![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
220 Cards in this Set
- Front
- Back
|
Differential Dx for:
Sudden painless visual loss |
⋅ Ocular media opacity due to: vitreous hemorrhage or posterior vitreous detachment
⋅ Retinal detachment ⋅ Vascular occlusions: Central retinal vein occlusion, central retinal artery occlusions, transient visual loss (amaurosis fugax), ischemic optic neuropathy (non-artertitic and arteritic) |
|
|
Differential Dx for:
Ocular Pain |
⋅ Orbital: Preseptal cellulitis or orbital cellulitis
⋅ Corneal: microbial keratitis ⋅ Endopthalmitis ⋅ Intraocular: acute angle closure glaucoma |
|
|
Differential Dx for:
Ocular Trauma |
⋅ Open globe injuries: laceration or rupture
⋅ Orbital compartment syndrome ⋅ Burns (chemical, thermal, UV, electrical ⋅ Hyphema ⋅ Superficial injuries: corneal abrasions or foreign bodies |
|
|
Review the clinical presentation of an afferent papillary defect:
|
A.k.a Marcus-Gunn Pupil; because it is an afferent issue, the “bad” eye will not be able to send any signals to the brain. To test for APD: “swinging flashlight test”: light in good eye, both pupils constrict. Without giving pupils a chance to re-dilate, quickly swing the light to the bad eye. Both pupils will dilate because no signals are going to the brain that light is entering the bad eye and there is no consensual constriction of the good eye because there is no signal.
|
|
|
Vitreous
Hemorrage |
Most common: proliferative diabetic retinopathy; also, retinal break w/o detachment, posterior vitreous detachment, retinal detachment, retinal neovascularization following retinal vein occlusion
Blood is trapped, so when looking in the eye, it will be red. Pt will report decreased vision and “floaters”; may also report seeing blood floating down their vision Tx: laser the outer retina so new vessels can’t proliferate |
|
|
Retinal
Detachment |
Pts with peripheral retinal thinning are vulnerable; also, myopia, trauma, prior cataract extraction (once there is a tear in retina, vitreous lodges behind and “pulls” retina off further
In addition to flashes of light and floaters, pt will report a curtain of darkness across vision, starting in the periphery on the side of the detachment; if fovea is included, there will be an afferent pupillary defect Refer to ophthalmologist urgently (b/c photoreceptors in retina will begin to die when detached from the choroid); also try to make sure macula doesn’t detach |
|
|
Retinal
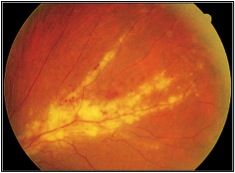
Vein Occlusions |
>50 y.o., HTN, diabetes mellitus, open angle glaucoma; <50 y.o., blood dyscrasias, vasculitis, hypercoagulable conditions, hyperviscosity syndrome
“blood and thunder” appearance in the fundus; sudden, monocular loss of vision Laser neovascularization; treat underlying issues, esp those leading to hypercoagulation. Aspirin tx may be benificial |
|
|
Retinal Artery Occlusions
|
Atherosclerotic thrombosis, embolization, giant cell arteritis White, ischemic retina, small arterioles with a cherry red spot that is the macula; sudden monocular loss of vision; retina will be swollen Inner 2/3 of retina must be perfused or it will die in ~2 hrs; immediate tx: lower IOP, produce arterial dilation by breathing carbogen; medical evaluation to include embolic workup, ESR
|
|
|
Transient Visual
Loss (Amaurosis Fugax) |
May be caused be retinal emboli (if binocular, suggests brain vascular issue); amaurosis fugax usually due carotid artery or cardiac disease Loss of vision lasting a few minutes with complete recovery; will possibly be able to see occluded vasculature in eye exam, but probably not
Reduce risk of stroke via aspirin and other antiplatelet drug and control other vascular issues |
|
|
Ischemic Optic
Neuropathy |
Damage to optic nerve head from microvascular occlusion; non-arteritic: risk factors include HTN, DM, high cholesterol, smoking;
Arteritic: elderly vasculopaths Presents with unilateral optic disc edema and afferent pupillary defect; arteritic ION also will present with v. painful head and jaw, slight or absent pulse in tender temporal artery, severe vision loss, fever, weight loss, malaise, myalgias, temporal headache and HIGH ESR Non-arteritic: visual loss won’t progress and won’t recover, swelling with resolve in 4-8 wks; no effective treatment Arteritic: temporal artery biopsy might be necessary, high doses of systemic steroids (to prevent blindness in other eye); vision won’t be restored |
|
|
Microbial
Keratitis |
Red, painful eye with discrete corneal infiltrate caused by bacteria (P. aeruginosa from contacts), fungus, acanthamoeba, or virus (HSV, etc.) Cornea ONLY: corneal pain caused by loss of epithelial layer; white, blocking infiltrate pus in the cornea and the sclera will be red; HSV will have characteristic “dendritic” ulceration…
Dx what microbe is responsible and treat the microbe. Topical tx are effective. If HSV, oral acyclovir and topical steroids (w/ extreme caution) |
|
|
Endopthalmitis
|
Bactererial, viral, fungal, or parasitic infection of the internal structures of the eye. Usually in the chronically ill, immunosuppressed or diabetic, esp. those with indwelling IV catheters; can also occur as a surgical complication, way after the fact. Ocular pain, injection, visual loss. Eye exam reveals white-centered retinal hemorrhages; super purulent and disgusting.
Tx: none specifically in notes or books, but Current does talk about treating infected eyes with topicals, since contact can be maintained longer (ointments are best, but they blur vision, so solutions are next best) |
|
|
Acute Angle
Closure Glaucoma |
Sudden rise in IOP, b/c the peripheral iris blocks the outflow of aqueous humor via the anterior chamber angle, in susceptible individual with dilated pupil (orientals, Eskimos, hyperopes, elderly; basically, those with shallow anterior chambers)
Severe ocular pain, frontal headache, blurred vision or profound visual loss, colored halos around light, nausea, vomiting; eye will be rock hard (but still mobile in socket), “steamy cornea”, dilated pupil First, tx with a medication to reduce IOP (topical beta blockers, acetazolamide, adrenergic agonists, prostaglandin analogs, pilocarpine). If medicine fails, laser iridotomy (cut a little hole in iris for drainage purposes) |
|
|
Preseptal Cellulitis
compare & contrast management of with orbital cellulitis |
Clinical Presentation
Eyelid edema, chemosis (swollen conjunctiva) **important: NO proptosis, eye WILL have mobility Management: none |
|
|
Orbital Cellulitis
compare & contrast management of with preseptal cellulitis |
Clinical Presentation:
Gross eyelid edema, chemosis, pt is toxic and febrile, proptosis, limited ocular mobility, may have decreased vision Management: Hospitalize, blood cultures, CT of orbits and frontal lobes, IV abx at meningitic doses |
|
|
Corneal abrasions
|
Clinical Presentation:
May result from injury, burn, incorrect contact lens wear and presents with red eye, photophobia, tearing, pain, maybe some blurred vision Management: Dx with fluorescein dye and cobalt blue light (via slit lamp) Tx: cycloplegic (reduces pain by relaxing ciliary body), abx ointment, and a tight patch |
|
|
Foreign bodies
|
Clinical Presentation:
Redness, pain, photophobia, foreign body sensation, can maybe see foreign body in cornea or a rust spot form metal; foreign body might be stuck in lids Management: Anesthetize (w/ proparacaine: don’t give to pt or set the bottle down), then remove foreign body (evert lids and flush or remove with swab), treat as a corneal abrasion: if rust ring, refer to ophthalmologist next day |
|
|
Globe injuries
|
Clinical Presentation:
Reduces visual acuity, reduced IOP (squish eye), change in anterior chamber depth, displacement of pupil, change in pupil shape, visible wound, prolapse of intraocular tissue (BROWN is BAD), marked bloody chemosis Management: Lacerations of cornea or sclera must be sutured; give abx to prevent infxn; patch with “no pressure” patch |
|
|
Chemical burns
|
Clinical Presentation:
Acid damages on contact, but doesn’t penetrate; alkali penetrates deeply and causes damage long after initial contact Management: Immediately irrigate with water or nontoxic liquid for 30 min or until tears are neutral pH; repeat on arrival at medical facility; consult ophthalmology if alkali burn; otherwise, treat as corneal abrasion |
|
|
Hyphema
|
Clinical Presentation:
Blood in anterior chamber (will be able to see it in there) Risk factors for rebleed: sickle cell disease or trait, black race, aspirin use, bad vision, initial hyphema of > 1/3 of anterior chamber; delayed medical attention > 1 day; elevated IOP Management: Medical treatment to prevent rebleeding: corticosteroids, antifibrinolytics; surgical tx to prevent optic nerve and anterior segment damage: paracentesis (to prevent acute IOP), removal of clot. (rebleed can cause intractable glaucoma and permanent visual loss) |
|
|
Discuss the indications for the immediate referral to an ophthalmologist for a patient with ocular trauma:
|
Open globe (brown stuff oozing out, etc), rock hard eyeball that won’t budge in the socket (or just your basic acute increase in IOP), alkali burns, total hyphema, rebleeding, loss of vision
|
|
|
Viral Rhinitis
|
Etiology:
Rhinovirus (30%); Adenovirus and Coronavirus (10-15%); Undetermined (40%); spread by direct contact or respiratory droplets; incubation is 2-4 days and viral shed is up to 3 days Clinical Presentation: Rhinorrhea (clear, watery, but could be green), nasal congestion, sneezing, sore throat, non-productive cough, ear pressure or pain; may see malaise, myalgias, low grade fever, headache; may have mild chest tighness; turbinates are congested/swollen, sticky looking; symptoms usually resolve themselves in 5-8 days Management: Rest and fluids, wait it out; analgesics to relieve fever, headache, myalgias; nasal wash/decongestants for congestion; mucolytics to reduce sputum production; NO ABX!!!!; also, no zinc nasal spray |
|
|
Influenza
|
Etiology:
Influenza A or B transmitted via respiratory droplets; adults are infectious day before and 5 days after onset of symptoms; children infectious several days before and after onset of symptoms Clinical Presentation: Acute onset of high fever, sore throat, retro-orbital headache, myalgias, malaise, non-productive cough; clear nasal discharge, pharyngeal erythema, cervical lymphadenopathy Management: Get thorough hx and PE, because if unusual presentation or in at risk population, can easily develop into bronchial pneumonia; supportive care (rest, antipyretics, fluids), if caught very early, antivirals might be effective; admit to hospital at any sign of compromise |
|
|
Discuss the indications and contraindications for influenza vaccination.
|
⋅ Indications: Although the flu vaccination is recommended for everyone over 6mo, high risk groups and those working with high risk groups are definitely indicated for the flu vaccine. High risk groups include the elderly, residents of long term care facilities, hx of pulmonary disease, hx of cardiovascular disease, pregnant females, immunocompromised;
⋅ Contraindications are mainly for the nasal spray vaccine: no pregnant women, children with hx of wheezing, no elderly, no one with hx of asthma, Guillan Barre syndrome, or an allergy to chicken eggs and basically, no one in the high risk group above; for the flu shot, anyone who has had an adverse rxn before, has an allergy to chicken eggs, or has had Guillan Barre syndrome should not get a flu vaccine. |
|
|
most common pathogens associated with acute sinusitis.
|
Streptococcus pneumoniae, Haemophilus influenzae,
Moraxella catarrhalis |
|
|
clinical presentation, and management of acute sinusitis
|
• Clinical Presentation:
⋅ Prior hx of URI w/ improvement, then relapse and hx of severe allergy exacerbation ⋅ Nasal congestion may follow a cycle ⋅ Purulent nasal discharge w/ turbinate hypertrophy and mucosal erythema and possible hyposmia ⋅ Facial pressure/pain that worsens when bent forward (often a combination of sinuses); sinuses may be tender to the touch ⋅ Postnasal Drip of posterior pharynx – causes “cobblestoning” of pharynx ⋅ Minor factors: halitosis, fever, headache, fatigue (feels bad), dental pain, cough, ear pressure • Management: ⋅ Antibiotic treatment: first line – amoxicillin, cefdinir, or azithromycin (for PCN allergy) for 10-14 day course; second line (for sensitivities or if not responding to first line)– augmentin, trimethropin-sulfamethoxale, or levofloxacin ⋅ Symptom management: hydration, decongestants, mucolytics, analgesics, maybe some topical nasal steroids and antihistamines if there is an allergic rhinitis component |
|
|
most common pathogens isolated in cases of chronic sinusitis
|
S. aureus,
Streptococcus pneumoniae, Haemophilus influenzae, Pseudomonas aeroginosa, anaerobes |
|
|
clinical presentation and management of chronic sinusitis
|
• Clinical Presentation: persistent sinusitis symptoms beyond 3 months – continues nasal congestion w/ purulent discharge and postnasal drip, facial pain/pressure, headache, erythematous nasal mucosa; look closely for deviated septum, nasal polyps, or turbinate edema
• Management: may need to treat allergies and inflammation with maintenance medications – nasal steroids, antihistamines, nasal saline; may need to use second line abx as initial tx |
|
|
Discuss the diagnostic evaluation used in the evaluation of upper respiratory infections, including sinusitis
|
Illness duration (big one), purulence of nasal discharge, facial pain, magnitude of fever
|
|
|
complications associated with sinusitis:
• Osteomyelitis: |
Bone infection that can occur because of infxn in sinuses; along with fever and headache, pt will present with doughy edema over the involved bone (mostly frontal sinus) that is gushy and won’t go away
|
|
|
complications associated with sinusitis:
• Cavernous Sinus Thrombosis |
Infxn spreads through venous channels; pt will be toxic and febrile, with headache, lid edema, ptosis, proptosis, and chemosis; also will have CN III, IV, and VI palsies; pupils are fixed and dilated; eye exam reveals venous congestion and papilledema; altered mental state
|
|
|
complications associated with sinusitis:
• Orbital Cellulitis |
Sinus infxn (most often ethmoid) gets into the orbit; pt will be febrile and look sick, with eyelid edema, ptosis, proptosis, and chemosis; extra-ocular muscle movements may be decreased and pressure on the optic nerve may lead to vision loss
|
|
|
Discuss the indications for referral to otolaryngology
|
Changes in vision, mentation (mental activity), or periorbital edema; also, proptosis
(forward displacement & entrapment of eye from behind lids) |
|
|
Review the retinal structure and function:
Structure |
o Fovea
• Center of Macula • Provides best visual accuity • High concentration of cones => Spatial discrimination • Other retinal layers displaced • Cones synapse directly with neurons • Very little attenuation • No rods • Macula/Fovea pathological changes hinder vision more than peripheral changes o Cones • Color perception and high spatial resolution • ~ 5 million o Rods • Dim (scotoptic) illumination • ~ 100 million o Optic nerve nasal to fovea o Choroid layer – deep to retina; delicate; very vascular; dissipates heat; metabolic exchange |
|
|
Review the retinal structure and function:
Function |
o Takes light signals and converts them into electrical impulses that are then sent to the brain to be interpreted as meaningful vision.
