![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
464 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are the 4 quadrants of the abdomen?
|

1. RUQ (right upper quadrant)
2. RLQ (right lower quadrant) 3. LUQ (left upper quadrant) 4. LLQ (left lower quadrant) |
|
|
|
What is the equipment needed for the abdominal exam?
|
stethoscope
ruler measuring tape pen gloves, lubricating gel for rectal |
Mosbys p532
|
|
|
What are 3 surface landmarks of the abdomen?
|
1. umbilicus
2. anterior superior iliac spine 3. inguinal ligament |
|
|
|
What structures are found in the RUQ?
|
liver
gallbladder head of pancreas pylorus of stomach duodenum hepatic flexure of colon portion of ascending and transverse colon RT adrenal gland upper portion of RT kidney |
Mosbys p534
|
|
|
What structures are found in the RLQ?
|
cecum
appendix portion of ascending colon lower portion of RT kidney RT ureter RT spermatic cord RT fallopian tube and ovary bladder if distended uterus if distended |
Mosbys p534
|
|
|
What structures are found in the LUQ?
|
left lobe of liver
spleen body of pancreas fundus and body of stomach splenic flexure of colon portion of transverse and descending colon LT adrenal gland upper portion of LT kidney |
Mosbys p534
|
|
|
What structures are found in the LLQ?
|
portion of descending colon
sigmoid colon lower portion of LT kidney LT ureter LT spermatic cord LT fallopian tube and ovary bladder if distended uterus if distended |
Mosbys p534
|
|
|
What structures are found in the RT hypochondriac region?
|
portion of liver
gallbaldder portion of duodenum hepatic flexure of colon RT adrenal gland portion of RT kidney |
Mosbys p534
|
|
|
What structures are found in the epigastric region?
|
portion of liver
head and body of pancreas portion of duodenum pylorus of stomach |
Mosbys p534
|
|
|
What structures are found in the LT hypochondriac region?
|
portion of liver
spleen tail of pancreas fundus and body of stomach splenic flexure of colon LT adrenal gland portion of LT kidney |
Mosbys p534
|
|
|
What structures are found in the RT lumbar region?
|
portion of duodenum and jejunum
ascending colon portion of RT kidney |
Mosbys p534
|
|
|
What structures are found in the umbilical region?
|
portion of duodenum, jejunum and ileum
omentum mesentary |
Mosbys p534
|
|
|
What structures are found in the LT lumbar region?
|
portion of jejunum and ileum
desending colon portion of LT kidney |
Mosbys p534
|
|
|
What structures are found in the RT inguinal region?
|
portion of ileum
cecum appendix LT ureter LT spermatic cord LT fallopian tube and ovary |
Mosbys p534
|
|
|
What structures are found in the hypogastric region?
|
portion of ileum
bladder uterus (in pregnancy) |
Mosbys p534
|
|
|
What structures are found in the LT inguinal region?
|
sigmoid colon
LT ureter LT spermatic cord LT fallopian tube and ovary |
Mosbys p534
|
|
|
What is diastasis recti and what causes it?
|
separation of rectus abdominis muscles; often caused by obesity or pregnancy (but of little clinical significance)
|
Mosbys p536
|
|
|
How long must you listen to bowel sounds to determine their absence?
|
5 min
|
Mosbys p536
|
|
|
Is bright red stool indicative of an upper or lower GI bleed?
|
usually lower GI bleed
(though can also occur in massive upper GI bleed) |
|
|
|
Is black tarry stool indicative of an upper or lower GI bleed?
|
upper GI bleed
|
|
|
|
What are the most common causes of hematochezia in adults?
|
hemorrhoids
diverticulitis colon cancer |
|
|
|
If you give a patient a narcotic for abdominal pain, will it obscure the correct diagnosis or delay appropriate treatment?
|
NO!
|
Cope p5
|
|
|
What is an intussusception?
|
medical condition where one part of the intestine invaginates into another part of the intestine; can result in obstruction
|
|
|
|
What is dyspepsia?
|
acute, chronic, or recurrent discomfort or pain in upper abdomen
epigastric pain or burning |
Current p502
|
|
|
Where does upper GI become lower GI?
|
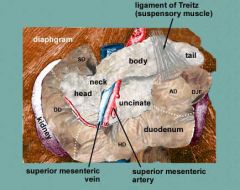
ligament of Treitz
located at duodeno-jejunal junction connects duodenum to diaphragm |
http://tiny.cc/ligamentoftreitz
|
|
|
Define transaminitis.
|
elevated transaminases:
1. ALT (alanine transaminase) 2. AST (aspartate transaminase) |
|
|
|
What do elevated ALT and AST indicate?
|
possible liver damage
|
|
|
|
What AST and ALT levels indicate alcoholic liver disease?
|
AST levels that are 2-3x ALT levels
|
|
|
|
What AST and ALT levels indicate ischemic hepatitis?
|
>1000
|
|
|
|
What are the risk factors for colorectal cancer?
|
1. >50y/o
2. poor diet (high in red meat, low in fiber) 3. lack of exercise 4. smoking 5. alcohol 6. obesity 7. PMH of colorectal cancer, intestinal polyps, chronic inflammatory bowel disease (Crohn's disease, ulcerative colitis), Gardner syndrome, breast cancer, endometrial cancer, ovarian cancer 8. FH of colon cancer, familial adenomatous polyposis (FAP), familial hereditary nonpolyposis colorectal cancer (HNPCC), Gardner syndrome 9. Ashkenazi Jewish descent |
Mosbys p531
|
|
|
What is Cullen's sign and what may it indicate?
|

