
|
What is the clinical presentation of typhoid fever?
|
pea soup diarrhea
rose spots → 2-3mm pink papules, fade with pressure, usually located on trunk Early: fatigue, fever, HA, sore throat, cough, constipation then diarrhea Later: bradycardia, abdominal distension and tenderness, splenomegaly, rose spots |
|
|
|
What is the diagnostic work-up for typhoid fever?
|
BC → positive within 1 week of ingestion in 80% of patients if no antibiotics given
*stool culture unreliable |
|
|
|
What disorder is characterized by "pea soup" diarrhea?
|
typhoid fever
|
Current p1312
|
|
|
What disorder is characterized by "rose spots"
|
typhoid fever
|
Current p1313
|
|
|
What are the complications of typhoid fever?
|
intestinal hemorrhage
intestinal perforation |
Current p1313
|
|
|
What is the management of typhoid fever?
|
Depending on patient's condition:
1. ciprofloxacin 750mg PO 2x daily x 5-7 days 2. ceftriaxone 2g IV x 7 days 3. fluids 4. lytes |
|
|
|
What is the prevention of typhoid fever?
|
1. multi-dose oral vaccination or single-dose parenteral vaccination
2. consider if household typhi carrier, traveling to endemic areas, or endemic outbreak 3. not always effective 4. adequate handling of water, food, and waste |
Current p1313
|
|
|
What is the prognosis for typhoid fever?
|
carrier state may occur
2% mortality rate in treated cases, especially if elderly, disabled, or complications 15% reoccurence |
Current p1313
|
|

|
rose spots → typhoid fever
|
|
|
|
What is included in a stool culture?
|
campylobacter
salmonella shigella |
|
|
|
What is the patient education for infectious diarrhea?
|
do not take anti-diarrheal medications; may worsen disease by not allowing body to rid itself of infection via diarrhea
|
|
|
|
What disorder is characterized by "rice water" diarrhea?
|
cholera
|
Current p1315
|
|
|
What is the etiology of cholera?
|
caused by vibrio cholerae toxin; spread via ingestion of contaminated water or food; associated with poor sanitation
|
Current p1315
|
|
|
What is the clinical presentation of cholera?
|
rice water diarrhea → sudden onset, severe, frequent, watery, gray, turbid
no blood, pus, or odor no fever |
Current p1315
|
|
|
What is the diagnostic work-up of cholera?
|
stool culture
|
Current p1315
|
|
|
What are the complications of cholera?
|
dehydration → hypotension/hypovolemia → death
|
Current p1315
|
|
|
What is the prevention of cholera?
|
1. cholera vaccinaton
2. 2 doses 1-4 weeks apart if traveling to endemic area 3. booster every 6 months if living in endemic area 3. short-lived, limited immunity 4. establish clean water and proper waste disposal |
Current p1315
|
|
|
What is the management of cholera?
|
1. if moderate to mild → oral rehydration solution (1 liter water, 1 tbsp sugar, 1 tsp salt)
2. if severe → IV fluids (lactate ringer) 3. azythromycin → 1g PO (may speed recovery but beware of resistance) |
Current p1315
|
|
|
What is the etiology of enterohemorrhagic e. coli gastroenteritis (EHEC)?
|
caused by enterohemorrhagic e. coli shiga-like toxin; spread by ingestion of contamined food (unpasteurized apple juice, undercooked hamburger); usually affects children or elderly; THINK JACK IN THE BOX FOOD POISENING
|
Current p1315
|
|
|
What is the clinical presentation of EHEC?
|
bloody diarrhea (though can be non-bloody)
|
Current p1315
|
|
|
What is the diagnostic work-up of EHEC?
|
E coli O157:H7
|
Current p1315
|
|
|
What is the management of EHEC?
|
1. symptomatic only
2. antibiotics may increase risk of HUS or worsen HUS |
Current p1315
|
|
|
What are the complications of EHEC?
|
HUS
TTP |
|
|
|
List infectious diarrhea manifestations and their associated causes?
|
rice water diarrhea → cholera
pea soup diarrhea → typhoid fever bloody diarrhea → salmonella, EHEC bloody mucous diarrhea → shigella |
|
|
|
What is the etiology of salmonella?
|
caused by salmonella (but not salmonella typhi); spread via ingestion of contaminated water or food; think FOOD POISENING
|
Current p1314
|
|
|
What is the clinical presentation of salmonella?
|
onset 8-48hr following ingestion; fever, chills, nausea, vomiting, cramping abdominal pain, bloody diarrhea
|
Current p1314
|
|
|
What is the diagnostic work-up for salmonella or shigella?
|
stool culture
|
Current p1314
|
|
|
What is the management of salmonella?
|
1. if uncomplicated → symptomatic only
2. if severely ill, malnourished, sickle cell disease or HIV → trimethoprim-sulfamethoxazole, ampicillin, or ciprofloxacin |
Current p1314
|
|
|
What are the complications of salmonella?
|
bacteremia localized in joints or bones, especially if sickle cell disease present
|
Current p1314
|
|
|
What is the etiology of traveler's diarrhea?
|
diarrhea acquired while traveling; common if changes in climate, social conditions, and sanitation standards; associated with unusual food and drink, changes in living habits, and changes in bowel flora
Most common causes: 1. enterotoxigenic E. coli 2. campylobacter jejuni 3. shigella Other causes: 1. salmonella 2. giardia lamblia 3. noncholera vibriones 4. aeromonas hydrophila 5. entameba histolytica 6. rotaviruses 7. adenoviruses |
Current p1174
|
|
|
What is the clinical presentation of traveler's diarrhea?
|
nausea, cramping abdominal pain, diarrhea
if ETEC → watery diarrhea, no fever if cambylobacter, shigella, or salmonella → fever, bloody diarrhea |
Current p1174
|
|
|
What is the management of traveler's diarrhea?
|
1. self-limiting within 1-5 days
2. oral rehydration solution 3. if non-bloody diarrhea → loperamide + ciprofloxacin 4. if bloody diarrhea or refractory to antibiotics → azythromycin 5. if bloody diarrhea → do not take loperamide which is an antimotility drug |
Current p1174
|
|
|
What are the complications of traveler's diarrhea?
|
increases risk of IBS
|
Current p1174
|
|
|
What is the prevention of traveler's diarrhea?
|
1. prescribe antimicrobials to be taken if diarrhea develops
3. prophylaxis if significant underlying disease 4. avoid fresh foods and water sources likely to be contaminated |
Current p1174
|
|
|
What is the diagnostic work-up of traveler's diarrhea?
|
if fever + bloody diarrhea or refractory to antibiotics → stool culture
|
Current p1174
|
|
|
What are the 3 most common causes of traveler's diarrhea?
|
ETEC, campylobacter jejuni, shigella
|
Current p1174
|
|
|
What are the indications for prescribing loperamide (Imodium)?
|
anti-diarrheal
*do not prescribe if bloody diarrhea |
|
|
|
What is dysentary?
|
group of disorders characterized by inflammation of the intestine + severe diarrhea containing blood and/or mucous
|
|
|
|
Compare inflammatory and non-inflammatory diarrhea.
|
Inflammatory:
1. involves bacteria, parasites, or toxins that are invasive 2. causes include invasive E. coli, EHEC, campylobacter, salmonella, shigella, entamoeba histolytica, yersinia, cdif 3. involves colon 4. small-volume bloody diarrhea 5. fever, abdominal cramps, fecal urgency, tenesmus 6. severe Non-inflammatory: 1. involves viruses and toxins that interfere with salt and water balance 2. causes include rotavirus, norwalk virus, enteric adenoviruses, ETEC, cholera, giardia 3. involves small intestine 4. large-volume watery diarrhea 5. nausea, vomiting, abdominal cramps 6. mild |
Current p1172
|
|
|
What is the etiology of viral gastroenteritis?
|
causes include rotavirus, norwalk virus, enteric adenoviruses, astrovirus, coronaviris; spread via ingestion of contaminated water or food; common among children, elderly, immunosuppressed
|
|
|
|
What is the common name for viral gastroenteritis?
|
stomach flu
|
|
|
|
What is the clinical presentation of viral gastroenteritis?
|
onset within 4-48hr of ingestion; nausea, vomiting, abdominal cramps, large-volume watery diarrhea
|
|
|
|
What is the diagnostic work-up of viral gastroenteritis?
|
usually not indicated
rotavirus if severe illness in child |
|
|
|
What is the most common cause of severe diarrhea in children?
|
rotovirus
|
|
|
|
Norwalk virus is associated with outbreaks on _?
|
cruise ships
|
|
|
|
What is the management of viral gastroenteritis?
|
1. self-limiting
2. rehydration via oral solution or IV fluids |
|
|
|
What is the prevention of rotavirus?
|
vaccination
|
|
|
|
What are the complications of viral gastroenteritis?
|
dehydration → death, especially in young children
|
|
|
|
What is hemolytic uremic syndrome (HUS)?
|
disorder characterized by thrombocytopenia, microangiopathic hemolytic anemia, and renal failure
|
|
|
|
What is the etiology of HUS?
|
associated with E. coli 0157:H7 → produces shiga-like toxin → damages endothelial cells → causing thrombus formation → platelet aggregation → thrombocytosis + microangiopathic hemolytic anemia; commonly affects children
|
|
|
|
What is the clinical presentation of HUS?
|
influenza-like or GI prodrome
bloody diarrhea hematuria oliguria actue renal failure (because kidneys require high volume of blood flow) |
|
|
|
What is the diagnostic work-up of HUS?
|
CBC → anemia, thrombocytopenia
RETIC → high blood smear → schistocytes indirect BILI → high LD → high CREAT → high PT → normal PTT → normal bleeding time → prolonged E. coli O157:H7 → positive |
|
|
|
What are the complications of HUS?
|
permanent kidney damage
death |
|
|
|
What is the managment of HUS?
|
1. hospitalize → observe
2. supportive care 3. dialysis if necessary 4. antibiotics and platelet transfusions contraindicated |
|
|
|
Candida albicans is part of normal flora, true or false?
|
true
found in oropharynx, large intestine, and vagina |
|
|
|
What are clue cells?
|
epithelial cells coated by Gardnerella vaginalis
indicative of bacterial vaginosis |
|
|
|
VULVOVAGINAL CANDIDIASIS
|
ETIOLOGY:
caused by candida albicans (90%) may be associated with pregnancy, obesity, systemic disorder (DM, HIV), medication (antibiotics, corticosteroids, oral contraceptives), chronic debilitation occurs in 75% of women CLINICAL PRESENTATION: severe vulvar pruritis vulvar erythema white cottage-cheesy vaginal discharge +/- burning following urination +/- labia minora erythema, excoriation, edema if affecting skin adjacent to labia, think DM or other systemic illness DIAGNOSTIC WORKUP pH normal (≤4.5) wet mount (KOH) → pseudohyphae fungal culture MANAGEMENT: 1. treat only if symptomatic 2. d/c antibiotics if possible 3. control underlying disease 4. avoid nonabsorbent undergarments 5. avoid douching |
|
|
|
BACTERIAL VAGINOSIS
|
ETIOLOGY:
altered vaginal flora (decreased lactobacilli + overgrowth of Gardnerella vaginalis, Mobiluncus, Prevotella, Porphyromonas, Bacteroides, Peptostreptococcus) CLINICAL PRESENTATION: grayish-white vaginal discharge fishy odor (more noticeable following unprotected intercourse) non-irritating DIAGNOSTIC WORKUP: pH 5.0-5.5 whiff test positive (fishy odor following application of KOH) wet mount → clue cells, ↓ lactobacilli, few WBCs gram stain → lots of small gram-negative bacteria, few lactobacilli *gram stain more sensitive (93%) and specific (70%) than wet mount MANAGEMENT: treat symptomatic patients and consider treating asymptomatic patients IF NON-PREGNANT: Options include: 1. metonidazole 2g PO single dose 2. metronidazole 500 mg PO twice daily x 5 days 3. clindamycin 300 mg PO 2x daily x 7 days 4. metronidazole gel 0.75% (1 full applicator, 5g) intravaginally once or twice daily x 5 days 5. clindamycin cream 2% (1 full applicator, 5g) intravaginally at bedtime x 7 days 6. clindamycin ovules 100g intravaginally at bedtime x 3 days 7. inform patients that condoms or diaphragms may be weakened during treatment with clindamycin cream since it is oil-based IF PREGNANT: Options include: 1. metronidazole 250mg PO 3x daily x 7 days 2. clindamycin 300 mg PO 2x daily x 7 days 3. do not use topical agents COMPLICATIONS: PID, post-abortion infection, post-hysterectomy vaginal cuff cellulitus PREVENTION: condoms hydrogen peroxide douches oral or vaginal application of yogurt containing lactobacillus acidophilus intravaginal planting of exogenous lactobacilli prophylaxis longer treatment periods *treatment of male does not help prevent recurrence in female MATERNAL-FETAL TRANSMISSION: BV may increase risk of preterm delivery, though treatment of asymptomatic pregnant women does not necessarily reduce risk of preterm delivery or adverse outcomes |
|
|
|
GONORRHEA
|
ETIOLOGY:
sexually transmitted infection caused by Neisseria Gonorrhoeae infects glandular structures of vulva, perineum, anus, urethra, and cervix CLINICAL PRESENTATION: symptoms range from asymptomatic (85%) to severe copious mucopurulent discharge DIAGNOSTIC WORKUP: gram stain → gram-negative diplococcic within WBCs NAAT or GCCHDNA MANAGEMENT: IF UNCOMPLICATED, options include: 1. ceftriaxone 125 mg IM single dose (3rd gen cephalosporin) 2. cefixime 400 mg PO single dose (3rd gen cephalosporin) 3. ciprofloxacin 500 mg PO single dose (2nd gen quinolone) 4. ofloxacin 400 mg PO single dose (2nd gen quinolone) 5. levofloxacin 250 mg PO single dose (3rd gen quinolone) 6. If infection acquired while in California, Asia, or the Pacific (including Hawaii) → spectinomycin 2g IM single dose (d/t cephalosporin or quinolone resistance) 7. treat for chlamydia COMPLICATIONS: salpingitis, tubo-ovarian abscess, peritonitis ectopic pregnancy, infertility PREVENTION: safe sex practices including condoms MATERNAL-FETAL TRANSMISSION: if active infection present during delivery, newborn may develop conjunctivitis |
|
|
|
CHLAMYDIA
|
ETIOLOGY:
sexually transmitted infection caused by Chlamydia Trachomatis CLINICAL PRESENTATION: may be asymptomatic dysuria post-coital bleeding mucopurulent cervicitis may present as lymphogranuloma venereum (LGV) → initially a painless, vesicular, transient lesion or shallow ulcer of vulva; retroperitoneal lymphadenopathy; may progress to genital or anal fistulas, strictures, or rectal stenosis; uncommon in U.S. but common in SE Asia and Africa DIAGNOSTIC WORKUP: NAAT or GCCHDNA MANAGEMENT: 1. treat patient and partner 2. azithromycin 1 g PO single dose 3. other options include doxycycline, erythromycin, ofloxacin, levofloxacin 4. avoid sex for 7 days 5. repeat screening 3-4 months following treatment 6. if persistent symptoms, recurrence, or pregnancy → test for cure 7. if LGV → doxycycline 100mg 2x daily x 21 days 8. treat gonorrhea COMPLICATIONS: salpingitis, tubual occlusion, ectopic pregnancy, infertility PREVENTION: screen all sexually active women safe sex practices including use of condoms MATERNAL-FETAL TRANSMISSION: neonatal conjunctivitis |
|
|
|
TRICHOMONIASIS
|
ETIOLOGY:
sexually transmitted infection caused by Trichomonas vaginalis (unicellular flagellate protozoan) infects lower urinary tract of women and men most prevalent non-viral STI in U.S. CLINICAL PRESENTATION: copious greenish-white frothy vaginal discharge vaginal wall erythema strawberry cervix +/- malodor, urinary symptoms, vulvar pruritis, labia minora edema and tenderness DIAGNOSTIC WORKUP: pH > 5.0 wet mount → motile trichomonads, ↑ PMNs *Trichomonas vaginalis are larger than PMNs but smaller than epithelial cells MANAGEMENT: 1. treat patient and partner 2. metronidazole 2g PO single dose 3. metronidazole 500mg PO 2x daily x 7 days 4. avoid alcohol to prevent severe nausea and vomiting 5. avoid sex or use condoms until treatment completed 6. if persistent symptoms → repeat metronidazole after 4-6 weeks if presence of trichomonads confirmed and WBC normal 7. if resistance → 2-4g daily x 10-14 days, consult CDC 8. evaluate for gonorrhea, chlamydia, syphilis, and HIV COMPLICATIONS: PREVENTION: safe sex practices including use of condoms use of spermicidal agents (Nonoxynol 9) MATERNAL-FETAL TRANSMISSION: increased transmission of HIV |
|
|
|
List opportunistic disorders associated with HIV.
|
Eyes:
CMV retinitis Mouth/Oral Cavity/Throat: oral hairy leukoplakia oral/esophageal candidiasis Kaposi's sarcoma Respiratory: pneumocystic pneumonia TB GI: enterocolitis Genitals: HSV vulvovaginal candidiasis Neuro: cryptococcal meningitis herpes zoster AIDs dementia complex Malignanices: cervical cancer lymphoma |
|
|
|
What body fluids can transmit HIV?
|
blood > semen > vaginal secretions > breast milk
|
|
|
|
What is the diagnostic work-up for HIV?
|
HIV for screening
western blot for confirmation |
|
|
What does this vaginal discharge indicate?
|
white curd-like discharge → vulvovaginal candidiasis
|
|
|

