![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
236 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are mongolian spots?
|
blue macules
|
Fitzpatrick pxxvii
|
|
|
What is alopecia areata?
|
spot baldness
|
|
|
|
How should lesions be described?
|
distribution, configuration, color, secondary changes, primary changes
for example → generalized, discrete, red, scaly papules |
|
|
|
What is alopecia totalis?
|
hair loss from entire scalp
|
|
|
|
What are milia?
|
tiny keratin-filled epidermal cysts
|
|
|
|
What is alopecia universalis?
|
hair loss from entire body
|
|
|
|
MILIA:
|

ETIOLOGY:
dead skin trapped in pockets at surface of skin or mouth CLINICAL PRESENTATION: tiny white bumps (1-2 mm keratin-filled epidermal cysts) found on face, typically nose, cheeks, and chin (in 40% of newborns) found in mouth and called Epstein pearls, typically roof and gums (in 60-85% of newborns) MANAGEMENT: self-limiting → resolves within first few weeks of life |
|
|
|
What are examples of macules?
|
freckles
white macules in vitiligo port-wine stains mongolian spots cafe-au-lait spots erythema |
Fitzpatrick pxxvii
|
|
|
Lichenification is found in what conditions?
|
atopic dermatitis
ezcematous dermatitis psoriasis lichen simplex chronicus mycosis fungiodes |
Fitzpatrick pxxviii
|
|
|
What is acne neonatorium?
|
neonatal acne vulgaris characterized by inflammatory papules and pustules + occasional comedones on face
|
|
|
|
Name 9 dermatological disorders due to fungal infection.
|
tinea capitis
tinea barbae tinea corporis tinea manuum tinea cruris tinea pedis tinea unguium/onychomycosis tinea versicolor candidiasis |
|
|
|
ACNE NEONATORIUM:
|

ETIOLOGY:
cause unknown may be associated with increased sensitivity of fetal sebaceous glands to maternal hormones during pregnancy CLINICAL PRESENTATION: may present at birth but usually develops between 2-4 weeks inflammatory papules and pustules occasionally comedones usually occur on face (in 20% of newborns) MANAGEMENT: self-limiting → resolves within 6-12 months without scarring |
|
|
|
What is urticaria?
|
rash consisting of wheals
|
Fitzpatrick xxviii
|
|
|
List the conditions characterized by dome-shaped vesicles.
|
contact dermatitis
dermatitis herpetiformis |
Fitzpatrick xxix
|
|
|
What is the common name for miliaria?
|
heat rash
|
|
|
|
List the conditions characterized by umbilicated vesicles.
|
herpes simplex
|
Fitzpatrick xxix
|
|
|
MILIARIA:
|
ETIOLOGY:
heat and high humidity → pore closure of eccrine sweat ducts → obstruction of eccrine sweat ducts superficial obstruction in stratum corneum causes miliaria crystallina deep obstruction in epidermis causes miliaria rubra CLINICAL PRESENTATION: miliaria crystalline → grouped, 1-2 mm, superficial clear vesicles miliaria rubra → grouped, deep erythematous papules; may progress to pustules; pruritic both found in intertriginous areas and adjacent skin (neck, upper chest) MANAGEMENT: cool environment to prevent sweating |
|
|
|
List the conditions characterized by flaccid vesicles.
|
pemphigus
|
Fitzpatrick xxix
|
|
|
List transient newborn skin disorders.
|
milia
acne neonatorum miliaria |
|
|
|
List disorders of sebaceous and apocrine glands.
|
acne vulgaris
acne conglobata rosacea perioral dermatitis hidradenitis suppurativa |
|
|
|
ERYTHEMA TOXICUM:
|

ETIOLOGY:
cause unknown associated with eosinophilia more common if full-term CLINICAL PRESENTATION: usually manifests at 24-48 hours but occasionally present at birth 2-3 cm blotchy erythematous macules may progress to wheals in center of macules may progress to pustules range from few to 100 usually occur on chest but also face, back, and extremities MANAGEMENT: self-limiting → resolve within 5-7 days |
|
|
|
What is the epidemiology for rosacea?
|
30-50y/o
females > males 10% of fair-skinned |
Fitzpatrick p9
|
|

|
erythema toxicum
|
|
|
|
What are the symptoms/signs that characterize early rosacea?
|
flushing
telangiectases papules/pustules Fitzpatrick p.9 |
|
|
|
MONGOLIAN SPOTS:
|