periumbilical ecchymosis; may indicate acute pancreatitis or hemoperitoneum (2° to blunt abdominal trauma, ruptured AAA or ruptured ectopic pregnancy)
|
Mosbys p557
|
|
|
Pain the RUQ may indicate?
|
hepatomegaly
hepatitis cholecystitis duodenal ulcer pneumonia |
Mosbys p551
|
|
|
Pain in the RLQ may indicate?
|
Meckel's diverticulitis
regional ileitis perforated cecum appendicitis ovarian cyst salpingitis ruptured ectopic pregnancy renal/ureteral stone strangulated hernia |
Mosbys p551
|
|
|
What is Meckel's diverticulum?
|
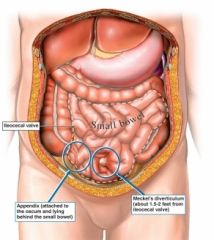
congenital bulge in distal ileum
|
|
|
|
Pain in the LUQ may indicate?
|
gastric ulcer
splenomegaly ruptured spleen perforated colon aortic aneurysm pneumonia |
Mosbys 551
|
|
|
Pain in the LLQ may indicate?
|
regional ileitis
sigmoid diverticulitis ulcerative colitis perforated colon renal/ureteral stone ovarian cyst salpingintis ruptured ectopic pregnancy strangulated hernia |
Mosbys 551
|
|
|
Periumbilical pain may indicate?
|
acute pancreatitis
early appendicitis diverticulitis intestinal obstruction aortic aneurysm mesenteric thrombosis |
Mosbys p551
|
|
|
What sounds are expected when percussing the abdomen?
|
tympany over stomach and intestines
dullness over organs |
Mosbys p537
|
|
|
What is Grey Turner's sign and what may it indicate?
|
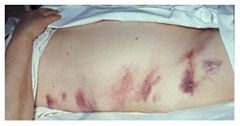
flank ecchymosis; may indicate acute pancreatitis or hemoperitoneum (2° to blunt abdominal trauma, ruptured AAA, ruptured ectopic pregnancy, or coagulopathy)
|
Mosbys p557
|
|
|
Where is McBurney's point located?
|
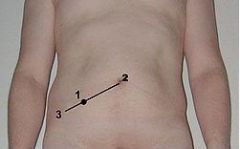
two-thirds the distance from the umbilicus to the ASIS
|
|
|
|
What is McBurney's sign and what may it indicate?
|
reboud tenderness and sharp pain when McBurney's point palpated; may indicate appendicitis
|
Mosbys p557
|
|
|
What is Murphy's sign and what may it indicate?
|
abrupt cessation of inspiration on palpation of gallbladder; may indicate cholecystitis
|
Mosbys p557
|
|
|
What is the ddx for generalized abdominal distension?
|
obesity
enlarged organs gas fluid |
Mosbys
|
|
|
What is the ddx for abdominal distension in RLQ/LLQ?
|
distended bladder
pregnancy ovarian tumor uterine fibroids (benign tumors) |
Mosbys
|
|
|
What is the ddx for abdominal distension in RUQ/LUQ?
|
gastric dilation
pancreatic cyst carcinoma |
Mosbys
|
|
|
What is the ddx for assymetric abdominal distension?
|
enlarged organ
bowel obstruction hernia cyst tumor |
Mosbys
|
|
|
What is the difference between a reducable and non-reducable hernia?
|
contents can be pushed back in if reducible
contents can't be pushed back in if non-reducable |
Mosbys
|
|
|
What is the definition of a strangulated hernia?
|
non-reducible hernia + blood supply to contents obstructed
|
Mosbys
|
|
|
Limited abdominal movement may indicate?
|
peritonitis
|
Mosbys
|
|
|
When evaluating abdominal movement, visible peristalis may indicate?
|
bowel obstruction
|
Mosbys
|
|
|
When evaluating abdominal movement, marked pulsation may indicate?
|
AAA
|
Mosbys
|
|
|
What is borborygmi?
|
stomach growling
|
|
|
|
What are the characteristics of normal bowel sounds?
|
generalized irregular clicks and gurgles
5-35 per minute |
Mosbys
|
|
|
Increased bowel sounds may indicate?
|
borborygmi
gastroenteritis early abdominal obstruction |
Mosbys
|
|
|
Decreased bowel sounds may indicate?
|
peritonitis
paralytic ileus |
Mosbys
|
|
|
High-pitched, tinkling abdominal sounds may indicate?
|
intestinal air or fluid under pressure (ex: early abdominal obstruction)
|
Mosbys
|
|
|
What are evaluating during abdominal inspection?
|
color (bruising, jaundice)
venous pattern lesions/masses (striae, scarring) contour (flat, rounded, scaphoid) symmetry (distension, bulges) surface movement |
Mosbys
|
|
|
What is normal liver span?
|
6-12 cm
if >12 cm, may indicate hepatomegaly if <6 cm, may indicate liver atrophy |
Mosbys
|
|
|
When might liver span be overestimated?
|
upper border obscured by pleural effusion or consolidation
|
Mosbys
|
|
|
Where is lower liver border normally?
|
at/slighly below costal margin
|
Mosbys
|
|
|
Where is upper liver border normally?
|
between 5th and 7th ICS
|
Mosbys
|
|
|
What is the most common cause of peptic ulcer disease?
|
h. pylori
|
|
|
|
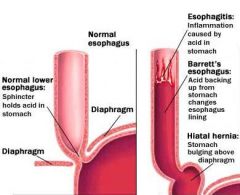
What is a hiatal hernia?
|
herniation of upper part of stomach into thorax through weakness or tear in diaphragm
|
|
|
|
What is SAAG and when would you order it?
|
serum ascites albumin gradient; to determine if ascites is transudate (portal HTN) or exudate
|
Current
|
|
|
How is SAAG calculated?
|
SAAG = serum ALB - ascitic fluid ALB
|
|
|
|
How is SAAG interpreted?
|
portal HTN if >1.1 g/dL
condition unrelated to portal HTN if <1.1 g/dL |
|
|
|
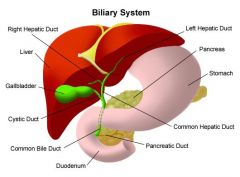
Where does bile drain?
|
gallbladder for storage or duodenum
|
Interpreting Laboratory Data p236
|
|
|
What foods should be eaten for diarrhea?
|
bananas
|
|
|
|
What foods prevent or treat constipation?
|
increase fluids (water, fruit juice)
increase fiber (fruit, prunes, apricots, vegetables, beans) increase bran (bran cereals, bran muffins, shredded wheat, whole wheat bread) decrease milk, bananas, cheese and yogurt |
|
|
|
How does hepatic dysfunction affect lab results?
|
reduced clotting factor production
increased PT increased PTT |
Interpreting Laboratory Data p11
|
|
|
What drugs are hepatotoxic?
|
rifampin
isoniazid |
Interpreting Laboratory Data p39
|
|
|
How do hepatotoxic drugs affect lab results?
|
↑ ALT
↑ AST |
Interpreting Laboratory Data p39
|
|
|
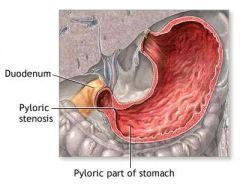
What is pyloric stenosis?
|
postnatal muscular hypertrophy of the pyloris causing stenosis
|
|
|
|
PYLORIC STENOSIS:
|
ETIOLOGY:
postnatal muscular hypertrophy of the pylorus with progressive gastric outlet obstruction cause unknown 1-8:1000 births, 4:1 male predominance, 13% positive FH CLINICAL PRESENTATION: postprandial projectile non-bilious blood-streaked vomiting, usually starts between 2-4 weeks (but may start at birth to 12 weeks) increased hunger, avid nursing fretfulness, constipation, weight loss, dehydration, apathy postprandial abdominal distention visible gastric peristalsis from left to right palpable RUQ oval mass 5-15 mm, especially after vomiting hypochloremic alkalosis upper GI contrast radiograph or abdominal US MANAGEMENT: 1. correct dehydration and electrolyte imbalances 2. Ramstedt pyloromyotomy → incision down to mucosa along pyloric length COMPLICATIONS: none PREVENTION: none |
|
|
|
What is intussusception?
|
invagination of intestine into another part of intestine causing obstruction
|
|
|
|
INTUSSUSCEPTION:
|
ETIOLOGY:
most common cause of intestinal obstruction in children <2y/o 3:1 female predominance 85% idiopathic other causes include small bowel polyp, Meckel diverticulum, omphalomesenteric remnant, duplication, Henoch-Schönlein purpura, lymphoma, lipoma, parasites, foreign bodies, viral enteritis with hypertrophy of Peyer patches, celiac disease, CF lymphoma most common cause if >6y/o usually occurs at ileocecal valve CLINICAL PRESENTATION: recurrent paroxysms of abdominal pain with screaming and drawing up of knees vomiting, diarrhea bloody mucoid stool within 12 hours lethargic between paroxysms +/- fever abdominal distention and tenderness sausage-shaped mass in epigastric region symptoms can persist for days if incomplete obstruction or spontaneous resolution MANAGEMENT: barium enema (contraindicated if signs of strangulated bowel, perforation, toxicity) or air enema for diagnosis and reduction surgery if extremely ill, perforation, or enema reduction unsuccessful COMPLICATIONS: incarceration, necrosis intestinal perforation, peritonitis, hemorrhage PREVENTION: |
|
|
|
Define melena.
|
black tarry stools due to presence of blood exposed to gastric acid
|
|
|
|
Define hematochezia.
|
bright red stools due to presence of blood
|
|
|
|
Define hematemesis.
|
vomiting blood
|
|
|
|
Define singultus.
|
hiccups
|
|
|
|
Define eructation.
|
belching
|
|
|
|
Define tenesmus.
|
feeling of incomplete defecation
|
|
|
|
*Define icterus.
|
AKA jaundice → yellow pigmentation of skin and mucous membranes due to accumulation of bilirubin in tissues
|
|
|
|
Define aerophagia.
|
air swallowing
|
|
|
|
Define odynophagia.
|
painful swallowing
|
|
|
|
Define dysphagia.
|
difficulty or painful swallowing
|
|
|
|
Define flatulence.
|
gas
|
|
|
|
Define heartburn.
|
substernal burning often radiating to neck
|
|
|
|
What disorder is characterized by heartburn?
|
GERD
|
|
|
|
List types of dysphagia.
|
oropharyngeal
esophageal |
|
|
|
What is the generic name for Advil?
|
ibuprofen
|
|
|
|
Describe the biliary system.
|
|
|
|
|
What is the approach to the patient with dysphagia?
|
1. distinguish between oral, pharyngeal, or esophageal dysphagia
2. upper endoscopy 3. ORAL DYSPHAGIA: 1. difficulty in transferring food from oropharnyx to upper esophagus 2. symptoms include drooling, spillage from mouth, inability to chew or initiate swallowing, dry mouth PHARYNGEAL DYSPHAGIA: 1. difficulty in transferring food to upper esophagus 2. symptoms include immediate sense of bolus catching in neck, need to swallow repeatedly to clear bolus, coughin or choking during meals, neurological symptoms (dysphonia, dysarthria) ESOPHAGEAL DYSPHAGIA: 1. impaired transport of bolus through esophagus 2. may be caused by obstruction of esophagus or impaired motility 3. if obstruction → usually occurs with solids, predictable, recurrent 4. if motility disorder → occurs with solids and liquids, unpredictable, episodic |
|
|
|
Define dysarthria.
|
impaired ability to articulate words
manifests as slurred speech |
|
|
|
Define dysphonia.
|
impaired ability to produce vocal sounds
|
|
|
|
What is the ddx for dysphagia?
|
OROPHARYNGEAL:
Neurologic disorders Brainstem cerebrovascular accident, mass lesion Amyotrophic lateral sclerosis, multiple sclerosis, pseudobulbar palsy, post-polio syndrome, Guillain-Barré syndrome Parkinson disease, Huntington disease, dementia Tardive dyskinesia Muscular and rheumatologic disorders Myopathies, polymyositis Oculopharyngeal dystrophy Sjögren syndrome Metabolic disorders Thyrotoxicosis, amyloidosis, Cushing disease, Wilson disease Medication side effects: anticholinergics, phenothiazines Infectious disease Polio, diphtheria, botulism, Lyme disease, syphilis, mucositis (Candida, herpes) Structural disorders Zenker diverticulum Cervical osteophytes, cricopharyngeal bar, proximal esophageal webs Oropharyngeal tumors Postsurgical or radiation changes Pill-induced injury Motility disorders Upper esophageal sphincter dysfunction ESOPHAGEAL: 1. Mechanical obstruction Mechanical obstruction Solid foods worse than liquids Schatzki ring Intermittent dysphagia; not progressive Peptic stricture Chronic heartburn; progressive dysphagia Esophageal cancer Progressive dysphagia; age over 50 years Eosinophilic esophagitis Young adults; small-caliber lumen, proximal stricture, corrugated rings, or white papules Motility disorder Solid and liquid foods Achalasia Progressive dysphagia Diffuse esophageal spasm Intermittent; not progressive; may have chest pain Scleroderma Chronic heartburn; Raynaud phenomenon |
|
|
|
What is upper endoscopy?
|
endoscope inserted into mouth and extended to esophagus, stomach, and duodenum
allows for visualization, foreign object removal, stricture dilation, bleeding cauterization, biopsy |
|
|
|
What are the indications for upper endoscopy?
|
GERD
peristent nausea and vomiting unexplained upper abdominal pain foreign body removal dysphagia monitor disease progession or treatment unclear findings on abdominal x-ray, CT, or MRI upper GI bleed |
|
|
|
What and where is virchow's node?
|
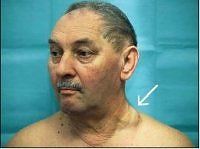
lymph node in left supraclavicular fossa
takes supply from abdominal cavity enlargment is strong indicator of abdominal cancer |
|
|
|
What is the difference between dyspepsia and heartburn?
|
dyspepsia → epigastric pain or burning
heartburn → retrosternal burning often radiating to neck |
|
|
|
What is another name for heartburn?
|
pyrosis
|
|
|
|
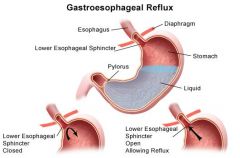
What is GERD?
|
esophageal disorder characterized by reflux of stomach contents into esophagus
|
|
|
|
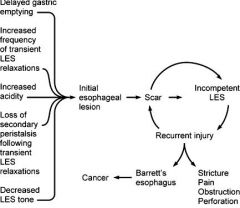
What is the etiology of GERD?
|
impaired lower esophageal sphincter function
worsened by hiatial hernia, diminished peristalsis (scleroderma), diminished salivation (sjogren's, anticholinergics, oral radiation), impaired gastric emptying affects 20% of adults |
|
|
|
What is the clinical presentation of GERD?
|
heartburn → substernal burning, 30-60 minutes following meals or upon bending/reclining, relief with antacids or baking soda
regurgitation dysphagia atypical manifestations include sore throat, chronic cough, non-cardiac chest pain, asthma, chronic laryngitis physical exam normal!!! |
|
|
|
What are the complications of GERD?
|
reflux esophagitis (1/3 of patients)
Barrett's esophagus |
|
|
|
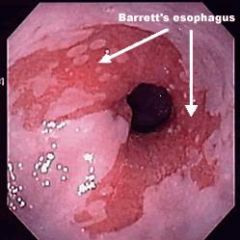
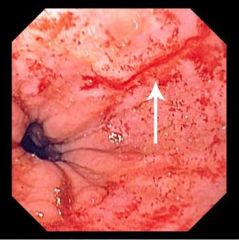
What is Barrett's esophagus?
|
complication of GERD where squamous epithelium of esophagus is replaced by metaplastic columnar epithelium containing columnar and goblet cells
|
|
|
|
What is the etiology of Barrett's esophagus?
|
chronic GERD (occurs in <10% of GERD patients)
|
|
|
|
What is the diagnostic workup of Barrett's esophagus?
|
endoscopy → orange gastric type epithelium that extends from stomach to distal esophagus in tongue-like or circumferential fashion
biopsy |
|
|
|
What is the clinical presentation of Barrett's esophagus?
|
chronic GERD → heartburn, regurgitation
|
|
|
|
What is the management of Barrett's esophagus?
|
1. long-term PPI → 1-2x daily
2. monitor with endoscopy every 3 years |
|
|
|
What are the complications and prognosis of Barrett's esophagus?
|
esophageal adenocarcinoma
though number of patients who progress to adenocarcinoma is small if treat with PPIs and surveillance |
|
|
|
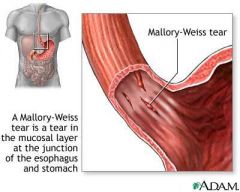
What is Mallory-Weiss Syndrome?
|
mucosal tear at gastro-esophageal junction
|
|
|
|
What is the etiology of Mallory-Weiss Syndrome?
|
sudden increase in trans-abdominal pressure → lifting, stretching, vomiting, retching, straining
|
|
|
|
What is the clinical presentation of Mallory-Weiss Syndrome?
|
history of vomiting, retching, straining
self-limited hematemesis +/- melena |
|
|
|
What is the diagnostic workup of Mallory-Weiss Syndrome?
|
upper endoscopy → 0.5-4cm linear mucosal tear in gastroesophageal junction or in gastric mucosa
|
|
|
|
What is the management of Mallory-Weiss Syndrome?
|
1. bleeding often self-limiting and no therapy required
2. if bleeding continues → endoscopic hemostatic therapy → can inject epinephrine, compress artery with endoclip, or cauterize 3. if endoscopic therapy fails → angiographic arterial embolization or surgery 4. fluid replacement and blood transfusions as needed |
|
|
|
What are the risk factors for Mallory-Weiss Syndrome?
|
alcoholism
|
|
|
|
What are the complications of Mallory-Weiss Syndrome?
|
35% complicated with peptic ulcer disease, erosive gastritis, AV malformations, esophageal varices
higher risk of continued bleeding if portal HTN |
|
|
|
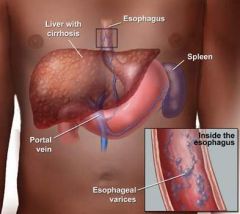
What are esophageal varices?
|
dilated submucosal veins in the esophagus
|
|
|
|
What is the etiology of esophageal varices?
|
secondary to portal HTN
causes of portal HTN include cirrhosis |
|
|
|
What are the risk factors of esophageal varices?
|
alcoholism
|
|
|
|
What is the clinical presentation of esophageal varices?
|
upper GI bleed (33%)
hypovolemia (manifests with postural vital signs or shock) *varices do not cause dysphagia or dyspepsia |
|
|
|
What is the diagnostic workup of esophageal varices?
|