What does this wet mount slide indicate?
|
budding yeast (6) and pseudohyphae (7) of candida → vulvovaginal candidiasis
|
|
|
|
How do you differentiate oral candidiasis from oral leukoplakia?
|
candidiasis will wipe off (and bleed when scraped) while leukoplakia will not
|
|
|
|
What is the etiology of oral hairy leukoplakia?
|
EBV opportunistic infection in immunocompromised host (especially HIV)
|
|
|

|
oral hairy leukoplakia → consider HIV!!!
|
|
|

|
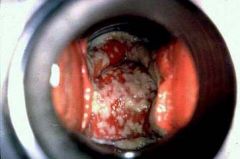
Kaposi's sarcoma + overlying oral candidiasis in HIV patient
|
|
|
|
What is oral candidiasis?
|
yeast infection of the mouth
|
|
|
|
What is the etiology of oral candidiasis?
|
caused by yeast Candida albicans; commonly associated with dentures, dibilitation, anemia, DM, HIV, broad-spectrum antibiotics, corticosteroids, chemotherapy, radiation therapy
|
|
|
|
What is the clinical presentation of oral candidiasis?
|

white curd-like patches overlying erythematous mucosa; painful; removable
*angular cheilitis is another manifestation of candidiasis |
|
|
|
What is the diagnostic workup of oral candidiasis?
|