o Similar to film in a camera. |
|
|
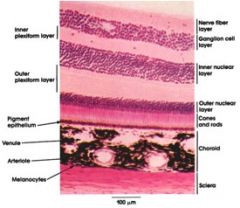
retinal layers card
|
|
|
Review the elements which should be included in a systematic description of the funduscopic examination
|
• Optic disc
o Sharpness or clarity of the disc outline (nasal margin may be blurred) o Color of the disc (yellowish orange to creamy pink) o Size of the central physiologic cup (horizontal diameter is usually less than half the horizontal diameter of the disc o Comparative symmetry of the eyes • Retina o Arteries (light red, 2/3 diameter of veins) o Veins (dark red, larger than arteries) o Follow the vessels peripherally in each of the 4 directions looking for lesions • Fovea and surrounding Macula • Anterior structures o Look for opacities in the vitreous of lens |
|

|
Cotton Wool Spots:
Focal swelling of nerve fiber layer. HTN, Lupus, Pregnancy, HIV retinopathy |
|
|
Exudates :
Lipid/protein. Wet MD, Nonproliferative diabetic retinopathy. |
|
|
Drusen (Dry MD)
Yellow spots. Metabolic waste buildup from atrophied pigmented epithelium. |
|
|
Chorioretinitis
(Uveitis) |
Intraocular inflammation. Primarily immunologic, also infection.
-->Anterior uveitis: inflammatory cells and flare w/in the aqueous; if severe, white cells and fibrin in anterior chamber. -->Posterior uveitis: vitreous; lesions in retina or choroid; fresh lesions yellow, old lesions pigmented. |
|

|
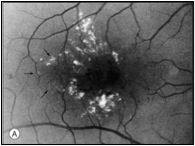
Wet MD
(neovascular) Choroidal vessels grow between the retinal pigment epithelium & Bruch membrane→serous fluid accumulation, hemorrhage, fibrosis. Onset of visual loss more rapid. |
|
|
Discuss the etiology, clinical presentation, and management of age-related macular degeneration
|
• Etiology
o Prevalence increase w/ age; Genetics o Leading cause of permanent visual loss in the older population CP: Central vision loss, Progressive, Usually bilateral Management: :Dry: Vitamins (oral:AREDS (Age-Related Eye Disease Study) Reduces progression, Observation -->Wet – Intravitreal injections • Antibodies against vascular endothelial growth factor (VEGF) Lucentis – studies show to be slightly better FDA approved, $2000/injection -->Avastin: Not FDA approved $40/injection •Inject 0.05 mL. Check pressures and vision post injection. •Stabilization w/ possible improvement |
|
|
Compare and contrast the clinical presentation of dry vs. wet macular degeneration.
|
• Dry
o Drusen – Buildup of metabolic waste products o Pigment epithelium • Normally disposes of old rods and cones • Stops functioning (atrophies) in dry MD => Drusen develops o Distortion of central vision; Gradual onset • Wet o Abnormalities in layers beneath retina down to Choroid => Break o Choroid very vascularized => dissipates heat o Break causes growth of abnormal vessels o Exudates o Onset of visual loss in more rapid and more severe |
|
|
Discuss the use of the Amsler grid for patients with age-related macular degeneration.
|
• Grid paper with a dot in the center.
• Allows pts with AMD to monitor vision changes at home. • Pts cover one eye at a time. • If pt sees abnormalities in the grid, they need to call their health care provider. |
|
|
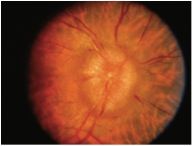
Discuss the etiology and clinical presentation of papilledema.
• Etiology o Bilateral optic disc (nerve head) swelling due to increased ICP (intracranial pressure) • Clinical presentation o Symptoms • Transient visual loss • Blurry vision • Enlarged blind spot o Blurred disc margin o Unable to distinguish complete path of vessels due to inflammation (which causes opacification of layer) of the nerve fiber layer (which is superficial to vessels) o Emergency! Requires immediate ophthalmic or neurologic consult |
|
|
Etiology of unilateral disc swelling
|
o HTN, CRVO (central retinal vein occlusion), pseudopapilledema (drusen), Opticneuritis (frequently seen in MS), DM, TED (thyroid dz)
|
|
|
Describe the retinal abnormalities found in hypertensive retinopathy.
|
-Copper wiring
-Macular star and swollen nerve -Cotton wool spots |
|

|
Copper wiring
Thickening of arterial wall due to high pressure. Able to see vessel wall itself, not just blood within it. |
|

|
Macular star and swollen nerve
|
|

|
Cotton wool spots
Focal swelling of nerve fiber layer. |
|
|
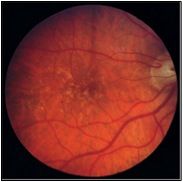
Compare and contrast the retinal abnormalities in proliferative and nonproliferative diabetic retinopathy.
|
• PDR
o Neovascularization arising from either the optic disc or the major vascular arcades o Vitreous hemorrhage common o W/o tx, prognosis is worse than NPDR • NPDR o Dilation of veins, microaneurysyms, retinal hemorrhages, retinal edema, and hard exudates • Clinically Significant Macular Edema (CSME) o Seen in many pts w/ diabetic retinopathy o Swelling in retina • W/ in 500 microns of fovea, or • W/ hard exudates w/in 500 microns, or • One disc area of swelling w/in disc diameter of fovea |
|
|
Discuss the recommendations for screening for patients with diabetic retinopathy.
|
• No DR: Annually
• Mild DR: 9-12 mos • Moderate DR: 6-9 mos • Severe NPDR: 4 mos • PDR: 2-3 mos • CSME: 1-4 mos (variable) |
|
|
clinical presentation of CMV in retina
|
|
|
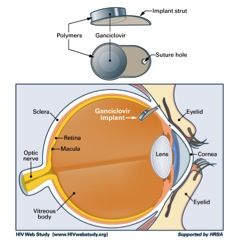
Describe the clinical presentation and management of cytomegalovirus (CMV) retinitis.
|
• Opportunistic virus
• Low CD4 count (<50/mcL) o Uncontrolled HIV o Transplant o Immunosuppressed • Perivascular (follows vessels) whitening of retina and/or hemorrhaging • Management o Ganciclovir o IV, Intravitreous injection, or Implant (good for 8 mos) |
|
|
ganciclovir implant
|
|
|
Discuss the diagnostic studies used in the evaluation of retinal disorders.
|
-->Laser
-->Sodium fluorescence dye -->Direct ophthalmoscope -->Indirect ophthalmoscope -->Optical coherence tomography (OCT) |
|
|
more on Laser therapy
|
Diabetic retinopathy => Kill off peripheral retina so that blood vessels cannot proliferate into center. Sacrifice peripheral retina to save central retina. No laser on optic nerve or macula. Very effective!
|
|
|
More on:
Sodium fluorescence dye |
IV => Visualize vascular
anatomy (inflammation,vessels that shouldn’t be there) |
|
|
Discuss retinal detachment
|
o Very near sighted, trauma, Marfan’s, Family hx, post-cataract surgery
o Vitreous humor normally pushes retina against back of eye (viscous) • Vitreous detachment => Retina detaches when Vitreous humor becomes fluid • Usually not a problem • Volume of fluid is the same • Floating retina may cast shadows • May see floaters |
|
|
Discuss the etiology of hoarseness.
|
-Neoplasms -Allergic rhinitis -reflux
-infections -irritants (like smoking or chemicals) -TVC (true vocal chord) polyps -Voice Strain -Trauma -Neurologic -Endocrine -Medication- ex: steroid inhalers -Lung Disease -Iatrogenic -Other-anatomic -physiologic -congential |
|
|
Symptom-Associated Diagnoses
of Hoarseness |
>Breathiness = Vocal fold paralysis, vocal fold mass lesion
>Vocal fatigue = Vocal fold atrophy or paralysis, neurogenic dysphonia Choking = Vocal fold paralysis, CVA >Odynophonia (pain with talking) = Vocal fold granuloma, >Muscular tension dysphonia (MTD) >Paralaryngeal pain or tension = MTD >Laryngospasm = Gastroesophageal reflux disease, LER (laryngoesophageal reflux), nerve injury Stridor= Bilateral vocal fold paralysis, laryngeal stenosis, paradoxical vocal fold motion >Stridor is a high pitched noise made b/c of Airway narrowing Stridor can be when inspiring(narrowing at vocal chords or above) or expiring (narrowing below vocal chords); Dysphagia= cancer, paralysis, CVA (cerebrovascular accident) >Vocal tremor= Parkinson's disease, spasmodic dysphonia, benign essential tremor, myoclonus >Velopharyngeal insufficiency (VPI) [a nasaly hoarseness]= myasthenia gravis, ALS, vagal paralysis >Globus [feel like have something in back of throat]= LER, neurologic disease |
|
|
Discuss the etiology, clinical presentation, and management of epiglottitis.
|
ETIOLOGY: “can be viral or bacterial in origin”
-H. influenzae type B in children -Multiple organisms in adults Presentation: 2-4 year old BOYS 6-12 hrs history of fever, irritability, dysphonia, and dysphasia No barking cough Unable to tolerate secretions Sitting up in bed (b/c if lying down, couldn’t breathe) Drooling Inspiratory stridor MANAGEMENT: - ABC’s -Secure the Airway (OR) -antiBiotics- cefotaime, ceftriaxone, ampicillin-sulbactam -supportive Care- -prophylax contacts <4 regardless if they have had a HIB vaccination series or not |
|
|
Discuss the etiology, clinical presentation, and management of laryngitis
|
ETIOLGY: can be infectious or non-infectious
Infectious: -viral -Bacterial:-Moraxella catarrhalis -Haemophils influenza Non-infectious: -reflux - neoplasm - vocal cord abuse CP: Recent-onset hoarseness, harsh voice, frequent voice breaks or aphonia, can be asc. with rhinorrhea, cough, and sore throat, and is usu. Self-limiting within 2 weeks MANAGEMENT- supportive care- don’t use voice as could make it worse causing vocal fold hemorrhage, polyps, and cysts) -Hydrate -Cough suppressant (not antihistamine!) -if asc with a URI Decongestant, Treat sinusitis Topical steroids of rhinitis -If caused by bacteria Antibiotics (but be sure its really a bacterial cause b/c don’t want to risk possible superinfection) -If asc with GERD: Acid suppression,Prokinectic agents Diet modification But there is a 2 week referral rule (indicating CHRONIC laryngitis)- if lasting longer than 2 weeks, esp with tmnt tried above, send it to ENT-lots of poss differentials |
|
|
Discuss the etiology and clinical presentation of laryngeal carcinoma
|
ETIOLGY: smoking is most common, is thought to be linked poss to HPV 16 or 18 in non smokers
CP- change in VOICE QUALITY is the most often noticed symptom, Throat or ear pain, Hemoptysis, Dysphagia, Weight loss, Airway compromise Complete head and neck examination, including laryngoscopy >CT or MRI to assess extent of tumor > Biopsy MANAGEMENT- these types of cancer are among the smallest detectable human malignancies and has a very high treatment success Treatment of laryngeal carcinoma has 4 goals: Cure, Preservation of safe effective swallowing Preservation of useful voice Avoidance or a permanent tracheostoma For early glottis and supragolittic cancers, radiation is standard Partial laryngectomy is also well advised ->advanced stages, multimodality therapy- including chemotx |
|
|
Discuss the diagnostic studies used in the evaluation of laryngeal disorders
|
1. History and Physical
2. Throat culture – takes 24 hours, but is more accurate than rapid strep test 3. Rapid Strep Test – results within 1 hour, but will not indicate whether sore throat is caused by a bacterium other than Streptococcus or a virus 4. Monospot Test – if mononucleosis is suspected 5. Airway Evaluation a. Stidor b. Controlling Secretions 6. Indirect Laryngoscopy 7. Oropharyngeal Exam |
|
|
Discuss the indications for referral for the evaluation of hoarseness
|
when evaluating hoarseness, during the H&P find out:
-duration of hoarseness -respiratory symptoms -smoking/drinking habits -previous surgeries -systemic diseases -travel -sick contacts any lasting >2 weeks should be referred to ENT to r/o CA |
|
|
etiology, clinical presentation, and management of:
Deviated nasal septum |
-Congenital
-Trauma Contributors: Sinusitis *NAO Epistaxis CP: OSA A curvature of the septal bone within the nose Could also have face pain, HA, sinusitis, and change in smell Tx: -Septoplasty -Nasal septal reconstruction |
|
|
etiology, clinical presentation, and management of:
Septal perforation |
-cocaine abuse -iatrogenic -occupational (welders)
-trauma, infection -syphillis -leprosy -TB >autoimmune dz -Wegners granulomatosis -Lupus -sarcoidosis -malignancy -hole in the nose! -Whistling in nose -*NAO -Nasal dryness -Nasal crusting [affects about <1% of adult pop.] -Blood work -c-ANCA for Wegners -RPR for syphilis -PPD for TB -biopsy -surgical repair if symptomatic |
|
|
etiology, clinical presentation, and management of:
Septal hematoma |
-nasal trauma
-accidental -iatrogenic [early recognition is KEY b/c this can cause long term deformity] -large, soft dark red or blueish mass -obstruction of one of both nares -suspicion in postop or trauma with progressive nasal obstruction -aspiration -incision and drainage -splints -s. aureus coverage |
|
|
Describe the complications associated with an untreated septal hematoma.