upper endoscopy
|
|
|
|
What is the management of esophageal varices?
|
HOSPITALIZATION:
1. bleeding often self-limited (50%) but can be life-threatening 2. rapid fluid replacement and blood transfusions 3. if platelet count <50,000/mcL or INR >2.0 → platelets or FFP 4. prophylactic antibiotics 5. vasoactive drugs to reduce portal HTN 6. if abnormal PT → subcutaneous vitamin K 7. endoscopy -active bleeding requires intubation -banding or sclerotherapy -banding is first-line -banding must be repeated every 1-3 weeks until obliterated -sclerotherapy often done when active bleeding present, then banding done after 8. if bleeding not controlled by above → consider balloon tube tamponade, portal decompression, shunt 9. prevention of rebleeding → B-blocker, liver transplant |
|
|
|
What is the prognosis of esophageal varices?
|
if no treatment → 60% chance of recurrent bleeding within 6 weeks
risk of bleeding increases if: -large size (>5cm) -endoscopy reveals red whale markings -severe liver disease -active alcoholism advanced liver disease has poor outcome |
|
|
|
What are the complications of esophageal varices?
|
rebleeding
|
|
|
|
What is the most common cause of portal HTN?
|
cirrhosis
|
|
|
|
What is the prevention of esophageal varices?
|
if cirrhosis → endoscopy → B-blocker and/or band ligation depending on results
|
|
|
|
What is Zenker's diverticula?
|
protrusion of pharyngeal mucosa that occurs at the pharyngeal esophageal junction between the inferior pharngeal constrictor and cricopharyngeus
|
|
|
|
What is the etiology of Zenker's diverticula?
|
loss of elasticity of upper esophageal sphincter → restricted opening during swallowing
|
|
|
|
What is the clinical presentation of Zenker's diverticula?
|
insidious onset over years
intially: vague oropharyngeal dysphagia throat discomfort coughing as diverticuum enlarges and retains food: haliotosis regurgitation throat gurgling nocturnal choking neck protrusion |
|
|
|
What is the diagnostic workup of Zenker's diverticula?
|

barium swallow
|
|
|
|
What is the management of Zenker's diverticula?
|
1. if small + asymptomatic → observation
2. if symptomatic → esophageal myotomy +/- surgical diverticulectomy |
|
|
|
What are the complications of Zenker's diverticula?
|
aspiration pneumonia
bronchiectasis lung abscess |
|
|

|
Zenker's diverticulum
|
|
|
|
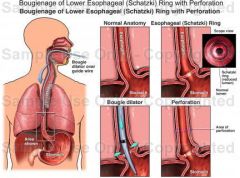
What is Schatzke's ring?
|
smooth, thin (<4mm), circumferential mucosal structure in distal esophagus at squamocolumnar junction
|
|
|
|
What is the etiology of Schatzke's ring?
|
associated with GERD, hiatal hernia
|
|
|
|
What is the clinical presentation of Schatzke's ring?
|
dysphagia → occurs with solid food (think steak), intermittent, not progressive
may pass after drinking fluids or regurgitation |
|
|
|
What is the diagnostic workup of Schatzke's ring?
|

barium swallow
|
|
|
|
What is the management of Schatzke's ring?
|
1. bougie dilator or endoscopic surgical incision of ring
2. if repeated dilation required or heartburn → PPI |
|
|
|
What is achalasia?
|
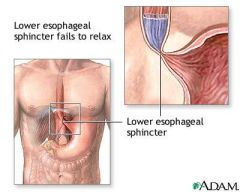
disorder of esophagus characterized by non-peristaltic esophageal contractions and impaired relaxation of lower esophageal spincter
|
|
|
|
What is the etiology of achalasia?
|
cause unusually unknown
associated with degeneration of postganglionic inhibitory neurons in myenteric plexus that release nitric oxide and VIP causes include genetics, Trypanosoma cruzi (organism that causes Chagas disease), carcinoma, and possibly viral or autoimmune rare most common in 25-50y/o |
|
|
|
What is the clinical presentation of achalasia?
|
dysphagia → esophageal, localized to lower chest, both food and liquids, worsens with hurried eating or emotional stress, slowly progressive
common complaints → taking longer to eat, having to drink lots of fluids to clear food, having to stand up and arch back or strain to clear food regurgitation → food non-digested, non-acidic, non-bilious, white and foamy, make wake up at night coughing or choking history of pneumonia mild weight loss |
|
|
|
What is the diagnostic workup for achalasia?
|
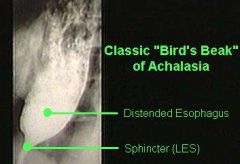
barium swallow → dilation and "bird-beaking" (smooth symmetrical narrowing) of distal esophagus, no peristaltic activity, poor esophageal emptying
esophageal manometry → no peristalsis + incomplete relaxation of lower esophageal sphincter on swallowing |
|
|
|
What is the management of achalasia?
|
surgical myotomy
pneumonic dilation botulin injections for symptoms → sublingual nitrogen, CCBs, phophodiesterase inhibitors, anticholinergics |
|
|
|
What are the complications and pronosis of achalasia?
|
severe weight loss if untreated
respiratory complications like stridor post-botulin injections → recurrence post-myotomy → GERD, strictures, Barrett's esophagus |
|
|
|
What is the prevention for Barrett's esophagus?
|
manage GERD appropriately
|
|
|

|
Barrett's esophagus
|
|
|

|
bird-beaking of achalasia
|
|
|

|
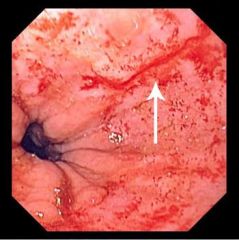
esophageal varices
|
|
|

|
candidal esophagitis
|
|
|

|
schatzke's ring
|
|
|
|
mallory-weiss tear
|
|
|
|
What is the diagnostic workup of GERD?
|
labs normal
initial endoscopy not indicated if typical symptoms suggestive of non-complicated GERD |
|
|
|
What is the management of GERD?
|
1. if typical symptoms → empiric therapy with PPI (omeprazole 20mg PO daily) 30 min before breakfast x 4-8 weeks
2. if alarm features (dysphagia, odynophagia, weight loss, iron deficiency anemia) or non-responsive to PPI → upper endoscopy with biopsy 3. appropriate counseling |
|
|
|
What is the patient education and prevention of GERD?
|
1. avoid coffee, alcohol, citrus fruit, tomatoes, spicy foods, fatty foods, chocolate, peppermint
2. stop smoking 3. eat smaller meals 4. avoid lying down within 3 hours of eating 5. elevate head of bed 6 inches 6. take antacids before meals or to relieve symptoms → quick onset, provide relief for <2 hours 7. take OTC H2-receptor antagonists before meals or to relieve symptoms → slow onset (30 minutes), provide relief for 8 hours |
|
|
|
What is dyspepsia?
|
1. acute, chronic or recurrent discomfort or pain in the epigastric region
2. epigastric pain or burning, early satiety or postprandial fullness |
|
|
|
What is the etiology of dyspepsia?
|
eating fatty foods, eating too quickly, overeating, eating during stressful situations
excessive coffee or alcohol consumption lactose intolerance medications → iron, aspirin, NSAIDs, opioids, antibiotics (metronidazole, macrolides), antihypertensives (ACE inhibitors, ARBs), cholesterol-lowering agents (niacin, fibrates), digoxin, DM (metformin), corticosteroids, estrogen, SSRIs, serotonin-norepinephrine reuptake inhibitors, cholinesterase inhibitors, parkinson drugs pregnancy functional dyspepsia GERD peptic ulcer disease diabetic gastroparesis malabsorption conditions parasitic infection (Giardia, Strongyloides) pancreatic carcinoma chronic pancreatitis MI paraesophageal hernia gastric volvulus intra-abdominal malignancy CKD DM thyroid disease occurs in 25% of adult population accounts for 3% of office visitis |
|
|
|
What are the risk factors for dyspepsia?
|
anxiety, depression, martial problems, employment problems, physical abuse, sexual abuse, history of psychotropic meds
|
|
|
|
What is the clinical presentation of dyspepsia?
|
epigastric pain or burning
early satiety postprandial fullness nausea and vomiting bloating |
|
|
|
What is the diagnostic workup of dyspepsia?
|
1. H. pylori testing
2. CBC, LYTES, Ca2+, HFP, thyroid function tests if >50y/o 2. endoscopy or abdominal imaging if >55y/o, constant or severe pain, weight loss, dysphagia, persistent vomiting, hematemesis, melena, anemia |
|
|
|
What is the management of dyspepsia?
|
1. identify and discontinue offending agents (coffee, alcohol, medications)
2. H. pylori testing → urea breath test, IgG serology or fecal antigen 3. if H. pylori negative → trial empiric PPI x 4 weeks +/- antibiotics 4. if H. pylori positive → antibiotics +/- PPI 5. endoscopy indicated if failure to respond to empiric therapy or relapse 6. if endoscopy normal → diagnose as functional dyspepsia 7. if endoscopy abnormal → treat underlying disorder 8. alternatives include peppermint, caraway, psychotherapy, hypnotherapy |
|
|
|
What is the patient education for dyspepsia?
|
1. reduce or discontinue drinking coffee and alcohol
2. if postprandial symptoms → eat small low-fat meals 3. keep food diary → food intake and symptoms |
|
|
|
What is the prevention of dyspepsia?
|
avoid precipitating factors
|
|
|
|
If H. pylori test negative and patient not taking NSAIDs, peptic ulcer disease can be excluded, true or false?
|
true
|
|
|
|
What is a hiatal hernia?
|
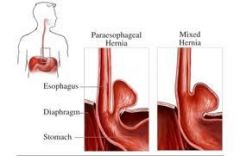
herniation of part of stomach into thoracic cavity through esophageal hiatus in diaphragm
types include sliding, paraesphageal, and mixed |
|
|
|
What is the etiology of a hiatal hernia?
|
cause unknown
associated with aging, obesity, smoking may be congenital very common usually seen in >50y/o |
|
|
|
What is the clinical presentation of a hiatal hernia?
|
asymptomatic
worsening of GERD |
|
|
|
What is the management of a hiatal hernia?
|
1. appropriate GERD management
2. if paraesophageal hernia or non-responsive to GERD management → surgery |
|
|
|
What are the complications of a hiatal hernia?
|
if paraesophageal hernia:
ulceration → bleeding → iron deficiency anemia incarceration strangulation |
|
|
|
What are the risk factors of hiatal hernia?
|
aging, obesity, smoking
|
|
|
|
What is the diagnostic workup of a hiatal hernia?
|

