![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
128 Cards in this Set
- Front
- Back
|
Function of Skeletal System
|
1. Support
2. Protection 3. Leverage 4. Storage of minerals 5. Blood cell production |
|
|
Storage of minerals =
|
the calcium salts of bone represents a valuable mineral reserve that maintains normal concentrations of calcium and phosphate ions in the body fluids. Calcium is the most abundant mineral in the human body. A typical human body contains 1-2 kg of calcium, with more than 98 % of it deposited in the bones of the skeleton.
|
|
|
Blood cell production =
|
also known as hematopoiesis; red blood cells, white blood cells, and platelets are produced in the red bone marrow, which fills the internal cavities of many bones.
|
|
|
Sutural bones =
|
also known as Wormian bones;
|
|
|
Sesamoid bones =
|
are generally small, flat, and shaped somewhat like a sesame seed. They develop inside of tendons and are most commonly located near joints at the knees, the hands, and the feet. Everyone has sesamoid patellae, or kneecaps, but individuals vary in the location and abundance of other sesamoid bones. This variation, among others, accounts for disparities in the total number of bones in the skeleton.
|
|
|
Depressions and openings allowing blood vessels and nerves to pass
|
i. Fossa
ii. Fissure iii. Foramen iv. Canal or meatus v. Sulcus or groove vi. Sinus |
|
|
Tuberosity=
|
large, round or rough projection that may cover a broad area
|
|
|
Epicondyle=
|
raised area above a condyle
|
|
|
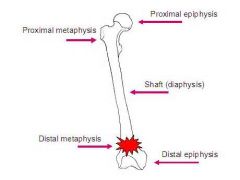
Diaphysis =
|
long tubular shaft that forms the axis of a typical long bone; the walls of the shaft are made primarily of compact bone.
|
|
|
Epiphyses =
|
ends of the bones composed primarily of spongy bone, also called trabecular bone.
|
|
|
Spongy bone
|
consists of an open network of struts and plates (called trabeculae) that resemble a latticework with red bone marrow filling in the spaces between.
|
|
|
The spongy bone
|
is then covered by a thin layer of compact bone and articular cartilage.
a. Proximal epiphyses b. Distal epiphyses |
|
|
Proximal epiphyses=
|
end closest to the origin of attachment.
|
|
|
Distal epiphyses=
|
end furthers from the origin of attachment.
|
|
|
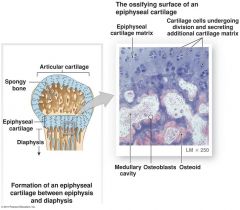
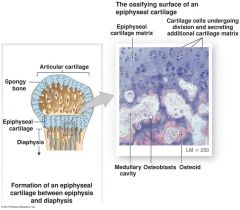
Metaphysis =
|
a narrow zone that connects the diaphysis to the epiphyses. The epiphyseal plate, a thin layer of hyaline cartilage more commonly called the growth plate, is important for growth in the length of bones.
|
|
|
Medullary cavity =
|
within the shaft of a long bone is a cavity where bone marrow is located. In childhood, the medullary cavity is filled with red bone marrow but as we age, fat accumulates within the red marrow transforming it to yellow bone marrow. Red bone marrow is important for hematopoiesis but yellow bone marrow is no longer hematopoietic and instead stores fat as an important energy source.
|
|
|
Membranes associated with bone:
Periosteum= |
outermost covering of bone made primarily of dense irregular tissue and held on by Sharpey’s fibers (collagen).
|
|
|
Membranes associated with bone:
Endosteum= |
internal membrane of bone made of connective tissue. Also lines the many canals that pass through bone to supply blood and nerves to the bone.
|
|
|
Nutrient foramen =
|
in order for bones to grow and be maintained, they require an extensive blood supply. The nutrient foramen is a tunnel that penetrates the diaphysis and provides access for the blood vessels into the shaft of the bone.
|
|
|
Nutrient foramen:
Nutrient artery = |
transports oxygenated, nutrient-rich blood to the bone.
|
|
|
Nutrient foramen:
Nutrient vein = |
transports deoxygenated, waste-laden blood from the bone.
|
|
|
Metaphyseal artery and metaphyseal vein =
|
carry blood to and from the area of the metaphysis and to the epiphysis.
|
|
|
Articular cartilage =
|
covers portions of the epiphysis that articulate with other bones. The cartilage is avascular, hyaline cartilage. It relies primarily of diffusion from the synovial fluid to obtain oxygen and nutrients and to eliminate wastes.
|
|
|
Microscopic anatomy of compact bone.
|
1. Osteon
2. Central canal 3. Perforating canals 4. Lamellae a. Circumferential lamellae b. Interstitial lamellae 5. Lacunae 6. Canaliculi |
|
|
Osteon =
|
