![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
260 Cards in this Set
- Front
- Back
|
Which membranes are AChesterases present on? Why?
|
both the post and presynaptic membrane because they are present by any ACh receptor and there is M2 on the presynaptic membrane
|
|
|
What do the direct cholinergic drugs do?
|
anything that acts directly on receptors, pre or post synaptic
|
|
|
Are indirect drugs necessarily directed on cholinergic receptors?
|
no, they just kind of increase ACh or it's effects. they can act at totally different receptors/
|
|
|
What are the two main classes of direct muscarinic agonists?
|
1. Choline esters
2. Alkaloids from plants |
|
|
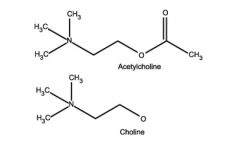
What does a choline ester look like compared to ACh?
|
almost the same except instead of acetate they have another group attached to choline
|
|
|
What are some examples of choline esters?
What root word do they all have in common? |
CHOL
1. ACh 2. Methacholine 3. Carbachol 4. Bethanechol |
|
|
For these drugs, say whether they act on Nicotinic, Muscarinic, or both.
1. ACh 2. Methacholine 3. Carbachol 4. Bethanechol |
1. ACh (both)
2. Methacholine (M) 3. Carbachol (M and some N) 4. Bethanechol (M) |
|
|
What are some examples of muscarinic alkaloids?
|
1. Muscarine
2. Pilocarbine |
|
|
Do we usually use ACh pharmacologically? Why? (3 reasons)
|
No because
1.. Short half life- it is broken down very quickly by cholinesterases (in seconds) 2. Not selective- if you put in a high dose, you could put you in hypotension and you have a bunch of other side effects with nicotinic and muscarinic receptors. 3. Can't cross BBB because too polar and large |
|
|
Why do these other cholinesterases last longer in the system to be useful?
|
Acetylcholinesterases don't break them down as effectively or at all (fit is not as good)
|
|
|
Show Choline structure vs acetylcholine
|
|
|
|
Where do we get choline from?
|
we can synthesize small amount of it, but we should probably supplement with foods like eggs. (unfortunately)
|
|
|
Mnemonic for action of Bethanechol?
Can bethanichol cross the BBB? Why? |
Beth activates Bowels and Bladder
No because it is incredibly similar to ACh in structure and isn't much more nonpolar. |
|
|
Show the structure and substitution group of bethanechol
What additional thing does it have to make it resistant to ACE action? |
it has an extra methyl group on the choline to make it impossible to bind to ACE.
|
|
|
What is a big contraindication to bethanechol for urinary reasons? Why?
|
if the person has some sort of urinary obstruction because then there will be increase pressure in the bladder and perhaps rupture
|
|
|
What are some causes ob obstructive urinary rention? (2)
|
1. stones
2. BPH |
|
|
What are some indications for using bathanechol?
|
1. post operative urinary retention - neural input is depressed to urinary system
2. post partum urinary retention - damage to muscle and nerves in birth 3. Basically anything that causes hypotonic, myogenic, or neurogenic bladder deficits |
|
|
What are contraindications to bethanichol for bowel reason?
|
any kind of obstructiion
|
|
|
What are some indications for bethanechol for bowel retention? (4)
|
1. Post operative adynamic ileus
2. Atonic stomach/gastroparesis 3. Ileus due to toxic reasons 4. Congenital megacolon |
|
|
Describe Post operative adynamic ileus
|
after an operation, the GI tract may not be mobile for a long time from paralysis.
|
|
|
Describe atonic stomach/gastric paralysis.
|
no contraction of stomach
|
|
|
How much of the colon is controlled sacrally via PS?
|
the last 1/3 of the transverse colon
|
|
|
Why does the sacrum only control the last third of the transverse colon?
|
before that, the vagus supplies the GIT
after that, the pelvic splanchnic nerves from S2-4 supply it |
|
|
Describe what is wrong in megacolon
|
there is a missing segment of the colon that didn't get PS from vagus or pelvic splanchnic nerves. Since it doesn't move, it starts to outpouch and expand.
|
|
|
Sum up what essentially are the side effects of bethanechol.
|
generalized parasympathetic stimulation
|
|
|
Describe these side effects. (hint: they are general side effects for all cholinergic drugs)
|
pupils- miosis and blurred vision
skin- flushing and sweating vessels- hypotension abdomen- cramps urine and bowel- urgency lungs- bronchoconstriction cardio- bradycardia |
|
|
What are some diseases that are contraindications on the general systemic level to cholinergic drugs in the...