1. KOH → reveals pseudohyphae
2. HIV if no other explainable cause |
|
|
|
What is the management of oral candidiasis?
|
1. prescribe antifungal, either fluconazole 100mg/d x 7-14 days, ketoconazole 200-400mg/d x 7-14 days (take with breakfast), clotrimazole troches, nystatin vaginal troches, or mouth rinses
2. for local relief, half-strength hydrogen peroxide mouth rinses or 0.12% chlorhexidine 3. if dentures, prescribe nystatin powder applied to dentures 3-4x daily x several weeks 4. if HIV, prescribe longer course of antifungal 3. if refractory, prescribe itraconazole 200mg PO daily |
|
|
|
What is the etiology of anthrax?
|
caused by bacillus anthracis spores; spread via contact with infected animals/hides (pigs, sheep, cows, horses, goats) or inhalation (bioterrorism)
|
Current p1300
|
|
|
What is the clinical presentation of athrax?
|
Cutaneous:
onset within 2 weeks of exposure; erythematous papule → vesicle → ulceration → necrosis → painless black eschar; fatigue, fever, HA, nausea, vomiting, regional adenopathy Inhalation: onset 10 days to 6 weeks after exposure; primary stage characterized by non-specific viral-like symptoms; chest pain → mediastinitis; altered mental status, delerium → hemorrhagic meningitis |
Current p1300
|
|
|
What is the diagnostic work-up of anthrax?
|
culture of skin lesion, blood, pleural fluid, or CSF
CXR → mediastinal widening, infiltrates or consolidation, pleural effusion |
Current p1301
|
|
|
What are the complications of anthrax?
|
Cutaneous:
possible meningitis or sepsis Inhalation: mediastinitis hemorrhagic meningitis death |
Current p1301
|
|
|
What is the prognosis for anthrax?
|
cutaneous → death extremely unlikely
inhalational → 85% mortality rate |
Current p1302
|
|
|
What is the management of anthrax?
|
1. ciprofloxacin + rifampin for treatment
2. ciprofloxacin for prophylaxis 3. report to CDC |
Current p1301
|
|
|
What is the prevention of anthrax?
|
anthrax vaccination → multiple injections over 18 months + annual booster; offered to people at high risk for exposure (miliatry personnel)
|
Current p1302
|
|

|
black eschar → cutaneous anthrax
|
|
|
|
What is the etiology of toxoplasmosis?
|
caused by protozoan toxoplasma gondii; spread via ingestion or direct inoculation
-raw or undercooked meat -water or food contaminated by cats -blood transfusion or organ transplant congenital due to infection during pregnancy reactivation due to immunocompromise |
Current p1363
|
|
|
What species house toxoplasma gondii?
|
humans
animals → especially CATS birds |
Current p1363
|
|
|
What is the prevention for toxoplasmosis?
|
avoid raw or undercooked meat
avoid contact with cat feces → do not change litter box |
Current p1365
|
|
|
What is the clinical presentation of toxoplasmosis?
|
Primary Infection:
usually asymptomatic, resembles mono when symptomatic, fatigue, fever, HA, sore throat, lymphadenopathy, myalgia, hepatosplenomegaly Congenital Infection: CNS abnormalities retinochoroiditis → presents weeks to years after infection Reactivated Infection: encephalitis pneumonitis myocarditis |
Current p1363
|
|
|
What is the management of toxoplasmosis?
|
1. if primary infection → self-limiting within few months
2. if complicated → pyrimethamine + sulfadiazine 3. folic acid to prevent bone marrow suppression 4. monitor CBC 5. if 1st trimester → spiramycin |
Current p1365
|
|
|
What is the diagnostic work-up for toxoplasmosis?
|
PCR or culture of blood, CSF, amniotic fluid, or tissue
tachyzoites indicate acute infection cysts indicate acute or chronic infection IgM and IgG -IgG present in 1-2 weeks -IgM may persist for years |
Current p1364
|
|
|
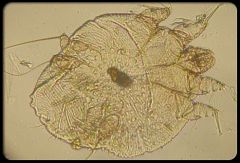
What is the common name for enterobiasis?
|
pinworms
|
|
|
|
What is the etiology of enterobiasis?
|
caused by parasitic pinworm enterobius vermicularis; spread person-to-person via ingestion of eggs after contact with contaminated hands, perianal area, food, clothing, bedding, or fomites
eggs hatch in duodenum → larvae migrate to cecum → 1 month maturation → migrate to perianal area to lay eggs at night |
|
|
|
What is the clinical presentation of enterobiasis?
|
nocturnal perianal pruritus
insomnia, restlessness, and enuresis common in children |
|
|
|
What is the diagnostic work-up of enterobiasis?
|
pinworm prep → microscopic examination for eggs
stool → gross examination for adult pinworms |
|
|
|
What are the complications of enterobiasis?
|
uncommon
|
|
|
|
What is the treatment of enterobiasis?
|
1. apply clear cellophane tape to perianal area in morning for pinworm prep
2. examine perianal area at night or gross stool for adult worms 3. albendazole 400mg PO single dose 4. repeat dose in 2 weeks due to frequent reinfection 5. treat infected family members 6. discourage perianal scratching 7. encourage handwashing, wash clothing and bedding, disinfect surfaces |
|
|
|
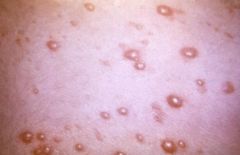
What is the etiology of scabies?
|
caused by parasitic mite sarcoptes scabiei; spread via close person-to-person contact, infected clothing and bedding
|
Current p137
|
|
|
What is the clinical presentation of scabies?
|

generalized severe pruritus and excoriation
small vesicles, pustules, and burrows located in axillae, beneath breasts, elbows, wrists, palms, feet, web spaces nodular lesions on penis and scrotum head and neck usually spared |
Current p137
|
|
|
What is the diagnostic work-up of scabies?
|
collect wet mount specimen → use No. 15 blade to scrape multiple unexcoriated lesions until they are flat; best lesions found in web spaces, wrists, elbows, or feet
wet mount → reveals ova, organism, or feces |
Current p137
|
|
|
What is the management of scabies?
|
1. apply permethrin 5% cream from neck down for 8-12 hours
2. repeat in 1 week 3. wash clothing and bedding at >60°C 4. if dermatitis → triamcinolone 0.1% cream 6. if refractory → repeat permethrin weekly for 2 weeks 7. treat close contacts |
Current p137
|
|
|
Describe scabies burrows.
|

irregular, 2-3mm long, width of hair
|
Current p137
|
|

|
pinworm eggs → enterobiasis
|
|
|

|
scabies
|
|
|

|
scabies
|
|
|

|
scabies
|
|
|
|
Describe how to collect a pinworm prep.
|

|
|
|

|
pinworms in perianal area
|
|
|
|
What is the etiology of cutaneous larva migrans?
|
usually caused by larvae of animal hookworms (especially dogs and cats); spread via migration of worms through skin; common in warm areas including SE united states; common in children
|
Current p1385
|
|
|
What is the clinical presentation of cutaneous larva migrans?
|

pruritic erythematous papules on hands and feet → serpiginous tracks
|
Current p1385
|
|
|
What is the diagnostic work-up of cutaneous larva migrans?
|
diagnosis made clinically
|
Current p1385
|
|
|
What is the management of cutaneous larva migrans?
|
1. if mild → no treatment
2. if moderate to severe → thiabendazole 10% aqueous suspension applied topically 3x daily x 5 days 3. albendazole 400mg PO 1-2x daily x 3-5 days |
Current p1385
|
|
|
What are the complications of cutaneous larva migrans?
|
2° bacterial infection of lesions
|
Current p1385
|
|
|
What disorder is characterized by serpiginous burrows?
|
cutaneous larva migrans
|
Current p1385
|
|

|
serpiginous burrow → cutaneous larva migrans
|
|
|
|
scabies
|
|
|
|
What are the indications for prescribing permethrin 5% cream?
|
scabies
|
|
|
|
What is the etiology of trichinosis?
|
caused by parasitic roundworm trichinella; spread via ingestion of undercooked meat, especially pork or game
cysts ingested → larvae released by gastric acid → migrate to small intestine → invade intestinal epithelial cells → mature into adults → release larvae → migrate to skeletal muscle via bloodstream → enlarge and form cysts |
Current p1383
|
|
|
What is trichinosis?
|
parasitic roundworm infection caused by eating undercooked meat
|
Current p1383
|
|
|
What is the clinical presentation of trichinosis?
|
Early abdominal symptoms:
vomiting, abdominal pain, diarrhea occurs within first week Later systemic symptoms: fever, periorbital edema, myalgias HA, subconjunctival and retinal hemorrhages, dyspnea, hoarseness, dysphagia, cough, petechiae or macular rash peaks within 2-3 weeks persists for 2 months |
Current p1383
|
|
|
What is the diagnostic work-up of trichinosis?
|
serum muscle enzymes → creatine kinase, LD, AST → high
serum IgM and IgG → positive ≥ 3 weeks after ingestion; rising titers highly suggestive of diagnosis |
Current p1383
|
|
|
What are the complications of trichinosis?
|
severe myalgia, edema, and weakness, especially in head and neck
myocarditis pneumonitis meningoencephalitis |
Current p1383
|
|
|
What is the management of trichinosis?
|
1. no effective therapy
2. if early → albendazole or mebendazole may limit invasion 3. if systemic → supportive therapy → antipyretics, analgesics, bed rest 4. if severe → corticosteroids |
Current p1384
|
|
|
What is the etiology of ascariasis?
|
caused by parasitic roundworm ascaris lumbricoides; spread via ingestion of eggs in contaminated food; common in areas with poor hygiene or sanitation; most common in children
larvae hatch in small intestine → penetrate to bloodstream → migrate to lungs → travel up airways and down into GI tract → mature into adults |
Current p1379
|
|
|
What is the size and lifespan of ascaris lumbricoides?
|
<40cm
1-2 years |
Current p1379
|
|
|
What is the clinical presentation of ascariasis?
|
During migration through lungs:
fever, dyspnea, nonproductive cough, chest pain, pneumonia abdominal discomfort |
Current p1379
|
|
|
What is the diagnostic work-up for ascariasis?
|
worms emerge from nose, mouth, or anus
white count → eosinophilia stool → gross examination reveals eggs |
Current p1379
|
|
|
What are the complications of ascariasis?
|
nutrional deficiencies
spread anywhere in GI tract, kidney, eye, spinal cord, brain → jaundice, obstruction, perforation, death |
Current p1379
|
|
|
What are the 2 most common causes of eosinophilia?
|
allergic reaction
parasitic infection |
|
|
|
What is the most common parasitic infection in the world?
|
ascarasis
|
|
|
|
What is the management of ascariasis?
|
albendazole 400mg PO single dose
mebendazole 500mg PO single dose |
Current p1379
|
|