|
-->Septal hematomas appears as a widening of the anterior septum, visible just posterior to the columella
The septal cartilage receives its only nutrition from its closely adherent mucoperichondrium (mucous membrane in nose). Hematomas separates mucopericondrium from the septal cartilage and removes blood supply. Untreated, will result in a saddle nose deformity, performation, or a broadened, fibrotic septum that ends up producing nasal obstruction. They may also get infected with S.aureus most commonly, and should be drained with an incision on both sides. Packing for 2–5 days is often helpful to help prevent re-formation of the hematoma. |
|
|
Septal hematomas appears as a widening of the anterior septum, visible just posterior to the columella (#2 on picture)
|
|
|
Describe the most common etiologic factors associated with epistaxis
|
a. Males more than Females
b. Colder months more than warmer months c. Older people more that younger people (>50 years) d. Local and Systemic |
|
|
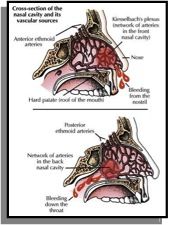
Local Causes of Epistaxis
|
-aneurysm
Causes: #1 digital trauma -nasal foreign body -acute nasal trauma -topical nasal steroids -iatrogenic Meds like NSAIDS, Coumadin, ASA Surgery -chronic cocaine abuse -mucosal inflammation URI, bacterial sinusitis, allergic disease -septal deformity -tumors JNA- exclusively boys <18 years of age- DON’T biopsy! -heredity Hered. Hemorrhagic telangctasias - Irritant or toxic inhalants |
|
|
Systemic Causes of Epistaxis
|
coagulopathy
-atherosclerotic disease -hereditary hemorrhagic telangiectasia -osler-weber-render disease - VWF deficiency -drug induced thrombocytopenia - liver disease - alcohol |
|
|
presentation and management of anterior epistaxis
|
Anterior CP: 82% are this type
You should see the bleeding visibly doing an ant rhinoscopy bleeding often from Kiesselbach’s plexus -->Management: 1.direct pressure on the site by compression of the nares continuously for 15 min (Venous pressure is reduced in the sitting position, and slight leaning forward lessens the swallowing of blood) 2. Short-acting topical nasal decongestants (eg, phenylephrine, 0.125–1% solution, one or two sprays), which act as vasoconstrictors, may also be helpful. 3.When the bleeding does not readily subside, the nose should be examined, using good illumination and suction, in an attempt to locate the bleeding site. Topical 4% cocaine applied either as a spray or on a cotton strip serves both as an anesthetic and a vasoconstrictor. If cocaine is unavailable, a topical decongestant (eg, oxymetazoline) and a topical anesthetic (eg, tetracaine or lidocaine) provide similar results. 4.When visible, the bleeding site may be cauterized with silver nitrate, diathermy, or electrocautery. A supplemental patch of Surgicel or Gelfoam may be helpful with a moisture barrier, such as petroleum-based ointment, to prevent drying and crusting. |
|
|
posterior epistaxis
.management &presentation |
CP: endoscopy- think upper GI issue causing bleeding
Posterior Management: If an anteriorly placed pneumatic nasal tamponade is unsuccessful, it may be necessary to consult an otolaryngologist for a pack In emergency, double balloon packs (Epistat) may facilitate rapid control of bleeding with little or no mucosal trauma. Because such packing is uncomfortable, bleeding may persist, and vasovagal syncope is quite possible, hospitalization for monitoring and stabilization is indicated. Opioid analgesics are needed to reduce the considerable discomfort and elevated blood pressure caused by a posterior pack. Problems that can occur with posterior epistaxis packing: -alar necrosis (side of nostrils part) -columellar necrosis (middle part) -10% can have Toxic Shock syndrome -increase poss. For nocturnal hypoxia -induce or exacerbate OSA (obstructive sleep apnea) -sudden death |
|
|
Further management of epistaxis
|
Surgical management of epistaxis, through ligation of the nasal arterial supply (internal maxillary artery and ethmoid arteries) is an alternative to posterior nasal packing.
After the bleeding has been controlled, don’t pick it!, not do any exercise or anything that could strain the fragile blood vessels, don’t use anything that vasodilates, and rec. moisturizers and humidifiers at home |
|
|
Discuss the prevention of epistaxis.
|
-avoid digital trauma
-moisturizers (suggested vasoline in class) -treat systematic disease -treat hypertension -correct coagulopathy (AKA: bleeding disorders |
|
|
nosebleed
|
|
|
management of cataracts
|
Tx:
Couching- ancient/nonpracticed; involved pushing lens into back of eye with needle Intra-capsular cataract extraction – complete removal of the lens, no longer widely practiced in US because of risk to vitreous body. Manual extra-capsular cataract extraction – aka ‘conventional ECCE’- manual expression of the lens through a 10-12 mm incision in the cornea. Almost complete removal of lens, leave the posterior capsule intact so artificial lens can be put on top of it. Phacoemulsification & extra-capsular cataract extraction – most successful: ultrasonic fragmentation of the lens nucleus and placement of foldable intraocular lenses –performed through very small incision, NO NEED for sutures. Reduces post-op complications & duplications. Artificial intraocular lens implant – placing an artificial lens on the remnant of the former lens Complications: Preop- retrobulbar hemorrhage, eyeball perforation Intraoperative – post capsular rupture, vitreous loss, corneal burn, zonular dehiscence, fragments of lens in vitreous, nucleus drop, suprachroidal hemorrhage, iris prolapse, detachment of Descemet’s membrane, lens position problems. Postop- wound leak, corneal edema, infection, inflammation, astigmatism, high intraocular pressure, lens problems, post capsular opacification**, retinal detachment, vitreous loss, macular edema. |
|
|
etiology, clinical presentation, and management of:
Dacryocystitis |
Infection of lacrimal sac: due to obstruction of nasolacrimal system. Stagnation of tear. Occurs in infants and pts over 40. Acute or chronic.
Acute: Staph. Aureus & β-Hemolytic Strep. Chronic: Stap. epidermidis, anaerobic streptococci, Candida albicans Acute: pain, swelling, tenderness and redness in the tear sac area; prurulent material may be expressed. Chronic: tearing, discharge principle signs. May also have mucus/pus. Hospital if orbital cellulitis Acute: systemic Abx. Surgical relief usually elective, but can be done urgently. →Culture – blood & lacrimal secretions →abx – IV if serious →warm compresses →drainage –if abscess Chronic: kept latent with Abx, but relief from the obstruction is only cure. Steroids, drainage. Dacryocystorhinostomy rarely required but is definitive tx. Dacryocystorhinostomy- standard procedure in adults. Laser assisted endoscopic Dcyst-ostomy& balloon dilation other options. --Congenital obstructions usually resolve spontaneously. Tx can be to probe nasolacrimal system. |
|
|
etiology, clinical presentation, and management of:
Dacryoadenitis |
Viral (common), bacterial/fungal (rare). **Inflammatory causes**: sarcoidosis, Grave’s disease, Sjorgren syndrome, orbital inflammatory disease, beign lymphoepithelial leson Infection and inflammation of lacrimal gland → swollen lacrimal gland Viral – self limiting
Bacterial – 1st gen cephalosporins Protozoan/fungal – antiamoebic, antifungal Inflammatory – investigate for etiology Biopsy if swelling doesn’t subside in 2 weeks |
|
|
etiology, clinical presentation, and management of:
Blepharitis (looks like dandruff of eyelashes) |
Chronic condition.
Anterior- involves eyelid skin,lashes & associated glands Posterior – results from inflammation of meibomian glands. May be bacterial infection esp w/ staph or 1° gland dysfunction Assoc w/ rosacea Bilateral inflammation of lid margins: Burning sensation, watering, injection, foreign body sensation, Anterior: scurf on eye lashes & crust on anterior eye lid. Posterior: turbid fluid on meibomian gland expression or difficulty doing so -Lid hygiene and scrub (baby shampoo on a q-tip) -Eye ointment -Fish oil (for posterior type) -Oral abx (doxycycline) -Steroids |
|
|
etiology, clinical presentation, and management of:
Hordeolum |
Infection of the eye lid.
External: infection of the eye lash follicles (Stye) Internal: infx of meiboman glands Pain Lump Redness Tenderness discharge Self-limited Warm compresses Antibiotics drainage |
|
|
etiology, clinical presentation, and management of:
Chalazion |
Granlunomatous inflammation of meiboman gland may follow internal hordeolum.
Accumulation of lipid in blocked meibomian gland. Hard non-tender swelling on the upper or lower lid no redness/tenderness itself but with redness & swelling of adjacent conjunctiva. If large enough to impress the cornea, vision distorted. -Warm compresses -incision and cutterage -steroid injections may be effective |
|
|
etiology, clinical presentation, and management of:
Ectropion |
Eversion of eye lid, caused from lid laxity /surgery: older people
Lid hanging lower/ gaping Surgery indicated if excess tearing, exposure keratitis, or cosmetic problem |
|
|
etiology, clinical presentation, and management of:
Entropion |
Inversion of eye lid, caused from lid laxity/surgery: older people Redness irritation, tearing Botox for temporary correction
|
|
|
etiology, clinical presentation, and management of:
Xanthelasma |
Most common xanthelomas; older people, asymptomatic Yellow plaques around eye lids/on eye lids No intervention or excision, treat underlying causes (hyperlipidemia) if any
|
|
|
Discuss the diagnostic studies used in the evaluation of lacrimal and eyelid disorders.
|
Dacryocystitis:
Dx Studies: dye disappearance test (for obstruction), XR for foreign bodies/skeletal anomalies, CT for trauma/malignancy, MRI for lacrimal sac diverticulitis, Dacryocystography for anatomical abnormalities Subtraction DCG with CT scan Nasal endoscopy |
|
|
Discuss the indications for referral to an ophthalmologist for management of eyelid disorders
|
Patients with cataract should be referred to an ophthalmologist when their visual impairment adversely affects their everyday activities.
Ophthalmology should be consulted with: →Emergencies include orbital cellulitis, gonococcal keratoconjunctivitis. Preseptal (periorbital) cellulitis usually arises from a local exogenous source such as an abrasion of the eyelid, from other infections (hordeolum, dacryocystitis, or chalazion). →Complications of dacryocystitis could warrant ophthalmology consult: complications include abscess, fistula, periorbital/orbital cellulitis, and cavernous sinus thrombosis. |
|
|
Discuss the etiology and risk factors associated with open-angle glaucoma
|
Etiology: optic nerve damage with visual field changes.
Risk Factors: incr prevalence with 1st degree relatives, elderly, black (more frequently, earlier age, more severe optic nerve damage), pts with: -elevated IntraOcularPressure, first relatives with glaucoma, high myopia (?), cardiovascular disease(?), diabetes (?) |
|
|
Discuss the etiology of secondary glaucoma.
|
-trauma, uveitis, diabetic retinopathy, ocular vascular occlusion. chronic steroid use, (or corticosteroid tx: whether inhaled, topical, systemic or by nasal spray)
|
|
|
Discuss the pathophysiology of glaucoma.
|
Chronic glaucoma characterized by gradually progressive excavation (“cupping”) and pallor of the optic disk with loss of vision progressing from slight constriction of peripheral fields to complete blindness.