ETIOLOGY:
spindle-shaped pigment cells deep in dermis occur in Native American, African American, or Asian descent normal variant CLINICAL PRESENTATION: blue-black macule found in lumbosacral area (and sometimes shoulder, back, or buttocks) MANAGEMENT: none → normal variant, may fade with time |
|
|
|
Where does rosacea occur?
|
face in symmetric pattern
rarely scalp, neck, chest, and back Fitzpatrick p.9 |
|
|

|
mongolian spot
|
|
|
|
What are the symptoms/signs that characterize late rosacea?
|
red facies
dense telangiectases dusky red papules, pustules, nodules Fitzpatrick p.9 |
|
|
|
CAFE AU LAIT MACULES:
|

ETIOLOGY:
increase in melanin content normal variant also consider neurofibromatosis type 1 (if ≥6 lesions >1.5 cm), McCune-Albright syndrome (if large and unilateral), tuberous sclerosis, Fanconi anemia CLINICAL PRESENTATION: light brown oval macule on light skin dark brown oval macule on dark skin found anywhere on body MANAGEMENT: typically none → normal variant, persist throughout life consider NF-1 if multiple present or increase in number |
|
|
|
What are the complications of rosacea?
|
sebaceous hyperplasia and fibrosis
causing disfigurement of the forehead (metophyma), eyelids (blepharophyma), ears (otophyma), nose (rhinophyma), or chin (gnathophyma) Fitzpatrick p.9 |
|
|

|
cafe au lait macules
|
|
|
|
What is rhinophyma?
|
sebaceous hyperplasia and fibrosis of the nose
complication of rosacea |
|
|

|
cafe-au-lait spot
|
|
|
|
Name the types of primary lesions.
|
macule/patch, papule/plaque, wheal, nodule, vesicle/bulla, pustule
|
|
|
|
PORT WINE STAINS:
|

ETIOLOGY:
vascular birthmark d/t permanent vascular abnormalities (dilation) consider Sturge-Weber syndrome (if bilateral facial lesion or covering entire half of face) or Klippel-Trenaunay syndrome (if over extremity) CLINICAL PRESENTATION: dark red macules found anywhere on body MANAGEMENT: laser treatment with pulsed dye laser |
|
|
|
Name the types of secondary lesions.
|
scale, crust, erosion, fissure, ulceration, excoriation, lichenification
|
|
|

|
port-wine stain
|
|
|
|
What is koebner pnenomenon?
|
skin lesion at site of trauma
|
|
|
|
What are port-wine stains?
|
dark red macules d/t permanent vascular abnormalies
|
|
|
|
What is auspitz sign?
|
removal of psoriatic scales that results in pinpoint bleeding
|
|
|
|
HEMANGIOMAS:
|

ETIOLOGY:
benign tumor of capillary endothelial cells CLINICAL PRESENTATION: permanent blanched area of skin at birth evolves into hemangioma at 2-4 weeks red rubbery nodule superficial, deep or mixed MANAGEMENT: 50% reach maximal regression by 5y/o, 70% by 7y/o and 90% by 9y/o redundant skin, hypopigmentation and telangiectasia remain laser therapy with pulsed dye laser may be helpful if ulcerated or bleeding complications requiring immediate treatment with prednisone: 1. visual obstruction 2. airway obstruction 3. cardiac decompensation |
|
|
|
What is nikolsky's sign?
|
slight rubbing of skin that results in sloughing of outermost layer of skin
|
|
|

|
hemangioma
|
|
|
|
Nikolsky's sign may be positive in what conditions?
|
pemphigus vulgaris
bulbous pemphigoid toxic epidermal necrolysis |
|
|

|
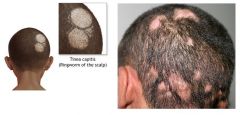
tinea capitis
|
|
|

|
tinea corporis
|
|
|
|
TINEA CAPITIS:
|
ETIOLOGY:
fungal infection of hair and/or scalp caused by Trichophyton tonsurans (90%) or Microsporum canis (10%) CLINICAL PRESENTATION: thickened, broken-off hairs 2-3 mm from follicle leaving “black dot” appearance erythema and scaling of underlying scalp +/- diffuse pustules on scalp +/- boggy fluctuant mass (kerion) on scalp suggesting exaggerated host response MANAGEMENT: 1. wood lamp → Trichophyton tonsurans doesn’t fluoresce, Microsporum canis fluoresces yellow-green 2. KOH 3. fungal culture 4. oral griseofulvin (take with fatty meal to increase absorption) 5. continue fungal cultures every 4 weeks 6. continue medication 4 weeks following negative fungal culture |
|
|
|
What is the treatment for tinea unguium/onychomycosis?
|
1. prescribe terbinafine 250mg tablets PO 1x per day for 6 weeks (fingernails) or 12 weeks (toenails)
2. order HFP mid-way through treatment to screen for hepatotoxicity |
Fitzpatrick p1020
|
|
|
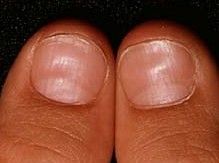
TINEA CORPORIS, CRURIS, PEDIS & UNGUIUM
|