|
ascariasis
|
|
|

|
ascariasis
|
|
|
|
What are the indications for prescribing albendazole or mebendazole?
|
antihelmintic
prescribed to combat worm infestations including: pinworms → enterobiasis hookworms → cutaneous larva migrans, hookworm disease roundworms → ascariasis, trichinosis tapeworms → cysticercosis |
|
|
|
What is the etiology of hookworm disease?
|
commonly caused by parasitic hookworms ancylostoma duodenale and necator americanus; spread via contact with infected soil or ingestion of larvae in food or water; common in tropical areas
penetrate skin if infected soil or ingested → penetrate bloodstream → migrate to lungs → up respiratory tract and down GI tract → invade small intestine mucosa → mature → suck blood |
Current p1381
|
|
|
What is the clinical presentation of hookworm disease?
|
pruritic maculopapular rash at site of penetration
During migration through lungs: low fever, wheezing, dry cough epigastric pain, diarrhea, anorexia |
Current p1381
|
|
|
What is the diagnostic work-up of hookworm disease?
|
CBCDP → eosinophilia, microcytic anemia
ALB → low OCCB → positive stool → eggs present |
Current p1381
|
|
|
List 12 infectious diseases that cause a rash.
|
1. varciella (chickenpox)
2. herpes zoster (shingles) 3. rubeola (measles) 4. rubella (german measles) |
|
|
|
What are the complications for hookworm disease?
|
iron deficiency anemia → pallor, weakness, dyspnea, CHF
protein malnutrition → hypoalbuminemia, edema, ascites impaired growth and cognitive development in children |
Current p1381
|
|
|
What is the common name for varicella?
|
chickenpox
|
|
|
|
What is the management of hookworm disease?
|
1. albendazole 400mg PO single dose or mebendazole 100mg 2x daily x 3 days
2. if iron deficiency anemia → ferrous sulfate 3. if severe anemia → blood transfusion |
Current p1381
|
|
|
What is etiology of varicella?
|
varicella zoster virus (VZV) AKA HHV-3
spread via respiratory droplets or lesion contact peak age 5-10 year round highly contagious |
Current p1239
|
|
|
List the categories and types of helminths and their associated diseases.
|
Nematodes:
pinworms → enterobiasis hookworms → cutaneous larva migrans, hookworm disease roundworms → ascariasis, trichinosis Cestodes: tapeworms → cysticercosis, tapeworm disease Trematodes: flukes → schistosomiasis |
|
|
|
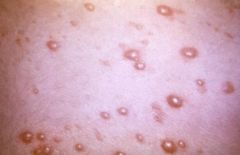
What is the clinical presentation of varicella?
|
10-21 day incubation period
1-3 day prodrome with variable symptoms (mild fatigue, fever, HA, respiratory sxs) red maculopapules → clear vesicles on erythematous base ("dew drop on a rose petal") → pustules (superficial and elliptical with serrated borders) → crusts over 5-6 days affects scalp, face and trunk → extremities lesions can also occur in nose, mouth, conjunctiva, vagina pruritis |
Current p1239
|
|

|
scabies burrow
|
|
|
|
What is the time frame for varicella lesions?
|
new lesions for 1-7 days
crusts slough in 7-10 days |
|
|
|
What is schistosomiasis?
|
parasitic fluke infection caused by fresh water exposure in endemic area
|
Current p1373
|
|
|
What is the diagnostic work-up for varicella or herpes zoster?
|
diagnosis usually made clinically; confirmation via DFA or PCR
|
Current p1241
|
|
|
What is the etiology of schistosomiasis?
|
caused by parasitic fluke schistosoma; spread via exposure to fresh water containing cercariae released by infected snails
penetration of skin or mucous membranes → migration to portal circulation → maturation → mate after 6 weeks → migration to mesenteric or bladder venules → lay eggs host reponds to eggs → inflammation → granuloma formation → fibrosis |
Current p1373
|
|
|
What are the complications of varicella?
|
pitted scars
2° bacterial skin infections → staph, group A strep |
Current p1241
|
|
|
What is the clinical presentation of schistosomiasis?
|
Acute:
fatigue, fever, HA, myalgia, cough, diarrhea, uticaria GI: fatigue, abdominal pain, diarrhea, hepatomegaly Urinary: dysuria, hematuria |
Current p1374
|
|
|
What is the management of varicella?
|
1. acetominphen for fever
2. antihistamines or cool soaks for pruritus 3. acyclovir if chronic disease or immunocompromised 3. keep fingernails short and skin clean to prevent 2° bacterial skin infections and scarring 4. bed rest until afebrile 5. isolation until crusts disappear |
Current p1242
|
|
|
What is the diagnostic work-up of schistosomiasis?
|
WBC count → eosinophilia
serology → positive urine or stool → eggs biopsy of rectum, colon, liver or bladder |
Current p1374
|
|
|
What is the prevention for varicella?
|
vaccination via VARIVAX (varicella only) or MMRV at 12-15 months and 4-6 years
|
Current p1241
|
|
|
What are the complications of schistosomiasis?
|
anemia
anorexia, weight loss growth retardation portal HTN esophageal varices pulmonary HTN hepatic failure UTI kidney disease bladder cancer |
Current p1374
|
|
|
When should the MMR and varicella vaccinations be given?
|
12-15 months and 4-6 years
|
Current p1241
|
|
|
What is the common name for rubeola?
|
measles
|
|
|
|
What is the management of schistosomiasis?
|
1. if intestinal disease → LFTs, liver imaging
2. if urinary disease → urinary system ultrasound 3. praziquantel 4. if recent → repeat praziquantel in few weeks 5. if severe → corticosteroids 6. follow-up every 3 months for 1 year for presence of eggs and retreat if necessary |
Current p1374
|
|
|
What is the etiology of rubeola?
|
caused by a paramixovirus; spread via respiratory droplets; virtually eliminated in U.S.
|
Current 1247
|
|
|
varicella
|
|
|
|
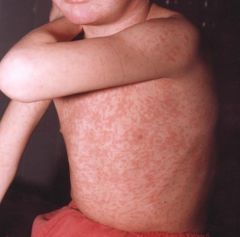
What is the clinical presentation of rubeola?
|
10-14 day incubation period for onset of rash; prodrome of fatigue, fever, conjunctivitis, photophobia, rhinorrhea, cough, Koplik spots; maculopapular rash, 3-4 days after onset of prodrome, brick-red, irregular; face → downward and outward including palms and soles
|
Current 1247
|
|
|
What is the prevention of schistosomiasis?
|
avoid fresh water exposure in endemic areas
towel vigorously after fresh water exposure in endemic areas |
Current p1374
|
|
|
What is the diagnostic work-up of rubeola?
|
usually diagnosed clinically; supported by IgM measles Ab
leukopenia |
Current 1248
|
|
|
What is the common name for herpes zoster?
|
shingles
|
|
|
|
What disease are Koplik spots associated with?
|
rubeola
|
Current 1248
|
|
|
What is the prognosis for acute schistosomiasis?
|
resolves in 2-8 weeks
|
Current p1374
|
|
|
What are Koplik spots?
|

prodromic enanthem of rubeola; resemble grains of salt on wet background; found on buccal mucosa
|
|
|
|
What is the etiology of herpes zoster?
|
varicella zoster virus (VZV) AKA HHV-3; manifests due to prior varicella + declining immunity; usually affects adults >60y/o
|
Current p1239
|
|
|
"Grains of salt on a wet background" describe?
|