Optic nerve changes: -Increased side of cup -Thinning of disc rim -Progressive loss of neural rim tissue -Disc hemorrhages -Loss of nerve fibers → Primary or Secondary Open Angle: intraocular pressure is elevated due to reduced drainage of aqueous fluid through the trabecular meshwork. Is bilateral. →Chronic angle-closure glaucoma: the flow of aqueous fluid into the anterior chamber angle is obstructed. → Normal Tension glaucoma: intraocular pressure is not elevated but same pattern of optic nerve damage occurs, probably due to vascular insufficiency. |
|
|
Describe the clinical presentation of open-angle glaucoma.
|
Chronic glaucoma (open angle) has no symptoms; often detected in routine eye tests. Screening: IOP measurements, optic disc evaluation, visual field testing.
|
|
|
Discuss the diagnostic evaluation of open-angle glaucoma.
|
Screening: IOP measurements, optic disc evaluation, visual field testing.
Dx requires: consistent/reproducible abnormalities in at least 2 of 3 parameters: optic disk, visual field, intraocular pressure Optic disk cupping: an absolute increase or asymmetry between the 2 eyes of the ratio of the diameter of the optic cup to the diameter of the whole optic disk. (cup-disk ratio). Visual field abnormalities start in the paracentral region, followed by constriction of peripheral visual field. Central vision okay till later in disease. NoRMal Range of IOP: 10-21 mmHg!! Note: there are many causes of optic disc abnormalities/visual field changes that mimic glaucoma. Significant portion of eyes w/ primary OAG have normal intraocular pressure at first but later present with elevated IOP.(normal tension glaucoma) |
|
|
Discuss the screening recommendations for open-angle glaucoma.
|
Most effective strategy: periodic, comprehensive eye exams, especially in high risk patient groups.
Suspects: normal visual fields, open normal-appearing angles + elevated IOP and/or abnormal optic disc/nerve fiber layer. |
|
|
Discuss the medical treatment of open-angle glaucoma, to include the classes of medications used and side effect profiles.
|
MEDICAL TX’s. Goal of TX: halt further visual loss, halt further optic nerve damage
1st line tx: prostaglandin analogs → effective, minimal systemic side effects, convenience of use (once daily dosing). SE's: conjunctival hyperemia, permanent darkening of iris & eyebrow color, and increased eyelash growth. >Topical β-adrenergic blocking agents: Nonselective (timolol, bevobunolol). Selective β-1 blockers (betaxolol) SE's: CHF, bronchospasm, bradycardia, depression/confusion, impotence, worsening of myasthenia gravis. >Topical Adrenergic Agonists: epinephrine, dipivefrin, α-2 agonists. SE: systemic- incr BP, tachyarrythmias, tremor, headache, anxiety. Ocular- burning, conjunctival injection, pupillary dilation, allergic rxns. >Topical Cholinergic Agonists: short acting- (pilocarbine), long acting-(demecarium bromide). SE's: systemic- incr bronchial secretion, nausea/vomiting, diarrhrea, apnea. Ocular- incr myopia, eye/brow pain, decr vision. >Carbonic Anhydrase Inhibitors: Oral- (acetazolamide). Topical (dorzolamide). Work directly in the eye. SE: malaise, anorexia, depression, electrolyte abormalities, renal calculi, blood dyscrasias. >Laser Therapy & Surgery: Laser trabeculoplasty is used as an adjunct to topical therapy (to defer surgery) and is advocated as a primary treatment. -Trabeculectomy remains standard procedure. |
|
|
Discuss the etiology, risk factors, clinical presentation and management of angle-closure glaucoma.
|
Primary -occurs ONLY with closure of a preexisting narrow anterior chamber angle.
-precipitated by papillary dilation (being in dark theater, stress, taking anticholinergic drugs/sympathetomimetic drugs) -Age / Elderly -Hyperopic -Inheritance: -> Eskimos-> Asians ->Females -> + family hx Extreme pain & blurred vision -blurred vision assoc. -Halos around lights -nausea & abd pain may occur -eye is RED, cornea ‘steamy’ and pupil moderately dilated & nonreactive to light -intraocular pressure over 50 mm Hg → hard eye on palpation Emergency! Reduction of intraocular pressure -IV dose of acetazolamide -osmotic diuretics (oral glycerin) → Laser Tx to peripheral iris (iridoplasty) is definitive tx** Secondary: -may occur in: uveitis, dislocation of the lens, or topiramate tx. CP: Same as primary. See above. Systemic acetazolamide, with or w/out osmotic agents. Tx determined by cause |
|
|
Discuss the indications for referral to ophthalmology for the management of glaucoma.
|
When to refer in acute angle closure glaucoma: - any pt with suspected acute angle closure glaucoma should be referred emergently to ophthalmology.
All pts with suspected chronic glaucoma should be referred to ophthalmology. |
|
|
List the important historical questions about oral health that should be included in the medical history.
|
Primary symptoms of concern related to oral disease include:
→Pain, which could be constant, it could with chewing or teeth brushing or in relation to cold or heat. → Bleeding gums, again could be constant or just with irritation during eating or brushing teeth. →A number of lesions of varying colors, shapes, sizes can occur, Halitosis refers to bad breath. →Swelling of the gums, tooth loss and malocclusion, commonly referred to as crowding or crooked teeth are all also common oral complaints and/or indications of a more serious problem. →You should questions your patients about the use of oral irritants, including tobacco, drugs, alcohol and sugar. →It is important to know the date of the last dental exam and Xrays, whether the patient is on a chronic blood thinner such as plavix or coumadin, whether he/she has an artificial heart valve or history of endocarditis, and whether there are known or suspected systemic diseases such as immune disorders, GERD, DM or bulimia that could be linked to oral pathology. →You should both question and inspect the patient’s mouth to evaluate for the presence and correct fit of dentures or dental appliances. |
|
|
etiology, clinical presentation, and management of:
apthous ulcers |
etiology: Unknown. Possible risk factors—infection, stress, trauma, irritants, autoimmune disorders.
Epidem: 20-50% adult population. F>M, familial? Prodromal burning x 2 days. Discrete vesicles that rupture, superficial ulcerations. Painful erosions, halitosis, blood-tinged saliva. Types: Occasional – single lesion, months-years between recurrence. Acute Multiple – sequential development w/in weeks, assoc with GI disorders. Chronic recurrent – 1+ lesions always present x years -Diet -Benadryl (diphenhydramine): Kaopectate (bismuth subsalicylate) (1:1) -Viscious lidocaine -chlorohexadine (peridex) mouthwash |
|
|
etiology, clinical presentation, and management of:
Herpes Stomatitis |
Oral herpetic lesions. Epidem: children, does NOT usually recur.
Adults: think immunocompromise -similar to aphthous ulcers but: smaller lesions, gingival & systemic involvement. Spontanoues resolution ~1week. Dx: Tzank smear, viral testing. Not necessary in immunocomp host. -NSAIDs -2% viscious lidocaine -Benadryl:Kaopectate -Consult infectious disease if immunity issues -Antivirals? |
|
|
etiology, clinical presentation, and management of:
Leukoplakia |
Hyperkeratoses occurring in response to chronic irritation (dentures, tobacco, lichen planus). 2% represent dyslplasia or early invasive SCC White lesion that cannot be removed by rubbing on mucosal surface No approved tx’s.
|
|
|
etiology, clinical presentation, and management of:
Sialoadenitis |
Infectious: MC- children/postop
Obstructive: MC- middle-aged man Infectious: painful enlarged gland, eating does NOT affect symptoms, erythema & tightness of skin, prurulent discharge Obstructive: painful, enlarged gland, eating exacerbates symptoms Infectious: Abx (PCN, clindamycin), analgesics, moist heat, liquid diet x 3 days Obstructive: referral to specialist. If lodged stone, tx as bacterial until resolved, then sialogram. Surgical removal of stone/gland. |
|
|
etiology, clinical presentation, and management of:
Dental Caries |
-plaque formation in fissures. Demineralization of tooth enamel & dentin.
-cause: Strep. mutans, Lactobacillus acidophilus. All ages/races/classes. Risks: poor hygiene, hi sugar diet. -Early on: asymptomatic -Advanced: sensitivity to temperature & sweet foods. Exam reveals darkened areas. Tx: removal & restoration (filling/crown) -tooth removal in periodontal disease. Prevention: brush/floss, limit sugars, Fluoride in H2O, coarse food, regular dental checkups, sealant placed over healthy teeth. Mouth guards, avoid oral piercings, |
|
|
etiology, clinical presentation, and management of:
Gingivitis |
-plaque buildup, gingival inflammation.
-Gram + rods, poor oral hygiene, tobacco use, DM,HIV, pregnancy. Medications: Ca+ channel blockers, cyclosporine, phenytoin Symptoms: gum bleeding & pain with brushing Signs: bright red gingivae, edema, visible tartar Scaling of tartar, hygiene, control systemic diseases, adjust medications if necessary Complications: peridontitis- loss of bony support structure |
|
|
etiology, clinical presentation, and management of:
Halitosis |
Local causes: food, meds, periodontal disease, dentures, smoking
Extra-oral causes: URI/LRI, food metabolism, GERD Bad breath Oral hygiene, treat underlying cause, frequent mouthwash, breath fresheners. |
|
|
etiology, clinical presentation, and management of:
dental abscess |
Progression of dental caries, infxn, trauma (polymicrobial). Continuous pain, sensitivity to pressure & temperature.
→may progress to cellulitis (facial swelling, fever, pain, bitter taste, dysphagia… airway is a concern!) -Abx: amoxicillin/clavulanate (augmentin) Clindamydin -Analgesia: Ibuprofen, hydrocodon/acetominophen (lortab & vicodin) -Soft Diet -Refer to Dentist/Oral Surgeon -abscess needs surgical intervention, correct underlying problems. Complications of abscess: endocarditis. |
|
|
Describe the clinical presentation and management of oral candidiasis.
AKA - Thrush |
Etiology: poor oral hygiene, malnutrition, Abx Tx, immune deficiency, DM ?
Presents as: pinpoint spots which develop into painful creamy white curd-like patches overlying erythematous mucosa. -white areas are easily rubbed off (Unlike leukoplakia & lichen planus) only underlying erythema may be seen. Red tongue, poor appetite, irritability. Dx: scrapings reveal pseudohyphae & budding yeast. Tx: nystatin or fluconazole suspension. Systemic fluconazole, patient education, considerations for infants |
|
|
Discuss the diagnostic studies used in evaluation of oral lesions.
|
Tzank Smear – shows multinucleated giant cells for herpetic lesions
Viral testing – test for HSV KOH/Wet prep – for candidiasis, will reveal spores & may show non-septate mycelia. Sialogram – x-ray of salivary ducts & glands: useful for sialadenitis |
|
|
Discuss the risk factors and screening exam for oral malignancies.
|
1. Risk factors: regular alcohol or tobacco use. 2. An RCT of visual screening for oral cancer (at 3-year intervals) showed decreased oral cancer mortality among screened males (but not females) who were tobacco and/or alcohol users over an 8-year period. (Lancet 2005;365:1927)
Well-defined risk factors for oral cancer include tobacco (in all its forms) as well as heavy alcohol use and occupational exposures. Hard liquor is a greater risk compared to wine or beer. Typical occupational exposures include chronic inhalation of dust and fumes such as one might encounter in an occupation or hobby involving significant wood-working, metal-working, painting, autobody/repair. -HPV is causative – in those who don’t meet above criteria. Gardisil has not been demonstrated to prevent cancer in mouth/throat. |
|
|
Discuss patient education recommendations to maintain oral health.
|
→Brushing should be done 2-3 times/day for a minimum of 2 minutes brushing each time, flossing once daily.
→Babies’ teeth can be cleaned with a soft cloth once the first tooth erupts. Frozen teething rings are useful for teething pain. → Limit sugary foods and drinks for a variety of reasons, only one of which is dental hygiene. →Babies should not be sent to bed with a bottle as evidenced on your next slide. →Alcohol and tobacco contribute to cavities and gingival disease and are also risk factors for oral cancers. →There is no evidence that tea or coffee lead to pathologic changes in the teeth or mouth but they do both cause significant staining, as do red wines and juices. →Encourage check ups annually or every 6 months in everyone age Most dental insurance packages will pay for sealants to be placed to prevent cavities. →Encourage anyone playing contact sports to utilize a mouth guard. →Discourage oral piercings (can chip teeth, risk of gum infection, aspiration) |
|
|
Discuss the etiology, clinical presentation, and management of:
viral pharyngitis |
Etiology:EBV (infectious mono) adenovirus, rhinovirus, echovirus, HSV, CMV, and coxsackie A and B
Coronavirus, influenza, parainfluenza, and adenovirus. less common viruses are HSV, coxsackie, CMV, and EBV. Clinical Presentation: odynophagia (painful swallowing), dysphagia (difficulty swallowing), rhinorrhea, cough, hoarseness, occasional mucopurulence, febrile, LAD (lymphadenopathy), myalgias (muscle aches), malaise >Lymphadenopathy& white-purple tonsilar exudate =EBV, >patient NOT present with all the four indicators of strep (temp >38, lack of cough, tonsilar exudate, and anterior cervical adenopathy) Symptoms of adenovirus&coronavirus are coryza, and fever, cervical-adenopathy/tonsilar exudates rare. >Pharyngitis from a flu virus can cause myalgias, headache, and cough; >adenovirus, HSV, and coxsackie virus can all cause an exudate. Mono d/to EBV&CMV can cause exudate, fever, fatigue, and lymphadenopathy. Management: hydration, Tylenol, and supportive care unless the virus is due to HSV, in which case Acyclovir can be used. -ASA, or acetaminophen, as well as salt-water gargling and lozenges – supportive care. |
|
|
Discuss the etiology, clinical presentation, and management of:
bacterial pharyngitis/ tonsillitis |
Etiology: mixed infections are the norm – Strep, Staph aureus, Pneumococcus, >group A beta-hemolytic Strep (GABHS) as the non-viral cause of pharyngitis..