ETIOLOGY:
fungal infection usually caused by Trichophyton mentagrophytes, Trichophyton rubrum, Microsporum canis, Epidermophyton floccosum CLINICAL PRESENTATION: tinea corporis → annular marginated plaques with a thin scale and clear center or annular confluent dermatitis tinea cruris → symmetrical, sharply marginated lesions in inquinal areas tinea pedis → red scaly lesions on soles of feet or fissuring between toes tinea unguium (onychomycosis) → yellowed, thickened, crumbling nails MANAGEMENT: 1. KOH → scrape thin scales from border of lesion, positive for hyphae 2. fungal culture 3. treat tinea corporis, tinea cruris, and tinea pedis with topical → imidazoles, allylamines, benzylamines, or ciclopirox applied twice daily x 3-4 weeks 4. treat tinea unguium with griseofulvin (if refractory, try itraconazole or terbinafine) |
|
|
|
What is the most common cause of acanthosis nigricans?
|
insulin resistance
|
|
|

|
tinea pedis
|
|
|

|
cherry angioma
|
|
|

|
tinea cruris
|
|
|

|
systemic lupus erythematosus
|
|
|

|
tinea corporis
|
|
|

|
xanthomas
|
|
|

|
tinea unguium
|
|
|

|
lyme disease
|
|
|

|
keloid scar
|
|
|

|
contact dermatitis
|
|
|

|
acanthosis nigricans
|
|
|

|
facial telangiectasias → rosacea
|
|
|

|
angiofibromas
|
|
|

|
lichen simplex
|
|
|

|
pitted keratolysis
|
|
|

|
telogen effluvium
|
|
|

|
rosacea
|
|
|

|
eczema herpeticum
|
|
|

|
hidradenitis suppurativa
|
|
|

|
alopecia areata
|
|
|

|
alopecia totalis
|
|
|

|
wheal
|
|
|

|
rhinophyma → rosacea
|
|
|

|
piebaldism
|
|
|

|
ichthyosis
|
|
|

|
ichthyosis
|
|
|

|
bullous pemphigoid
|
|
|

|
acanthosis nigricans
|
|
|

|
livedo reticularis
|
|
|
|
List 1° dermatological lesions.
|
macule, patch, papule, plaque, vesicle, pustule, bulla, nodule, wheal
|
|
|
|
List 2° dermatological lesions.
|
erosion, ulceration, fissure, scale, crust, scar, keloid, atrophy
|
|
|
|
List special dermatological lesions.
|
excoriation, comedone, milia, lichenification, burrow, cyst, telangiectasia, petechiae, purpura
|
|
|
|
What is the ddx for hirsutism?
|
1. idiopathic → hereditary predisposition
2. physiologic → 3rd trimester pregnancy, menopause 3. endocrine disorder → adrenal enzyme deficiency, polycystic ovarian syndrome, cushing's syndrome 4. neoplasm → adrenal (adenoma, adenocarcinoma, ectopic ACTH-secreting tumor), ovarian 5. medications |
Fitzpatrick p990
|
|
|
What are the 3 stages of hair growth?
|
anagen → growth phase
catogen → degenerative phase telogen → resting phase |
|
|
|
*What is anagen and its duration?
|
growth phase of hair growth; 1-6 years depending on site of hair follicle
|
|
|
|
*What is catogen and its duration?
|
degenerative phase of hair growth where growth stops; lasts 1-2 weeks
|
|
|
|
*What is telogen and its duration?
|
resting phase of hair growth where hair sheds; lasts 5-6 weeks
|
|
|
|
Define hirsutism.
|
excessive hair growth (abnormal location) in women in androgen-dependent areas
|
|
|
|
Define hypertrichosis.
|
excessive hair growth (density, length) in non-androgen-dependent areas
|
|
|
|
What systemic disorder is associated with acnathosis nigricans?
|
diabetes mellitus
|
|
|
|
List 5 pigmentation disorders.
|
albinism
piebaldism vitiligo melasma post-inflammatory hypo- or hyperpigmetation |
|
|
|
What is the etiology of albinism?
|
genetic disorder (usually autosomal recessive); characterized by normal number of melanocytes but defective synthesis of melanin
|
Fitzpatrick p341
|
|
|
What is the clinical presentation of albinism?
|