the basic structural and functional unit of bone consisting of bone cells organized around a central canal and separated by concentric lamellae.
|
|
|
Central canal =
|
also known as the Haversian canal, runs parallel to the axis of bone and are located in the middle of each osteon. Each central canal possesses an artery and vein, lymph vessel, and nerve.
|
|
|
Perforating canals =
|
passageways that extend perpendicular to the axis of the bone and connect the central canals of adjacent osteons.
|
|
|
Lamellae =
|
nested, concentric rings of matrix surrounding the central canal.
a. Circumferential lamellae b. Interstitial lamellae |
|
|
Circumferential lamellae =
|
specialized lamellae found at the outer and inner surfaces of bone, where they are covered by the periosteum and endosteum, respectively. These lamellae are produced during the growth and maintenance of bone.
|
|
|
Interstitial lamellae =
|
fill in the spaces between adjacent osteons of compact bone. These lamellae are remnants of osteons whose matrix components have been almost completely recycled by the action of bone digesting cells.
|
|
|
Lacunae =
|
mature bones cells, called osteocytes, are trapped within an open space called a lacuna. Osteocytes cannot divide and therefore each lacuna contains only one osteocyte.
|
|
|
Canaliculi =
|
processes of the osteocytes extend into narrow crevices, called canaliculi, that penetrate the lamellae and connect the lacunae to the central canal.
|
|
|
Bone is associated with four cells that account for approximately 2% of the bones weight.
|
1. Osteocytes
2. Osteoblasts 3. Osteoprogenitor cells 4. Osteoclasts |
|
|
Osteocytes =
|
mature bone cells that maintain the protein and mineral content of the surrounding matrix through the turnover of matrix components. Osteocytes secrete chemicals that dissolve the adjacent matrix, and the release minerals enter the circulation. The osteocytes then rebuild the matrix, stimulating the deposition of mineral crystals. Osteocytes also participate in the repair of damaged bones.
|
|
|
Osteoblasts =
|
immature bone cells located on the surface of bone; produce new bone matrix in a process called osteogenesis, or ossification. Osteoblasts make and release the proteins and other organic components of the matrix. Before calcium salts are deposited, this organic matrix is called osteoid. Osteocytes develop from osteoblasts that have become completely surrounded by bone matrix and trapped within a lacuna.
|
|
|
Osteoprogenitor cells =
|
mesenchymal cells located with the periosteum and endosteum. These stem cells divide to produce daughter cells that differentiate into osteoblasts, and they are important in the formation of osteocytes.
|
|
|
Osteoclasts =
|
bone digesting cells that remove and recycle bone matrix. These are giant cells with 50 or more nuclei. Osteoclasts are not related to osteoprogenitor cells or their descendants. Instead, they are derived from the same stem cells that produce phagocytic white blood cells, called monocytes. Acids and proteolytic enzymes secreted by osteoclasts dissolve the matrix and release stored minerals. This process, called osteolysis, or resorption, is important in bone remodeling.
|
|
|
Chemical composition of bone:
|
1. Organic Osteoid
2. Inorganic Hydroxyapatites |
|
|
Organic Osteoid =
|
roughly 1/3 of the weight of bone is contributed by collagen fibers. Collagen fibers are strong and flexible, but if they are compressed, they bend.
|
|
|
Inorganic Hydroxyapatites =
|
mineral salts account for almost 2/3 of the weight of bone. Calcium phosphate interacts with calcium hydroxide to form crystals of hydroxyapatite. As they form, these crystals incorporate other calcium salts, such as calcium carbonate, and ions such as sodium, magnesium, and fluoride. By combining the hydroxyapatite with the collagen fibers, a strong, somewhat flexible, material is produced. Furthermore, this protein-crystal combination is highly resistant to shattering. In fact, bone is far superior to concrete and is more in par with steel-reinforced concrete.
|
|
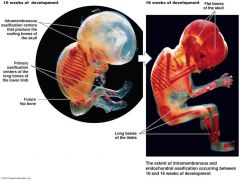
The formation of bone
|
osteogenesis or ossification, begins in the embryo around the 8th week of gestation.
|
|
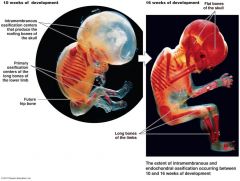
Two types of osteogenesis occur in the embryo:
|
1. Endochondral Ossification
2. Intramembranous Ossification |
|