>Strep pyogenes is the most common cause, as well as several other group A Streps. Clinical Presentation:odynophagia, dysphagia, rhinorrhea, cough, hoarseness, occasional mucopurulence, fevers, tonsilar exudates, most with adenopathy 4 key findings of a GABHS are fever over 38 C, tender anterior cervical adenopathy, pharyngotonsilar exudate, and a lack of cough. If three of the four exist, it’s still quite likely to be GABHS, but if only one is present, it’s highly unlikely.> cough, hoarseness, and rhinorrhea would suggest a viral source of infection. Strep can cause mild/serious symptoms, but almost always includes a reddened pharynx and enlarged tonsils with exudate, as well as anterior cervical adenopathy. Usually coryza is not present but indicative of a viral infection if it is. Management: hydration and Benzathine PCN, Clindamycin, Amoxicillan, a 2nd generation cephalosporin > PCN V potassium, cefuroxime axetil, erythromycin, and cephalosporins. >penicillin or erythromycin. |
|
|
Discuss the etiology, clinical presentation, and management of:
infectious mononucleosis |
Etiology: The notes and Current both say EBV is the primary cause.
Clinical Presentation: Very similar to pharyngitis, but marked posterior lymphadenopathy and hepatosplenomegaly. Also, Current states that a “shaggy white-purple exudate, often extending into the nasopharynx” is indicative of mono. Gross. Management: Again, this is pretty much standard viral treatment, ie symptomatic. Ampicillin should not be given to patients when there is a suspicion of mono, as it causes a morbilliform rash that can be mistaken for a penicillin allergy and can cause a glomulonephritis. Mono can lead to a secondary Strep infection. |
|
|
Discuss the etiology, clinical presentation, and management of:
peritonsillar abscess |
(aka “quincy,”)
Etiology: tonsillitis extending into the peritonsillar space; a complication of pharyngitis Clinical Manifestations: Muffled, “hot potato” voice (??), drooling due to odynophagia, unilateral swelling of soft palate with uvular deviation Management: drainage with a scalpel or large-gauge needle, staying medial to the molar and shallow to avoid the internal carotid. The notes call for IV antibiotics, but Current calls for parenteral antibiotics followed by orals when the patient is able to swallow – the but both call for penicillin/amoxicillin or clindamycin. An elective tonsillectomy when the infection has cleared may be considered, but there is debate on when it is needed, although there seems to be agreement that more than one abscess is good cause. |
|
|
Discuss the etiology, clinical presentation, and management of:
Parotitis |
Parotitis (sialadentis is the term for inflammation of a salivary gland)
Etiology: the notes list that in a non-suppurative situation (no pus), the cause could be mumps, HIV, granulomatous, lymphoma, or autoimmune. In a suppurative infection, the notes just say Staph or Strep, while Current lists Staph aureus specifically as the most common cause. Dehydration can also can it. Clinical Manifestations: pain, swelling, pus from Stenson’s duct (behind 2nd molar); also increased pain and swelling with meals Management: Current’s calls for IV antibiotics, switching to orals when ducts are more patent, but the notes just call for amoxicillin, clindamycin, or 2nd generation cephalosporins. Both discuss increasing salivary flow with lemon drops, warm compresses, hydration, and massage of the gland. If there is suspicion of a stone blocking the duct, a CT can be taken and surgery may be required to break or remove the stone, or to drain a abscess that resulted from it. There is also a concern of facial nerve involvement. |
|
|
Contrast the clinical presentation of viral and bacterial pharyngitis.
|
the only real difference in their presentations was a tonsilar exudate and having a positive Strep test. The texts both made note that a bacterial infection was more likely to cause a higher fever and lymphadenopathy, and less likely to cause coryzal symptoms. Exudates are far more common in a bacterial infection, but can be caused by a few viruses, as well; however, they are far more likely to begin as vesicles on the soft palate.
|
|
|
Discuss the differential diagnosis of pharyngitis
|
Additionally, a rapid Strep test can be done. It is considered specific but not sensitive, but is still recommended to prevent a bacterial infection from going untreated, as they are capable of going on to a secondary infection. Harrison also mentions that there are other blood tests that can be ordered to test for specific viruses.
|
|
|
Discuss the diagnostic studies used in the evaluation of pharyngeal disorders.
|
The rapid Strep antigen test and throat cultures were mentioned in all three sources. Our lecturer said that the culture was almost useless, and Current implied that the reliability of the rapid antigen test made the delay of the culturing impractical. The rapid Strep test is quite specific, but not very sensitive. If there is concern about HSV, CMV, EBV, influenza, there are blood tests that can be ordered to identify those as well. In children it is still recommended that a rapid antigen test be followed up by a throat culture.
|
|
|
Discuss the complications associated with pharyngeal infections
|
Dehydration and airway obstruction are a complication of both. A viral infection can go on to become a bacterial infection, and bacterial infections can cause peritonsilar or pharyngeal abscesses, scarlet fever, rheumatic fever, post-strep glomerular nephritis, (PSGN), otitis media.
|
|
|
Mentioned in lecture, not the objectives:
Diphtheria |
causes a grey-black exudate on the mucosa of the upper respiratory tract, causing inflammation and necrosis. It is most common in the first decade of life (and one of the books mentioned its prevalence in alcoholics). It’s not likely we’ll see it too often due to immunizations, but if you do, don’t pull on the membrane for a culture – it’s necrotic and will bleed all over. There’s a danger of the exotoxin it produces to spread to the glottis or cause myocarditis. The only treatment is an antitoxin from the CDC.
|
|
|
Mentioned in lecture, not the objectives:
Gonococcal pharyngitis |
caused by activities I shouldn’t have to explain to you. It is usually asymptomatic, but can cause pharyngitis-like symptoms of a sore throat and tonsillar/lode swelling. Treat with ceftriazone, and treat for chlamydia.
|
|
|
Mentioned in lecture, not the objectives:
Oral candidiasis |
usually Candida albicans and occurs when the normal oral flora is compromised somehow. It presents as “cheesy or creamy mucosal plaques” that can be scraped off, and can be ID’d on a Gram stain. For just oral involvement, a nystatin swish and swallow is the treatment, but if it extends beyond the mouth they need oral fluconazole.
|
|
|
Mentioned in lecture, not the objectives:
Oral cancer |
most often found in patients who use tobacco and alcohol. Patients present with weight loss, pain (sometimes referred and feeling like an earache), odynophagia, dysphagia, lymphadenopathy, an oral mass with possible bony erosion. Treatment is cancer stuff.
|
|
|
OPTIC DISC SWELLING
|
UNIlateral
optic nerve swelling ischemic optic neuropathy orbital nerve lesions |
|
|
PAPILLEDEMA
|
bilateral
increased IntraCranial pressures (eg tumor) |
|
|
Epiphoria means...
|
overflow of tears
|
|
|
Hyperemia means...
|
increased blood flow to an area
|
|
|
Chemosis means...
|
swelling on the conjunctiva
|
|
|
etiology, clinical presentation, and management of:
Viral conjunctivitis “pink eye” |
Etiology: -Adenovirus
(most common) -HSV, Varicella-Zoster, Enterovirus, Coxsackie A24, molluscum cont., HIV & syphilis *preauricular adenopathy*, CP: Epiphora, Hyperemia, chemosis, subconjunctival hemorrhage, FB sensation, follicular conjunctival rxn (cobblestoning) -can be uni. Or bilat. -hx of recent exposure to someone with red eye -recent sxs of URI -rarely seen during influenza infxn Usu. Benign and self limited. Runs a longer course of time compared to bacterial conj. (appx 2 weeks) TX; Supportive care- cold compresses. Artificial tears, hand washing |
|
|
etiology, clinical presentation, and management of:
Bacterial conjunctivitis |
Etiology: Staph, Step (esp. S, pneumonia) Cornyebacterium, Haemophillus, Pseudomonas, Moraxella
More severe- gonococcal and chlamy varieties CP: -Conjuctinval injection may be present segmentally or diffusely, -purulent discharge -“mattering” of lid margins and difficult getting eyes open after sleeping -No blurring vision -Mild pain Usu self limiting, last about 10-14 days if untreated *topical antibiotic therapy (but Dave says no Neomyacin) Clears that mess up in 2-3 days Tx: Systemic abx may be needed for more severe infxns like gohorrhea and chlamy. Referral is recommended , esp gonococcal (ocular emergency!) |
|
|
what are the 4 kinds of
Allergic conjunctivitis? |
1-seasonal allergic c.
(SAC) 2-vernal keratoconjunctivitis c. (VKC) 3-atopic keratoconjunctivitis c. (AKC) 4-giant papillary c. (GPC) |
|
|
etiology, clinical presentation, and management of:
-seasonal allergic conjunctivitis (SAC) |
etiology: Same allergens that trigger all. Rhinitis
(usu seasonal) CP: Itching, clear discharge, injection of conj. Vessels and varying degrees of chemosis, eyelid edema, papillary rxn (little bumps) Tx:SAC, VKC, & AKC -Artificial tears -histamine blockers -mast cell stabilizers -opthaml. Referreal -top. NSAIDS - low dose steroids |
|
|
etiology, clinical presentation, and management of:
vernal keratoconjunctivitis c. (VKC) |
Etiology: Personal and/or family
hx of atopy (asthma, eczema, all. Rhinitis, atopic derm) (usu seasonal in book, notes say chronic) CP: giant papillae giving a cobblestoning appearance on upper tarsal conjunctiva -affects conj AND cornea! -shield ulcers on conj. Tx: SAC, VKC, & AKC -Artificial tears -histamine blockers -mast cell stabilizers -opthaml. Referreal -top. NSAIDS - low dose steroids |
|
|
etiology, clinical presentation, and management of:
atopic keratoconjunctivitis c. (AKC) |
etiology:asc with atopic derm
(more chronic) CP:-Bilateral inflammation of conjunctiva AND eyelids on upper and lower tarsal conjunct. -Eyelid skin may be eczematous with dry, scaley, inflamed skin Tx: SAC, VKC, & AKC -Artificial tears -histamine blockers -mast cell stabilizers -opthaml. Referreal -top. NSAIDS - low dose steroids |
|
|
etiology, clinical presentation, and management of:
-giant papillary c. (GPC) |
Etiology: contact lens use?
CP: *Ocular itching with a mucoid-like discharge just on conj (NO cornea) -large cobblestoning -FB sensation when using contacts -uni or bilateral -in severe cases, may have ptosis Tx: contact lens holiday: SAC, VKC, & AKC -Artificial tears -histamine blockers -mast cell stabilizers -opthaml. Referreal -top. NSAIDS - low dose steroids |
|
|
etiology, clinical presentation, and management of:
Pterygium |
Et: Asc with constant exposure to wind, sun (esp living in tropical climates), sand, and dust,
CP: -Elevated, superficial external ocular mass that usu forms over the prelimbal conj. And extends onto the corneal surface -degeneration of collagen and fibrovascular prolif. -fleshy, triangular encroachment of the conjunctiva onto the nasal side of the cornea -often bilateral -can distort corneal topography -poss redness, discomfort, or FB sensation TX: None usu required -artifical tears -poss short course of topical NSAIDS or weak corticosteroids -excision if growth threatens vision, induced astigmatism, or severe ocular irritation -recurrence is common and usu more aggressive than the first time |
|
|
etiology, clinical presentation, and management of:
Episcleritis (2 types) |
Et: -Most idiopathic
-some have underlying systemic conditions (ex. Collagen vascular diseases like RA, SLE, IBS; infections, malignancies, etc.) CP: -Irritation without pain -Usu redness is on nasal or temp. side but not both- Dave -Vessels blanch with topical vasoconstrictor -Vessels are pink to light red 1. Simple: intermittent bouts that often recur at 1-3 mo. Intervals; episodes usu last 7-10 days and most resolve after 2 weeks 2.Nodular: has a nodule!; prolonged attacks of inflammation; more acute onset, moderate pain, may be more likely to be asc with systemic causes Tx: Self-limiting disease with little or no permanent damage to the eye (in contrast to scleritis) Most pts. Will NOT require treatment -oral NSAIDS may help with pain and curb underlying inflame. Conditions in nodular type. |
|
|
etiology, clinical presentation, and management of:
Herpes keratitis “herpectic lesion on cornea” |
Et: HSV-1 mostly
(virus is hanging out in trigeminal nerve and is induced with stuff like fever, excessive sun exposure, or immunodeficiency) -Only involves the cornea -pain -photophobia -blurred vision -tearing -redness 4 catagories: Infectious epithelia keratitis-DENDRITIC ULCER! Branching terminal buds, swollen epithelial border that contains live virus, central ulceration then ulcer enlarges, its shape is no longer linear (so now considered a geographic ulcer) 3 others note noted separately Most cases resolve spontaneously within 3 weeks Tx: -rationale for treatment is to minimize stromal damage and scaring -Any pt with a hx of HSV keratitis and an acute red eye should be referred Antiviral therapy good for epithelial infections- topical and systemic (def. NO steroids or patching!) |
|
|
etiology, clinical presentation, and management of:
Subconjunctival hemorrhage |
Et: -Idiopathic
-trauma -hypertension -valsalva -blood thinners -infections -bleeding disorders CP: Blood in the subconjunctival space -No treatment needed -Will self-resolve, vision not affected -Artificial tears “Tell pt will prob get worse looking before better but that’s ok” |
|
|
etiology, clinical presentation, and management of:
Uveitis/iritis |
Et: -Trauma
-inflammatory :>Ankylosing spondylitis, RA, Behcet’s disease, crohns, SLE, Psoriatic arthritis, sarcoidosis, scleroderma, ulcerative colitis, gout -infectious: >TB, lyme disease, syphillis, toxoplasmosis, toxocariasis, Herpes simplex, herpes zoster CP: -Extreme photopbobia -CONSENSUAL photophobia -occular and perioribal pain -blurred or cloudy vision’ -cilliary flush -tiny white dots seen (called cell &flare) that WBC and protein collected, when they settle it makes a hypopyon Tx: *-Referral to ophthalmology* and consider poss to rheumatology -rheumatologic and infectious workup -steroid anti-inflam eye drops -dilating eye drops (to reduce the photophobia) -possible pressure reducing drops -oral steroids -subconjunctival steroid injection -steroid sparing agents like methotrexate |
|
|
Discuss the etiology and clinical presentation associated with a CILIARY FLUSH
|
Etiology: iritis/uveitis, acute angule closure glaucoma, corneal abrasion of trauma
Little clarification just for sake of it- uveitis basically means inflammation of the iris, cornea, and cilliary body and can be acute or chronic. iritis is a form of uveitis= iritis is an acute anterior uveitis. CP- ciliary (aka circumcorneal) injection involves branches of the anterior ciliary arteries and indicates inflammation of the corena, iris, or cilliary body. When looking at eye, redness will be right around iris in the limbus area (no white halo around iris and then redness like you see in conjunctival injection). Sometimes it can be more diffuse but still will see redness right up there near the iris! |
|
|
Discuss the diagnostic studies used in the evaluation of:
conjunctival and corneal disorders. |
A complete ophthalmologic exam including:
-visual acuity -EOMs -slit lamp examination of the cornea for edema, defects, or opacification with and without fluorescein -ant. Chamber evaluation for depth, cells, and flare -intraoccular pressure (IOP) measurements -eyelid inspection with aversion (if poss suspect a FB issue) -pupil reactivity -pupil shape -pupil direct and consensual reaction to light A simple culture or staining by the laboratory of the conjunctival material helps in determining the cause and subsequent management of the condition. There are some immunologic tests available for testing GC Chlamydia. b. Use of Fluorescein stain is helpful with dealing with the cornea |
|
|
CN VIII
Vestibulocochlear nerve |
AKA auditory or acoustic nerve) responsible for transmitting sound and equilibrium (balance) info from inner ear to brain.