upper endoscopy best for sliding hiatal hernia
barium swallow best for paraesophageal hernia |
|
|
|
What is erosive/hemorrhagic gastritis?
|
damage to stomach lining without inflammation
|
|
|
|
What is the etiology of erosive/hemorrhagic gastritis?
|
alcoholism
NSAIDS portal HTN stress associated with severe illness less common → caustic ingestion, radiation |
|
|
|
What are the risk factors for erosive/hemorrhagic gastritis?
|
if stress associated →
trauma, liver failure, kidney disease, CNS injury, multi-organ failure, burns, coagulopathy, sepsis, shock, mechanical ventilation |
|
|
|
What is the clinical presentation of erosive/hemorrhagic gastritis?
|
often asymptomatic
epigastric pain nausea and vomiting anorexia upper GI bleed → hematemesis (coffee grounds), melena, bloody aspirate from NG suction |
|
|
|
What is the diagnostic workup of erosive/hemorrhagic gastritis?
|
upper endoscopy → subepithelial petechiae, erosions, hemorrhages → vary in size, superificial, focal or diffuse
labs nonspecific → possible anemia |
|
|
|
What diseases comprise inflammatory bowel disease?
|
ulcerative colitis
Crohn's disease toxic megacolon |
|
|
|
What is ulcerative colitis?
|
chronic recurrent inflammatory bowel disease characterized by diffuse mucosal inflammation of the rectum and colon
|
|
|
|
What is Crohn's disease?
|
chronic recurrent inflammatory bowel disease characterized by patchy transmural inflammation of any segment of the GI tract from mouth to anus
|
|
|
|
What part of the GI tract is affected by ulcerative colitis?
|
occurs at rectum and extends proximally to colon
|
|
|
|
What part of the GI tract is affected by Crohn's disease?
|
occurs in patches anywhere from mouth to anus
|
|
|
|
List the extra-intestinal manifestations of ulcerative colitis and Crohn's disease.
|
erythema nodosum
pyoderma gangrenosum episcleritis or uveitis oral ulcers hepatitis sclerosing cholangitis arthritis → oligoarticular or polyarticular, peripheral, non-deforming spondilitis or sacroiliitis thromboembolism |
Current ch15
|
|
|
What is erythema nodosum?
|

inflammatory disorder characterized by red indurated tender subcutaneous nodules
|
|
|
|
Where does erythema nodosum most commonly present?
|
shins
|
|
|

|
erythema nodosum
|
|
|

|
pyoderma gangrenosum
|
|
|
|
What is diverticulosis?
|
GI condition characterized by outpocketings in colon
|
|
|
|
What is the etiology of diverticulosis?
|
usually caused by long-standing fiber deficiency
other causes include inherent weakness in colonic wall or connective tissue disease (scleroderma, Marfan syndrome, Ehlers-Danlos syndrome) possible hereditary factors |
|
|
|
What is the incidence of duverticulosis for <40y/o, 60/yo and 80y/o?
|
<40y/o → <5%
60y/o → 30% 80y/o → >50% |
|
|
|
What is the clinical presentation of diverticulosis?
|
usually asymptomatic and discovered incidentally via colonoscopy or barium enema
may have abdominal pain, chronic constipation, or fluctuating bowel habits physical exam usually normal may have LLQ tenderness with palpable thickened sigmoid and descending colon |
|
|
|
What is imaging modality is most sensitive for detecting diverticulosis?
|
barium enema
|
|
|
|
What is the diagnostic workup of diverticulosis?
|
barium enema most sensitive for detecting diverticulosis
screening labs normal imaging not indicated for diagnosis |
|
|
|
What is the management of diverticulosis?
|
1. high-fiber diet → fruits, vegetables, and whole-grains
2. fiber supplements → bran powder, pysllium, or methylcellulose |
|
|
|
What are the complications of diverticulosis?
|
lower GI bleeding
diverticulitis |
|
|
|
What is the patient education for diverticulosis?
|
1. recommended daily fiber intake:
-38g for men <50y/o -30g for men >50y/o -25g for women <50y/o -21g for women >50y/o 2. increase fiber intake by eating more fruits, vegetables and whole-grains 3. increase fiber intake slowly to prevent gas, cramping, and bloating 4. drink plenty of fluids 5. exercise regularly |
|
|
|
What is the prevention for diverticulosis?
|
eat fiber!
|
|
|
|
What part of the GI tract does diverticulosis affect?
|
nearly always affects sigmoid and descending colon
15% affects proximal colon |
|
|
|
What are the USPSTF and American Cancer Society's screening recommendations for colorectal neoplasms?
|
USPSTF:
1. recommends screening for colorectal cancer via fecal occult blood, sigmoidoscopy, or colonoscopy from 50-75y/o 2. recommendes against screening from 76-85y/o unless specific circumstance 3. recommends against screening >85y/o ACS: Beginning at age 50: Tests that find polyps and cancer •Flexible sigmoidoscopy every 5 years* or •Colonoscopy every 10 years or •Double-contrast barium enema every 5 years* or •CT colonography (virtual colonoscopy) every 5 years* Tests that primarily find cancer •Yearly fecal occult blood test (gFOBT)** or •Yearly fecal immunochemical test (FIT) every year** or •Stool DNA test (sDNA), interval uncertain** if test positive → do colonoscopy for fecal occult blood tests → do series of 3 |
|
|
|
What is pruritus ani?
|
itching of the anogenital area
|
|
|
|
What is the etiology of pruritus ani?
|
contact dermatitis (soaps, colognes, douches, contraceptives, scented toilet paper)
irritating secretions (diarrhea, vaginal discharge, trichomoniasis) infectious disorders (candidiasis, dermatophytosis, erythrasma, pinworms) dermatologic disorders (intertrigo, seborrheic dermatitis , psoriasis, lichen simplex chronicus, lichen sclerosus) hemorrhoids nerve impingement of lumbosacral spine SCC of anus paget disease |
|
|
|
What is the clinical presentation of pruritus ani?
|

anal pruritus
+/- erythema, fissuring, maceration, lichenification, excoriations |
|
|
|
What is the diagnostic workup of pruritus ani?
|
wet mount → trichimoniasis, yeast
stool → pinworms wood lamp → coral red fluorescence with erythrasma spinal radiograph → spinal disease |
|
|
|
What is the management and appropriate referral of pruritus ani?
|
pramoxine cream or lotion
hydrocortisone-pramoxine cream, lotion or ointment capsaicin balneol perianal cleansing lotion tucks premoistened pads, ointment or cream apply after a bowel movement no referral |
|
|
|
What are the complications and prognosis of pruritus ani?
|
often persistent or recurrent
|
|
|
|
What is the patient education of pruritus ani?
|
practice proper anal hygiene
change underwear daily |
|
|
|
What is proctitis?
|
inflammation of anal and rectal mucosa
|
|
|
|
What is the etiology of proctitis?
|
INFECTIOUS:
usually STI via anal intercourse → gonorrhea, chlamydia, syphilis, HSV, condylomata acuminata NON-INFECTIOUS: fissures, fistulas, abscesses, ulcerative colitis, Crohn's disease, colorectal cancer |
|
|
|
What is the clinical presentation of proctitis?
|
anorectal discomfort
tenesmus constipation mucus or bloody discharge other symptoms dependent on etiology |
|
|
|
What is the diagnostic workup of proctitis?
|
dependent on suspected etiology
GCCHDNA RPR HSV culture biopsy for warts |
|
|
|
What is the management, appropriate referral, and patient education for proctitis?
|
dependent on underlying cause
gonorrhea → ceftriaxone chlamydia → doxycycline syphilis → benzanthine penicillin HSV → acyclovir condylomata acuminata → cryosurgery, excision, etc. |
|
|
|
What are the complications and prognosis of proctitis?
|
if untreated → abscesses, strictures, fistulas
|
|
|
|
What is rectal prolapse?
|
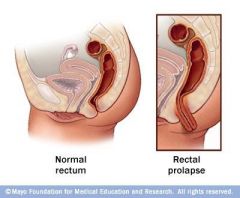
protrusion through the anus of some or all layers of the rectum
|
|
|
|
What is the etiology of rectal prolapse?
|
mucosal prolapse (common):
hemorrhoids full prolapse (uncommon): chronic constipation + weakened pelvic support (especially elderly, paraplegic, psychotic) trauma surgery |
|
|
|
What is the clinical presentation of rectal prolapse?
|

rectal prolapse
intially reduces spontaneously after defecation over time becomes chronically prolapsed mucous discharge bleeding anal sphincter weakness incontinence |
|
|
|
What is the diagnostic workup of rectal prolapse?
|
none
|
|
|
|
What is the management, appropriate referral, and patient education of rectal prolapse?
|
1. manual reduction
2. rectal exam to confirm complete reduction 3. apply lubricant and gauze tape over anal opening for several hours following reduction 4. refer for colonoscopy or surgical consult 5. prevent constipation 6. if severe, cannot be reduced, recurs after reduction, suspected ischemia or necrosis → emergency surgical consult and hospitalization |
|
|
|
What are the complications and prognosis of rectal prolapse?
|
superficial ulceration
venous engorgement thrombosis rectal incarceration, strangulation, ischemia and necrosis |
|
|
|
What is a perirectal abscess?
|
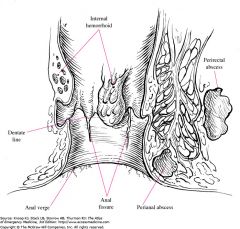
abscess near rectal wall
may be ischiorectal, intersphincteric, or supralevator |
|
|
|
What is the etiology of perirectal abscess?
|
blocked gland
infected fissure STI Crohn's disease (36%) DM leukemia malignancy |
|
|
|
What is the clinical presentation of a perirectal abscess?
|

pain
fever mucous or bloody discharge with bowel movement fluctuant mass palpable along rectal wall |
|
|
|
What is the diagnostic workup of a perirectal abscess?
|
none
|
|
|
|
What is the management, appropriate referral, and patient education of a perirectal abscess?
|
1. if uncomplicated → I&D under local anesthesia
2. if complicated → surgical consult 3. consider admitting if ill-appearing, febrile, elderly, obese, debilitated 4. FU d/t high incidence of fistula |
|
|
|
What are the complications and prognosis of a perirectal abscess?
|
sepsis
high incidence of fistula |
|
|
|
What is an anal fissure?
|
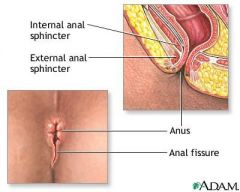
linear or rocket-shaped anal ulcers <5mm in length
|
|
|
|
What is the etiology of anal fissures?
|
trauma during defecation → straining, constipation
if off midline → suspect Crohn's disease, TB, syphilis, HIV, anal carcinoma |
|
|
|
What is the clinical presentation of anal fissures?
|

severe tearing pain during defecation → throbbing discomfort → constipation due to fear of recurrent pain
mild hematochezia → blood on stool or toilet paper anal fissure → looks like crack in epithelium |
|
|
|
What is the diagnostic workup of anal fissures?
|
none
|
|
|
|
What is the management, appropriate referral, and patient education of anal fissures?
|
topical anesthetics → EMLA cream
sitz baths treat constipation → fiber supplements |
|
|
|
What are the complications and prognosis of anal fissures?
|
chronic anal fissures
fibrosis skin tags healing occurs within 2 months recurrence occurs in 40% |
|
|
|
What are hemorrhoids?
|
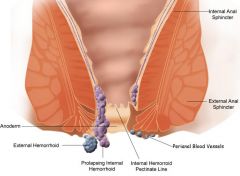
dilated veins in lower rectum or anus
|
|
|
|
What is the etiology of hemorrhoids?
|
straining, constipation, low fiber diet, obesity, pregnancy, prolonged sitting, ulcerative colitis, Crohn's disease
|
|
|
|
What is the clinical presentation of hemorrhoids?
|