Koplik spots
|
|
|
|
What is the etiology of non-invasive tapeworm infection?
|
causes include:
beef tapeworm taenia saginata pork tapeworm taenia solium fish tapeworm diphyllobothrium laturn dwarf tapeworm hymenolepis nana spread when cattle, pigs, or fish ingest human feces → humans ingest undercooked beef, pork, or fish dwarf tapeworm spread person-to-person via ingestion of food contaminated with human feces |
Current p1376
|
|
|
What are the complications of rubeola?
|
1. diarrhea and protein-losing enteropathy → especially significant in malnourished
2. bronchopneumonia or broncholitis 3. secondary bacterial infections 4. encephalitis |
Current p1248
|
|
|
What is the clinical presentation of herpes zoster?
|

severe pain before onset of rash; lesions resembling chickenpox; dermatomal distribution
|
Current p1241
|
|
|
What is the management of rubeola?
|
Supportive:
1. acetominophen for fever 2. vitamin A 200,000 units/d PO x 2 days 3. antibiotics for 2° bacterial infections 4. fluids as necessary 5. bed rest until afebrile 6. isolation for 1 week following onset of rash |
Current p1249
|
|
|
What is clinical presentation of non-invasive tapeworm infection?
|
GI symptoms
abdominal pain diarrhea anorexia |
Current p1376
|
|
|
What is the prevention of rubeola, mumps, rubella, and varicella?
|
MMRV vaccine at 12-15 months and 4-6 years
|
Current 1249
|
|
|
What dermatomes are most commonly affected in herpes zoster?
|
thoracic and lumbar roots
|
Current p1241
|
|

|
koplik spots → rubeola
|
|
|
|
What is the diagnostic work-up of non-invasive tapeworm infection?
|
WBC count → eosinophilia
stool → proglottids (segment of tapeworm) or eggs *examine multiple specimens since egg release is irregular |
Current p1376
|
|

|
rubeola
|
|
|
|
What is the most common complication of herpes zoster?
|
postherpetic neuralgia → 60-70% if >60y/o
|
Current p1241
|
|
|
rubeola
|
|
|
|
Which type of non-invasive tapeworm infection is most severe and difficult to treat?
|
dwarf tapeworm
|
Current p1376
|
|
|
What is the common name for rubella?
|
german measles
|
|
|
|
What is the management of herpes zoster?
|
if uncomplicated → acyclovir 800mg PO 5x daily x 7 days within 72 hours of rash onset
|
Current p1242
|
|
|
What is the etiology of rubella?
|
caused by a togavirus; spread via respiratory droplets; fetal rubella common in third world countries
|
Current p1254
|
|
|
What is the management of non-invasive tapeworm infection?
|
1. if beef, pork, or fish tapeworm → praziquantel 5-10mg/kg PO single dose
2. if dwarf tapeworm → praziquantel 25mg/kg PO single dose, repeat in 1 week 3. follow-up |
Current p1376
|
|
|
What is the clinical presentation of rubella?
|
50% asymptomatic
fatigue, fever, rhinorrhea suboccipital, postauricular and posterior cervical lymphadenopathy rash → maculopapular, fine, pink; face → trunk → extremeties; fades quickly lasting 1 day each area if adult → 25% polyarticular arthritis of wrists, fingers, knees for 1 to several weeks |
Current p1254
|
|
|
What is the prevention for herpes zoster?
|
VZV vaccine at ≥60y/o
|
Current p1241
|
|
|
What is the diagnostic work-up of rubella?
|
IgM Ab, 4-fold rise in IgG Ab, viral PCR, or viral culture
|
Current p1254
|
|
|
What is the etiology of cysticercosis?
|
caused by parasitic tapeworm taenia solium; spread via ingestion of food contaminated with eggs from human feces; invasive form of pork tapeworm
|
Current p1377
|
|
|
What is the procedure for serological testing of rubella on pregnant women?
|
1. rubella ordered to R/O possibility of prenatal infection
2. positive IgG suggests vaccination or past infection 3. positive IgM suggests POSSIBLE current infection but interpret with caution 4. negative IgM and IgG requires clinical observation and serological follow-up |
Current p1254
|
|

|
herpes zoster
|
|
|
|
What are the complications of rubella?
|
congenital rubella → teratogenic → permanent congenital defects, high mortality rate
|
Current p1254
|
|
|
What is the clinical presentation of cysticercosis?
|
Neurocysticercosis:
HA, seizures, focal neurologic deficits, altered cognition, psychiatric disease symptoms due to CNS lesions and intraventricular cysts which lead to inflammation and ventricular obstruction |
Current p1377
|
|
|
What is the management of rubella?
|
Supportive:
1. acetominophen If prenatal: 1. possible therapeutic abortion |
Current p1254
|
|
|
What is the diagnostic work-up of cysticercosis?
|
serology
CSF → high cell count and protein, low glucose CT or MRI brain imaging → cysts |
Current p1377
|
|
|
What are the differences between postnastal and congenital rubella?
|
postnatal → mild, usually lasts 3-4 days
congenital → teratogenic → congenital defects and high mortality rate |
|
|
|
What is the management of cysticercosis?
|
1. difficult to determine when treatment needed → not always beneficial
2. albendazole 10-15mg/kg PO daily x 8 days 3. corticosteroids 4. if seizures → anticonvulsant therapy |
Current p1378
|
|

|
rubella
|
|
|
|
What are the complications of cysticercosis?
|
neurologic impairment
death 20 million infected yearly → 400,000 with neurological symptoms → 50,000 deaths |
Current p1377
|
|
|
What disease is characterized by rash starting on face and spreading downward and outward to palms and soles?
|
rubeola
|
|
|
|
What is strawberry tongue?
|

tongue with red inflamed papillae
|
|
|
|
What disease is characterized by rash starting on trunk and spreading to extremities?
|
varicella
|
|
|
|
What is the ddx for strawberry tongue?
|
scarlet fever
kawasaki disease toxic shock syndrome |
|
|
|
What disease is characterized by rash starting on face, then spreading to trunk, then extremeties in quick sucession, lasting 1 day each?
|
rubella
|
|
|

|
strawberry tongue → scarlet fever, kawasaki disease, toxic shock syndrome
|
|
|
|
What is the etiology of toxic shock syndrome (TSS)?
|
caused by staph aureus toxin; associated with tampon use, abscess, etc.
|
Current p1296
|
|

|
strawberry tongue → scarlet fever, kawasaki disease, toxic shock syndrome
|
|
|
|
What are 3 disorders caused by S. aureus toxins?
|
1. scalded skin syndrome → affects children
2. toxic shock syndrome → affects adults 3. enterotoxin food poisoning |
Current p1296
|
|
|
When is varicella no longer contagious?
|
when crusts begin to form
|
|
|
|
What is the clinical presentation of TSS?
|
diffuse "sun burn" rash
desquamation, especially palms and soles, over 1-2 weeks high fever, hypotension, involvement of 3 or more organ systems HA, nonpurulent conjunctivitis, sore throat, vomiting, watery diarrhea, myalgia |
Current p1296
|
|
|
What is the diagnostic work-up of TSS?
|
BC → negative since caused by toxin not systemic infection
vaginal or wound culture |
Current p1296
|
|
|
What is the management of TSS?
|
1. rapid rehydration
2. remove tampon, drain abscess, etc. 3. antibiotics |
Current p1296
|
|
|
What are the complications of TSS?
|
heart failure
kidney failure liver failure shock 15% mortality rate |
Current p1296
|
|
|
What is the prevention of tampon-associated TSS?
|
avoid use of tampons or use less frequently
change tampons often |
|
|
|
What is the etiology of Kawasaki disease?
|
idiopathic; usually affects children 3 months to 5 years, Asians or Pacific Islanders
|
Current p1288
|
|
|
What is the clinical presentation of Kawasaki disease?
|
fever + 4 of the following criteria x 5 days:
1. bilateral nonexudative conjunctivitis 2. mucous membrane changes → swelling and fissuring of lips, erythematous pharnyx, or strawberry tongue 3. peripheral extremity changes → erythema, edema, induration, desquamation 4. polymorphous rash 5. beau lines 6. cervical lymphadenopathy >1.5cm |
Current p1288
|
|
|
What is Kawasaki disease?
|
vasculitis characterized by infiltration of vessel walls with mononuclear cells and later by IgA secreting plasma cells → destruction and aneurysm formation
|
Current p1288
|
|
|
What are the complications of Kawasaki disease?
|
arteritis of the coronary vessels
coronary aneurysm MI |
Current p1288
|
|
|
What is the management of Kawasaki disease?
|
1. IVIG within first 10 days
2. if fever persists → 2nd dose of IVIG 3. if fever persists → methylprednisolone 4. echocardiogram 5. if coronary aneurysm → low-dose aspirin + warfarin 3. if MI → thrombolytics, CABG, PCCI, cardiac transplant 4. regular follow-up with cardiologist → coronary aneurysms may occur at 30-50y/o |
Current p1288
|
|
|
Define arteritis.
|
inflammation of arterial walls
|
|
|

|
kawasaki disease
|
|
|
|
When is varicella no longer contagious?
|
when crusts begin to form
|
|
|

|
chancre of 1° syphilis + condylomata acuminata
|
|
|

|
skin rash of 2° syphilis
|
|
|

|
skin rash of 2° syphilis
|
|
|
|
What is a chancre?
|
1° lesion of syphilis
|
|
|
|
What is the etiology of syphilis?
|
caused by the gram-negative bacteria treponema pallidum; spread via sexual contact, lesion-to-skin contact
|
|
|
|
What is the clinical presentation of 1° syphilis?
|
painless chancre; indurated borders with clear base; found on foreskin, glans penis, or labia; manifests 2-10 weeks after exposure
|
|
|
|
What is the etiology of oral herpes?
|
usually caused by HSV1, sometimes HSV2; transmitted via lesion-to-skin contact
|
|
|
|
What is the clinical presentation of oral herpes?
|
small pustule → ulceration → crust; usually found on lip or around mouth; sometimes found on nose, cheeks, chin, or fingers
|
|
|
|
What is the clinical presentation of genital herpes?
|
burning and stinging
painful small grouped vesicles on erythematous base → crust → heal in 1 week found on glans penis, penile shaft, base of penis, labia, perianal skin, and buttocks inguinal lymphadenopathy neuralgia |
Mosbys p658
|
|
|
What is Herpes Whitlow?
|
herpes lesions on the fingers
|
|
|
|
What is the etiology of chlamydia?
|
caused by parasite chlamydia trachomatis; spread via sexual contact
|
Current p1328
|
|
|
Coinfection with gonorrhea and chlamydia is common, true or false?
|
true
|
Current p1328
|
|
|
What is an important cause of post-gonococcal urethritis?
|
chlamydia trachomatis
|
Current p1328
|
|
|
What is the diagnostic work-up of chlamydia?
|
DNA probe → urethral, cervical
NAAT → urine, cervical GC RPR HIV |
Current p1328
|
|
|
What is the clinical presentation of chlamydia?
|
urethral or cervical discharge less painful, less purulent and watery compared to gonorrhea
females: often asymptomatic cervicitis, salpingitis, or PID males: urethritis occasionally epidiymitis, prostatitis, proctitis |
Current p1328
|
|
|
What are the complications of chlamydia?
|
infertility in females
|
Current p1328
|
|
|
What is the leading cause of infertility in women?
|
chlamydia
|
Current p1328
|
|
|
If urethritis or cervicitis present + negative GC, what should you assume until proven otherwise?
|
chlamydia infection present
|
Current p1328
|
|
|
Define proctitis.
|
inflammation of the rectum
|
|
|
|
What is the management for chlamydia?
|
azithromycin → 1g PO single dose
|
Current p1329
|
|
|
What are the indications for chlamydia screening?
|
1. all sexually active women ≤25y/o
2. all pregant women 3. older women with risk factors for STIs 4. men with risk factors for STIs → gay, HIV-positive |
Current p1328
|
|