Damage: hearing loss vertigo false sense of motion loss of equilibrium (in dark places) nystagmus motion sickness gaze-evoked tinnitus. |
|
|
CN IX
Glossopharyngeal Nerve |
It receives general sensory fibers (ventral trigeminothalamic tract) from the tonsils, the pharynx, the middle ear and the posterior 1/3 of the tongue.
It receives special sensory fibers (taste) from the posterior one-third of the tongue. It receives visceral sensory fibers from the carotid bodies. It supplies parasympathetic fibers to the parotid gland via the otic ganglion. It supplies motor fibers to stylopharyngeus muscle, the only motor component of this cranial nerve. It contributes to the pharyngeal plexus. Damage: rare to just IX aone ->loss of taste from the back of the tongue and absence of the gag reflex |
|
|
CN X
Vagus (what doesn't it do?) |
It has motor control over the voluntary muscles of the pharynx, vocal cords, larynx, heart (slows the heart rate), lungs digestive organs.
Damage: produces palpitation (forcible pulsation of the heart), tachycardia (rapid beating of the heart), vomiting, slowing of respiration, and a sensation of suffocating, paralysis of the vocal cords and larynx. |
|
|
CN XII
|
Supplies the muscles of the tongue, thyroid cartilage and hyoid bone. Complete damage to this nerve causes unilateral paralysis of the tongue and atrophy of that side. When the tongue is protruded, it deviates to the paralyzed side because of the unopposed action of the normal half.
|
|
|
A large, poorly reacting pupil may be due to...
|
...third nerve palsy, acute tonic pupil, iris damage caused by acute glaucoma, or pharmacologic mydriasis.
|
|
|
A small pupil occurs in ...
|
...Horner syndrome, inflammatory adhesions between iris and lens (posterior synechiae), long-standing tonic pupil, or neurosyphilis (Argyll Robertson pupils).
|
|
|
Physiologic anisocoria is ...
|
a common cause of unequal pupils that react normally.
|
|
|
Discuss the differential diagnosis of “red eye.”
|
Red eye can be conjuntival injection, cilliary injection, or both…
-viral, baterical, or allergic conjunctivitis -episcleritis -sclerritis -pterygium -subconjunctival hemorrhage -corneal abrasion and erosion -bacterial or viral keratitis -uveitis/iritis -acute angle closure glaucoma -trauma |
|
|
Discuss the indications and contraindications for the use of topical steroids in the treatment of *corneal disorders*.
|
Indications: uveitis/iritis and giant cell arteritis
Contra: herpes simplex (dendritic) keratitis, fungal infection, open-angle glaucoma, and cataract formation. --> perforation of the cornea may occur when the corticosteroids are used for herpes simplex keratitis. Topical nonsteroidal anti-inflammatory agents are being used increasingly. The potential for causing or exacerbating systemic hypertension, diabetes mellitus, gastritis, osteoporosis, or glaucoma must always be borne in mind. Definitely don’t use it for conditions where you want the body to heal itself like corneal abrasion- it slows the healing down. |
|
|
Discuss the indications for referral to an ophthalmologist
|
-->Sudden visual loss in an uninflamed eye
-->giant cell arteritis = EMERGENCY -->orbital cellulitis, gonococcal keratoconjunctivitis, and ocular trauma. -> people with gradual vision loss, but aren't emergencies -->diabetics should have eye exams at least annually |
|
|
What are some causes of sudden visual loss in an uninflamed eye ?
|
vitreous hemorrhage, including due to proliferative diabetic retinopathy; retinal detachment; neovascular age-related macular degeneration; retinal vein occlusion; retinal artery occlusion; and anterior ischemic optic neuropathy, either possibly due to giant cell arteritis, and optic neuritis.
|
|
|
Discuss the indications for URGENT referral to an ophthalmologist
|
SUDDEN VISION LOSS
FLOATERS, FLASHES. – Retinal Detachment/Tear -PAINFUL RED EYE IN A SOFT CONTACT LENS WEARER -PAINFUL RED EYE AND A -METALLIC CORNEAL FOREIGN BODY -HEADACHE, BLURRED VISION, AND PERIPHERAL SCOTOM |
|
|
otitis externa
Otits Externa – aka Swimmer’s Ear Prevention |
Prevention/Prophylaxis/ 2% acetic acid (VoSol) to acidify the EAC, use isopropyl alcohol or hydrogen peroxide, can be drying and irritating
Treat underlying infection: Bacterial origin 1st line Corticosporin Otic Suspension (Polymixin/ treats Pseudomonas, Neomycin/ treats Staph, and Hydrocortisone/ treats inflammation -Alternative Ofloxacin Otic Solution/Floxin Otic Fungal Origin -Sulfanilamide Powder – one time dusting -Clotrimazole 1% solution - Acetic acid irrigation >Relieve pain >Avoid triggers >keep canal dry >no swimming until infection is resolved ->Vaseline-coated cotton ball in ear during bathing >Culture discharge if severe or recurrent disease |
|
|
Necrotizing Otitis Externa – Malignant Otitis Externa
|
Etiology
Pseudomonas Infection with involvement of the underlying bone - osteomyelitis can spread intra-cranially Clinical Presentation 1. Fever 2. Increasing deep-seated ear pain 3. Red, granulation tissue in EAC - may see a facial nerve palsy 4. Seen in Diabetics and Immunocompromised patients Management 1. Diagnose with CT scan or MRI 2. Hospital admission 3. Intravenous antibiotics - broad spectrum Penicillin (piperacillin-tazobactum/Zosyn) or Cephalosporin (ceftazidime/Fortaz) 4. ENT consult for surgical debridement, if needed |
|
|
Describe clinical presentation and management of external auditory canal foreign bodies
|
Clinical Presentation
1. Ear fullness 2. Possible hearing loss 3. Pain/discomfort 4. foreign body sensation Management 1. Removal with forceps or irrigation 2. Referral to ENT, if needed |
|
|
Describe the predisposing factors for the development of a cerumen impaction.
|
• Predisposing factors – use of cotton-tipped swabs, hearing aids and ear plugs
|
|
|
Describe the management of a cerumen impaction
|
• Treatment – Ear curetes
• Irrigation – rule out TM perforation first! • Hydrogen peroxide • Ceruminolytics – Murine Ear/Debrox • If needed, refer to ENT |
|
|
Discuss the etiology, clinical presentation, and management of
acute otitis media. |
Etiology: Streptococcus pneumoniae – 40-50% Haemophilus influenzae – 30-40% Moraxella catarrhalis – 10-15% Staphylococcus aureus - 2%. Viral 45-70%.
CP: Pediatric pt: Irritability, decr appetite, Fever Otalgia (tugging on the ear), Hearing loss, Conjunctivitis, Rhinorrhea, Otorrhea, emesis, Diarrhea Adult patient: Otalgia Rare to have fever, but may subjectively feel warm Reddened TM with decreased TM mobility -TM may be distorted, loss of landmarks --a bulging TM is the hallmark of AOM--Check for conductive hearing loss Tx: Symptomatic care of pain/fever. 75% of M. cat infx resolve w/o tx. 50% w/o flu, 10% S. pnuemo. hi-dose Amoxicillin/augmentin in 1st uncomplicated case. (or IM ceftriaxone for all, esp <2y/o. If no respnose, try another abx. DON'T use decongestants. |
|
|
Describe the clinical presentation, management and complications of
recurrent otitis media |
1. 3 or more documented episodes in a 6 month time frame or 4 or more episodes in a 12 month time frame
2. TM perforation with purulent discharge 3. Conductive hearing loss Management Refer to ENT for evaluation for placement of tympanostomy tubes Complications 1. Ear Complications - Chronic Otitis Media, TM perforations, mastoiditis, hearing loss, labyrinthitis 2. Neurologic Complications -Meningitis, Encephalitis, Intracranial abscess 3.Progression of Symptoms: new onset of neurologic signs, stiff neck, persistent hearing loss warrant further investigation |
|
|
Explain the rationale for patient referral for possible myringotomy and tube placement.
|
A patient should be referred for possible tube placement if they have the following indications:
- Persistent symptoms - Hearing loss greater than 40 dB - Evidence of TM damage |
|
|
Discuss the etiology, clinical presentation, and management of serous otitis media.
|
Etiology 1.Middle ear effusion secondary to inflammation or Eustachian tube dysfunction
2.Considered to be “sterile”, but 50% have bacteria present in effusion 3.May be seen following a viral URI, AOM or in association with allergic rhinitis CP:Ear fullness, Decreased hearing – usually painless Afebrile, Amber colored (straw) fluid behind TM Retraction of TM produces prominent landmarks TM will not move with otoscopy, Conductive hearing loss Tympanogram – Type B Mgmt: Majority of cases resolve spontaneously within 12 weeks -Watchful waiting for 3 months if: -No speech or language problems No hearing loss >Re-evaluate at 3 months, if persistent or evidence of hearing loss treat with antibiotics >Must refer adults with unilateral symptoms to ENT to rule out nasopharyngeal carcinoma >Antibiotics are appropriate since 50% patients have bacteria due to chronic OM: 10 day course of Amoxicillin also may use: amoxicillin/clavunate (Augmentin) or Trimethoprim-Sulfamethoxazole (Bactrim) >Re-evaluate after 4-6 weeks >Refer to ENT for persistent fluid and/or hearing loss |
|
|
Describe the diagnostic use of pneumatic otoscopy in serous otitis media.
|
• The use of pneumatic otoscopy is to establish the motility of the TM as the pressure in the external auditory canal is increased or decreased. The clinical presentation of serous otitis media is retracted TM, which produces prominent landmarks, complaints of fullness, decreased hearing – usually painless, afebrile, amber-colored (straw) fluid behind the TM with possible visible air-fluid level and bubbles. The fluid build-up will place pressure on the TM and decrease its mobility.
|
|
|
1Discuss the clinical presentation and management of barotrauma
Note: Barotrauma is due to the pressure differences between the middle ear and the external auditory canal |
Clinical Presentation
1. Ear pressure/pain 2. Patient may have vertigo with damage to the inner ear 3. TM will be retracted and may see bleeding into the TM or the middle ear (hemotympanum) 4. May have hearing loss • usually conductive, but may be sensorineural if inner ear is damaged 5. Can be associated with Eustachian tube dysfunction and can be seen with URI’s Acute Otitis Media, allergies and flying or scuba diving Management 1. Prevention • uses of decongests prior to flying or diving • valsalva maneuvers, chewing gum 2. Referral to ENT for patients with vertigo and SNHL |
|
|
Describe the clinical presentation and management of a perforated tympanic membrane.
|
Clinical Presentation
1. Ear pain 2. hearing loss 3. tinnitus (ringing in the ear) • with vertigo if the inner ear is involved 4. No movement of the TM with pneumatic otoscopy Management 1. Practice dry ear precautions until healed • no swimming • Vaseline-coated cotton ball during bathing 2. Refer to ENT if surgery is needed |
|
|
Discuss the indications for referral of a patient with a perforated T.M. to an otorhinolaryngologist
|
perforation is large and in need of surgical repair. (>25% of TM)
or if perf is on margin/is >40% in size. |
|
|
Distinguish between an acute and a chronic T.M. perforation.
|
• Acute TM perforations are typically smaller and more likely to heal on their own with minimal defects
• Chronic TM perforations are typically a larger defect and are less likely to close spontaneously, may require surgical repair (tympanoplasty |
|
|
Discuss etiology and clinical presentation of a cholesteatoma
|
Etiology: chronic, negatively pressurized environment that causes TM to thin from retraction & adhere to the middle ear tissue. Squamous epithelium starts to form in the pocket and can expand into the mastoid air cells & erode the ossicles. Does NOT have to start with TM perforation. Can start with eustachain tube dysfunction after chronic ear infections.