1. lings 2. stomach 3. heart 4. thyroid 5. brain |
1. asthma/COPD
2. peptic ulcer 3. ischemic heart disease 4. hyperthyroidism 5. parkinson's |
|
|
Why is it contraindicated in ischemic heart disease?
|
there is a risk of hpoperfusion with hypotension
|
|
|
Why is it contraindicated in hyperthyroidism?
|
they already are at risk for a flutter/fib so decreasing the atrial refractory period even more is bad more them.
|
|
|
Why is it contraindicated in Parkinson's?
|
their balance between dopamine and ACh is also dysbalanced
ou can exacerbate the symptoms |
|
|
What is the scope of carbachol?
|
both M and N
|
|
|
Is carbachol used systemically? Why?
|
no because it activates preganglionic nicotinic for S and PS so it kinda fights with itself for overall effects
|
|
|
What context do we use carbachol in?
|
for glaucoma in eyes
|
|
|
What is the action in the eyes of carbachol? What is the net result?
|
constriction of pupillary sphincter for miosis
constriction of ciliaris for near sightedness net result is to reduce intraocular pressure |
|
|
Is it the first drug we use for glaucoma?
|
No, that is pilocarpine
|
|
|
When is carbachol used then?
|
as a second line treatment when pilocarpine doesn't work
|
|
|
Mnemonic for carbachol
|
if you have glaucoma fluid in your eye, dab a piece of bread (CARB) to clear it up
|
|
|
What is methacholine used for? Why?
|
it is used as a challenge test for diagnosis of hyperreactive airways (asthma). Normal people will only slightly bronchoconstrict but asthmatic pts will have a larger reaction.
|
|
|
What should you have on hand for a methacholine test?
|
a bronchodilator
|
|
|
Mnemonic for methacholine?
|
breath-a-choline
you are inhaling choline (esterase) which is a bronchoconstrictor to test for asthma. (why else would you wanna inhale choline? |
|
|
Why isn't pilocarpine ending with a -chol if it is cholinergic?
|
it is one of those plant derivatives that don't have choline esterases
|
|
|
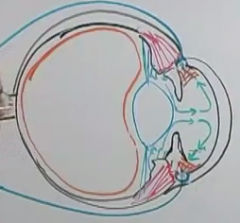
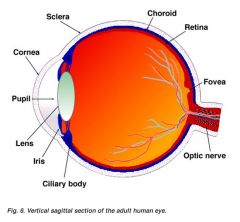
Describe the circulation of aqueous humor in the eye. Relate it to CSF circulation when you can. (4 steps)
|
1. fluid is produced by epithelium of ciliaris (like choroid plexus) in the posterior chamber
2. flows in front of the iris/lens through the pupil into the anterior chamber 3. hits the cornea and bounces back around to the corneal-sclera junction (reticular meshwork) 4. ah drained by canal of schlemm which is a venous drainage system (like arachnoid granulations) |
|
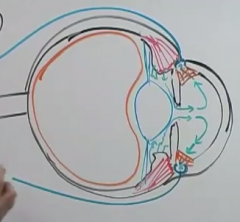
What is the big orange sac?
what is the sclera? |
orange sac- vitreous humore
sclera- the majority of the lining of the eye that isn't the cornea |
|
|
show the anterior and posterior chamber
|
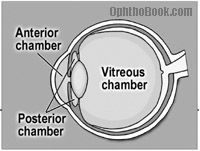
|
|
|
What is the pathophysiology of glaucoma?
|
buildup of aqueous humor in the eye
|
|
|
What does open and narrow angle glaucoma refer to?
|
the angle of the scleral-corneal junction
|
|
|
why would you have glaucoma in open angle? What population usually gets this?
|
the reticular meshwork is probably too tight together. old people usually get this.
|
|
|
WHat happens when the ciliaris contracts?
|
it will pull back the reticular meshwork and make it less dense.
|
|
|
Who gets narrow angle glaucoma?
|
those who were born with shallow anterior chambers
|
|
|
Under what conditions does the angle become too narrow?
|
when their pupils are dilating?
|
|
|
Why? show a pic.
|
because the pupillary dilator muscle are contraction and taking up space at the angle
|
|
|
What is an additional risk that happens with narrow angle when aqueous humor starts accumulating in the posterior chamber? Pic?
|
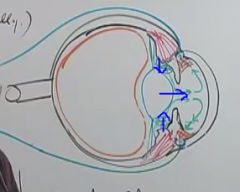
the iris gets pushed out and the angle closes even more
|
|
|
What sx would you get in this case?
|
a very red and painful eye
|
|
|
how does pilocarpine help in narrow angle?
|
the contraction of the pupillary sphincter will pull the pupil back tight and then the pupil dilatory muscle won't be blocking the drainage anymore.
|
|
|
Sum up, according to 1st aid, how pilocarpine helps open vs narrow angle glaucoma.
|
open- ciliaris contrction
narrow- pupillary sphincter contraction |
|
|
Mnemonic for side effects of Pilocarpine?
|
You dry, sweat, and drool onto your PILOw
|
|
|
What condition could you treat in the mouth using pilocarpine?