|
chlamydial discharge
|
|
|

|
chlamydial cervicitis
|
|
|
|
What is the etiology of lymphogranuloma venereum?
|
caused by chlamydia trachomatis; spread via sexual contact or contact with contaminated exudate from active lesions
|
Current p1327
|
|
|
What does LGV stand for?
|
lymphogranuloma venereum
|
Current p1328
|
|
|
What is the clinical presentation of LGV?
|
5-21 day incubation period
Males: initially → vesicular or ulcerative lesion found on external genitals that disappears within few days 1-4 weeks later → infection spread to inguinal lymph nodes → manifests as bilateral inguinal buboes → draining sinuses → scarring Females and gay men: primary lesion often out of sight on vaginal wall spread of infection to perirectal lymph nodes → manifests as proctitis, tenesmus, bloody purulent discharge → inflammation, stricture, fistulas |
Current p1328
|
|
|
Define tenesmus.
|
feeling of incomplete defecation
|
|
|
|
What is the ddx for inguinal buboes?
|
STI:
lymphogranuloma venereum chancroid Insect/Animal: bubonic plague (flea vector) tularemia (tick vector) cat scratch disease (cat vector) |
|
|
|
What is the diagnostic work-up of LGV?
|
serology using complement fixation testing → titer >1:64 highly indicative; 80% sensitive after 2 weeks
|
Current p1328
|
|
|
What is the managment of LGV?
|
1. if diagnostic testing unavailable → treat empirically
2. doxycycline → 100mg PO 2x daily x 21 days |
Current p1328
|
|

|
inguinal buboes → lymphogranuloma venereum
|
|
|
|
What is the organism that causes lymphogranuloma venereum (LGV)?
|
chlamydia trachomatis
|
|
|
|
What is the etiology of gonorrhea?
|
caused by gram-negative bacteria neisseria gonorrhoeae; spread via sexual contact; common among 15-29y/o
|
Current 1319
|
|
|
What is the diagnostic work-up of gonorrhea?
|
DNA probe → urethral or cervical
NAAT → urine or cervical (gram stain → gram-neg diplococci in PMNs) Chlamydia RPR HIV |
Current 1319
|
|
|
What is the management of gonorrhea?
|
1. if uncomplicated urethral, cervical, or rectal gonorrhea → cefixime 400mg PO single dose (or cefriaxone 125mg IM)
2. if pharyngeal gonorrhea → cefriaxone 125mg IM 3. azithromycin 1g PO single dose unless chlamydia ruled out by negative DNA probe/NAAT 4. treat partners |
Current 1320
|
|
|
Aside from gonococcal urethritis and cervicitis, what are other manifestations of gonorrhea?
|
conjunctival
pharyngeal rectal disseminated |
Current 1319
|
|
|
What is the clinical presentation of disseminated gonorrhea?
|
gonococcal bacteremia: intermittent fever
arthralgia skin lesions → maculopapular, pustular or hemorrhagic; few; peripherally located arthritis of wrists, knees, ankles tenosynovitis endocarditis meningitis |
Current 1319
|
|
|
Define tenosynovitis.
|
inflammation of the sheath surrounding a tendon
|
|
|
|
What is the clinical presentation of gonorrhea?
|
2-8 day incubation period
Men: intially → burning on urination; serous or milky discharge 1-3 days later → urethral pain, yellow, creamy, profuse, sometimes bloody discharge Women: symptomatic during menses dysuria, urinary frequency and urgency, purulent urethral discharge, inflammation of bartholin glands, vaginitis, cervicitis |
Current 1319
|
|
|
What are the complications of gonorrhea?
|
Men:
epididymitis, prostatitis, inflammation of periurethral glands, urethral strictures Women: salpingitis → scarring of fallopian tubes → sterility |
Current 1319
|
|
|
List STIs and the appropriate medications to prescribe for treatment.
|
gonorrhea → cefixime PO or ceftriaxone IM
conjunctival gonorrhea → ceftriaxone pharyngeal gonorrhea → ceftriaxone IM chlamydia → azithromycin syphilis → penicillin herpes → acyclovir lymphogranuloma venereum → doxycycline chancroid → azithromycin or ceftriaxone granuloma inguinale → azithromycin |
|
|
|
What is the common name for gonorrhea?
|
clap
|
|
|

|
gonococcal discharge
|
|
|

|
gonococcal cervicitis
|
|
|
|
What is the etiology of chancroid?
|
caused by gram-negative bacteria haemophilus ducreyi; spread via sexual contact
|
Current p1320
|
|
|
What is the diagnostic work-up of chancroid?
|
swab lesion for culture
|
Current p1320
|
|
|
What is the management of chancroid?
|
azithromycin 1g PO single dose or cefriaxone 250mg IM
|
Current p1320
|
|
|
What are the complications of chancroid?
|
balanitis
phimosis |
Current p1320
|
|
|
What is the clinical presentation of chancroid?
|
3-5 day incubation period
vesicle → painful soft ulcer with necrotic base, surrounding erythema, and undermined edges located at site of inoculation may be multiple lesions if autoinoculation occurs inguinal lymphadenopathy → moderately sized, erythematous, matted, tender lymph nodes may become fluctuant and rupture → draining sinus signs of infection may not occur in women |
Current p1320
|
|
|
How do you distinguish between a syphilitic chancre and a chancroid?
|
syphilitic chancre → painless, hard
chancroid → painful, soft |
|
|

|
2° lymphadenopathy due to chancroid
|
|
|

|
chancroid
|
|
|
|
What is the etiology of granuloma inguinale?
|
caused by gram-negative bacteria Calymmatobacterium granulomatis; spread via sexual contact; rare in U.S. (100 cases per year, usually in SE); common in tropical areas
|
Current p1320
|
|
|
What is the diagnostic work-up of granuloma inguinale?
|
tissue scrapings or secretions → donovan bodies
|
Current p1321
|
|
|
What is the management of granuloma inguinale?
|
azithromycin 1g PO weekly x 3 weeks or until lesions healed
(ciprofloxacine, doxycycline, erythromycin also work) |
Current p1321
|
|
|
What disease is characterized by donovan bodies?
|
granuloma inguinale
|
Current p1320
|
|
|
What is the clinical presentation of granuloma inguinale?
|
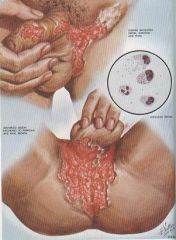
8 day to 12 week incubation period
painless infiltrated nodules → shallow ulcer with beefy-red friable base and sharp margins located on genitals or perianal area |
Current p1320
|
|
|
What are the complications of granuloma inguinale?
|
slow spread → genital destruction and scarring
|
Current p1321
|
|

|
granuloma inguinale
|
|
|
|
What are aggravating factors for herpes outbreaks?
|
trauma
infection sun exposure stress |
Current p113
|
|
|
What is the diagnostic work-up for genital herpes?
|
HSV culture
HSV PCR *HSV serology not used for diagnosis of acute genital lesions |
Current p114
|
|
|
In monogomous heterosexual couples where 1 partner is infected with HSV-2, what percent of non-infected partners undergo seroconversion within 1 year?
|
10%
|
Current p113
|
|
|
What is the etiology of genital herpes?
|
caused by HSV-2, sometimes HSV-1; spread via sexual contact
|
|
|
|
What is the management of primary genital herpes?
|
acyclovir 200mg PO 5x daily (or 800mg PO 3x daily) x 7-10 days
(valacyclovir 1000mg 2x daily or famciclovir 250mg 3x daily also work) |
Current p114
|
|
|
What is the management of recurrent genital herpes?
|
1. if mild → no therapy
2. for recurrences → acyclovir 200mg PO 5x daily x 5 days (valacyclovir or famciclovir also work) 3. initiate treatment at first sign of recurrence 4. only reduces outbreaks by 12-24 hours 5. if frequent recurrences or severe → suppressive therapy 6. acyclovir 400mg 2x daily everday (valacyclovir or famciclovir also work) |
Current p114
|
|
|
What is the patient education for reducing oral or genital herpes recurrences?
|
1. use sunscreen to help prevent sun-induced recurrences
2. if impending UV exposure or dental surgery → acyclovir prophylaxis 3. acyclovir 200mg 4x daily 24 hours prior to event (valacyclovir or famciclovir also work) |
Current p114
|
|
|
What is the prognosis for genital warts?
|
no treatment can guarantee remission or prevent recurrences
may spontaneously resolve recurrences common |
Current p132
|
|
|
What is the management for condyloma acuminata?
|
1. podophyllum resin → 10-25% in tincture of benzoin, wash off after 2-4 hours
2. 80-90% trichloroacetic or bichloracetic acid 3. liquid nitrogen 4. electrocautery 5. patient applied → podofilox 0.5% solution gel or imiquimod 5% cream 6. condom use does not prevent transmission but may accelerate regression of lesions |
Current p132
|
|
|
What is the common name for condyloma acuminata?
|
genital warts
|
|
|
|
What is the diagnostic work-up of condyloma acuminata?
|
diagnosed clinically if obvious lesions
apply 4% acetic acid → perform colposcopy → lesions appear whitish with prominent papillae |
Current p678
|
|
|
What is the etiology of condyloma acuminata?
|
caused by HPV; spread via sexual contact; associated with pregancy and immunosuppression
|
Current p678
|
|
|
What is the prevention of condyloma acuminata?
|
HPV vaccination
|
|
|
|
What is the clinical presentation of condyloma acuminata?
|
warty lesions on vulva, vaginal walls, cervix, or perianal area
possible hypertrophy or cobblestone appearance |
Current p678
|
|
|
Max braking speed
|
35 kts
|
|
|
|
If patient tests postive for gonorrhea, what should you empirically treat for?
|
chlamydia
|
|
|
|
If patient tests positive for gonorrhea/chlamydia, what should you also test for?
|
RPR
HIV |
|
|