CP: hearing loss that has worsened, may have chronic discharge from ear that will not clear up w/ typical meds. Fullness. Usually NOT painful. Pt has hx of recurrent ear infxns or previous surgery to ear. Exam: pearly white mass in middle ear, squamous debris that extends from the attic or pars flaccida to the canal. May have chronic discharge. Conductive hearing loss. TX: refer to an ENT, order CT of temporal bone to evaluate extend of ear involved. Surgically remove all visualized epithelial tissue in middle ear/mastoid area. →most of time middle ear bones have been eroded & need reconstructive surgery. |
|
|
Describe the clinical presentation and management of mastoiditis
|
*Mastoiditis is an extension of Otitis External or Acute Otitis Media into the mastoid air cells caused by same bacterial pathogens as OE and AOM
CP: Slow resolution of symptoms pt will c/o deep temporal pain >Pinna displaced with posterior auricular edema and erythema >>Mastoid tenderness Dx: CT scan, shows cloudiness of mastoid air cells & bony destruction Mgmt >Outpatient 1st line – Amoxicillin 80-90 mg/day for 10 days >active against 90% of S. pneumo strains Alternatives – Amoxicillin/clavunate (Augmentin) *PCN allergy> •Cefdinir (Omnicef) •Cefuroxime (Ceftin) •Azithromycin (Zithromax) •Carithromycin (Biaxin) -Symptomatic care of pain/fever •acetaminophen, ibuprofen •topical pain reliever – Auralgan •encourage fluids OTC cold meds useless Pt Educ>> pain and fever should resolve after 3 days: if do not resolve/worsen return for evaluation >>otherwise, >recheck @1 week for regular follow-up >hearing loss may take up to 1 mo to resolve, *there may be speech delays* Inpt : IV Abx – Cefotaxime (Claforan) or Ceftriaxone (Rocephin) > ENT consult |
|
|
Describe the prognosis of untreated mastoiditis
|
• CN VII palsy
• Intracranial extension (abscess) • Meningitis • Encephalitis |
|
|
Discuss the etiology of hearing loss to include genetic and congenital etiologies.
|
1.Genetic/ Hereditary> Syndromic (33%)
Brachio-oto-renal , Treacher-Collins,Stickler Waardenburg’s, Pendreds, Ushers, Kippel-Feil, Alport’s , Nonsyndromic (66%), Hypoplasias & Aplasias >Genetic without morphological abnormality -90% are recessive - no family history 2. Acquired/Congenital >Neurofibromatosis-Type II, Trauma, Ototoxicity, Bacterial Meningitis, TORCH culprits |
|
|
etiology for
Conductive Hearing Loss |
Canal - Obstructions
Tympanic Membrane - Perforations Middle Ear – effusions or Barotraumas Ossicles – Cholesteatoma or Fracture Eustachian Tube – Nasopharyngeal mass or Middle Ear Effusion Atresia – the opening and the ear canal did not form |
|
|
Etiology For
Sensorineural Hearing Loss |
Age/Heredity
Noise Induced – Bilateral Infection Drugs Surgery Acoustic Neuroma – a tumor that grows slowly on the nerve Meniere’s Disease Sensorineural Hearing Loss can be within the Cochlea or Eighth Cranial Nerve |
|
|
Distinguish between the clinical presentation of sensorineural and conductive hearing defects
|
Conductive Hearing Loss
The sounds are not “conducted” or transmitted through the ear canal, tympanic membrane or middle ear Sensorineural Hearing Loss There is a problem with the auditory nerve or the cochlea Hearing Loss can be a mixture or combination of conductive or sensorineural as well |
|
|
When to order an audiogram
|
1. Patient/ Parent Concern
2. Noise Exposure 3. Family History of Hearing Loss 4. Trauma 5. Baseline/Monitoring for ototoxic drugs 6. Facial Nerve Paralysis 7. Cholesteatoma 8. Middle Ear Effusion 9. Vertigo |
|
|
Discuss the diagnostic studies used in the evaluation of hearing loss
|
1. Whisper Test
2. Tuning Fork Test a. Weber Test – Sound is transmitted through the bone to the inner ear, the sound will be louder in the ear with the conductive loss b. Rinne Test – normal air conduction should be better than bone conduction 3. Formal Audiogram |
|
|
Compare & Contrast the Audiogram findings of Conductive & Sensorineural hearing loss
|
Conductive Hearing loss: audiogram findings –bone conduction responses within normal limits, and air conduction responses depressed.
Sensorineural Hearing Loss: both air and bone conduction are decreased equally, but the difference between them is unchanged |
|
|
management of sensorineural hearing loss
|
Assistive Listening Devices – Amplified hand piece for phone, Headphones for TV, Pocket Talker (Short Term) and FM System very effective for classroom
Cochlear Implants Amplification |
|
|
management of conductive hearing loss
|
Cerumen Removal
Surgery – Mastoidectomy, Tympanoplasty, Ossicular Chain Reconstruction and Repair of Ear Canal Atresia Amplification |
|
|
Discuss the indications for referral to an otolaryngologist for the evaluation of hearing loss
|
1. Unable to clean wax out of ear
2. Uncertain finding on physical exam 3. Unresolved middle ear effusion 4. Tympanic Membrane perforation which does not heal 5. Asymmetric Hearing Loss a. Conductive b. Sensorineural 6. Facial Nerve Paralysis 7. True Spinning Vertigo |
|
|
Compare the etiologies of central and peripheral vertigo
|
1. Central – think neuro (vertical nystagmus)
a. Mild to moderate b. Constant c. Other signs and symptoms of a center nervous system disorder d. No other otologic findings e. Order MRI f. May be associated with Multiple Sclerosis, Brain Tumor, Head Injury, Medication side effect 2. Peripheral – think ear (horizontal or rotary nystagmus) a. Due to inner ear problem b. Severe c. Associated with nausea, vomiting and diaphoresis (clammy and sweating) d. Paroxysmal e. May or may not be associated with hearing loss, tinnitus and fullness in the ear |
|
|
Distinguish between dizziness, presyncope, disequilibrium, and lightheadedness
|
Dizziness – definition can be unclear as it can mean different things to different patients. The evaluation of dizziness: 1. True Spinning vertigo, 2. Benign Positional Vertigo, 3. Meniere’s Disease, 4. Vestibular Neuronitis – viral, 5. Facial Nerve paralysis
Presyncope – Impending faint or Loss of Consciousness Disequilibrium – Sense of imbalance Lightheadedness – nonspecific dizziness Vertigo – The Illusion of Movement |
|
|
Discuss the etiology, clinical presentation, and management of benign paroxysmal positional vertigo
|
1. Intense episodic vertigo
2. Initiated by certain head positions (usually with the affected ear in the down position) 3. Not due to tumor, caused by calcium carbonated crystals in the semicircular canals 4. Diagnosed by the Dix-Hallpike Maneuve 5. May be cured by physical therapy (repositioning of the crystals) |
|
|
Discuss the etiology, clinical presentation, and management of
Labyrinthitis |
1. Inflammation of the 8th cranial nerve or inner ear balance organs
2. Etiology – Viral 3. Hearing is stable 4. Nausea with or without vomiting 5. Severe for 24-48 hours 6. Resolves over weeks 7. Treat with vestibular suppressants (Valum) and Anti-emetics |
|
|
Discuss the etiology, clinical presentation, and management of
Meniere’s Disease |
1. Episodic Vertigo
2. Fluctuating Hearing Loss 3. Roaring Tinnitus 4. Sensation of fullness in the ear 5. Etiology – an Inner Ear Fluid Imbalance (endolymphatic hydrops) |
|
|
Discuss the diagnostic studies used in the evaluation of vertigo.
|
1. Audiogram
2. Dix-Hallpike Maneuver for BPV 3. Electronystagmogram (ENG) 4. Electrocochleagraphy (ECOG) 5. Physical Therapy Evaluation 6. MRI of the internal auditory canals with gadolinium |
|
|
Describe the Etiology and Treatment of Tinnitus:
|
Etiology: usually due to noise exposure, hearing loss or medication side effect. Pitch varies (is often pitch of maximal hearing loss). Treatment: masking with white nose (fan). Biofeedback (put in a hearing aid that makes sound at same frequency as tinnitus). Stop culprit medications (Aspirin, NSAIDS).
Vascular Tinnitus: synchronous with pulse, may be heard by another person (bruit heard with stethoscope). Etiology: vascular neoplasm/formation (glomous tumor, arteriovenous malformation). Benign intracranial HTN. Pulsatile Tinnitus needs further eval. (neurology consult). |
|
|
Discuss the Indications for referral to otolaryngology for vertigo
|
True Spinning Vertigo (there are lots of diagnoses for ‘dizziness’ including BPV, meneire’s, vestibular neuronitis, facial nerve paralysis and true spinning vertigo).
2. DON'T refer for Syncope (is not caused bye ear problem) and Episodic hypotension. |
|
|
Discuss the Diagnostic studies used in the evaluation of nasal disorders
|
-->Allergic Rhinitis: Hx Smpt: Timing,Duration,Quality,Triggers -Physical Exam &Lab Tests
>RAST – measures allergen specific IgE from blood sample, used when skin testing is impossible >Skin Testing – more sensitive, more specific, lower cost, fast results -->Nasal Polyps: -->Acute sinusitis: --Sinus Radiographs --Plain Films (Caldwell AP/ Lateral/ Waters view) --CT scan (Coronal views) --Endoscopy --Sinus Aspirate Culture- “gold standard” for confirming the dx --Predicative Clinical Features --Radiographic findings: -->Chronic Sinusitis: --Plain films may show bony erosion --CT scan will show mucosal thickening; also r/o any anatomic obstruction |
|
|
Etiology, clinical presentation, diagnostic studies, and management of allergic rhinitis
|
Type 1 Rxn >>Allergen-specific antibodies (IgE) bound to mast cells interact with an inhalant allergen > symptoms of sneezing, pruritis, congestion, rhinorrhea and PND
CP: 1.Sneezing 2.Pruritis 3Rhinorrhea 4.Nasal Obstruction 5.Stuffiness Management 1. Avoidance 2. Medical Management a. target therapy – address mediator effects of allergy - antihistamines - decongestants (Pseudephedrine) - Mucolytics (Guaifensin) - Anticholinergics (Atrovent) - Anti-leuoktrienes (Singulair) - Mast Cell stblzrs: (Nasalcrom) b.immunomodulation -Nasal Steroids (Flonase) -Systemic Steroids (Prednisone) -Immunotx (allergy shots) >>Single medication often does not achieve total relief of all symptoms>>Combine medications of various classes to maximally control pt's symptoms >>Tailor pharmacologic regimen - prevention – cromolyn - maintenance – tropical nasal steroid - rescue - antihistamine |
|
|
first line agents for allergic rhinitis
|
1. FIRST LINE AGENTS
a. Antihistamines - block histamine’s effect at target tissues - address the irritative symptom of allergy - NOT effective at alleviating congestion on their own, therefore decongestant (pseudoephedrine) often added too formulation b. Topical Nasal Steroids (Flonase) i. Down regulate the immune response ii. Decrease inflammatory cytokines iii. Must be used regularly iv. Delayed onset of symptom relief….weeks |
|
|
adjunctive agents for allergic rhinitis
|
i. Decongestants
1. topical sprays – risk of rebound rhinitis (rhinitis medicamentosa) 2. systemic ii. Mast Cell Stabilizers (Cromolym sodium – Nasalcrom) 1. prevent mast cell degranulation 2. good for anticipated or situational allergy exposure 3. requires pretreatment for several days for maximal efficacy iii. Anti-leukotrienes (montelukast – Singulair) 1. effective in reducing congestion 2. once a day dosing |
|
|
etiology, clinical presentation, and management of
Vasomotor rhinitis |
Etiology:Non-allergic/Non-infectious rhinitis
-results from autonomic dysfunction -parasympathetic system predominates -results in vasodilation and edema CP:Congestion, Profuse rhinorrhea (clear fluid/runny nose) -Exacerbated by :cold air, spicy foods, pollutants, strong emotions, medications Medical Management: -topical anticholinergic sprays (Ipratropium bromide .03%) -dosing early in day -dosing thruout day to control symptoms (qid), minimal side effects Surgical Management: Vidian Nerve Section iReserved for severe cases after failure of medical mgmt **Unresolving or unexplained clear rhinorrhea warrants ENT evaluation for possible CSF leak*** |
|
|
Differentiate between the clinical presentation of vasomotor rhinitis and allergic rhinitis
|
-->Vasomotor Rhinitis
Congestion , Profuse rhinorrhea (clear fluid/runny nose) Exacerbated by cold air, spicy foods, pollutants, strong emotions and medications -->Allergic Rhinitis Sneezing, Pruritis, Rhinorrhea, Nasal Obstruction and Stuffiness |
|
|
etiology, clinical presentation, and management of
rhinitis medicamentosa |
Rhinitis Medicamentosa
Etiology Rebound rhinitis of nasal mucosa following sudden cessation of topical decongestants (Afrin and Phenylephrine) after prolonged use Clinical Presentation 1. Extreme nasal obstruction and pressure 2. Can occur with 3-5 days of repeated use Management 1. Prevention - Short term use of topical decongestants “3 sprays, 3 times a day, for 3 days” 2. Abstinence 3. Medical Management – to wean off Afrin a. Topical nasal steroids (Flonase) b. Possible role for systemic steroids |
|
|
etiology, clinical presentation, and management of
nasal polyps (the – End result of chronic nasal inflammation) |
Etiology 1. Can be an isolated phenomena – idiopathic nasal polyposis 2. Often a component of other rhinologic diseases
-chronic rhinosinusitis -allergic fungal sinusitis Samter’s Triad (oNasal polyps oAsthma o Aspirin Sensitivity) CP: Congestion, Nasal Fullness -Usually a bilateral, -if unilateral, raises concern for neoplasm, possibility for SCC Mgmt: Early ENT referral, Treat underlying inflammatory disorder, Anti-leukotrienes (Singulair), Topical Nasal Steroids Systemic Corticosteroids >>Surgical debulking usually required (Endoscopic Sinus Surgery) |
|
|
most common pathogens associated with acute sinusitis.