Endochondral Ossification
|
Formation of most bones using a hyaline cartilage model.
|
|

Endochondral Ossification
|
Hyaline cartilage does not turn into bone instead it is broken down as ossification occurs.
|
|

Steps of endochondral ossification:
|
i. Cavitation of hyaline shaft
ii. Invasion of internal cavities iii. Formation of the Medullary cavity iv. Formation of epiphyses |
|

Cavitation of hyaline shaft:
|
Chondrocytes within the shaft hypertrophy (enlarge) and the surrounding matrix begins to calcify.
|
|

Cavitation of hyaline shaft:
|
The impermeable matrix causes chondrocytes to die from lack of nutrients leaving the matrix that starts to deteriorate (cavitate).
|
|

Cavitation of hyaline shaft:
|
Blood vessels grow around the edges of the cartilage.
|
|

Cavitation of hyaline shaft:
|
The cells of the perichondrium convert to osteoblasts producing a superficial layer of bone sometimes called the bony collar.
|
|

Invasion of internal cavities:
|
Blood vessels penetrate the cartilage and invade the central region. This area within the shaft of hyaline cartilage is called the primary ossification center.
|
|

Invasion of internal cavities:
|
Migrating with the blood vessels are fibroblasts (which differentiate into osteoblasts), lymph vessels, nerve fibers, red marrow elements. Collectively, these are called the periosteal bud.
|
|

Invasion of internal cavities:
|
The osteoblasts secrete osteoid around remaining fragments of hyaline, forming trabeculae, or spongy bone.
|
|

Formation of the Medullary cavity:
|
As the primary ossification center enlarges, osteoclasts break down newly formed spongy bone and opens up a medullary cavity in the center of the diaphysis.
|
|

Formation of the Medullary cavity:
|
The osseous tissue of the outer shaft becomes thicker forming compact bone.
|
|

Formation of epiphyses:
|
Secondary ossification centers appear in the area at the opposite ends of the bone. The cartilage in the epiphyses calcifies and deteriorates, forming cavities that allow entry of a periosteal bud.
|
|

Formation of epiphyses:
|
Soon the epiphyses are filled with spongy bone. The spongy bone is NOT broken down during the remodeling process.
|
|

Intramembranous Ossification
|
Formation of bones without a cartilage model. Typical in flat bones, mandible, clavicles, and patella.
|
|

Intramembranous Ossification
|
Mesenchyme cells differentiate into osteoblasts within fibrous connective tissues. This type of ossification normally occurs in the deeper layers of the dermis or in the connective tissues of tendons.
|
|

Steps of intramembranous ossification:
|
i. Formation of bone matrix within fibrous membrane
ii. Formation of woven bone and periosteum iii. Formation of compact bone plate |
|

Formation of bone matrix within fibrous membrane:
|
Mesenchymal cells cluster and secrete organic components of the matrix. The location of this activity is the ossification center.
|
|

Formation of bone matrix within fibrous membrane:
|
The resulting osteoid mineralizes and the mesenchymal cells differentiate into osteoblasts.
|
|

