![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Innervation of lip (both sensory & motor)? |
Sensory: Trigeminal nerve (V2) Motor: Facial nerve (VII) |
|
|
|
Chance of a parent with cleft lip/palate have a child affected? |
A parent affected by CL/P has a 3% to 5% risk of having an affected child. |
|
|
|
Three components of microform cleft lip? |
Microform (forme fruste) cleft lip has three components: Small notch in vermilion, band of fibrous tissue running from edge of red lip to nostril floor, and a deformity of the ala on the side of the notch. |
|
|
|
Typical age of cleft lip repair? |
3 months |
|
|
|
Typical age of palatoplasty? |
9-18 months |
|
|
|
Typical timing of alveolar bone grafting in CL/P? |
9-12 years |
Utah tends to do this much earlier. |
|
|
In Millard rotation advancement, what does the C stand for? |
C flap, or columellar flap, is triangle of skin beginning interiorly at high point of Cupid's bow. |
|
|
|
Palate embryology: 1. What makes up the primary palate? Weeks of gestation? 2. What makes up the secondary palate? Weeks of gestation? |
Primary: The lip, nostril sill, alveolus, and hard palate anterior to the incisive foramen. Weeks 4-7. Secondary palate: The hard palate posterior to the incisive foramen. Weeks 5-7. |
|
|
|
Which two bones is the secondary palate made of? |
Palatine processes of maxilla Palatine processes of palatine bone |
|
|
|
Dominant blood supply to the hard palate? Where does it come from? Dominant innervation? How do they get to the hard palate? |
Greater palatine artery (from the maxillary artery, via the descending palatine artery) and greater palatine nerve (CN V) pass through the greater palatine foramen, providing dominant hard palate supply |
|
|
|
Which muscle of the velum is not innervated by the pharyngeal plexus, and what is its innervation? |
All muscles of the velum are innervated by the pharyngeal plexus (CN IX, CN X, and contributions from CN XI), except for the TVP, which is supplied by CN V. |
|
|
|
Parent with CL/P, one child with CL/P: Risk for next child is ?% |
Parent with CL/P, one child with CL/P: Risk for next child is 17% |
|
|
|
Most common cleft lip/palate associated anomaly? What is the palate like? |
Robin sequence (RS) is the most common associated anomaly. •Triad includes micrognathia/retrognathia, glossoptosis, and airway obstruction. CP is a common but not essential finding. •When present, the palatal cleft is typically very wide and U-shaped, compared with the V-shaped cleft of the palate without RS. |
|
|
|
Which syndrome/genetic mutation in Type II collagen is responsible for cleft palate? Three other associated findings? |
Stickler syndrome: 25% of syndromic ▸Autosomal dominant ▸Mutation in gene for type 2 collagen ▸RS, ocular malformations, hearing loss, and arthropathies |
|
|
|
If a cleft palate patient has Cardiovascular abnormalities, abnormal facies, developmental delay, which syndrome do we think of? How is it diagnosed? |
Velocardiofacial (Shprintzen's) syndrome: 15% of syndromic CP18 ▸Autosomal dominant with variable expression ▸22q11 “CATCH 22” chromosomal deletion (diagnose with fluorescence in situ hybridization [FISH]) cardiac anomalies, abnormal facies, thymic aplasia, cleft palate, hypocalcemia/hypoparathyroidism—CATCH). |
|
|
|
Which cleft syndrome has findings of lip pits? Inheritance pattern? Gene? |
Van der Woude syndrome: 19% of syndromic CL/P and CP15 ▸Autosomal dominant with 70%–100% penetrance IRF6 is the mutation |
|
|
|
Where do most palatal fistula occur? Indication for treatment? |
Incidence: 5%–60%, most at hard-soft palate junction Treat only if symptomatic. |
|
|
|
Which muscle is the target of VPI surgeries? |
The palatopharyngeus muscle is one of the two structures (arches) that surround the oropharyngeal tonsils. Its action is to pull the pharynx upward during swallow to help separate the oropharynx from the nasopharynx. A sphincter pharyngoplasty transposes bilaterally the palatopharyngeal muscles to create an even greater barrier from the oropharynx to the nasopharynx to decrease velopharyngeal insufficiency (VPI). |
|
|
|
Which tooth is most affected by cleft lip/palate? |
Lateral incisor |
|
|
|
Failure of fusion of which of the following results in the formation of a cleft of the lip? A) Frontonasal and maxillary prominences during the first 4 to 5 weeks of gestation B) Frontonasal and maxillary prominences during the first 9 to 11 weeks of gestation C) Lateral nasal and maxillary prominences during the first 2 to 4 weeks of gestation D) Medial nasal and maxillary prominences during the first 9 to 11 weeks of gestation E) Medial nasal and maxillary prominences during the first 6 to 8 weeks of gestation |