Hair → varies depending on type; white to light brown, red, platinum
Skin → varies depending on type; white to light tan Eyes → iris translucency, decreased retinal pigment, nystagmus, strabismus, photophobia, reduced visual acuity, foveal hypoplasia |
Fitzpatrick p341
|
|
|
What is the management of albinism?
|
sun avoidance, protective clothing, daily sunblock SPF >30 to prevent skin cancer; regular visits to dermatologist and ophthamologist; support group
|
Fitzpatrick p341
|
|
|
What are the complications of albinism?
|
dermatoheliosis
skin cancer → squamous cell carcinoma, basal cell carcinoma, melanoma |
Fitzpatrick p341
|
|
|
What is dermatoheliosis?
|
photo-aging
|
|
|
|
What is melasma?
|
acquired brown hyperpigmentation in sun-exposed areas
|
Fitzpatrick p344
|
|
|
What is the etiology of melasma?
|
caused by sunlight exposure; idiopathic or associated with pregnancy, oral contraceptives, estrogen + progesterone replacement therapy, phenytoin
|
Fitzpatrick p344
|
|
|
What is the clinical presentation of melasma?
|

hyperpigmented brown macules; sharp borders; located in sun-exposed areas, usually face
|
Fitzpatrick p344
|
|
|
What class of drug is phenytoin (dilantin)?
|
anti-epileptic
|
|
|
|
What is the management of melasma?
|
1. may resolve spontaneously months after delivery or cessation of hormones
2. topical → hydroquinone or azelaic acid |
Fitzpatrick p345
|
|
|
What is the patient education for melasma?
|
melasma may or may not return with subsequent pregnancies
|
Fitzpatrick p346
|
|
|
What is the prevention of melasma?
|
daily use of opaque sunblock containing titanium dioxide and/or zinc oxide
|
Fitzpatrick p346
|
|

|
melasma
|
|
|

|
albinism
|
|
|
|
What is vitiligo?
|
acquired depigmentation
|
Fitzpatrick p335
|
|
|
What is the etiology of vitiligo?
|
absence of melanocytes; associated with autoimmune disease, endocrine disease, trauma, infection, stress
|
Fitzpatrick p335
|
|
|
What is the clinical presentation of vitiligo?
|

white macules; sharp borders; symmetric; gradual enlargement of macules or development of new ones; usually generalized
|
Fitzpatrick p335
|
|
|
What is the diagnostic work-up of vitiligo?
|
TSH, T4 → thyroid disease associated with 30% of cases
GLUF → DM associated with 5% of cases |
Fitzpatrick p336
|
|
|
What is the management of vitiligo?
|
1. suncreen SPF >30
2. cosmetic coverup 3. if local → repigmentation via topical glucocorticoids or psoralens + UVA 4. if widespread → repigmentation via oral psoralens + UVA 4. if extensive or failed repigmentation → depigmentation by bleaching |
Fitzpatrick p340
|
|

|
hirsutism
|
|
|

|
vitiligo
|
|
|

|
vitiligo
|
|
|
|
List 5 conditions characterized by scaling lesions.
|
psoriasis
seborrheic dermatitis pityriasis rosea lichen planus icthyosis |
|
|
|
What systemic disorder is associated with xanthomas?
|
hyperlipidemia
|
|
|
|
What systemic disorder is associated with blue-grey macules on the lips?
|
Peutz-Jeghers syndrome
|
|
|
|
Define petechiae.
|

small (<0.3cm) red or purple skin discoloration; non-blanching; indicative of broken capillary
|
|
|
|
Define purpura.
|