|
xerostomia
|
|
|
breakdown xero-stomia
|
xero- dry
stomia- condition of the mouth |
|
|
how would you administer pilocarpine for xerostomia? why
|
as a spray so that it hopefully hits our parotid glands.
|
|
|
What autoimmune disease can pilcarpine treat?
|
sjogren's syndrome which is commonly seen in females which destroys the lacrimal and salivary glands.
|
|
|
What other drug that is longer lasting can we use to treat sjogren's syndrome?
|
ceviline (another muscarinic agonist)
|
|
|
What drug that is put in the eye can you use pilocarpine to reverse?
|
something that results in mydriasis like atropine
|
|
|
Why would you ever switch back and forth between pilocarpine and atropine? (miosis and mydriasis)
|
if you have a condition where there are adhesions of the pupil dilatory muscles to the iris and you want to break them.
|
|
|
Mnemonic for both pilocarpine and carbachol used for glaucoma?
|
both have CARB/P's for the bread
|
|
|
NOW WE TALK ABOUT INDIRECT CHOLINERGIC DRUGS
|
HALFWAY THROUGH!
|
|
|
What is the main target for all indrect cholinergics?
|
to inhibit ACh esterases. (ACE)
|
|
|
What are the two main groups of indirect cholinergics?
What are they both referred to as? |
reversible and irreversible
anti-cholinesterases |
|
|
What is the difference in effect time between the two? Why?
|
reversible- shorter effect time because they get displaced after a while
irreversible- longer because you have to wait for the synthesis of all new ACE's. |
|
|
First we talk about the reversible ones
|
prganized
|
|
|
What is the two big divisions in the structures of the anticholinesterases?
|
some are tertiary amines and some are quartenary amines
|
|
|
What difference does this make? (3 places)
|
quartenary amines have a positive charge and so cannot cross the BBB, Gi mucosa, and ganglia as well
|
|
|
Which are the only two anticholinesterase that are tertiary amines?
|
physostigmine and donepezil
|
|
|
mnemonic for physostigmine and donepezil.
|
sounds like pfizer.
pfizer is the don of pharmaceuticals. they can get inside your head (quite literally) and everywhere else. |
|
|
What is unique about physostigmine about it origin?
|
it is the only anticholinesterase that is derived from an alkaloid plant. the rest are synthesized. (ironic when I think about the pfizer mnemonic.
|
|
|
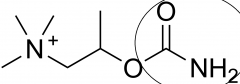
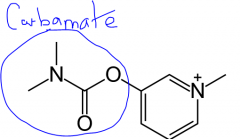
What are the functional groups on the anticholinesterases? Show pic.
|
all the -stigmines- carbamate
edrophonium- alcohol |
|
|
What difference does this make?
|
alcohol (edrophonium) doesn't make a covalent bond and dissociates quickly.
carbamate makes a labile covalent bond |
|
|
what is a labile covalent bond?
|
a covalent bond that can break easily
|
|
|
Show a stigmine with it's signature carbamate group
|
|
|
|
How long do the carbamates vs alcohols last then?
|
stigmines- 30 min - 2 hours
edrophonium- 10-20 min |
|
|
What suffixes do the irreversible antiACE's have?
|
-phate and -thion
|
|
|
What are the irreversible anticholinesterases? (not in 1st aid)
|
1. isoflurophate
2. ecothiophate 3. malathion 4. parathion |
|
|
What functional group makes a drug irreversibly bind with ACE?
|
an alkyl group
|
|
|
How doe this mechanism with the alkyl group work?
|
in the first 30mmin, the alkyl group is attached and you can pull the drug off ACE. But once it dettaches, there is no taking the drug off ACE.
|
|
|
What can pull off the drug with the alkyl group? (the antidote)
Mnemonic |
pralidoxime
I will pry the lid off this ACE |
|
|
What is the process by which the alkyl group is removed?
|
aging
|
|
|
Where do we encounter most of these irreversible anti ACE's?
|
in pesticides
|
|
|
What class of pesticides are they?
What is the danger that the produce? |
organophosphates
no ACE's means that there is a ton of ACh in the body and lots of PS effects |
|
|
What happens if ACh build up in....
1. the brain 2. ganglia 3. post effector site 4. NMJ |
1. the brain- seizures
2. ganglia- PS outflow 3. post effector site- PS outflow 4. NMJ- paralysis from overworked channels |
|
|
What should you give to treat all the parasympathetic effects of anti ACE toxicity?