E) Medial nasal and maxillary prominences during the first 6 to 8 weeks of gestation |
|
|
|
A 5 yo boy with a history of cleft palate repair has VPI with satisfactory lateral wall motion. Which surgery should be used to correct this? Which surgery would be used if he had a large posterior gap & poor lateral wall motion instead? |
Satisfactory lateral pharyngeal wall movement and sagittal or circular velopharyngeal closure patterns should be treated with a pharyngeal flap. A large posterior gap with coronal, circular, or bowtie patterns of closure and good velar elevation, but poor lateral wall motion, should be treated with a sphincter pharyngoplasty. |
|
|
|
A 6-year-old boy with velopharyngeal insufficiency is brought to the office for sphincter pharyngoplasty. History includes repair of a cleft palate as an infant. Innervation of the muscle used to create the sphincter arises from which of the following? A) Cranial part of the accessory (XI) nerve B) Glossopharyngeal (IX) nerve C) Greater and lesser palatine branches of the pterygopalatine ganglion D) Hypoglossal (XII) nerve E) Medial pterygoid nerve
|
The correct response is Option A. Sphincter pharyngoplasty for correction of velopharyngeal insufficiency is performed by elevation of myomucosal flaps from the posterior tonsillar pillar, which involves the palatopharyngeus muscle. The palatopharyngeus muscle is supplied by the cranial part of accessory (XI) nerve through the pharyngeal branch of vagus (X) nerve via the pharyngeal plexus. |
|
|
|
Which of the following structures arises from the lateral nasal processes during embryologic development? A) Columella B) Nasal ala C) Nasal septum D) Nasal tip E) Premaxilla
|
The correct response is Option B. Nasal ala. |
|
|
|
Draw the 4 types of Veau palates. |
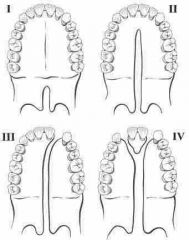
Back (Definition) |
4 types. 1&2 are a different entity than 3&4 |
|
|
Which muscle is used in a posterior pharyngeal flap? |
The superior pharyngeal constrictor is the muscle from the posterior pharyngeal wall that is utilized in the posterior pharyngeal flap. |
|
|
|
A 2-year-old boy with a cleft palate and recurrent episodes of serous otitis media caused by impaired eustachian tube function is scheduled to undergo cleft repair. In reconstructing the palate, repair of which muscle is most likely to improve eustachian tube function? |
Levator veli palatini |
|
|
|
Best tool to make decisions to diagnose & treat VPI after speech evaluation has been performed? |
Video nasal endoscopy |
|
|
|
Biggest benefit of NAM in bilateral cleft cases? |
biggest benefit of NAM in the bilateral cases is the correction in columella height |
|
|
|
PTCH1 is found in ____ syndrome, also known as ____ syndrome. |
PTCH1 is found in Gorlin syndrome, also known as basal cell nevus syndrome |
|
|
|
Which gene mutation is associated with Kallmann syndrome (hypogonadotrophic hypogonadism with anosmia, cleft lip and/or palate, renal aplasia/agenesis, dental defects)? |
FGFR1 is associated with Kallmann syndrome (hypogonadotrophic hypogonadism with anosmia, cleft lip and/or palate, renal aplasia/agenesis, dental defects). |
|
|
|
Trisomy 13 is associated with ____ syndrome (cleft ___, what type of feet? Head? Which system also has defects?) |
Trisomy 13 is associated with Patau syndrome (cleft palate, CNS disorders, microcephaly, polydactyly, rocker bottom foot, urogenital defects, and cardiac anomalies. |
|
|
|
A 3-year-old boy is evaluated for unilateral cleft lip and palate. Tympanogram shows bilateral noncompliance. Which of the muscles is most likely responsible for this finding? |
Flat tympanograms indicate the eustachian tubes are not draining properly. The action of the tensor veli palatini is key in the equalization of pressure between the middle ear and nasopharynx. In a child with a cleft palate, the tensor is abnormally inserted into the levator palatini, and as a result, there is an increased incidence of ear eustachian tube dysfunction. |
|
|
|
A 10-year-old boy who previously underwent palatoplasty for cleft palate is evaluated because of velopharyngeal insufficiency associated with minimal palatal elevation and coronal closure pattern. The most appropriate procedure to treat this patient targets which of the muscles? What is the procedure? |