discomfort
hematochezia protrusion internal: normally painless (above dentate line → not innervated by cutaneous nerves) but can cause irritation and pruritus if prolapse mucus discharge bleeding external hemorrhoids: visible |
|
|
|
What is the diagnostic workup of hemorrhoids?
|
positive fecal occult blood
anoscopy for internal hemorrhoids hematocrit if excessive bleeding or anemia suspected |
|
|
|
What is the management, referral, and patient education of hemorrhoids?
|
1. treat constipation → high fiber diet, increase fluid intake with meals, bran fiber, commercial bulk laxatives
2. if refractory to above treatment → injection sclerotherapy, rubber band ligation, or application of electrocoagulation 3. if severe bleeding → surgical excision 4. refer if conservative treatment fails or surgery required |
|
|
|
What are the complications and prognosis of hemorrhoids?
|
internal hemorrhoids may become strangulated
external hemorrhoids may become thrombosed recurrence common unless diet altered |
|
|
|
What is the difference between internal and external hemorrhoids?
|
internal hemorrhoids occur above dentate/pectinate line while external hemorrhoids occur below it
|
|
|
|
What are the 4 stages of internal hemorrhoids?
|
•Stage I - Internal hemorrhoids that bleed
•Stage II – Internal hemorrhoids that cause bleeding and prolapse with straining but return to their resting point by themselves •Stage III - Internal hemorrhoids that bleed and prolapse with straining and require manual effort for replacement into the anal canal •Stage IV - Internal hemorrhoids that do not return into the anal canal and are therefore constantly outside |
|
|

|
thrombosed external hemorrhoids
|
|
|
|
What is hepatitis A?
|
acute infectious disease of the liver
|
|
|
|
hepatitis A ETIOLOGY
|
hepatitis A virus (RNA virus)
route of transmission = fecal/oral risk factors = undercooked shellfish, crowding, poor sanitation, IV drugs |
|
|
|
hepatitis A CLINICAL PRESENTATION
|
30 day incubation
more severe in adults than children abrupt or insidious onset prodrome → fatigue, nausea, vomiting, diarrhea or constipation, anorexia, upper respiratory symptoms, myalgia, arthralgia, aversion to smoking low-grade fever jaundice RUQ or epigastric pain → mild, constant, worse with exertion or jarring hepatomegaly and tenderness splenomegaly enlarged cervical and epitrochlear lymph nodes |
|
|
|
hepatitis A DIAGNOSTIC WORKUP
|
WBC → normal to low
markedly elevated AST/ALT proteinuria bilirubinuria elevated AST/ALT → elevated BILI and ALK PHOS positive IgM and IgG |
|
|
|
hepatitis A PREVENTION
|
hepatitis A vaccine
hand washing |
|
|
|
hepatitis A COMPLICATIONS
|
acute cholecystitis
if concomitant hepC → fulminant hepatitis |
|
|
|
hepatitis A PROGNOSIS
|
subsides in 2-3 weeks
complete recovery in 3 months may persist for 1 year does not cause chronic hepatitis |
|
|
|
hepatitis A MANAGEMENT
|
symptomatic:
bed rest if symptoms marked IV 10% glucose if vomiting marked meals as tolerated avoid alcohol, exercise, hepatotoxic drugs HOSPITALIZATION: 1. encephalopathy 2. INR >1.6 3. unable to maintain hydration |
|
|
|
What is the etiology of spontaneous bacterial peritoninitis?
|
absence of apparent intra-abdominal infection
cirrhosis complicated by ascites (20-30%) gram-negative (klebsiella, E coli) gram-positive (strep pneumo, viridans strep, enterococci) NO anaerobic bacteria |
|
|
|
What is the clinical presentation of spontaneous bacterial peritonitis?
|
history of chronic liver disease and ascites
fever abdominal pain signs of chronic liver disease change in mental status sudden worsening of renal function |
|
|
|
What is the diagnostic workup of spontaneous bacterial peritonitis?
|
paracentesis → ascitic fluid
cell count w/ diff → PMN >250 cells/mcL diagnostic BC |
|
|
|
What is the management, referral, and patient education for spontaneous bacterial peritonitis?
|
1. antibiotics if PMN >250 → 3rd generation cephalosporin → cephtriaxone
2. repeat paracentesis after 48 hours → adjust antibiotics if PMN not decreased 3. IV albumin if at risk for kidney injury 4. prevention → ciprofloxacin daily x 1 year |
|
|
|
What are the complications and prognosis of spontaneous bacterial peritonitis?
|
recurrence within 1 year (70%)
kidney injury (40%) → major cause of death 30% mortality (<10% if treated early) |
|
|
|
Define ascites.
|

pathological accumulation of fluid in peritoneal cavity
|
|
|
|
What is alcoholic hepatitis?
|
acute or chronic inflammation and parenchymal necrosis of the liver due to excessive alcohol intake
|
|
|
|
What is the etiology of alcoholic hepatitis?
|
excessive alcohol intake
>80g/day for men |
|
|
|
What is the clinical presentation of alcohol hepatitis?
|
history of >50g alcohol daily x 10 years
recent history of heavy drinking fever nausea anorexia jaundice RUQ pain hepatomegaly and tenderness possible splenomegaly or ascites may be asymptomatic or progress to cirrhosis |
|
|
|
What is the diagnostic workup of alcohol hepatitis?
|
elevated AST → rarely above 300 units/L
AST 2x > ALT elevated ALK PHOS → rarely 3x above normal elevated bilirubin leukocytopenia or leukocytosis folate deficiency anemia hypoalbuminemia prolonged PT |
|
|
|
What is the management, patient education, and referral for alcoholic hepatitis?
|
1. d/c alcohol
2. treat deficiencies if present HOSPITALIZATION: 1. inability to maintain hydration 2. total bilirubin >10mg/dL 3. INR >1.6 4. hepatic encephalopathy |
|
|
|
What are the complications and prognosis of alcoholic hepatitis?
|
reversible but most common cause of cirrhosis
|
|
|
|
What is the prevention of alcoholic hepatitis?
|
avoid alcohol
|
|
|
|
Excessive alcohol can result in?
|
alcoholic hepatitis
fatty liver cirrhosis |
|
|
|
What are the most common causes of cirrhosis?
|
1. alcoholism
2. hepC |
|
|
|
What is fatty liver?
|
abnormal accumulation of triglycerides in hepatic cells
|
|
|
|
What is the etiology of fatty liver?
|
alcoholic fatty liver → excessive alcohol intake
non-alcoholic fatty liver: obesity obstructive sleep apnea hypertriglyceridemia endocrinopathies → DM, Cushing's syndrome, polycystic ovary syndrome, hypopituitarism medications → corticosteroids, TPN poisons starvation and refeeding syndrome risk increased if psoriasis |
|
|
|
What is the clinical presentation of fatty liver?
|
often asymptomatic
mild RUQ pain hepatomegaly |
|
|
|
What is the diagnostic workup of fatty liver?
|
mildly elevated AST/ALT
mildly elevated ALK PHOS AST/ALT ratio >1.0 in non-alcohlic fatty liver liver biopsy → steatosis |
|
|
|
What is the management, patient education, and referral for fatty liver?
|
1. treat underlying cause
2. dietary fat restriction 3. exercise 4. weight loss |
|
|
|
What is metabolic syndrome?
|
obesity
HTN hypertriglyceridemia DM |
|
|
|
*What does the AST/ALT ratio tell you?
|
think alcoholic hepatitis if >2.0
think viral hepatitis if <1.0 |
|
|
|
What is hemocromatosis?
|
autosomal recessive disease characterized by increased iron absorption and subsequent iron overload
|
|
|
|
What is the etiology of hemochromatosis?
|
autosomal recessive genetic disorder → increased iron absorption in duodenum → accumulation of iron (hemosiderin) in pituitary, heart, liver, pancreas, kidneys, adrenals, testes
rarely recognized until 5th decade |
|
|
|
What is the clinical presentation of hemochromatosis?
|
usually asymptomatic
FH or abnormal iron studies onset >50y/o fatigue, arthralgias skin pigmentation, cardiomegaly, hepatomegaly, cirrhosis, DM, impotence, arthritis |
|
|
|
What is the management, patient education, and referral for hemochromatosis?
|
1. avoid dietary iron (red meat), raw shellfish, alcohol, iron supplement, vitamin C
2. therapeutic phlebotomy → 1-2 units weekly 3. liver biopsy to determine if cirrhosis present 4. genetic testing for 1st-degree relatives 5. monitor hct and iron studies |
|
|
|
What are the complications and prognosis for hemochromatosis?
|
CHF
hepatic insufficiency pancreatic insufficiency hypogonadism |
|
|
|
What is the diagnostic workup of hemochromatosis?
|
elevated IRON, TIBC, and FERR
mildly elevated AST and ALK PHOS |
|
|
|
What is Wilson's disease?
|
autosomal recessive disorder characterized by abnormal copper accumulation
|
|
|
|
What is the etiology of Wilson's disease?
|
autosomal recessive genetic disorder → excessiveabsorption of copper in small intestine → decreased secretion of copper by liver → accumulation of copper in liver, brain, kidney, and cornea
usually presents <40y/o |
|
|
|
What is the clinical presentation of Wilson's disease?
|
consider if:
adolescent with hepatitis, splenomegaly, coombs-negative hemolytic anemia, portal HTN, neurological or psychological abnormalities, chronic or fulminant hepatitis |
|
|
|
What is the diagnostic workup of Wilson's disease?
|
↓ serum ceruloplasmin
↑ urinary copper |
|
|
|
What is the management of Wilson's disease?
|
1. restrict dietary copper (mushrooms, organs, shellfish, nuts, chocolate)
2. oral penicillamine 3. refer all patients |
|
|

