![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Myeloproliferative disorders definition and classifications |
Clonal disorder of hematopoetic stem cell Acute-ANLLs Chronic-Myeloproliferative disorders |
|
|
MPD diseases |
Chronic Myelogenous Leukemia (CML or CGL) Chronic Neutrophilic Leukemia Chronic Monocytic Leukemia Polycythemia Vera (PV) Essential (primary) Thrombocytosis (ET) Chronic Idiopathic Myelofibrosis |
|
|
Characteristics of chronic MPDs |
Panhyperplasia of BM Extramedularry hematopoeisis BM fibrosis Overlapping manifestations between diseases Frequently terminate in an acute leukemia BM-increased megakaryocytes-often abnormal Plt dysfunction Cytogenetic abnormalities |
|
|
Chronic Myelogenous Leukemia |
CML (formly CGL) Most common over 45 yrs of age Abnormal Philadelphia chromosome Eosinophili and basophilic leukemias are rare varients of CML and usually run an extremely acute course |
|
|
Philadelphia Chromosome formation |
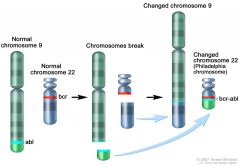
Ph22 or Ph1
Translocation of long arm of 22 to long arm of 9 Results in fusion gene BCR-ABL (Ph22) |
|
|
Philadelphia chromosome function |
BCR-ABL gene produces specific new protein-Tyrosine Kinase Tyrosine kinase stimulates uncontrolled production of abnormal blood cells by the BM Apoptotic functions are lost |
|
|
CML lab findings |
90% of CMl are Ph22 positive Ph22 negative CML tend to have atypical disease, more acut ecourse, less responsive to chemotherapy WBC 50,000- 800,000 / mm3 Blood resembles marrow Shift to the left with fewer than 10% blasts Pseudo pelger huet possible LAP DECREASED Thrombocytosis Anemia-few nrbcs Increased basophils, occ eos Hypercellular marrow, M:E ratio 10 to 50:1 May see pseudo-gaucher cells- -sea blue histiocytes in marrow (tissue macrophage) |
|
|
CML blast crisis |
AKA acute transformation Transforms to AML (M2) or ALL After acute phase transition- life expectancy is 2-6 months |
|
|
CML treatment |
BM transplant Imatinib mesylate (Gleevec) Dr. Brian Druker-OHSU Inhibits mutant tyrosine kinase activity of the BCR-ABL fusion gene Prolongs chronic phase, but blast crisis still occurs |
|
|
Chronic Neutrophilic Leukemia |
Very rare Very high WBC Slightly decreased plt Mild anemia **Persistence of neutrophilic leukocytosis without evidence of left shift and absence of sepsis** Bands present yet <10% immature neutrophils in blood Toxic granulation and Dohle bodies may be present Extremely high LAP (350-400) |
|
|
Chronic Monocytic Leukemia |
Very rare Not a WHO classification anymore Increased number of mature monocytes in blood and or marrow Monocytosis is often not initially seen- often develops after splenectomy |
|
|
Polycythemias |
Polycythemia vera (PV)- polycythemia rubra vera Secondary Polycythemia Relative Erythrocytosis |
|
|
Polycythemia Vera |
Malignant increase in Red Cell Mass JAK2V617F gene mutation Extramedullary hematopoiesis **BM hypercellular- malignant increased erythropoeisis, myelopoesis, and megakaryopoiesis Rbcs initially normal As progresses-ineffective extramedullary hematopoiesis leads to increased aniso and poik |
|
|
JAK2V617F Gene mutation |
PV Allows production of rbcs independent of EPO -Endogenous erythroid colony formation (EEC) Rbcs are extremely sensitive to EPO -Decreased EPO level typically |
|
|
Polycythemia vera lab findings |
Increased granulocytes and platelets Increased LAP Normal arterial O2 saturation **Hemostasis results may be effected by improper anticoagulant to blood ratio |
|
|
Polycythemia vera Iron studies |
Iron deficiency develops Ongoning bleeding from plt hypo function Repeated therapeutic phlebotomy Increased rbc production and Fe turnover Decreased rbc survival Actually a desired effect because it limits the expanding rbc mass. A greatly expanded rbc mass increases change of thrombosis. Portal vein thrombosis is a classic presenting symptom |
|
|
Long term PV |
Tear drop cells Increasing myelofibrosis Most common transition of PV to "spent phase" or postpolycythemic myeloid metaplasia |
|
|
Secondary Polycythemia |
Due to hypoxia Decreased arterial O2 saturation EPO increased RBC mass increased BM-increased erythropoeisis Normal granulocytes and platelets LAP normal |
|
|
Relative Erythrocytosis |
Decreased plasma volume-elevated hcct, normal rbc mass Normal O2 saturation Normal EPO Normal granulocytes and plts-LAP normal 2 groups -dehydration most common -asymptomatic middle-aged white males --hypertensive, obese, long history of heavy smoking |
|
|
Essential Thrombocythemia (ET) Primary |
BM-increased megakaryopoeisis-slightly increased granulopoeisis Plt count >600,000 / mm3-often > 1,000,000 Spontaneous plt aggregation and plt fxn defect Thrombotic and hemorrhagic complications 30-50% pts have JAK2 gene mutation w/ EEC |
|
|
ET blood smear |
Large masses of plt aggregates Giant and bizarre forms, many small forms also Occ. megakaryocyte fragment Mild normocytic, normochromic anemia -unless iron defic. due to excessive bleeding Elevated WBC- neutrophilia, occ increased eos and basos |
|
|
Chronic Idiopathic Myelofibrosis (CIMF) |
Formerly myeloid metaplasia w/ myelofibrosis *Marrow fibrosis- JAK2 gene mutation results in higher CD 34+ cell count which correlates to progression to marrow fibrosis *Extramedullary hematopoeisis *Leukoerythroblastosis Hallmark of disease is many tear drop cells and abnormal megakaryocyte proliferation |
|
|
CIMF lab results |
WBC/Plts- Increased, normal or decreased. granulocytes may have nuclear or cytoplasmic anomalies, platelets have impaired aggregation, may be agranular Anemia- BM failure, ineffective erythropoeisis and hemolysis, bleeding As disease progresses- mroe nrbcs, immature granulocytes, megakaryocytic fragments and microplatelets |