medium (0.3-1cm) red or purple skin discoloration; non-blanching
|
|
|
|
Define ecchymosis AKA hematoma AKA bruise.
|
large (>1cm) red or purple skin discoloration; non-blanching
|
|
|
|
What does non-blanchable indicate?
|
blood located outside vessel walls
|
|
|
|
nail pitting
|
psoriasis
alopecia areata (transverse bands) |
|
|
|
splinter hemorrhages
|
if distal: minor trauma, atopic dermatitis, psoriasis
if proximal: sideropenic anemia, bacterial endocarditis, trichinosis, antiphospholipid antibody syndrome, altitude sickness |
|
|
|
Upon palpation of a lesion, what are you assessing?
|
temperature (hot, cold)
depth (dermal, subcutaneous) consistency (soft, firm, hard, fluctuant) mobility tenderness Fitzpatrick xxxiii |
|
|
|
Upon inspection of a lesion, what are you assessing?
|
type
size shape (linear, round, oval, annular, target, serpiginous) color margination (well-defined, ill-defined) number (single, multiple) arrangement (discrete, grouped, confluent) extent of distribution (localized, generalized) pattern of distribution (random, symmetric, sun exposed areas, pressure points, dermatomal) |
|
|
|
Describe a positive auspitz sign.
|
when slight scraping of a scaly lesion reveals bleeding points in lesion
suggestive of psoriasis but non-specific Fitzpatrick xxxv |
|
|
|
Describe a positive Nikolsky sign.
|
when lateral shearing pressure from a finger causes epidermis to dislodge from dermis resulting in an erosion
suggestive of pemphigus, staphylococcal scaled skin syndrome, or toxic epidermal necrolysis Fitzpatrick xxxvi |
|
|
|
Describe a positive Darier sign.
|
when a macule/papule becomes a palpable wheal after being vigorously rubbed w/ an instrument such as the blunt end of a pen
wheal may not appear for 5-10min. Fitzpatrick xxxv |
|
|
|
In dermatology, should the history be taken before or after the physical exam?
|
after
b/c patient's can see skin lesions and thus the history may be flawed w/ their own interpretation of the cause b/c clinician more objective w/out preconceived ideas Fitzpatrick p. xxvi |
|
|
|
What is a macule?
|
circumscribed flat lesion
any size any color non-palpable well or ill-defined Fitzpatrick p. xxvii |
|
|
|
What is diascopy?
|
examination of red skin lesions by pressing glass slide to lesion to determine if blanching (erythema) or non-blanching (purpura) lesion
Steman's & Fitzpatrick p. xxvii, xxxv |
|
|
|
In diascopy, what do blanching lesions indicate?
|
if redness disappears, lesion is due to vascular dilation
Fitzpatrick p. xxvii |
|
|
|
In diascopy, what do non-blanching lesions indicate?
|
if redness remains, lesion is due to extravasated RBCs (i.e. purpuric)
Fitzpatrick p. xxvii |
|
|
|
What are 13 criteria for describing inspection and palpation of skin lesions?
|
type
size shape color margination number arrangement distribution temperature depth consistency mobility tenderness Fitzpatrick p. xxvii, xxxiii |
|
|
|
What is a papule?
|
superficial elevated solid lesion <0.5cm in diameter
flat-topped, dome-shaped, cone-shaped, or vegetation (multiple, small, closely packed) palpable well (superifical) or ill-defined (deeper dermal) Fitzpatrick p. xxvii |
|
|
|
What is a plaque?
|
superficial elevated solid lesion >0.5cm in diameter
plateau-like (large surface area in comparison to height) often well-defined often formed by confluence of papules Fitzpatrick xxviii |
|
|
|
What is lichenification?
|
ill-defined plaque
thickened skin accentuated skin markings Fitzpatrick xxviii |
|
|
|
What is a patch?
|
lesion b/w macule and plaque
barely elevated plaque Fitzpatrick xxviii |
|
|
|
What is a nodule?
|
palpable, solid, round or ellipsoidal lesion that is larger/deeper than a papule
may involve epidermis, dermis, or subcutaneous tissue dome-shaped and smooth, crater-like central depression, or warty soft or hard well (superificial) or ill-defined (deep) Fitzpatrick xxviii |
|
|
|
What is a wheal?
|
elevated papule or plaque
flat or round-topped round, gyrate, or irregular w/ pseudopods (slender extensions from wheal) pale red changes rapidly in size and shape due to shifting edema in papillary body of dermis disappears w/in 24 hours Fitzpatrick xxviii |
|
|
|
What is a vesicle?
|
superficial circumscribed elevated fluid-filled cavity <0.5cm in diameter
dome-shaped, umbilicated, or flaccid subcorneal, epidermal, or epidermal-dermal often transparent roof yellowish (if serum-filled) or red/black (if blood-filled) well-defined Fitzpatrick xxix |
|
|
|
Are well-defined lesions superficial or deep?
|
superficial
Fitzpatrick xxix |
|
|
|
Are ill-defined lesions superficial or deep?
|
deep
Fitzpatrick xxix |
|
|
|
What is a bulla?
|
superficial circumscribed elevated fluid-filled cavity
>0.5cm in diameter dome-shaped, umbilicated, or flaccid subcorneal, epidermal, or epidermal-dermal often transparent roof yellowish (if serum-filled) or red/black (if blood-filled) well-defined Fitzpatrick xxix |
|
|
|
How would you describe the color of a lesion?
|
white, yellow, pink, red, purple, blue, tan, brown, grey, black
uniform or variegated Fitzpatrick xxxiii |
|
|
|
How would you describe the margination of a lesion?
|
well-defined (can be traced w/ pencil) or ill-defined
Fitzpatrick xxxiii |
|
|
|
How would you describe the shape of a lesion?
|
linear
round oval annular (ring-shaped) reticular (net-like) serpiginous (snake-like) umbilicated target/iris Fitzpatrick xxxiii |
|
|
|
What are Blaschko lines?
|
a distribution pattern of skin lesions or pigmentary anomolies
linear on extremities, S-shaped on abdomen, V-shaped on back though to result from genetic mosaicism Stedman's |
|
|
|
How would you describe the arrangement and distribution of lesions?
|
number: single or multiple
arrangement: discrete, grouped, or confluent distribution extent: isolated, localized, regional, generalized, universal distribution pattern: random, symmetric, exposed areas, pressure sites, follicular, dermatomal, following Blaschko lines Fitzpatrick xxxiii |
|
|
|
When using a wood lamp, what does coral red fluorescence indicate?
|
erythrasma
Fitzpatrick xxxv |
|
|
|
When using a wood lamp, what does pinkish-red fluorescent urine indicate?
|
porphyria
Fitzpatrick xxxv |
|
|
|
When using a wood lamp, what does yellow-green fluorescence indicate?
|
dermatophytosis
Fitzpatrick xxxv |
|
|