When can this be done? |
atropine to cover the muscarinic receptors.
this can be done at anytime. |
|
|
When can you give pralidoxin?
|
within the half hour before aging has occurred.
|
|
|
So who gets organophosphate toxicity?
|
farmers
|
|
|
What is the recommended treatment? (2 drugs)
|
atropine- block muscarinic receptor
pralidoxime- regenerate active ACE |
|
|
mnemonic for pralidoxime?
|
farmers working in the PRArie mayy need pralidoxime as an antidote
|
|
|
What drug does Physostigmine have the same use as? (as only one of it's uses)
|
Bethanechol
|
|
|
How is it different than bethanechol? Why would it not be first line for urine and bowel?
|
it is an ACE inhibitor rather than a muscarinic agonist
it can cross the BBB so it is not used first |
|
|
How can you use physostigmine to improve glaucoma tx?
|
add it long with pilocarpine or carbachol
|
|
|
Mnemonic for which drugs to use first for glaucoma.
|
first, try to cry into your PILOw (pilocarpine). If that doesn't work, you can try dapping another piece of bread into your eyes (Carbachol) or calling Pfizer (physostigmine) or backup.
|
|
|
What is the main use of physostigmine though? Mnemonnic?
|
to reverse the effect of atropine
Physostigmine "phyxes" atropine overdose (or anything that has anticholinergic effects) |
|
|
What are some other drugs that have anticholinergic effects that are "phyxed" by physostigmine?
|
antipsychotic- phenothiazine
TCA's |
|
|
What are some potential unwanted side effects of anti-ACE's? (3)
These are cross referenced with lippincott. |
1. CNS overstimulation (convulsions)
2. Overstimulation and resulting failure at NMJ (paralysis) 3. Cardiac understimulation and collapse |
|
|
Is there is high chance that these side effects will occur? Why?
|
no, these are not common at therapeutic doses
|
|
|
Mnemonic for NEOstigmine? (2)
|
NO CNS penetration
Also NEO from the matrix can do a lot of stunt, which require very good working muscles. (great at stimulating NMJ) |
|
|
What is NEOstigmine more effective at than physostigmine?
|
it is much more potent at the NMJ and can stimulate contraction before it induces paralysis
|
|
|
So what types of conditions is NEOstigmine good for? (3)
|
anything to do with muscles
1. non obstructive ileus and urinary retention 2. reversal of NMJ bloackage post op 3. myasthenia gravis |
|
|
What is responsible for the pathophysiology of myasthenia gravis?
|
you produce autoantibodies to nicotinic receptors which causes the muscle to degrade it's own receptors
|
|
|
Breakdown myathenia gravis
What other term uses -asthenia? |
my- muscle
asthenia- weakness gravis- serious serious muscle weakness asthenic person = having abnormal physical weakness |
|
|
What type of drugs are used to treat MG?
|
anti-ACE's that do not cross the BBB (quaternary amines)
|
|
|
Do the sx of masthenia gravis get better or worse with exercise?
|
worse. you feel even more fatigued
|
|
|
What disease creates autoantibodies on the calcium channels on the presynaptic neuron of the NMJ?
|
eaton-lambert syndrome (or lambert-eaton)
|
|
|
How are the sx progression different between myasthenia gravis and eaton-lambert syndrome?
|
gravis starts out strong then weakens
eaton-lambert starts out weak and then strengthens |
|
|
Mnemonic for eaton-lambert vs myasthenia gravis?
|
there are two people and a cooked lamb on the table.
MG- starts out eating it well and then can no longer EL- starts out slow, but is eventually able to successfully EAT the LAMB |
|
|
What disease is eaton lambert associated highly with? Mnemonic?
|
Small cell (oat cell) carcinoma (lung cancer)
You have the lamb with a side of oats |
|
|
which disease responds to anti-ACE therapy? Why?
|
myasthenia gravis because a lot of ACh at the synapse can overcome the bound nicotinic receptors
But in eaton lambert, you don't have much ACh to begin with because the vesicles aren't releasing it so that doesn't help much. |
|
|
Which one is more common? How much so?
|
Myasthenia gravis- it is the most common NMJ disorder
Eaton-Lambert syndrome is fairly rare |
|
|
Which muscles are most affected in each syndrome?
|
MG- facial muscles, especially the eyes
EL- proximal limb muscles (out of 1st aid) |
|
|
What disease is myasthenia gravis highly associated with? Why?
|
thymic hyperplasia or thymoma
the thymus can be creating a ton of autoantibodies if it has unregulated growth |
|
|
What surgery usually helps with myastenia gravis? In what way?
|
the progression stops with a thymectomy
(the damage to the receptors has already been done?) |
|
|
Are there any more NMJ diseases?
|
not according for 1st aid
|
|
|
What type of toxin imitates myasthenia gravis?
|
tubocurarin
|
|
|
What is the cure for tubocurarin toxicity?
|
same as MG tx.
give non BBB crossing ACE inhibitor to increase ACh to competitively displace the toxin on the Nm receptors. |
|
|
Mnemonic for short and long term drugs to treat myasthenia gravis?
|
NEO(stigmine) uses a lot of muscle to climb the PYRImids (pyridostigmine).