|
Kaiser-Fleischer brownish ring at rim of cornea → Wilson's disease
|
|
|
|
What is Budd-Chiari syndrome?
|
hepatic vein obstruction
|
|
|
|
What is the etiology of Budd-Chiari syndrome?
|
hereditary or acquired hypercoagulable state → polycythemia vera, myeloproliferative disease, FVL, protein S or C deficiency,
|
|
|
|
What is the clinical presentation of Budd-Chiari syndrome?
|
may be fulminant, acute, subacute, or chronic (usually subacute)
jaundice RUQ pain, hepatomegaly, tenderness splenomegaly ascites |
|
|
|
What is the diagnostic workup of Budd-Chiari syndrome?
|
imaging → occlusion/absence of flow in hepatic vein(s) or inferior vena cava
|
|
|
|
What are the complications of Budd-Chiari syndrome?
|
hepatocellular carcinoma
|
|
|
|
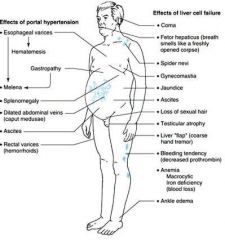
What is the clinical presentation of cirrhosis?
|
|
|
|
|
What is cholelithiasis?
|
gallstones
may be cholesterol or calcium bilirubinate (<20%) |
|
|
|
What is the etiology of cholelithiasis?
|
affect women > men
highest rates if >60y/o, Mexican American, Native American |
|
|
|
What are the risk factors of cholelithiasis?
|
>60y/o
Mexican American Native American obesity, especially women rapid weight loss DM cirrhosis, HepC in men hypertriglyceridemia drugs Crohn's prolonged fasting hormone replacement therapy |
|
|
|
What is the clinical presentation of cholelithiasis?
|
often asymptomatic and discovered incidentally
epigastric or RUQ pain → severe pain, radiation to RT scapula, episodic |
|
|
|
What is the diagnostic workup of cholelithiasis?
|
ultrasound
|
|
|
|
What is the management of cholelithiasis?
|
1. if asymptomatic + no indications for cholecystectomy → lifestyle modifications
2. if asymptomatic + >3cm, Native American, bariatric surgery candidate, heart transplant candidate → cholecystectomy 3. if symptomatic → cholecystectomy 4. if cholecystectomy refused → oral cheno- and ursodeoxycholic acids x 2 years to dissolve stones |
|
|
|
What are the complications and prognosis of cholelithiasis?
|
gallstone ileus
recurrence common in cholecystectomy not performed or ursodeoxycholic acids discontinued |
|
|
|
What is the prevention of cholelithiasis?
|
low-carb diet
physical activity caffeine (women) magnesium and unsaturated fats (men) aspirin, NSAIDs cholecystectomy |
|
|
|
What is cholecystitis?
|
inflammation of the gallbladder
|
|
|
|
What is the etiology of acute cholecystitis?
|
gallstones (90%) → gallstone obstructs cystic duct → inflammation of gallbladder
suspect acalculous cholecystitis if RUQ pain following surgery or in critically ill + no oral intake for prolonged period infection in AIDs patient |
|
|
|
What are the risk factors of acute cholecystitis?
|
gallstones
AIDs surgery or critically ill + no oral intake for prolonged period |
|
|
|
What is the clinical presentation of acute cholecystitis?
|
RUQ or epigastric pain → steady, severe, precipitated by large fatty meal, lasting 12-18 hours
fever nausea and vomiting Murphy sign rebound tenderness palpable gallbladder |
|
|
|
What is the diagnostic workup of acute cholecystitis?
|
CBC → leukocytosis
abdominal x-ray → radiopaque gallstones (15%) RUQ ultrasound → gallbladder wall thickening, pericholecystic fluid, sonographic murphy sign HIDA scan → obstructed cystic duct |
|
|
|
What is the management of acute cholecystitis?
|
HOSPITALIZATION:
1. IV antibiotics 2. analgesics 3. NPO 4. cholecystectomy 5. |
|
|
|
What are the complications and prognosis of cholecystitis?
|
chronic cholecystitis
gangrene of gallbladder |
|
|
|
What is the patient education and prevention of cholecystitis?
|
cholecystectomy
|
|
|
|
HIDA scan only reliable if bilirubin ...
|
<5 mg/dL
|
|
|
|
Chronic Cholecystitis
|
caused by recurrent acute cholecystitis or chronic irritation of gallbaldder by stones
treat with cholecystectomy complications include pancreatitis, gallbladder carcinoma |
|
|
|
What is choledocolithiasis?
|
gallstone in common bile duct
|
|
|
|
What is the etiology of choledocolithiasis?
|
gallstones (15%) → obstruction of common bile duct → biliary pain and jaundice
|
|
|
|
What is the clinical presentation of choledocolithiasis?
|
history of biliary pain or jaundice
RUQ or epigastric pain → sudden onset, severe, radiation to RT scapula fever nausea & vomiting jaundice RUQ tenderness hepatomegaly |
|
|
|
What is the diagnostic workup of choledocolithiasis?
|
increased AST/ALT
increased serum bilirubin bilirubinuria ERCP or PCT |
|
|
|
What is the management of choledocolithiasis?
|
HOSPITALIZATION:
1. assess liver function → correct prolonged PT with IV vitamin K → ERCP → endoscopic sphincterotomy → stone extraction → cholecystectomy |
|
|
|
What are the complications and prognosis of choledocolithiasis?
|
pancreatitis
if obstruction >30 days → cirrhosis → hepatic failure with portal HTN |
|
|
|
What is the patient education and prevention of choledocolithiasis?
|
cholecystectomy
|
|
|
|
What is Charcot triad?
|
classic presentation of cholangitis → biliary pain + fever + jaundice
|
|
|
|
What is cholangitis?
|
infection of the common bile duct
|
|
|
|
What is the etiology of cholangitis?
|
choledocolithiasis
|
|
|
|
What is the clinical presentation of cholangitis?
|
Charcot triad → biliary pain + fever + jaundice
|
|
|
|
What are the diagnostic criteria for cholangitis?
|
Charcot triad (biliary pain + fever + jaundice)
or 2 elements of the Charcot triad + lab evidence of inflammation (elevated WBC, elevated CRP), elevated liver function tests, and evidence of biliary dilation or obstruction |
|
|
|
What is the management of cholangitis?
|
HOSPITALIZATION:
same as choledocolithiasis + IV antibiotics |
|
|
|
What is primary sclerosing cholangitis?
|
diffuse inflammation of the biliary tract leading to fibrosis and strictures
|
|
|
|
primary sclerosing cholangitis ETIOLOGY
|
associated with ulcerative colitis, less with Crohn's
rare men 20-50y/o |
|
|
|
primary sclerosing cholangitis RISK FACTORS
|
ulcerative colitis
Crohn's disease FH smoking = decreased risk |
|
|
|
primary sclerosing cholangitis CLINICAL PRESENTATION
|
progressive jaundice
fatigue, pruritus, indigestion, anorexia symptoms of cholestasis |
|
|
|
primary sclerosing cholangitis DIAGNOSTIC WORKUP
|
elevated ALK PHOS
magnetic resonance cholangiography → segmental fibrosis of bile ducts with saccular dilations between strictures |
|
|
|
primary sclerosing cholangitis MANAGEMENT
|
antibiotics for cholangitis
balloon dilation stenting cancer surveillance liver transplant |
|
|
|
primary sclerosing cholangitis COMPLICATIONS
PROGNOSIS |
osteoporosis
malabsorption of fat-soluble vitamins gallstones etc. cholangiocarcinoma (20%) → CA 19-9 + RUQ US annually for serveillance colorectal cancer if ulcerative colitis → annual colonoscopy 12-17 year survival rate |
|
|
|
What is pancreatitis?
|
inflammation of the pancreas
|
|
|
|
acute pancreatitis ETIOLOGY
|
MOST COMMON:
biliary tract disease alcoholism LESS COMMON: idiopathic genetics abdominal trauma infection hypercalcemia hypertriglyercidemia chylomicronemia vasculitis neoplasma (rare) drugs peritoneal dialysis |
|
|
|
acute pancreatitis RISK FACTORS
|
smoking increases risk of alcoholic and idiopathic causes
older age obesity |
|
|
|
acute pancreatitis CLINICAL PRESENTATION
|
epigastric pain → abrupt onset, steady, severe, boring, deep, radiation to back, history of episodes, associated with heavy meal or alcohol intake, better by sitting and leaning forward, worse by walking or lying down
fever weakness sweating nausea and vomiting hypotension tachycardia pallor, cool clammy skin, mild jaundice abdominal distension and tenderness, guarding, rigidity, rebound |
|
|
|
acute pancreatitis DIAGNOSTIC WORKUP
|
elevated amylase and lipase 3x above normal within 24 hours
lipase more accurate than amylase lipase remains elevated longer than amylase leukocytosis etc abdominal radiographs → possible gallstone, sentinal loop, cutoff sign, |
|
|
|
What are the ranson criteria for acute pancreatitis?
|
3 or more of the following predicts severe course complicated by pancreatic necrosis:
>55y/o WBC >16,000/mcL glucose >200 mg/dL LD >350 units/L AST >250 units/L Worsening prognosis if develop any of the following in the first 48 hours: Hct decreases >10% calcium <8 mg/dL BUN increase >5% arterial PO2 <60 mmHg base deficit >4 mEq/L fluid sequestration >6 L mortality rates based on number of above criteria present: 0-2 = 1% 3-4 = 16% 5-6 = 40% 7-8 = 100% |
|
|
|
What is the clinical significance of the ranson criteria?
|
predicts prognosis and mortality rate of pancreatitis
|
|
|
|
What is pancreatitis?
|
inflammation of the pancreas
|
|
|
|
acute pancreatitis ETIOLOGY
|
MOST COMMON:
biliary tract disease alcoholism LESS COMMON: idiopathic genetics abdominal trauma infection hypercalcemia hypertriglyercidemia chylomicronemia vasculitis neoplasma (rare) drugs peritoneal dialysis |
|
|
|
acute pancreatitis RISK FACTORS
|
smoking increases risk of alcoholic and idiopathic causes
older age obesity |
|
|
|
acute pancreatitis CLINICAL PRESENTATION
|
epigastric pain → abrupt onset, steady, severe, boring, deep, radiation to back, history of episodes, associated with heavy meal or alcohol intake, better by sitting and leaning forward, worse by walking or lying down
fever weakness sweating nausea and vomiting hypotension tachycardia pallor, cool clammy skin, mild jaundice abdominal distension and tenderness, guarding, rigidity, rebound |
|
|
|
acute pancreatitis DIAGNOSTIC WORKUP
|
elevated amylase and lipase 3x above normal within 24 hours
lipase more accurate than amylase lipase remains elevated longer than amylase leukocytosis etc abdominal radiographs → possible gallstone, sentinal loop, cutoff sign, |
|
|
|
What are the ranson criteria for acute pancreatitis?
|
3 or more of the following predicts severe course complicated by pancreatic necrosis:
>55y/o WBC >16,000/mcL glucose >200 mg/dL LD >350 units/L AST >250 units/L Worsening prognosis if develop any of the following in the first 48 hours: Hct decreases >10% calcium <8 mg/dL BUN increase >5% arterial PO2 <60 mmHg base deficit >4 mEq/L fluid sequestration >6 L mortality rates based on number of above criteria present: 0-2 = 1% 3-4 = 16% 5-6 = 40% 7-8 = 100% |
|
|
|
What is the clinical significance of the ranson criteria?
|
predicts prognosis and mortality rate of pancreatitis
|
|
|
|
What is hemolytic uremic syndrome (HUS)?
|
disorder characterized by thrombocytopenia, microangiopathic hemolytic anemia, and renal failure
|
|
|
|
What is the etiology of HUS?
|
associated with E. coli 0157:H7 → produces shiga-like toxin → damages endothelial cells → causing thrombus formation → platelet aggregation → thrombocytosis + microangiopathic hemolytic anemia; commonly affects children
|
|
|
|
What is the clinical presentation of HUS?
|
influenza-like or GI prodrome
bloody diarrhea hematuria oliguria actue renal failure (because kidneys require high volume of blood flow) |
|
|
|
What is the diagnostic work-up of HUS?
|
CBC → anemia, thrombocytopenia
RETIC → high blood smear → schistocytes indirect BILI → high LD → high CREAT → high PT → normal PTT → normal bleeding time → prolonged E. coli O157:H7 → positive |
|
|
|
What are the complications of HUS?
|
permanent kidney damage
death |
|
|
|
What is the managment of HUS?
|
1. hospitalize → observe
2. supportive care 3. dialysis if necessary 4. antibiotics and platelet transfusions contraindicated |
|
|
|
What are the 4 types of diarrhea?
|
secretory
osmotic exudative altered intestinal transit time |
|
|
|
What is the duration for acute and chronic diarrhea?
|
acute <2 weeks
chronic >2 weeks |
|
|
|
Define diarrhea.
|
increased number of bowel movements (>3 per day) or liquidity of feces
|
|
|
|
What is the etiology of acute diarrhea?
|
NON-INFLAMMATORY:
viruses → norovirus, rotavirus (schools, nursing homes, cruiseships) protozoa → giardia lamblia, cryptosporidium, cyclospora non-invasive bacteria: -preformed enterotoxin → s. aureus, b. cereus, c. perfringens -enterotoxin production → v. cholerae, ETEC INFLAMMATORY: viral → CMV protozoa → entamoeba histolytica invasive bacteria → shigella, campylobacter jejuni, salmonella, EIEC, yersinia, listeria, gonorrhea, chlamydia toxin-producing bacteria → CDIF (recent antibiotics), vibrio parahaemolyticus can also be caused by drugs |
|
|
|
What is the clinical presentation of acute diarrhea?
|
<2 weeks in duration
NON-INFLAMMATORY: diarrhea typically mild, large volume stool → watery, non-bloody nausea and vomiting periumbilical cramps and bloating INFLAMMATORY: fever diarrhea typically small volume (<1L/day) stool → bloody, pus LLQ cramps, urgency, tenesmus |
|
|
|
What is the diagnostic workup of acute diarrhea?
|
NON-INFLAMMATORY:
none unless severe or persists >7 days negative fecal leukocytes INFLAMMATORY: positive fecal leukocytes or lactoferrin stool culture O&P E coli 0157:H7 CDIF if risk factors |
|
|
|
What is the management, referral, and patient education for acute diarrhea?
|
NON-INFLAMMATORY:
1. self-limited within 5 days 2. rehydration therapy → 1 liter water, 1 tbsp sugar, 1 tsp salt 3. antidiarrheals → loperamide 4. peptol-bismol → traveler's diarrhea, viral enteritis 5. if persists >7 days → order fecal leukocytes or lactoferrin, stool culture, O&P INFLAMMATORY: 1. do not treat with antidiarrheals 2. antibiotic treatment depends on underlying cause -if empiric → consider if bloody stool, severe fever, tenesmus, fecal lactoferrin (but not due to E coli) -if specific → shigellosis, cholera, extraintestinal salmonellosis, traveler's diarrhea, C difficile infection, giardiasis, and amebiasis HOSPITALIZATION: severe dehydration severe or worsening bloody diarrhea severe or wrosening diarrhea in >70y/o or immunocompromised severe abdominal pain severe infection (high fever, rash, leukocytosis) or sepsis |
|
|
|