|
clubbing
|
|
|
|
koilonychia (AKA spooning)
|
|
|

|
pitting
|
|
|

|
Beau's lines
|
|
|

|
onycholysis
|
|
|

|
Terry's nails (AKA white nails)
|
|
|

|
yellow nails
|
|
|

|
splinter hemorrhages
|
|
|

|
half-and-half nails
|
|
|

|
Muehrcke's lines
|
|
|

|
onychomycosis
|
|
|
|
What is the pathophysiology of clubbing?
|
connective tissue enlargement resulting from chronic oxygen deficiency
|
|
|
|
What is the ddx for clubbing?
|
atrioventricular malformations
congenital heart disease endocarditis asbestosis chronic bronchitis COPD pulmonary malignancy cirrhosis inflammatory bowel disease celiac disease fistulas |
|
|
|
What sign tests for clubbing?
|
Schamroth sign
|
|
|
|
How do you perform Schamroth sign?
|
oppose distal phalanges
positive if normal diamond-shaped space b/w phalanges is missing |
|
|
|
What is the ddx for koilonychia (AKA spooning)?
|
trauma
iron deficiency anemia hemochromatosis SLE Raynaud's disease nail-patella syndrome |
|
|
|
What is the ddx for pitting?
|
alopecia areata
psoriasis incontinentia pigmenti reactive arthritis |
|
|
|
What is the ddx for Beau's lines?
|
trauma
severe illness pemphigus Raynaud's disease + cold exposure |
|
|
|
What is onycholysis?
|
detachment of nail from nail bed resulting in white discoloration in affected area
|
|
|
|
What is the ddx for onycholysis?
|
trauma
infection psoriasis hyperthyroidism amyloidosis sarcoidosis connective tissue disorders |
|
|
|
What is the ddx of Terry's nails (AKA white nails)
|
malnutrition
CHF cirrhosis hepatic failure DM hyperthyroidism |
|
|
|
What is the ddx for splinter hemorrhages?
|
trauma
psoriasis bacterial endocarditis (associated w/ fever & heart murmur??) peptic ulcer disease RA SLE antiphospholipid syndrome malignancies pregnancy oral contraceptive use |
|
|
|
What is the ddx of half-and-half nails?
|
renal failure
|
|
|
|
What is the ddx for Muehrcke's lines?
|
hypoalbuminemia 2° to:
malnutrition hepatic disease (liver synthesizes albumin) |
|
|
|
What are the ABCs of potentially cancerous lesions?
|
A → assymetry
B → irregular borders C → color changes D → diameter >6mm E → elevation |
|
|
|
During a skin exam, what are you assessing?
|
color
moisture temperature texture mobility turgor lesions |
|
|
|
List 12 infectious diseases that cause a rash.
|
1. varciella (chickenpox)
2. herpes zoster (shingles) 3. rubeola (measles) 4. rubella (german measles) |
|
|
|
What is the common name for varicella?
|
chickenpox
|
|
|
|
What is etiology of varicella?
|
varicella zoster virus (VZV) AKA HHV-3
spread via respiratory droplets or lesion contact peak age 5-10 year round highly contagious |
Current p1239
|
|
|
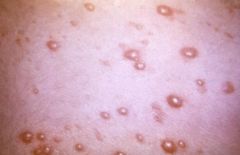
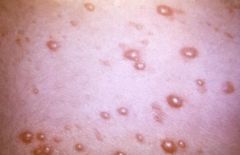
What is the clinical presentation of varicella?
|
10-21 day incubation period
1-3 day prodrome with variable symptoms (mild fatigue, fever, HA, respiratory sxs) red maculopapules → clear vesicles on erythematous base ("dew drop on a rose petal") → pustules (superficial and elliptical with serrated borders) → crusts over 5-6 days affects scalp, face and trunk → extremities lesions can also occur in nose, mouth, conjunctiva, vagina pruritis |
Current p1239
|
|
|
What is the time frame for varicella lesions?
|
new lesions for 1-7 days
crusts slough in 7-10 days |
|
|
|
What is the diagnostic work-up for varicella or herpes zoster?
|
diagnosis usually made clinically; confirmation via DFA or PCR
|
Current p1241
|
|
|
What are the complications of varicella?
|
pitted scars
2° bacterial skin infections → staph, group A strep |
Current p1241
|
|
|
What is the management of varicella?
|
1. acetominphen for fever
2. antihistamines or cool soaks for pruritus 3. acyclovir if chronic disease or immunocompromised 3. keep fingernails short and skin clean to prevent 2° bacterial skin infections and scarring 4. bed rest until afebrile 5. isolation until crusts disappear |
Current p1242
|
|
|
What is the prevention for varicella?
|
vaccination via VARIVAX (varicella only) or MMRV at 12-15 months and 4-6 years
|
Current p1241
|
|
|
When should the MMR and varicella vaccinations be given?
|
12-15 months and 4-6 years
|
Current p1241
|
|
|
varicella
|
|
|
|
What is the common name for herpes zoster?
|
shingles
|
|
|
|
What is the etiology of herpes zoster?
|
varicella zoster virus (VZV) AKA HHV-3; manifests due to prior varicella + declining immunity; usually affects adults >60y/o
|
Current p1239
|
|
|
What is the clinical presentation of herpes zoster?
|