|
genital herpes
|
|
|

|
genital herpes
|
|
|
|
Where are condyloma acuminatum lesions found in men?
|
prepuce, glans penis, penile shaft, and sometimes within urethra
|
Mosbys p659
|
|

|
lymphogranuloma venereum + inguinal lymphadenopathy
|
|
|
|
Describe vaginal discharge due to trichomonas.
|
greenish-white frothy discharge
|
|
|

What does this vaginal discharge indicate?
|
white frothy discharge → trichomoniasis
|
|
|

What does this vaginal discharge indicate?
|
white frothy discharge → trichomoniasis
|
|
|
|
What organism causes trichomoniasis?
|
trichomonas vaginalis
|
|
|
|
Which type of the following vaginitis is sexually transmitted: vulvovaginal candidiasis, trichomoniasis, or bacterial vaginosis?
|
trichomoniasis
|
|
|
|
What is the treatment for trichomoniasis?
|
metronidazole (Flagyl)
|
|
|

What does this cervix indicate?
|
strawberry cervix → trichomoniasis
|
|
|

What does this cervix indicate?
|
strawberry cervix → trichomoniasis
|
|
|
|
What is strawberry cervix?
|
cervix that is inflammed and speckled with petechiae → indicative of trichomoniasis
|
|
|
|
Describe the procedure for collecting a pap smear using a broom and liquid vial.
|

1. insert central bristles of broom into endocervical canal
2. allow shorter bristles of broom to contact ectocervix 2. push gently and rotate broom clockwise 5 times 3. remove broom 4. push broom into bottom of vial 10 times 5. swirl broom vigorously in vial 6. discard broom or deposit in vial |
Mosbys p602
|
|
|
Describe the procedure for collecting a wet mount.
|
1. insert sterile cotton swab into vagina
2. swab vaginal secretions 3. remove swab 4. insert swab into saline solution |
Mosbys p603
|
|
|
Describe the procedure for collecting a gonorrhea/chlamydia DNA probe.
|
1. insert discard swab into vagina and remove excess mucus from cervical os and surrounding mucosa
2. discard swab 3. insert DNA probe swab 1.0-1.5cm into endocervical canal avoiding contact with vaginal membranes 4. rotate swab clockwise for 30 sec 5. remove swab avoiding contact with vaginal membranes 6. insert swab into media |
Mosbys p603
http://www.gen-probe.com/pdfs/pi/103267RevJ.1.pdf |
|

|
oral herpes
|
|
|

|
oral herpes
|
|
|
|
What may rust-colored sputum indicate?
|
pneumococcal pneumonia
|
|
|
|
What may currant jelly sputum indicate?
|
klebsiella pneumonia
|
|
|
|
What are the clinical features of typical vs atypical pneumonia?
|
TYPICAL:
acute onset prostration high fever cough with sputum lobar consolidation ATYPICAL: insidious onset little to no fever cough without sputum hazy diffuse infiltrates (no signs of consolidation) |
|
|
|
List organisms that cause typical vs atypical pneumonia.
|
TYPICAL:
streptococcus pneumoniae staphyloccocus aureus haemophilus influenzae klebsiella pneumoniae ATYPICAL: mycoplasma pneumoniae chlamydia pneumoniae legionella species influenza viruses |
|
|
|
What are the CDC guidelines for prevention of active TB in a patient with history of exposure or positive PPD?
|
1. most people with latent TB never develop active TB
2. certain populations with latent TB are at an increased risk for developing active TB -infected within last 2 years -young children -elderly -IV drug users -HIV+ -immunocompromised -people not correctly treated for TB in past 3. treatment can reduce risk of active TB by 90% 4. treatment consists of isoniazid x 9 months (longer if child or HIV+) 5. directly observed therapy recommended 6. prevention if exposure to active multi-drug resistant TB may not be an option |
http://tiny.cc/TBprevention
|
|
|
Describe the difference between active and latent TB.
|
ACTIVE:
infectious LATENT: not infectious disease can reactivate to active TB if immunocompromised will progress to active TB in 10% of people not given preventive therapy for latent TB (half of these cases occur in first 2 years) |
|
|
|
What is the etiology of TB?
|
caused by mycobacterium tuburculosis
spread via inhalation of droplets affe cts 20-43% of world population risk factors included malnourished, homeless, crowding housing, HIV+ |
|
|
|
What is the clinical presentation of TB?
|
fatigue, fever, night sweats, weight loss, chronic cough (initially dry, becomes productive as disease progresses), blood streaked sputum, posttussive apical crackles
|
|
|
|
What is diagnostic workup of TB?
|
CXR →
small homogenous infiltrates → often apical hilar and paratracheal lymph node enlargement segmental atelectasis possible pleural effusion, cavitation miliary TB → diffuse small nodular densities → seen if hematogenous or lymphatic spread PPD 3 consecutive morning sputum samples AFB → not diagnostic of TB, may be positive with other mycobacteria bronchoscopy if suspicion but negative sputum pleural fluid analysis if associated pleural effusion biopsy → granulomatous inflammation |
|
|
|
What percentage of people infected with TB develop active TB?
|
5%
|
|
|
|
Extrapulmonary TB is most common in what population?
|
HIV+ → who display lymphadenitis and miliary TB
|
|
|
|
What is the typical manifestations of extrapulmonary TB?
|
meningitis
brain TB Pott's disease → vertebral TB lymphadenitis intestinal TB renal TB |
|
|
|
PPD distinguises between latent and active TB, true or false?
|
false
|
|
|
|
When might a false negative PPD occur?
|
exposure <2-10 weeks prior
immunologic disorders corticosteroid therapy concurrent infections malnutrition advanced age improper testing techinque chronic kidney disease HIV+ lymphoreticular malignancies |
|
|
|
When might a false positive PPD occur?
|
previous BCG vaccination
infection with non-tuberculous mycobacteria |
|
|
|
Describe PPD testing.
|
1. 0.1mL of purified protein derivative (PPD) containing 5 tuberculin units injected intradermally on volar surface of forearm using 27-gauge needle
2. transverse width of induration measured after 48-72 hours 3. if ≥ 5mm → positive for HIV+, recent contact with active TB, suspected prior TB indicated by fibrosis on CXR, corticosteroid therapy (organ transplant, other immunosuppressed patients) 4. if ≥ 10mm -children <4 -children >4 exposed to high risk adults -recent immigrants from endemic countries -IV drug users -comorbities → below ideal body weight, DM, CKD, silicosis, malignancies, gastrectomy -residents/employees → medical, homeless shelters, jails 5. if ≥15 mm → positive if no risk factors |
|
|
|
How is interpretation of a PPD affected if previous BCG vaccination?
|
interpretation is the same as if no BCG vaccination received
|
|
|
|
What is the most common cause of infertility worldwide?
|
TB
|
|
|
|
IGRA can distinguish between latent and active TB, true or false?
|
true
|
|
|
|
What does IGRA stand for?
|
interferon-gamma release assays
|
|
|
|
What are the advantages of IGRA vs PPD?
|
IGRA
-requires single patient visit -results in 24 hours -distinguishes between latent and active TB -prior BCG does not cause false-pos -does not cause "boosting" |
|
|
|
Who should get an IGRA vs PPD?
|
-previous BCG vaccination
-at risk populations who do not return in 48-72 hours DO NOT test children <5 → no IGRA data for this population DO NOT test people with low risk for TB |
|
|
|
What is the treatment for active TB?
|
1. combination drug therapy with isoniazid, rifampin, pyrazinamide, ethambutol x 2 months
2. then combination therapy of isoniazid + rifampin x 4 months 3. treatment 3 months following negative sputum cultures 4. directly observed therapy (DOT) recommended 5. report to state authorities 6. exact regimen depends on pregnancy, resistance, etc. |
|
|
|
What is the treatment for latent TB?
|
isoniazid x 9 months
DOT recommended |
|
|
|
What is the patient education for TB?
|
1. compliance → adhering to drug protocol is essential in preventing drug-resistant TB!
2. latent TB is not infectious |
|
|
|
What are the reporting requirements for TB?
|
report suspected and confirmed cases of TB to local health department within 1 day
|
http://www.oregon.gov/DHS/ph/tb/docs/investigativeguide.pdf
|
|
|
What is the clinical presentation of extrapulmonary TB?
|
vague symptoms
fatigue, intermittent fever, night sweats, weight loss, reduced appetite, pain/abscess most often affects kidneys and lymph nodes also affects bones, brain, abdominal cavity, pericardium, joints, and reproductive organs meningitis pericarditis |
|
|
|
Discuss community acquired pneumonia vs hospital acquired pneumonia.
|
CAP:
occurs outside hospital or within 48 hours of admission in patient who is ambulatory and did not reside in long-term care facility HAP: occurs in hopsital after 48 hours of admission excludes infections at time of admission common in patients requiring mechanical ventilation |
|
|
|
What is the treatment of CAP?
|
If not being admitted:
oral clarithromycin, azithromycin, or doxycycline x 5 days to 2 weeks and until patient afebrile x 2-3 days If admitting: order BC IV extended spectrum B-lactam (ceftriaxone or cefotaxime) + macrolide (clarythromycin or azithromycin) |
|
|
|
What is the clinical presentation of HAP?
|
fever, purulent sputum, leukocytosis, new or progressive infiltrate on CXR, symptoms for CAP
|
|
|
|
What is the treatment of HAP?
|
2nd-generation cephalosporin, 3rd-generation cephalosporin, or B-lactam + B-lactamase inhibitor
|
|
|
|
What are the risk factors for anaerobic pneumonia?
|
aspiration risk factors → unprotected airway (alcoholics, drug overdose, seizure disorders) + gingivitis
|
|
|
|
What are the complications of anaerobic pneumonia?
|
parapneumonic effusion
empyema abscess |
|
|
|
What type of disease is mumps?
|
parotitis
|
|
|
|
What is the etiology of mumps?
|
caused by a paramyxovirus; spread via respiratory droplets; usually affects children
|
Current p1250
|
|
|
What is the clinical presentation of mumps?
|