What are the complications and prognosis of acute diarrhea?
|
severe dehydration → hypokalemia, metabolic acidosis
toxic colitis sepsis |
|
|
|
Bacteria of >14 days in duration can be caused by bacteria, true or false?
|
false except for CDIF
|
|
|
|
What is the non-pharmacologic management of diarrhea?
|
1. adequate oral fluids with carbs and lytes (oral rehydration solution → 1L water, 1 tbsp sugar, 1 tsp salt)
2. drink tea or flat carbonated beverages 3. eat soft easily digested foods (bananas, applesauce, soup, crackers, toast, rice) 3. avoid fiber, fats, milk products, caffeine, alcohol |
|
|
|
List malabsorption disorders.
|
Whipple's disease
short bowel syndrome celiac sprue |
|
|
|
What is Whipple's disease?
|
rare multisystemic malabsorption disorder caused by bacteria Tropheryma whippelii
|
|
|
|
What is the etiology of Whipple's disease?
|
bacteria Tropheryma whippelii
source of infection unknown commonly affects men 40-70y/o |
|
|
|
What is the clinical presentation of Whipple's disease?
|
arthralgias → migratory, non-deforming, typically first symptom
intermittent low-grade fever abdominal pain distension flatulence chronic diarrhea steatorrhea (excess fat in stool) malabsorption weight loss lymphadenopathy hyperpigmentation of sun-exposed areas peripheral edema |
|
|
|
What is the diagnostic workup of Whipple's disease?
|
possible abnormalities include:
iron deficiency anemia B12/folate deficiency anemia decreased calcium, magnesium, cholesterol, vitamin A, vitamin D hypoalbuminemia increased fecal fat endoscopy → biopsy of duodenum → periodic acid-Schiff (PAS)-positive macrophages with characteristic bacillus confirm by PCR |
|
|
|
What is the management, referral, and patient education for Whipple's disease?
|
1. antibiotics → TMP-SMX x 1 year
2. if severely ill → IV ceftriaxone x 2 weeks, then TMP-SMX x 1 year 3. repeat duodenal biopsy at 6 and 12 months |
|
|
|
What are the complications and prognosis of Whipple's disease?
|
CHF
valvular regurgitation (heart murmur) CNS involvement (lethargy, dementia, myoclonus, seizures, coma recovery in 1-3 months relapse in 33% when d/c treatment |
|
|
|
What is celiac disease?
|
permanent dietary disorder caused by immunlogic response to gluten
|
|
|
|
What is the etiology of celiac disease?
|
autoimmune → immunologic response to gluten → diffuse damage to proximal small intestinal mucosa → malabsorption
1:100 whites |
|
|
|
What is the clinical presentation of celiac disease?
|
symptoms often present for 10 years before diagnosis
weakness abdominal distention chronic diarrhea steatorrhea weight loss muscle wasting growth retardation atypically fatigue, depression, short stature, delayed puberty, amenorrhea, infertility, dermatitis herpetiformis (pruritic papulovesicles over the extensor surfaces of the extremities and over the trunk, scalp, and neck) |
|
|
|
What is the diagnostic workup of celiac disease?
|
SCREENING:
positive IgA endomysial antibody test positive IgA tTG antibody test CONFIRMATION: endoscopy → distal duodenum or proximal jejunum mucosal biopsy increased fecal fat possible abnormalities include: iron, B12, and folate deficiency hypocalcemia mild increased AST/ALT elevated alk phos hypoalbuminemia decreased vitamin A or D prolonged PT |
|
|
|
What is the management, referral, and patient education of celiac disease?
|
1. gluten-free diet → avoid wheat, rye, barley
2. avoid dairy until GI symptoms improve (often lactose intolerant) 3. avoid dietary supplements initially 4. bone scan to assess for osteoporosis → calcium, vitamin D and bisphosphonate if positive 5. monitor IgA endomysial antibody and IgA tTG antibody → negative after 6-12 months of gluten-free diet 6. dietician/support groups |
|
|
|
What are the complications and prognosis of celiac disease?
|
COMPLICATIONS:
associated autoimmune disorders refractory to gluten-free diet PROGNOSIS: excellent improvement within few weeks if strict gluten-free diet |
|
|
|
What is gluten?
|
storage protein found in certain grains (wheat, rhy, barley)
|
|
|
|
What is short bowel syndrome?
|
disorder of malabsorption due to removal of segment of small intestine
|
|
|
|
What is the etiology of short bowel syndrome?
|
surgical resection of small intestine
d/t Crohn's disease, trauma, volvulus, mesenteric infarction, tumor, radiation enteritis |
|
|
|
What is the clinical presentation of short bowel syndrome?
|
symptoms dependent on site and length of resection
terminal ileum → malabsorption of bile salts, vitamin B12, fat-soluble vitamins extensive small bowel → diarrhea, weight loss, |
|
|
|
What is the diagnostic workup of short bowel syndrome?
|
vitamin deficiencies
increased fecal fat |
|
|
|
What is the management of short bowel syndrome?
|
dependent on location and severity of resection:
low-fat diet vitamin B12 IM injections bile salt binding resins vitamins antidiarrheals PPIs parenteral nutrition |
|
|
|
What is the management of laxative abuse syndrome?
|
refer to mental health professional, dietician, and support groups
|
|
|
|
What is the prophylaxis and treatment for traveler's diarrhea?
|
PROPHYLAXIS:
1. not recommended unless comorbidities → heart disease in elderly, IBD, IBS, DM, HIV, immunosuppressant therapy 2. daily ciprofloxacin 3. start upon arrival and continue 1-2 days after leaving 4. not recommended if travel >3 weeks TREATMENT: 1. usually self-limited occuring within 1 week of travel 2. supply traveler in case significant diarrhea develops 3. loperamide → 4mg loading dose then 2mg after each loose stool up to 16mg/day (only if no fever or bloody stool) 4. single oral dose of ciprofloxacin 5. oral rehydration solution |
|
|
|
What is the etiology of traveler's diarrhea?
|
bacteria (80%)
most common → ETEC, shigella, campylobacter jejuni less common → Aeromonas, Salmonella, noncholera vibriones, E histolytica, G lamblia sometimes caused by virus (rotavirus, adenovirus) associated with change in climate, living conditions/sanitation, food/drink, bowel flora |
|
|
|
What is a fecal impaction?
|
large mass of dry hard stool in the rectum due to chronic constipation
|
|
|
|
What is the etiology of fecal impaction?
|
chronic constipation d/t:
colon neurogenic disorders spinal cord disorders severe psychiatric disease prolonged bed rest medications (opioids) |
|
|
|
What is the clinical presentation of fecal impaction?
|
decreased appetitie
nausea and vomiting abdominal pain and distention paradoxical diarrhea (fluids leak around impaction) firm feces palpable on DRE |
|
|
|
What is the management of fecal impaction?
|
enemas (saline, mineral oil, diatrizoate)
digital disruption prevent constipation (stool softeners, regular bowel movements) |
|
|
|
What is the clinical presentation of acute upper GI bleed?
|
hematemesis → bright red or brown "coffee grounds"
melena (usually) hematochezia (if massive bleed) |
|
|
|
What is the etiology of acute upper GI bleed?
|
peptic ulcer disease (80%)
cirrhosis → portal HTN → esophageal varices, gastric or duodenal varices, portal HTN gastropathy (10-20%) mallory-weiss tear (5-10%) vascular anomalies (7%) gastric neoplasms (1%) erosive gastritis erosive esophagitis |
|
|
|
Why should you be wary when ordering a hct if suspect active bleeding?
|
poor early indicator of bleed (just because normal does not mean that there is no blood loss)
takes 24-72 hours to normalize |
|
|
|
What is the management of upper GI bleed?
|
1. 80% self-limited
2. assess hemodynamic status → BP, HR 3. IV fluids 4. labs → CBC, CREAT, liver enzymes, PT/INR, type&screen 5. packed RBCs, platelets, and FFP as needed 6. NG tube 7. endoscopy |
|
|
|
What is the anatomical distinction between upper and lower GI bleed?
|
ligament of Treitz
|
|
|
|
What is the clinical presentation of active lower GI bleed?
|
maroon stool = small intestine or RT colon
hematochezia -bright red streaking = anorectal -bright red large = colon *but remember 10% are d/t massive upper GI bleed |
|
|
|
What is the etiology of active lower GI bleed?
|
if <50y/o:
infectious colitis anorectal disease → hemorrhoids (10%), rectal ulcers (9%) IBD if >50y/o: diverticulosis (50%) malignancy (7%) vascular ectasias (3%) ischemia 20% idiopathic |
|
|
|
What is the management of active lower GI bleed?
|
1. initial management same as upper GI bleed
2. NG aspiration to exclude upper GI source 3. if <45y/o + small volume bleed → anoscopy or sigmoidoscopy 4. if large bleed → colonoscopy 5. nuclear bleeding scan and angiography |
|
|
|
What is an occult GI bleed?
|
bleeding unapparent to patient
|
|
|
|
What is the etiology of occult GI bleed?
|
35-55% upper GI bleed
15-30% colon 1. neoplasm 2. vascular abnormalities 3. acid-peptic lesions → esophagitis, peptic ulcer disease, hiatal hernia erosions 4. infections → TB, hookworm 5. medications → aspirin, NSAIDs 6. IBD |
|
|
|
How is an occult GI bleed detected?
|
fecal occult blood (FOBT, FIT)
iron deficiency anemia in absence of visible blood loss |
|
|
|
What is the management of occult GI bleed?
|
1. if asymptomatic + routine colorectal cancer screening → colonoscopy
2. if symptomatic → upper endoscopy + colonoscopy 3. if <60y/o + still unexplained despite above → further eval of small intestine 4. if >60y/o + still unexplained → empiric trial of iron supplementation → further eval if refractory 5. d/c antiplatelet agents |
|
|
|
What is the pathophysiology of Gilbert's syndrome?
|
familial form of unconjugated hyperbilirubinemia
decreased activity of uridine diphosphate-glucuronyl transferase (which normally conjugates bilirubin) → unconjugated hyperbilirubinemia |
|
|
|
What is the clinical presentation of Gilbert's syndrome?
|
usually asymptomatic
mild jaundice if fasting, exertion, stress, infection unconjugated hyperbilirubinemia normal LFTs |
|
|
|
What is the pathophysiology of hemolysis?
|
increased destruction of RBCs → increase in unconjugated bilirubin → unconjucated hyperbilirubinemia
|
|
|
|
What is the ddx for indirect hyperbilirubinemia?
|
indirect = unconjugated
1. physiologic → neonatal jaundice 2. increased production → hemolytic disorders → sickle cell anemia, G6PD deficiency, hematomas, drug rxn (probenecid, rifampin), transfusion rxn 3. impaired uptake → CHF, drugs, contrast 4. impaired conjugation → Gilbert's syndrome, Crigler-Najjar syndrome |
|
|
|
What is the ddx for direct hyperbilirubinemia?
|
direct = conjugated
1. hepatocellular disease → hepatitis, hemochromatosis, Wilson's disease, acute fatty liver of pregnancy, hepatotoxicity 2. biliary obstruction → choledocolithiasis, cholangitis, primary biliary cirrhosis, pancreatitis 3. congenital disorders → Dubin-Johnson syndrome, Rotor's syndrome |
|
|
|
What is the pathophysiology of jaundice in biliary obstruction?
|
biliary obstruction → impaired flow of bile into intestine → bile contains conjugated bilirubin → conjugated hyperbilirubinemia
|
|
|
|
What is the pathophysiology of jaundice in hepatocellular disease?
|
hepatocellular disease → impaired secretion of conjugated bilirubin into bile → conjugated hyperbilirubinemia
|
|
|
|
List categories of tests to think about when evaluating the liver.
|
1. synthetic liver function
2. excretory liver function and cholestasis 3. hepatocellular injury 4. detoxifying liver function and serum ammonia 5. specific diseases |
|
|
|
What is included in an LFT panel?
|
ALT
AST bilirubin alkaline phosphatase albumin |
|
|
|
What does AST stand for?
|
aspartate aminotransferase
|
|
|
|
What does ALT stand for?
|
alanine aminotransferase
|
|
|
|
What liver tests are used to evaluate plasma protein synthesis?
|
albumin
prealbumin PT/INR (clotting proteins) |
|
|
|
What liver tests are used to evaluate hepatocellular injury?
|
AST
ALT |
|
|
|
What liver test is used to evaluate detoxification?
|
ammonia
|
|
|
|
What liver tests are used to evaluate cholestasis?
|
bilirubin
alkaline phosphatase |
|
|
|
What is albumin?
|
major plasma protein
|
|
|
|
What are the functions of albumin?
|
maintain oncotic pressure
bind and transport anions, FAs, hormones, and drugs |
|
|
|
Why are serum album levels often normal in acute viral hepatitis or drug-related hepatotoxicity?
|
serum albumin half-life = 20 days
complete cessation of albumin synthesis results in only 25% decrease in serum concentration after 8 days thus serum albumin concentrations are slow to fall following injury |
|
|
|
Why are the indications for ordering albumin?
|
measure of protein synthetic function
|
|
|
|
What is the normal range of albumin?
|
3.5-5.5 grams/dL
|
|
|
|
What is the significance of a decreased albumin level?
|
LIVER DYSFUNCTION:
viral hepatitis hepatic cirrhosis toxin ingestion NON-LIVER: malnutrition malabsorption protein loss from gut (nephrotic syndrome) protein loss from kidney (protein-losing enteropathy) protein loss from skin (burns) inflammation (negative acute phase reactant) volume overload (IV fluids) |
|
|
|
What does it mean that albumin is a negative acute phase reactant?
|
in setting of inflammation, liver produces less albumin
|
|
|
|
When does hypoalbuminemia produce symptoms?
|
not until albumin really low (<2-2.5g/dL)
|
|
|
|
What are the symptoms of hypoalbuminemia?
|
peripheral edema
pulmonary edema ascites |
|
|
|
What is the significance of hyperalbuminemia?
|
anabolic steroids
FALSELY ELEVATED: marked dehydration ampicillin heparin |
|
|
|
What is the normal range for prealbumin?
|
19.5-35.8 mg/dL
|
|
|
|
What are the indications for ordering a prealbumin?
|
evaluation of protein nutrition
especially to monitor IV or tube feeding |
|
|
|
Compare albumin and prealbumin.
|
both synthesized by liver
both bind and transport solutes prealbumin → short half life (2 days), levels respond quickly to disease, high % of tryptophan and amino acids albumin → long half life (20 days), levels respond slowly to disease |
|
|
|
What is string sign?
|