severe pain before onset of rash; lesions resembling chickenpox; dermatomal distribution
|
Current p1241
|
|
|
What dermatomes are most commonly affected in herpes zoster?
|
thoracic and lumbar roots
|
Current p1241
|
|
|
What is the most common complication of herpes zoster?
|
postherpetic neuralgia → 60-70% if >60y/o
|
Current p1241
|
|
|
What is the management of herpes zoster?
|
if uncomplicated → acyclovir 800mg PO 5x daily x 7 days within 72 hours of rash onset
|
Current p1242
|
|
|
What is the prevention for herpes zoster?
|
VZV vaccine at ≥60y/o
|
Current p1241
|
|

|
herpes zoster
|
|
|
|
What is the common name for rubeola?
|
measles
|
|
|
|
What is the etiology of rubeola?
|
caused by a paramixovirus; spread via respiratory droplets; virtually eliminated in U.S.
|
Current 1247
|
|
|
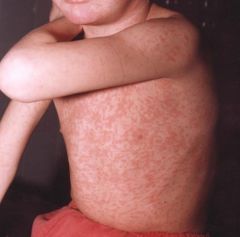
What is the clinical presentation of rubeola?
|
10-14 day incubation period for onset of rash; prodrome of fatigue, fever, conjunctivitis, photophobia, rhinorrhea, cough, Koplik spots; maculopapular rash, 3-4 days after onset of prodrome, brick-red, irregular; face → downward and outward including palms and soles
|
Current 1247
|
|
|
What is the diagnostic work-up of rubeola?
|
usually diagnosed clinically; supported by IgM measles Ab
leukopenia |
Current 1248
|
|
|
What disease are Koplik spots associated with?
|
rubeola
|
Current 1248
|
|
|
What are Koplik spots?
|

prodromic enanthem of rubeola; resemble grains of salt on wet background; found on buccal mucosa
|
|
|
|
"Grains of salt on a wet background" describe?
|

Koplik spots
|
|
|
|
What are the complications of rubeola?
|
1. diarrhea and protein-losing enteropathy → especially significant in malnourished
2. bronchopneumonia or broncholitis 3. secondary bacterial infections 4. encephalitis |
Current p1248
|
|
|
What is the management of rubeola?
|
Supportive:
1. acetominophen for fever 2. vitamin A 200,000 units/d PO x 2 days 3. antibiotics for 2° bacterial infections 4. fluids as necessary 5. bed rest until afebrile 6. isolation for 1 week following onset of rash |
Current p1249
|
|
|
What is the prevention of rubeola, mumps, rubella, and varicella?
|
MMRV vaccine at 12-15 months and 4-6 years
|
Current 1249
|
|