P for prolonged NEO in short term |
|
|
A person who was dx with myasthenia gravis 5 years ago is probably on which drug?
|
pyridostigmine
(climbing the pyrimid) |
|
|
Mnemonic for use of Edrophonium?
|
This is a PHONEY drug
You use it to dx myasthenia gravis because it lasts for such a short time (doesn't bind tightly to ACE because of OH instead of carbamate group) |
|
|
Why is it's short action time so useful? How long does it last?
|
any diffuse side effects of PS stimulation will go away quickly within 10-20 min
|
|
|
What is the term for diffuse PS overstimulation?
|
cholinergic crisis
|
|
|
What is the cure if you start going into cholinergic crisis?
|
atropine
|
|
|
What is this dx test called? Mnemonic?
|
tensilon test (testing to see if they develop more ability for muscle tension)
|
|
|
Does the immunological assault on Nm receptors in MG stay constant?
|
no it waxes and wanes
|
|
|
What states is your body in if you are on a constant dose of anti ACE and the immune attack wanes? if it waxes?
|
wanes- too much ACh- cholinergic crisis
waxes- too little ACh- myasthenia crisis (very weak) |
|
|
What can you use to differentiate myasthenic and cholinergic crisis in a MG person?
|
inject edrophonium
if it gets better- myasthenic crisis if sx get worse- cholinergic crisis |
|
|
How come you can't just tell them apart by the sx?
|
muscles get weak when they are overstimulated AND understimulated by ACh
|
|
|
What does ACh do in the brain?
|
helps with learning and memory
|
|
|
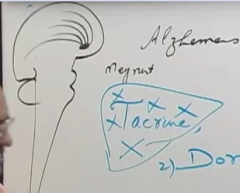
Where in he brain is ACh for this purpose mainly created?
|
nucleus of meynert
|
|
|
Show this nucleus and where it's fibers go.
|
|
|
|
What disease involves the degradation of these cholinergic fibers?
|
Alzheimer's
|
|
|
Mnemonic for which drug is used for alzheimer's.
|
The old DON has Alzheimer's
|
|
|
What is the mnemonic for cholinergic crisis?
|
Sine ACh help learning, when you have a lot of it, you are....
DUMBBLESS! Diarrhea Urinary incontinence Miosis Bradycardic Bronchoconstriction Lacrimation Excitation of skeletal muscle and CNS Sweating Salivating |
|
|
What is a good way to make sure you don't miss any of these sx?
|
go from head to toe and look at all the organ systems
|
|
|
NOW WE TALK ABOUT ANTICHOLINERGIC DRUGS!
|
ONLY 2/3 AS LONG AS CHOLINERGIC
|
|
|
do any of the antocholinergics work on ACE?
|
no
|
|
|
What are the 3 classes of anticholinergics?
|
1. muscarinic antagonists (M1-5)
2. ganglionic antagonists (Nn for S and PS) 3. NMJ blockers (Nm) |
|
|
If they all act directly, what does that mean about their structure?
|
they all resemble ACh
|
|
|
What is the similarity and difference between direct choinergic and anticholinergic drugs?
|
they both have affinity for the receptor, but antichoinergics lack intrinsic activity.
|
|
|
What are the two types of muscarinic antagonists?
|
Nonselective- bind M1-5
Selective- bind one or 2 types |
|
|
Whats the classic example and related compound of a nonselective muscarinic antagonist?
|
Atropine
and scopolamine |
|
|
What is an example of a M1 selective and M3 selective antagonist? (not in 1st aid, but in lippincottt)
|
M1- pirenzapine
M3- Darifenacine |
|
|
FIRST WE TALK ABOUT ANTIMUSCARINIC DRUGS
|
I'M TIRED BUT FUNCTIONING RIGHT NOW
|
|
|
What ACh receptors are present in the CNS? Where?
|
muscarinic in the brain
Nicotinic in the spinal cord |
|
|
What is another name for anti muscarinic drugs?
|
parasympatholytic drugs (even if they cross the BBB)
|
|
|
What happens to autonomic effector sites if you give an antimuscarinic drug?
|
they start to have unopposed sympathetic action
|
|
|
What plant is atropine derived from?
|

atropa belladonna
|
|
|
breakdown atropa belladonna
|
atropos- one of the 3 fates that was responsible for cutting the lifeline. people used to use this plant to poison enemies
bella donna- beautiful lady- women put this in their eyes to look more alluring |
|
|
What is the duration of atropine taken systemically vs put in the eye?
|
systemically- 3-4 hours
eye- 3-4 day |
|
|
What is the downside to wearing atropine to a date? Mnemonic with duration?
|
you get relaxation of ciliaris and can't see your date. It's a big sacrifice for beauty because atropine in the eyes creates cycloplegia for 3-4 days.
|
|
|
What does cyclo- mean?
|
referring to the ciliaris muscle
|
|
|
What is paralysis of the ciliaris muscle called?