Formation of bone matrix within fibrous membrane:
|
As ossification proceeds, the osteoblasts get trapped within lacunae and differentiate into osteocytes.
|
|

Formation of woven bone and periosteum:
|
Osteoid accumulates, fuses together forming struts called trabeculae, or spicules, around blood vessels.
|
|

Formation of woven bone and periosteum:
|
The overall structure is similar to spongy bone.
|
|
Formation of compact bone plate:
|
Initially, the intramembranous bone consists of spongy bone only.
|
|
Formation of compact bone plate:
|
Subsequent remodeling around trapped blood vessels can produce osteons typical of compact bone.
|
|
Formation of compact bone plate:
|
As the rate of growth slows at the surface, the connective tissue around the bone becomes organized into the fibrous layer of the periosteum.
|
|
The growth of bone occurs by two primary processes:
|
1. Longitudinal Growth (length)
2. Appositional Growth (width) |
|

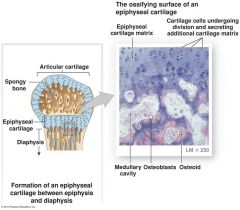
Longitudinal Growth (length)
|
Hyaline cartilage cells form tall columns at the epiphyseal plate (or growth plate) and within the articular cartilage.
|
|
Longitudinal Growth (length)
|
The cells at the top of the stack divide quickly, increasing the thickness of the epiphyseal plates and causing the entire long bone to lengthen.
|
|
Longitudinal Growth (length)
|
Older chondrocytes closer to the shaft enlarge, die, and the surrounding cartilage matrix deteriorates.
|
|

Longitudinal Growth (length)
|
The deterioration leaves spicules of calcified cartilage.
|
|

Longitudinal Growth (length)
|
Osteoblasts in the medullary cavity then ossify the cartilage spicules, forming spongy bone.
|
|

Longitudinal Growth (length)
|
The hyaline cartilage at the epiphyseal plate is eventually replaced entirely by bone. Once completely replaced with bone, the epiphyseal plate is now called the epiphyseal line. This typically occurs in the person’s early twenties and as a result the person stops growing in height.
|
|

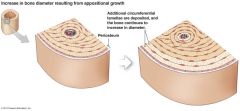
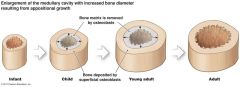
Appositional Growth (width)
|
Osteoprogenitor cells beneath the periosteum differentiate into osteoblasts and form new osteons on the external bone surface.
|
|

Appositional Growth (width)
|
While bone is being added to the outer surface through appositional growth, osteoclasts are removing and recycling lamellae at the inner surface. As a result, the medullary cavity gradually enlarges as the bone increases in diameter.
|
|