A sphincter pharyngoplasty transposes bilaterally the palatopharyngeal muscles to create an even greater barrier from the oropharynx to the nasopharynx to decrease velopharyngeal insufficiency (VPI). |
|
|
|
Lefort I advancement & lengthening is known to cause facial changes: - upper lip vermillion? - upper lip height? - depth of nasolabial folds? - tooth show in repose? - alar base? - nasolabial angle? |
Le Fort I advancement and lengthening can result in dramatic changes to facial appearance. These include increased midfacial projection and fullness, increased upper lip vermilion fullness, decreased upper lip height, decreased depth of the nasolabial folds, and increased tooth show in repose and smile. Additionally, as the bony platform of the caudal piriform region is advanced, the alar base widens, and the tip rotates cephalad, increasing the nasolabial angle. |
|
|
|
An 8-year-old boy with a history of submucous cleft palate presents with persistent velopharyngeal insufficiency. Surgical history includes a Furlow palatoplasty 3 years ago, with subsequent revision to a superiorly based pharyngeal flap for persistent hypernasality 1 year ago. He had no improvement after the second surgery and speech therapy. Physical examination shows an intact, high and wide pharyngeal flap. Nasoendoscopy shows patent lateral oronasal ports and poor palatal and lateral pharyngeal wall motion. Which of the following treatments is most appropriate in this patient? A) Fabrication of a custom palatal elevator B) Pharyngeal flap port revision C) Posterior wall augmentation with fat grafting D) Speech therapy with retraining E) Sphincter pharyngoplasty |
Because this is neurogenic, it will be difficult to correct with surgery, so the best option becomes a palatal elevator used when talking to close off the nose posteriorly by pushing up the posterior soft palate. Posterior augmentation with fat grafting would decrease the size of the posterior gap but without adequate closure would still not correct the problem. The child has been in therapy and has failed to show improvement so additional therapy especially in light of the neurologic problem is unlikely to do anything but frustrate the child. A sphincter pharyngoplasty is not a viable option because a pharyngeal flap has been done and without adequate muscle function would fail. |
|
|
|
Stigmata of cleft lip repair: 1. Rotation advancement? 2. Tennison or triangular flap repair? 3. Straight line? 4. Bilateral? |
1. If there is inadequate rotation, the rotation-advancement repair can result in a short lip (white upper lip). 2. A Tennison, or triangular, flap repair can result in an elongated lip and a visible scar across the lower philtrum. The advantage of the rotation-advancement flap is that the design places the scar along the philtral ridge. 3. Straight-line repairs have been shown to result in blunting of Cupid’s bow. 4. An overly wide philtrum is a surgical stigma of a repaired bilateral cleft lip. |
|
|
|
A 6-year-old boy with a repaired unilateral complete cleft lip and palate presents for an annual cleft team clinic visit. Initiation of palatal expansion is discussed with the child’s parents. Timing for initiation of palatal expansion should be based upon? |
Canine eruption |
|
|
|
Satisfactory lateral pharyngeal wall movement and sagittal or circular velopharyngeal closure patterns should be treated with _________. |
a pharyngeal flap |
|
|
|
A 4-year-old girl who has velocardiofacial syndrome is evaluated because of severe velopharyngeal insufficiency. Reconstruction using a superiorly based pharyngeal flap is planned. What is the most important factor in determining the width of the flap? |
Lateral pharyngeal wall motion. This procedure involves elevating a rectangular flap, based superiorly or inferiorly, from the posterior pharynx and insetting it into the soft palate. The posterior raw surface of the flap is typically lined with trapezoidal flaps raised from the nasal side of the soft palate to limit contraction. The flap serves to obstruct air leakage into the nasal passage during speech. Extremely wide flaps can, consequently, also result in obstructive sleep apnea. In such situations, sphincter pharyngoplasties (Hynes) are sometimes used to avoid this potential complication. |
|
|
|