|
cycloplegia
|
|
|
In what condition is atropine absolutely contraindicated? Why?
|
people with history of narrow angle glaucoma because there is unopposed action of the pupil dilatory muscle
|
|
|
What sx comes about from mydriasis?
|
photophobia
|
|
|
What are three ophthalamic uses of atropine?
|
1. Checking for refractive errors
2. Fundoscopic exams 3. Iridocyclitis or keratitis |
|
|
What is a refractive error from?
|
different curvatures of the cornea created by frequently focusing too much on far or near objects.
|
|
|
Why do you need clycloplegia to check for refracctive errors?
|
because the ciliaris will accomodate to make up somewhat for refractory errors. You cant to eliminate this.
|
|
|
What does the cornea/eyeball look like in near sightedness? What is this condition called?
|
it has a smaller radius of curvature. they eye is football shaped.
this is called myopia |
|
|
Is the refractive power higher or lower in myopia?
|
higher (image is projected earlier than the retina)
|
|
|
What is the opposite of myopia? Show a pic of the two.
|
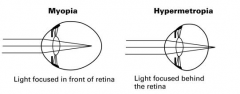
hyperopia/hypermetropia
|
|
|
What is iridocyclitis and keratitis?
|
iridocyclitis- inflammation of the iris and the ciliaris muscle
keratitis- inflammation of the cornea |
|
|
What is the pathological consequence of iridocyclitis and keratitis?
|
lots of proteins and inflammation will cause adhesions to form
|
|
|
Why would atropine be useful in this case?
|
if you paralyze the ciliaris and the pupillary sphinceter, all those structures will pull away from each other and prevent adhesion formation of iris and cornea or iris and lens
|
|
|
Show what the iris, lens, and cornea are
|
|
|
|
What are the satefty recommendations for someone going in for a dilation on eye exam? Why?
|
bring sunglasses- photophobia from mydriasis
bring someone to drive you home- blurry vision from cycloplegia |
|
|
Why don't we use atropine for this test anymore?
|
it takes too long to wear off
|
|
|
What drugs have the same action, but shorter half life?
|
1. Homoatropine
2. Tropicamide 3. Cyclopentalate |
|
|
Mnemonic for each of these dilating pupil drugs?
1. Homoatropine 2. Tropicamide 3. Cyclopentalate |
1. Homoatropine - works just like atropos belladonna
2. Tropicamide - better bring sunglasses if you are going to the tropics 3. Cyclopentalate- cyclopentalate causes CYCLOplegia |
|
|
What is an alternate way to shorten the time?
|
give a cholinergic like physostigmine to displace the anticholinergic with ACh
|
|
|
How can you cause mydriasis without cycloplegia? (drug)
|
give phenylephrine to activate sympathetic stimulation of pupillary dilator muscle
|
|
|
What receptor does phenylephrine act on?
|
excitatory so a1
|
|
|
When would you want to use phenylephrine instead of the others in the ED?
|
if you don't need to check for refractory errors.
say you just want a fundoscopic exam to check for AV nicking or optic disc blurring. |
|
|
What demographic doesn't need cycloplegia to check for refractory errors? Why?
|
people over 40 whose lens have become semisolid and don't change shape in response to ciliary contraction, which is also weakened.
|
|
|
Are their lens stuck in a more stretched or globular shape? how do you know?
|
more stretched because they lose the capacity for near vision.
|
|
|
Why can myopic people not make up for their deficits by squinting and hyperopic people can?
|
in myopic, your refractory power is already too high.
try it. distant things look blurrier when you squint. |
|
|
Why can looking at nature help with myopic vision? Why is looking at a screen all day bad?
|
you are stressing your eyes out by contracting the ciliaris all day looking at a screen
nature has many distant object which allow your ciliaris to relax |
|
|
What is the condition of losing your vision after 40 called?
|
presbyopia
|
|
|
breakdown presby-opia.
|
presby- old age
opia- a condition of vision |
|
|
What is the mnemonic for actions of atropine throughout the body? (5)
|
Blind as a bat
Dry as a bone Hot as a hare Red as a beet Mad as a hatter |
|
|
In what respects is the person blind as a bat? (2)
|
cycloplegia and mydriasis
|
|
|
In what respects is the person dry as a bone? (4)
|
1. Xero ophthalmia
2. Xerostomia 3. Decreased nasal and lower respiratory secretions 4. Anhydrosis |
|
|
What type of drug also incorporates antimuscarinics to help with nasal secretions?
|
antihistamines will be mixed with antimuscarinics to decrease nasal and respiratory secretions
|
|
|
What are decongestants?
|
drugs that relieve nasal congestion
|
|
|
What is usually the route of action of decongestant?
|
selective a1 smpathetic stimulation
|
|
|
What drugs are typically used as decongestants?