|
koplik spots → rubeola
|
|
|

|
rubeola
|
|
|
|
rubeola
|
|
|
|
What is the common name for rubella?
|
german measles
|
|
|
|
What is the etiology of rubella?
|
caused by a togavirus; spread via respiratory droplets; fetal rubella common in third world countries
|
Current p1254
|
|
|
What is the clinical presentation of rubella?
|
50% asymptomatic
fatigue, fever, rhinorrhea suboccipital, postauricular and posterior cervical lymphadenopathy rash → maculopapular, fine, pink; face → trunk → extremeties; fades quickly lasting 1 day each area if adult → 25% polyarticular arthritis of wrists, fingers, knees for 1 to several weeks |
Current p1254
|
|
|
What is the diagnostic work-up of rubella?
|
IgM Ab, 4-fold rise in IgG Ab, viral PCR, or viral culture
|
Current p1254
|
|
|
What is the procedure for serological testing of rubella on pregnant women?
|
1. rubella ordered to R/O possibility of prenatal infection
2. positive IgG suggests vaccination or past infection 3. positive IgM suggests POSSIBLE current infection but interpret with caution 4. negative IgM and IgG requires clinical observation and serological follow-up |
Current p1254
|
|
|
What are the complications of rubella?
|
congenital rubella → teratogenic → permanent congenital defects, high mortality rate
|
Current p1254
|
|
|
What is the management of rubella?
|
Supportive:
1. acetominophen If prenatal: 1. possible therapeutic abortion |
Current p1254
|
|
|
What are the differences between postnastal and congenital rubella?
|
postnatal → mild, usually lasts 3-4 days
congenital → teratogenic → congenital defects and high mortality rate |
|
|

|
rubella
|
|
|
|
What disease is characterized by rash starting on face and spreading downward and outward to palms and soles?
|
rubeola
|
|
|
|
What disease is characterized by rash starting on trunk and spreading to extremities?
|
varicella
|
|
|
|
What disease is characterized by rash starting on face, then spreading to trunk, then extremeties in quick sucession, lasting 1 day each?
|
rubella
|
|
|
|
What is the etiology of toxic shock syndrome (TSS)?
|
caused by staph aureus toxin; associated with tampon use, abscess, etc.
|
Current p1296
|
|
|
What are 3 disorders caused by S. aureus toxins?
|
1. scalded skin syndrome → affects children
2. toxic shock syndrome → affects adults 3. enterotoxin food poisoning |
Current p1296
|
|
|
What is the clinical presentation of TSS?
|
diffuse "sun burn" rash
desquamation, especially palms and soles, over 1-2 weeks high fever, hypotension, involvement of 3 or more organ systems HA, nonpurulent conjunctivitis, sore throat, vomiting, watery diarrhea, myalgia |
Current p1296
|
|
|
What is the diagnostic work-up of TSS?
|
BC → negative since caused by toxin not systemic infection
vaginal or wound culture |
Current p1296
|
|
|
What is the management of TSS?
|
1. rapid rehydration
2. remove tampon, drain abscess, etc. 3. antibiotics |
Current p1296
|
|
|
What are the complications of TSS?
|
heart failure
kidney failure liver failure shock 15% mortality rate |
Current p1296
|
|
|
What is the prevention of tampon-associated TSS?
|
avoid use of tampons or use less frequently
change tampons often |
|
|
|
What is the etiology of Kawasaki disease?
|
idiopathic; usually affects children 3 months to 5 years, Asians or Pacific Islanders
|
Current p1288
|
|
|
What is the clinical presentation of Kawasaki disease?
|
fever + 4 of the following criteria x 5 days:
1. bilateral nonexudative conjunctivitis 2. mucous membrane changes → swelling and fissuring of lips, erythematous pharnyx, or strawberry tongue 3. peripheral extremity changes → erythema, edema, induration, desquamation 4. polymorphous rash 5. beau lines 6. cervical lymphadenopathy >1.5cm |
Current p1288
|
|
|
What is Kawasaki disease?
|
vasculitis characterized by infiltration of vessel walls with mononuclear cells and later by IgA secreting plasma cells → destruction and aneurysm formation
|
Current p1288
|
|
|
What are the complications of Kawasaki disease?
|
arteritis of the coronary vessels
coronary aneurysm MI |
Current p1288
|
|
|
What is the management of Kawasaki disease?
|
1. IVIG within first 10 days
2. if fever persists → 2nd dose of IVIG 3. if fever persists → methylprednisolone 4. echocardiogram 5. if coronary aneurysm → low-dose aspirin + warfarin 3. if MI → thrombolytics, CABG, PCCI, cardiac transplant 4. regular follow-up with cardiologist → coronary aneurysms may occur at 30-50y/o |
Current p1288
|
|
|
Define arteritis.
|
inflammation of arterial walls
|
|
|

|
kawasaki disease
|
|
|
|
When is varicella no longer contagious?
|
when crusts begin to form
|
|