|
i. Viral
• Rhinovirus/Influenza virus (15-20%) ii. Bacterial • Streptococcus pneumoniae • Haemophilus Influenzae • Morexella catarrhalis iii. Nosocomial • Staph. aureus • Pseudomonas aeruginosa • Klebsiella pneumoniae • Enterobacter • Proteus Mirabills -->Fungal in immunocompromise |
|
|
etiology of acute sinusitis
|
1. The most common etiology is a previous viral URI/Common Cold
v. Paranasal sinuses are sterile; lined with ciliated epithelium that clear the mucus to the ostiomeatal complex vi. Common cold infection leads to mucosal edema, impaired ciliary clearance, and sinus inflammation vii. Decreased drainage of thick secretions leads to obstruction of sinus ostia viii. Entrapment of bacteria leads to infection 3. Can also be associated with allergies, tumors, polyps, deviated nasal septum or foreign bodies |
|
|
management of acute sinusitis.
|
Management
Hydration:•fluids, humidification of air (vaporizers), saline nasal spray Decongestants – promote sinus drainage •Topical: Phenylephrine (Neo-synephrine) Oxymetazoline (Afrin) •Systemic: Pseudoephredrine (Sudafed) 120 mg BID May also use topical nasal steroids for recurrent symptoms or allergic rhinitis >Antihistamines may be used if associated allergic component: Tend to thicken secretions and worsen obstruction Analgesics – NSAIDs, acetaminophen If Bacterial - Antibiotic Tx oFirst line treatment: Amoxicillin, 500 mg, TID Trimethoprim-sulfamethoxale oFor penicillin-allergy: Levofloxacin (Levaquin) 750mg q24 x 5 days oContinue antibiotics for 10-14 day course oFor continued symptoms beyond 2 weeks of treatment: Amoxicillin/clavunate (Augmentin) Cefuroxime (Ceftin) Azithromycin (Zithromax) Clarithromycin (Biaxin) o For continued symptoms after two rounds of antibiotic treatment…refer to ENT |
|
|
medical management of allergic rhinitis
|
Medical Management
a. target therapy – address mediator effects of allergy - antihistamines - decongestants (Pseudephedrine) - Mucolytics (Guaifensin) - Anticholinergics (Atrovent) - Anti-leuoktrienes (Singulair) - Mast Cell Stabilizers (Nasalcrom) b. immunomodulation - Topical Nasal Steroids (Flonase) - Systemic Steroids (Prednisone) - Immunotherapy (allergy shots) 3. Single medication often does not achieve total relief of all symptoms 4. Combine medications of various |
|
|
Complications of acute sinusitis & red flags:
|
o Uncommonly seen, but potentially life-threatening
Osteomyelitis Cavernous sinus thrombosis Orbital cellulitis Meningitis, brain abscess, epidural empyema o Important to recognize and refer immediately to ENT Red flags: o Changes in vision, mentation or periorbital edema o Hospitalization, imaging, IV antibiotics, surgery |
|
|
the most common pathogens isolated in cases of chronic sinusitis.
|
i. S. aureus, S. pneumoniae, H. influenzae, P. aeroginosa, anaerobes
|
|
|
clinical presentation,, and management of chronic sinusitis
|
Clinical Presentation
1. Symptoms – continued nasal congestion with purulent nasal discharge/PND, facial pain/pressure, headache 2. Signs – mucopurulent nasal discharge, inflammed mucosa 3. Look for deviated septum, nasal polyps or turbinate edema Management -Treatment: • Amoxicillin/clavulante (Augmentin) 500 mg BID for 3-6 weeks • Alternatives: - Cefuroxime (Ceftin) 500 mg BID - Clindamycin (Cleocin) 300 mg QID (or 400 mg TID) • Two-drug therapy: - Metronidazole (Flagyl) with either cefdinir (Omnicef) OR levofloxacin (Levaquin) OR trimethoprim-sulfamethaxole (Bactrim) • Continue systemic decongestants • Nasal irrigation – saline • Inhaled topical steroids (fluticasone (Flonase)) may be helpful if underlying history of allergies -Referral to ENT for evaluation and potential endoscopic sinus surgery |
|
|
Discuss the complications associated with sinusitis.
|
1. Uncommonly seen, but potentially life-threatening
2. Osteomyelitis 3. Cavernous sinus thrombosis 4. Orbital cellulitis 5. Meningitis, brain abscess, epidural empyema 6. Important to recognize and refer immediately to ENT 7. Red flags: i. Changes in vision, mentation or periorbital edema 8. Hospitalization, imaging, IV antibiotics, surgery |
|
|
Disuss Indications for referral to otolaryngology:
|
Sinusitis:
1. Important to recognize and refer immediately to ENT 2. Red flags: i. Changes in vision, mentation or periorbital edema 3. Hospitalization, imaging, IV antibiotics, surgery 4. Referral to ENT for evaluation and potential endoscopic sinus surgery o Important to recognize and refer immediately to ENT -- Osteomyelitis -- Cavernous sinus thrombosis -- Orbital cellulitis --Meningitis, brain abscess, epidural empyema |
|
|
Discuss the etiology, clinical presentation, and management of viral upper respiratory infections.
|
Et: Rhinovirus 30%,Coronavirus 10-20%,Parainfluenza virus 5%,Influenza virus 5%,Respiratory Syncytial virus 5%, Adenovirus 5%
Symptx:-Lo-grade fever, occas chills --Rhinorrhea – clear, watery -Nasal congestion, Sneezing, Sore throat, Non-productive cough --- malaise, myalgias, and HA -->Symptoms usually resolve in 5-8 days >Low grade fever may be present, Nasal & pharyngeal erythema •Not typical for adults to have enlarged tonsils -Congested turbinates & discharge -Sinus tenderness may be present -Occasional mild cervical adenopathy -May have mild pulmonary findings Tx: Stay home! Push fluids! NO Abx. Analgesics – •ASA, acetaminophen, NSAIDs Antihistamines – reduce sneezing, nasal discharge •Chlorpheniramine (Chlortrimeton) •Diphenhydramine (Benadryl) -Decongestants – decrease nasal symptoms •Pseudoephedrine (Sudafed) Expectorants – reduce sputum production •Guaifenesin -Zinc -Immune booster; inhibits viral replication |
|
|
Complications of a URI
|
Acute sinusitis
Acute otitis media (AOM) May precipitate acute asthmatic attack, or acute bronchitis Pneumonia may develop in susceptible patient DDx: May need to r/o acute strep pharyngitis |
|
|
Influenza
|
Acute febrile illness secondary to Influenza A or B
• Transmitted by respiratory droplets Outbreaks common during the winter Increased infection rates in children Increased complication rates in the elderly • Especially patients with history of COPD, diabetes mellitus, heart disease, or immunocompromise • Deaths due to secondary bacterial pneumonia - Prevention with vaccination • Different vaccine developed each year for most likely strain to appear |
|
|
Influenza continued
|
• Abrupt onset of fever – can be as high as 106F
• Sore throat, headache, myalgias, malaise, non-productive cough Clinical presentation – signs • Fever, clear nasal discharge, pharyngeal erythema, cervical lymphadenopathy • May see confusion and weakness in the elderly Severity of presentation separates influenza from URI Symptoms last from 3 days-2 weeks with convalescence 1-4 weeks |
|
|
Discuss the diagnostic evaluation used in the evaluation of upper respiratory infections including sinusitis.
|
Diagnostic Approach
Thorough history & physical CBC – signs of infection Electrolytes/glucose – hydration status Pulse oximetry/arterial blood gases – oxygenation Chest x-ray – for productive cough/fever Viral cultures from the nose or pharynx Enzyme immunoassays Treatment Management • Supportive care, including bedrest and anti-pyretics • Rimantadine and amantadine can help shorten the course • Neuraminidase inhibitors, Zanamivir and oseltamivir, are active about influenza A & B • May need to admit for signs of compromise Approximately 10% develop bacterial pneumonia as a complication |
|
|
Discuss Indications & Contraindications for influenza vaccination
|
Prevention: Mainstay is Vaccination
High risk patients: • Age > 50 • Resident of a long term care facility • History of pulmonary disease COPD or asthma • History of cardiovascular disease • Female in 2nd or 3rd trimester of pregnancy • Immunocompromised patients -Target groups at risk of transmitting virus to others….especially those at high risk • Health care providers • Employees at long term care facilities • Home care providers • Household members who have high risk family members |
|
|
Surgical Tx for Glaucoma, and Tx for Chronic Angle Closure Glaucoma.
|
In Chronic Angle-Closure Glaucoma: laser peripheral iridotomy/surgical peripheral iridotomy may be helpful.
SURGICAL PROCEDURES: -laser surgery -filtering surgery -cyclodestructive surgery -drainage device surgery |
|
|
Global epidemiology of Glaucoma
|
--In the US it’s estimated that 2% of people over 40 y/o have glaucoma, 25% of which are undetected. 90% of cases are open angle type. Worldwide 4.5 million people are bilaterally blind from chronic open-angle glaucoma and 4 million (50% of which live in China) are bilaterally blind from chronic angle-closure glaucoma.
|
|
|
Clinical Presentation of Acute Sinusitis
|
Clinical Presentation
1. Prior history of an URI with some improvement followed by a relapse 2. Fever, usually low grade 3. Nasal congestion 4. Purulent nasal discharge, PND seen in posterior pharynx 5. Facial pain/pressure (worse when bending over) i. Cheek pain with maxillary sinusitis ii. Retro-orbital pain with ethmoid sinusitis iii. Lower forehead pain with frontal sinusitis 6. Decreased smell 7. Dental Pain 8. Cough 9. Halitosis 10. Sinus tenderness to palpation – inconsistent 11. Transillumination of frontal or maxillary sinuses Absence of light transmission suggestive of fluid in sinus |
|
|
Otitis Externa
Presenatation & Management of |
Etiology Bacterial
GNR's - E. coli, Pseudomonas aeruginosa and Proteus vulgaris Gram + cocci – Staphylococcus aureus Fungal :Asperigillis 80-90%, Canada albicans CP: Ear Pain, Pruritis, Discharge -Pseudomonas infx – green discharge -Staphylococcus aureus – yellow discharge -Fungal Infection – can be fluffy and either white or black >External Auditory Canal may be erythematous and edematous May have decreased hearing if marked swelling of the EAC or significant discharge - Conductive hearing loss as a result of swelling Note the appearance of the TM whether TM is intact Mgmt: Keep EAC clean, remove debri to promote healing -irrigate with hydrogen peroxide if TM intact -clean ear under direct vision using a wire loop/cotton swab --refer to ENT (they have special microscope to use) |
|
|
Clinical Presentation and Etiology of Cataracts
|
Etiology: leading cause of blindness worldwide. Usually bilateral.
→May be congenital (from TORCH infections esp. CMV & rubella AND inborn errors of metabolism). →Traumatic →2ndary to systemic disease → DM, myotonic dystrophy, atopic dermatitis →systemic or inhaled corticosteroid tx →Uveitis Senile Cataract is most common type; most over 60y/o have some lens opacity. SMOKING increases risk for formation. Clinical Presentation: Cataract = opacity of crystalline lens. Pt will experience gradually progressive blurred vision (but will notice ‘second sight’ where there is temporary improvement in vision before opacifying). No pain or redness. Cataracts clinically present as: progressive blurring of vision. It may be seen through a dilated pupil (even at early stages) with an ophthalmoscope or slit lamp. As the cataract matures the retina will become increasingly difficult to see. Final: fundus reflection is absent, pupil is white. |