|
phenylephrine and pseudoephedrine
|
|
|
Why were anti muscarinics helpful in surgery in the past?
|
some anesthetics (old ones like ether) increased respiratory secretions, which would lead to pneumonia
antimuscarinics would dry out the respiratory system and prevent this |
|
|
Why do antimuscarinics create anhydrosis? I thought loss of sympathetic stimulation was supposed to do this.
|
the neurons may be sympatetics, but the NT is ACh and the receptor is muscarinic
|
|
|
In what respects is the person hot as a hare?
|
they can't sweat
"atropine fever" |
|
|
What demographic is atropine contradindicated in because of it anhydrosis?
|
infants because they can easily overheat and die
|
|
|
In what respects is the person red as a beet?
|
the person looks flushed on their skin
"atropine flush" |
|
|
Why are they flushed?
|
probably because they are overheating so the sympathetic stimulation is selectively turned off there (like in exercise)
|
|
|
In what respects is the person mad as a hatter?
|
overstimulation of ACh in the brain causes overactivation such as confusion and hallucinations.
|
|
|
What is the antimuscarinic of choice to treat COPD and asthma?
|
Ipatropium (ATROVENT)
|
|
|
What effect do antimuscarinics have on the GIT?
|
antispasmodic- stops movement
constipation |
|
|
What drug in america is used to control parietal glands in peptic ulcers?
|
glycopyrrolate
|
|
|
What else is glycopyrrolate used for?
|
to reduce airway secretions for preop
and to reduce Gi secretions of H+ and saliva |
|
|
How do you control which effect you get from glycopyrrolate?
What drug does Lippencott's say is used to limit basal H+ gastric secretion? |
parenteric route- respiratory
oral route- GI Lippencott- pirenzepine as a selective M1 inhibitor |
|
|
What is parenteric?
|
any route of drug administration that is not oral or rectal
|
|
|
What effect can antimuscarinics have on the urinary system?
|
decreases urination
|
|
|
Who would you want to use this on?
|
women with stress incontinence and people with cystitis
|
|
|
What is stress incontinence?
|
when your detrusor inappropriately contracts, causing excess pressure/stress on your bladder
|
|
|
What drug would work well for this purpose?
|
Oxybutynin
|
|
|
Mnemonic for oxybutynin?
|
If I need to pee like an ox, I should PUT IN oxybutynin.
antimuscarinic for stress incontinence (bladder spasms) and cystitis |
|
|
Draw out the PS innervation of the heart and include the receptors on the neuron and heart
|
presyaptic neuron- M1
heart- M2 |
|
|
What does atropine do to the heart rate at a low vs high dose?
|
low- bradycardia
high- tachycardia |
|
|
Explain this phenomenon.
|
at low dose, atropine preferentially binds with M1, which blocks the autoinhibition of the PS system
at a high dose, it will also block M2, taking off PS stimulation |
|
|
Will it be a large or modest tachycardia?
|
modest
|
|
|
If the atropine is working on the SA node for HR, what else is it working on?
|
the AV node, shortening the conduction velocity
|
|
|
What is atropine used to treat in the heart? (2)
|
1. AV blocks mobitz type 1.
2. sinus bradycardia |
|
|
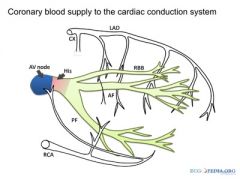
What condition could cause both of those two disorders? How?
|
A posterior inferior left myocardial infarction.
This blood vessel is the right coronary artery and it also supplies the AV node and SA node. |
|
|
Show the course of this vessel
|
|
|
|
And another pic from najeeb
|
|
|
|
What two drugs are used preoperatively?
|
atropine or glycopyrrolate
|
|
|
What are the 2 purposes of giving the anti muscarinics preoperatively?
|
1. decreases respiratory and salivary secretions to prevent later pnemonia
2. decrease vagal reflex |
|
|
Why do you want vagal reflexes inhibited before surgery?
|
the GIT has lot of vagal sensory fibers. If you disturb these, they can fire and initiate vagal efferent firing to the heart which would be really bad.
|
|
|
What will you give after surgery to reverse effects?
|
the muscle man, NEOstigmine to allow ACh to displace glycopyrrole
|
|
|
Mnemonic for glycopyrrolate
|
I am getting ULCERS just thinking about my surgery. My stomach (digests glucose) is on fire (pyrrole).
treats ulcers and used for preop |
|
|
What do you have to give neostigmine along with for the heart's sake? Why?
|
atropine
initially there is no antagonist on the heart so deactivating ACE there would cause undue PS action. You put in atropine to counter that. |
|
|
In what condition can atropine be used to prevent a toxicity?
|
anything that causes a cholinergic crisis (DUMBBLESS)
such as amanita muscarin poisoning, physostigmine overdose, and organophosphate toxicity |
|
|
In which of those can you also use pralidoxime?