Which side is the nasal spine deviated to in unilateral cleft lip/palate? What about the projection of the pyriform aperture and dentoalveolar arch on the cleft side? |
Deviation to the noncleft side and decreased projection of the pyriform aperture and dentoalveolar arch on the cleft side |
|
|
|
A 7-year-old girl with a history of cleft lip and palate is brought to the office because of hyponasal speech, which is confirmed by the speech language pathologist. The patient and her family report that people have no trouble understanding her speech. Medical history includes primary cheiloplasty, primary rhinoplasty, primary palatoplasty, and posterior pharyngeal flap. Which of the following is the most appropriate next step in management? A) CT scan of the face B) Genetics referral C) MRI of the palate D) Polysomnography E) Swallow study |
D) Polysomnography Hyponasal speech describes the sound production when not enough air gets through the velopharyngeal sphincter, resulting in a muffled nasal voice, as if someone was holding his or her nose. This is in contrast to hypernasal speech, where the velopharyngeal sphincter is incompetent, resulting in leakage of excess air with an airy nasal voice. In this scenario, the most likely reason for hyponasal speech is an exuberant posterior pharyngeal flap that is blocking too much of the velopharyngeal complex. The two reasons to treat this are for speech issues that prevent normal interaction and obstructive sleep apnea (OSA). Given that the patient has no problems with people understanding her speech, the most reasonable next step among the choices is polysomnography to evaluate for OSA. |
|
|
|
In a child with prior straight line cleft palate repair, what should be done for hypernasality if the velum appears to vault and the palate elevated well with phonation? |
conversion Furlow palatoplasty- vaulting of the velum is indicative of anterior placement of the levator veli palatini muscles |
|
|
|
A 2-year-old has a midline cleft of the upper lip. This cleft results from failure of fusion of which embryologic structures? |
Median cleft lip results from failed fusion of the medial nasal prominence during embryologic development. A unilateral cleft lip results from failed fusion of the medial nasal prominence and the maxillary prominence. |
|
|
|
percentage of patients with isolated cleft palate who are most likely to have middle ear effusion? |
90% |
|
|
|
A 7-year-old boy with a history of bilateral cleft lip and palate has undergone multiple procedures including lip and nose repair, palate repair, and closure of an oronasal fistula. His parents note that during the past 6 months he has had nighttime snoring, frequent pauses in his breathing, and daytime somnolence. Physical examination shows mixed dentition with severe midface hypoplasia and Angle class III malocclusion with 12 mm of negative overjet. A polysomnogram demonstrates an obstructive apnea-hypopnea index (AHI) of 12.5 per hour. The patient is otherwise healthy. What is the best treatment option for this patient?
|
Continuous positive airway pressure (CPAP) Although midface advancement surgery (either conventionally or with distraction) is often used to address obstructive sleep apnea, this patient is a poor candidate for the surgical options provided. The patient is in mixed dentition, and a Le Fort I level surgery would risk permanent injury to his unerupted adult teeth. Although a Le Fort III osteotomy would avoid injury to tooth roots, it would also advance his infraorbital rims, which are not affected in patients with cleft lips. A tracheostomy will bypass his midface level obstruction; however, it is associated with significant cost, burden of care, and a 1% annual mortality risk and should be avoided if less invasive options exist. |
|
|
|
Is cleft lip/palate or cleft palate only more likely to be syndrome associated? Gender difference? |
The majority of orofacial clefts are nonsyndromic (70% of all cleft lip/palate; 50% of all cleft palate only). Cleft lip/palate is more common in males (2:1) and cleft palate only is more common in females (1:2). |
|
|
|
Risk of child having a cleft if one parent & one sibling are affected? |
17% |
|
|
|
3-month-old infant with 22q11.2 deletion syndrome is evaluated for an isolated cleft of the soft palate (Veau I). A Furlow palatoplasty is planned at age 9 months. Compared with nonsyndromic patients with the same cleft type, this patient will have a higher postoperative risk for? |
VPI |
|