1. radiographic sign seen on contrast GI studies
2. indicates narrowing of bowel loop (potentially dispensible or permanently narrowed) 3. usually seen in terminal ileum in Crohn's disease where bowel loop irritability → severe spasm → may lead to fibrosis and permanent narrowing 4. may also be caused by carcinoid, hypertrophic pyloric sphincter |
|
|

|
string sign
|
|
|
|
What is an apple core lesion?
|

1. radiographic sign seen on barium enema
2. usually occur in sigmoid colon, sometimes esophagus 3. appears when mass encircles and narrows a tubular structure of the body 4. often caused by adenocarcinoma or lymphoma |
|
|

|
apple core lesion
|
|
|

|
subdiaphragmatic free air
|
|
|
|
What is subdiaphragmatic free air?
|

1. radiograph sign seen on abdominal x-ray
2. air beneath diaphragm 3. indicates pneumoperitoneum 4. caused by perforation → most often peptic ulcer perforation |
|
|
|
What is a sentinal loop?
|

1. radiographic sign seen on abdominal x-ray
2. isolated distended loop of bowel near site of inflammation/injury 3. body attempts to localize inflammation → distension caused by local paralysis and accumulation of gas |
|
|
|
What is the most common cause of string sign?
|
Crohn's disease
|
|
|
|
What is the normal range for total bilirubin?
|
0.3-1.0 mg/dL
|
|
|
|
What is the normal range for indirect (unconjugated) bilirubin?
|
0.2-0.7 mg/dL
|
|
|
|
What is the norma range for direct (conjugated) bilirubin?
|
0.1-0.3 mg/dL
|
|
|
|
Describe bilirubin metabolism.
|
RBC breakdown in spleen → unconjugated bilirubin released, bound to albumin, and transported to liver → unconjugated bilirubin converted to conjugated bilirubin → conjugated bilirubin secreted into bile and excreted in feces
|
|
|
|
At what total bilirubin concentration does jaundice develop?
|
2-4 mg/dL
*normal 0.3-1.0 mg/dL |
|
|
|
What does the MELD score stand for?
|
model for end-stage liver disease score
|
|
|
|
What does the MELD score consist of and what is its clinical usefulness?
|
Criteria include:
1. serum total bilirubin mg/dL 2. serum creatinine mg/dL 3. INR Clinical usefulness: 1. to determine liver transplant allocation in U.S. 2. to predict mortality in cirrhotic patients undergoing non-transplant surgical procedures -mortality increases 1% for each MELD point up to 20 and 2% for every MELD point over 20 |
|
|

|
colon cut-off sign
|
|
|

|
string of pearls sign (small bowel obstruction)
|
|
|
|
What are the causes of false positive and negative of fecal occult blood?
|
false positive: aspirin, NSAIDs, fish, poultry, red meat, turnips, horseradish
false negative: vitamin C |
|
|
|
What is psyllium?
|
AKA metamucil
bulk-forming laxative used to treat constipation |
|
|
|
What is methycellulose?
|
used to treat constipation
|
|
|
|
When should diarrhea NOT be treated with antidiarrheals?
|
bloody stool
high fever systemic toxicity d/c if worsening diarrhea okay if mild to moderate diarrhea with none of the above |
|
|
|
What is the clinical presentation of laxative abuse syndrome?
|
dehydration
electrolyte imbalance prolonged use causes constipation laxative dependency → larger doses of laxative needed to produce same effect on colon intestinal paralysis, colonic infection, IBS, colon cancer, liver damage bloody stool → anemia if recovering → water retention, edema, weight gain |
|
|
|
Antibiotics are not recommended in diarrhea caused by?
|
salmonella
campylobacter E coli O157:H7 Yersinia Aeromonas |
|
|
|
Why is ipecac no longer used to induce vomiting?
|
only causes partial evacuation
delays or prevents use of activated charcoal increases risk of pulmonary aspiration increases risk of toxic effects on heart |
|
|
|
List type of drugs used to treat diarrhea.
|
antiperistaltic agents
absorbents bismith subsalicylate polycarbophil bile acid sequestrants |
|
|
|
bismuth subalicylate (AKA pepto-bismol)
|
antidiarrheal
MOA: INDICATIONS: symptomatic treatment of mild nonspecific diarrhea adjunct for traveler's diarrhea adjunct for H pylori CONTRAINDICATIONS: children recovering from viral illness due to risk of Reye's syndrome breast feeding ADVERSE EFFECTS: black tongue black stool DRUG INTERACTIONS DOSING: PATIENT EDUCATION: |
|
|
|
List antiperistaltic agents.
|
loperamide
diphenoxylate paregoric |
|
|
|
loperamide
|
antiperistaltic agent
MOA: acts on opioid receptor to inhibit peristalsis and prolong transit time INDICATIONS: chronic diarrhea associated wtih IBD acute nonspecific diarrhea traveler's diarrhea CONTRAINDICATIONS: children <2 breast feeding abdominal pain w/out diarrhea bloody diarrhea diarrhea with high fever acute dysentary bacterial enterocolitis pseudomembranous colitis acute ulcerative colitis ADVERSE EFFECTS: constipation nausea abdominal cramps dizziness DRUG INTERACTIONS DOSING: PATIENT EDUCATION: |
|
|
|
List categories of drugs used to treat constipation.
|
bulk forming agents
surfactants/stool softeners lubricants osmotic agents stimulants enemas sugar alcohol/synthetic sugar |
|
|
|
Castor oil should be avoided in what patient population?
|
pregnant women → may stimulate contractions
|
|
|
|
List bulk forming agents.
|
psyllium
methylcellulose polycarbophil |
|
|
|
Polycarbophil can be used to treat diarrhea and constipation, true or false?
|
true
|
|
|
|
psyllium
|
Bulk-producing laxative
antidiarrheal MOA: Soluble fiber Absorbs water in intestine to form viscous liquid which promotes peristalsis and reduces transit time INDICATIONS: Dietary fiber supplement Treatment of constipation lasting <1 week CONTRAINDICATIONS: Nausea, vomiting, abdominal pain Fecal impaction, GI obstruction Use caution in elderly, swallowing disorders, esophageal disorders ADVERSE EFFECTS: Abdominal cramps, constipation, diarrhea, esophageal or bowel obstruction DRUG INTERACTIONS None DOSING: PATIENT EDUCATION: Take with 8oz water to prevent choking |
|
|
|
What type of drug is docusate?
|
stool softener
|
|
|
|
dronabinol (THC)
|
marijuana derivative
antiemetic appetite stimulant INDICATIONS: chemotherapy-related nausea and vomiting AIDs-related anorexia CONTRAINDICATIONS: hypersensitivity history of schizophrenia, mania, depression caution if elderly, hepatic disease, seizures, history of substance abuse ADVERSE EFFECTS: sedation, dysphoria, vertigo, disorientation, vertigo PATIENT EDUCATION: use caution when performing taks that require mental alertness potential for abuse may cause withdrawl with abrupt discontinuation psychiatric monitoring |
|
|
|
metoclopramide
|
INDICATIONS:
symptomatic treatment of GERD or diabetic gastric stasis MOA: blocks dopamine receptors in CNS blocks seratonin receptors enhances response to Ach in upper GI tract → enhanced motility and accelerated gastric emptying ADVERSE EFFECTS: extrapyrimidal symptoms → restlessness, |
|
|
|
What causes pruritus in patients with liver disease?
|
deposition of bile acids in skin
|
|
|
|
Why does bile acid malabsorption manifest as chronic diarrhea?
|
larger amounts of bile acids than normal enter colon, stimulating water secretion and intestinal motility, causing symptoms of chronic diarrhea
|
|
|
|
What occurs first, jaundice or conjuctival icterus?
|
conjunctival icterus
|
|
|
|
Where does colon cancer most commonly metastasize to?
|
liver
|
|
|
|
Most colon cancers arise from?
|
adenomas
|
|
|
|
Which has a greater risk of malignancy, tubular adenomas or villous adenomas?
|
villous adenomas
|
|
|
|
What are the risk factors for colon cancer?
|
>50y/o
hx of adenomatous poyps - villous > tubular hx of IBD - ulcerative colitis > Crohn's disease positive FH - first-degree relatives |
|