|
any that involve antiACE's that haven't aged yet
(physostigmine and organophosphate) |
|
|
Is atropine anti-DUMBBLESS all the way?
|
No, it doesn't reverse the E. (excitation of brain and skeletal muscle)
|
|
|
Why doesn't it reverse E?
|
because those are nicotinic receptors
|
|
|
What sx does atropine cause in the brain initially?
|
initially stimulates the brain
1. delirium 2. hallucinations 3. convulsions |
|
|
What is delirium?
|
an acute confusional state with hyperactivity
|
|
|
What are hallucinations?
|
a perception present without an external stimulus
|
|
|
What will atropine cause in the brain later on? (1 general 4 specific)
|
depression of the brain
1. coma or depression 2. collapse of circulatory and respiratory systems 3. death |
|
|
Comparison of cholinergic and anticholinergic drug effects on the brain.
|
They both initially cause excitation of the brain, but the anticholinergics eventually cause depression, coma, and death
|
|
|
What mnemonic does this aspect of atropine toxicity refer to?
|
Mad as a hatter
|
|
|
What is scopolamine's effect in the CNS compared to atropine?
|
it depresses from the getgo while atropine excites then depresses
it also crosses the BBB better |
|
|
What is the main thing scopolomine is used to treat?
|
motion sickness
|
|
|
How does it help motion sickness?
|
it depresses the signals from the vestibular system
|
|
|
How is scopolamine usually given for motion sickness?
|
as a patch for behind the ear
|
|
|
Mnemonic for medical use of scopolamine
|
motion sickness
at least those drugged up women won't get car sick while they are being kidnapped |
|
|
Another name for scopolamine?
|
hyoSCine
|
|
|
What are the effects of someone drugged with scopolamine? Worst case scenario?
|
they don't know what is going on and have anterograde amnesia.
coma and death from respiratory failure could occur |
|
|
They used to use scopolamine and morphine as anesthesia for delivering babies. "twilight sleep" Why?
|
so the women could neither feel the pain nor remember that the experience
|
|
|
Why was this stopped?
|
1. Women felt uncomfortable not remembering it
2. the CNS depressive effects on the baby were not good for respiration |
|
|
What is the similarity and difference between ipatropium and tiotropium?
|
they both bronchodilate for asthma and COPD, but tiotropium has a longer half life
|
|
|
What anticholinergic is used for parkinson's? Why?
|
Benztropine
You want one that can cross the BBB and them tilt the balance of ACh and Dopamine in the basal ganglia more back towsrd dopamine. |
|
|
What other anticholinergic is used?
|
trihexylphenidyl
|
|
|
Mnemonic for use of Benztropine and trihexylphenidyl?
|
tropine- atropine (anticholinergic)
used for Parkinson's "A triple hex upon me for forgetting where I Parked my Benz" |
|
|
Mnemonic for ipatropium and tiotropium?
|
I PRAy (ipatropium) I can breathe soon. TIO prays for me later.
|
|
|
Other than oxybutyrin, what other drugs are used to treat overactive bladder disease according to lippincott?
|
Darifenacin, fesoterodine, oxybutynin, solifenacin, tolterodine, and trospium chloride
|
|
|
Why do we use oxybutnin though?
|
it can be used as a transdermal patch as so causes less side effects elsewhere
|
|
|
Are ganglionic blockers typically used? What receptor would it be?
|
no
it is Nn |
|
|
Why don't we use ganglionic blocking agents?
|
because it is very nonspecific and would inhibit all of autonomic outflow.
|
|
|
What is one famous example of a ganglion blocker?
|
Nicotine
|
|
|
How is nicotine's effect at the ganglia similar to ACh at the NMJ?
|
at low doses it excites, but at high doses it inhibits because the channel receptors stop responding
|
|
|
How come channel receptors go through this phenomenon?
|
if they are constantly stimulated, then the cell is stuck on depolarization and gets depleted because it has no chance to recover. (reset actin and myosin or regain NT's)
|
|
|
What is the only medical use for nicotine?
|
to wean people off smoking
|
|
|
there are also other ganglionic blockers. do they have the same mechanism of action as nicotine?
|
no they are non depolarizing competitive antagonists
|
|
|
What are they used for?
|
not medical used. they are used in experimental tests so we can see the direct effect of a drug on a tissue without any of the autonomic compensation
|
|
|
What one emergency would we use ganglion blockers for?
|
aortic dissection
|
|
|
Why aortic dissection? What is the aim?
|
it is an emergency and other drugs may be contraindicated. the aim is to lower bp to limit damage.
|
|
|
Why would ganglion blockers lower BP if they depress PS and S.
|
vessel control is mainly by the S NS.
|
|
|
This holds true for all organs. The ganglion blockers will favor the effects of the minority autonomic innervation. The majority of organs have which innervation prevailing?
|
PS
|