incubation 2-3 weeks before onset
fatigue and fever → variable parotid gland enlargement → unilateral or bilateral, usually one enlarges before the other stenson's duct → erythematous, edematous parotid tenderness facial edema +/- trismus +/- submaxillary and sublingual gland involvement |
Current p1250
|
|
|
What is the diagnostic work-up of mumps?
|
usually diagnosed clinically; swab parotid duct for confirmation via NAAT (more sensitive), viral culture or serum IgM
|
Current p1250
|
|
|
What are the complications of mumps?
|
pancreatitis →affects children; upper abdominal pain, nausea, vomiting
orchitis → affects 25-40% postpubertal men, high fever, testicular swelling and tenderness oophoritis → affects 5% of postpubertal women, lower abdominal pain, ovarian enlargement meningitis → high fever, headache, stiff neck, lethargy |
Current p1250
|
|
|
Mumps is the most common cause of what disease in children?
|
pancreatitis
|
Current p1250
|
|
|
What is the management of mumps?
|
Symptomatic:
1. topical compresses 2. bed rest until afebrile 3. isolation until swelling subsides (9 days following onset) |
Current p1250
|
|
|
What is the ddx for parotidis?
|
dehydration → stasis of salivary flow
sialolithiais of stenson's duct bacterial infection viral infection cyst or tumor etc |
Current p1250
|
|

|
mumps
|
|
|

|
mumps
|
|
|
|
What is the etiology of diphtheria?
|
caused by corynebacterium diphtheriae; spread via respiratory droplets; rare due to TDAP vaccine; infectious disease emergency
|
Current p204
|
|
|
What is the clinical presentation of pharyngeal diphtheria?
|
mild fatigue, fever, sore throat; gray tonsillar pseudomembrane covering tonsils and pharynx
|
Current p204
|
|
|
What is the diagnostic work-up of diphtheria?
|
diagnosis made clinically but can be confirmed by culture
|
Current p1302
|
|
|
What are the complications of diphtheria and their associated symptoms?
|
myocarditis → cardiac arrhythmias, heart block, heart failure
neuropathy → initally affects CNs → diplopia, dysphagia, slurred speech |
Current p1302
|
|
|
What is the management of diphtheria?
|
1. antitoxin (obtained from CDC)
2. if potential or current airway obstruction → remove pseudomembrane via laryngoscopy or bronchoscopy 3. penicillin 250mg PO 4x daily x 14 days or erythromycin 500mg PO 4x daily x 14 days 4. isolation until 3 consecutive cultures at completion of therapy confirm elimination 5. treat patient contacts → erythromycin 500mg PO 4x daily x 7 days; diphtheria booster |
Current p1302
|
|
|
What is the prevention of diphtheria?
|
TDAP vaccination
|
|
|
|
Compare and contrast the clinical presentation of the common cold, influenza, and H1N1.
|
common cold → gradual onset, sneezing, nasal congestion, watery rhinorrhea, sore throat, cough
influenza → rapid onset, fatigue, high fever, headache, body aches, chills, nasal congestion, rhinorrhea, sore throat, cough H1N1 → fatigue, fever, headache, body aches, chills, nasal congestion, rhinorrhea, sore throat, cough, vomiting, diarrhea |
|
|
|
How long does a SPUTC remain positive?
|
possibly several weeks
*do not give additional antituberculous drugs b/c you think the patient is not responding to tx |
Interpreting Laboratory Data p7
|
|
|
What is another name for pneumococcal pneumonia?
|
strep pneumonia
|
|
|
|
What is the etiology of pneumococcal pneumonia?
|
caused by streptococcus pneumoniae; community-acquired and hospital-acquired pneumonia
|
|
|
|
What is the diagnostic work-up of pneumococcal pneumonia?
|
BC
sputum gram → gram-pos diplococci sputum culture CXR → consolidating lobar pneumonia |
|
|
|
What is the definition of a good sputum sample?
|
<10 epithelial cells and >25 PMNs per high-power field
|
Current p1252
|
|
|
What are the complications of pneumococcal pneumonia?
|
parapneumonic effusion
empyema pericarditis endocarditis |
Current p1252
|
|
|
What is the clinical presentation of pneumococcal pneumonia?
|
high fever, chills, dyspnea, productive cough, +/- hemoptysis, pleuritic chest pain, bronchial breath sounds
|
Current p1252
|
|
|
What is the management of pneumococcal pneumonia?
|
1. empiric treatment until isolation of s. pneumo
2. if uncomplicated → amoxicillin 3. if penicillin-resistant strain → vancomycin |
Current p1252
|
|
|
What is the common name for pertussis?
|
whooping cough
|
Current p1308
|
|
|
What is the etiology of pertussis?
|
caused by bordetella pertussis; spread via respiratory droplets; 50% before 2y/o
|
Current p1308
|
|
|
What is the prevention of pertussis?
|
TDAP vaccination
|
Current p1308
|
|
|
What is the management of pertussis?
|
1. erythromycin 500mg PO 4x daily x 7 days
2. offer erythromycin to contacts if exposed within 3 weeks of onset |
Current p1308
|
|
|
What is the clinical presentation of pertussis?
|
1. catarrhal stage → fatigue, lacrimation, sneezing, rhinorrhea, hacking night cough, anorexia
2. paroxysmal stage → whooping cough 3. convalescent stage → decrease in severity of whooping cough, 4 weeks after onset entire illness lasts 6 weeks |
Current p1308
|
|
|
What is the diagnostic work-up of pertussis?
|
collect nasopharyngeal dacron swab
pertussis PCR or pertussis culture with bordet-gengou agar |
Current p1308
|
|
|
What is the etiology of legionnaire's disease?
|
caused by bacteria legionella pneumophilia; transmitted via contaminated water sources like heating and cooling systems of hospitals; not spread via person-to-person; increased risk in smokers, chronic lung disease, immunocompromised
|
Current p1310
|
|
|
What is the clinical presentation of legionnaire's disease?
|
fatigue, fever, chills, HA, cough
atypical pneumonia → scant sputum, pleuritic chest pain |
Current p1310
|
|
|
What type of pneumonia is legionnaire's disease?
|
community acquired
atypical |
Current p1310
|
|
|
What is the diagnostic work-up of legionnaire's disease?
|
sputum GRAM → no bacteria
sputum PCR or culture CXR → patchy infiltrates or consolidation, often bibasal consolidation |
Current p1310
|
|
|
Where is legionella naturally found?
|
water
|
|
|
|
What is the management for legionnaire's disease?
|
1. azithromycin 500mg PO 1x daily x 10-14 days
2. if immunocompromised → extend treatment to 21 days 3. DO NOT prescribe erythromycin |
Current p1311
|
|
|
Is legionnaire's contagious from person-to-person?
|
no
|
|
|
|
What is the etiology of hemophilus influenzae pneumonia?
|
caused by bacteria hemophilus influenzae; community-acquired pneumonia
|
|
|
|
What is the diagnostic work-up of hemophilus influenzae pneumonia?
|
sputum GRAM → gram-neg coccobacilli
sputum PCR or culture CXR |
|
|
|
What is the general presentation of community-acquired pneumonia?
|
acute fever, dyspnea
cough +/- sputum fatigue, chills, rigors, sweats, HA, hemoptysis, pleuritic chest pain, abdominal pain, myalgia, altered breath sounds, crackles, dullness to percussion if parapneumonic pleural effusion |
Current p246
|
|
|
What are the most common causes of community-acquired pneumonia?
|
1. pneumococcal pneumoniae
2. mycoplasmal pneumoniae 3. hemophlius influenza 4. legionnairese 5. aspiration 6. respiratory viruses |
|
|
|
What are the most common causes of hospital-acquired pneumonia?
|
1. streptococcal pneumoniae
2. staph aureus 3. legionnaires |
|
|
|
Grey pseudomembrane in posterior orpharynx indictes?
|
diphtheria
|
Mosbys p343
|
|

|
grey pseudomembrane → diphtheria
|
|
|
|
List 4 types of pharyngitis/tonsillits.
|
1. viral pharyngitis
2. group A beta-hemolytic streptococcal pharyngitis (GABHS) 3. mononucleosis 4. diphtheria |
|