Appositional Growth (width)
|
Appositional growth is important in increasing the diameter of existing bones but it does not form the original bone.
|
|
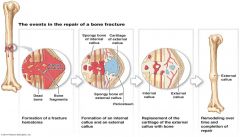
Repair of broken bones:
|
1. Hematoma formation
2. Fibrocartilage callus formation 3. Bony callus formation |
|
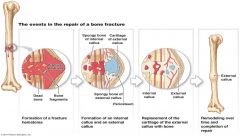
Hematoma formation
|
Blood vessels in bone tear and hemorrhage occurs.
|
|
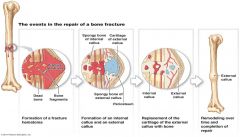
Hematoma formation
|
Over a period of several hours, a large blood clot, or _______________ , develops.
|
|
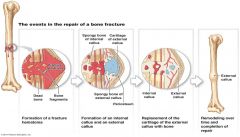
Fibrocartilage callus formation
|
Capillaries grow into the hematoma and phagocytic cells invade the area.
|
|
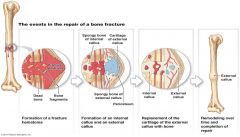
Fibrocartilage callus formation
|
Fibroblasts and osteoblasts migrate to the fracture.
|
|
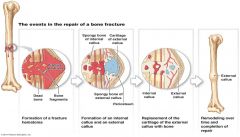
Fibrocartilage callus formation
|
Fibroblasts secrete collagen fibers and/or differentiate into chondroblasts that secrete a cartilage matrix.
|
|
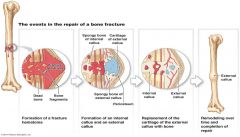
Fibrocartilage callus formation
|
Osteoblasts form spongy bone.
|
|
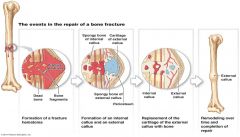
Fibrocartilage callus formation
|
The mass of repair tissue is referred to as a
|
|
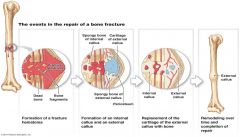
Fibrocartilage callus formation
|
An internal callus connects bone ends and an external callus protrudes from the outer bone surface.
|
|
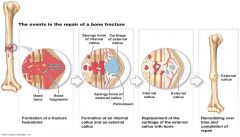
Bony callus formation
|
Osteoblasts and osteoclasts continue to migrate inward and multiply rapidly in the fibrocartilaginous callus.
|
|
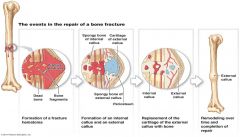
Bony callus formation
|
As the material calcifies, the tissue becomes a
|
|
remodeling.
|
Bone is constantly undergoing deposition and resorption in a process known as
|
|
|
Coordinated activity by osteoblasts and osteoclasts regulates both processes.
|
a. Bone deposition
b. Bone reabsorption |
|

Bone deposition
|
occurs where bone is injured or added bone strength is needed and is accomplished by osteoblasts. Bands of new matrix deposited in the area are referred to as an osteoid seam.
|
|
Bone reabsorption
|
is accomplished by osteoclasts. Osteoclasts secrete lysosomal enzymes that digest the organic matrix and then secrete metabolic acids that convert calcium salts into soluble forms.
|
|
|
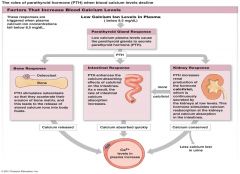
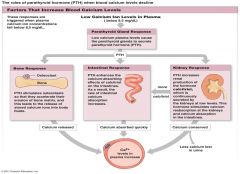
Remodeling is under negative feedback hormonal control.
|
Changes in the levels of blood calcium will trigger the release of either parathyroid hormone (PTH) or calcitonin.
|
|
|
Remodeling is under negative feedback hormonal control.
|
When blood calcium levels are too low: the parathyroid gland secretes parathyroid hormone, or PTH.
|
|
PTH has three effects all leading to a drop in blood calcium levels:
|
i. Bone response
ii. Intestinal response iii. Kidney response |
|
|
Bone response =
|
stimulates osteoclasts so they accelerate the erosion of bone matrix which leads to the release of stored calcium ions into the blood.
|
|
|
Intestinal response =
|
PTH enhances the calcium-absorbing effects of calcitriol on the intestine. As a result the rate of intestinal calcium absorption increases.
|
|
|
Kidney response =
|
PTH increases the production of the hormone calcitriol, which is continuously secreted by the kidneys at low levels. This hormone in turn stimulates calcium reabsorption at the kidney tubules.
|
|
|
When blood calcium levels are too high:
|
the C cells of the thyroid gland secrete calcitonin.
|
|
|
Calcitonin has three effects all leading to a drop in blood calcium levels:
Bone response = |
calcitonin inhibits osteoclasts but does not affect osteoblasts so that they continue to deposit calcium ions into the matrix of bone.
|
|
|
Calcitonin has three effects all leading to a drop in blood calcium levels:
Intestinal response = |
calcitonin decreases the rate of calcium absorption from foods in the digestive tract.
|
|
|
Calcitonin has three effects all leading to a drop in blood calcium levels:
Kidney response = |
calcitonin inhibits the absorption of calcium in urine so that more calcium is excreted from the body.
|
|
|
the skeleton
|
By providing a calcium reserve, ___________plays the primary role in the homeostatic maintenance of normal calcium ion concentration of body fluids.
|
|
|
the skeleton
|
is also important in the homeostatic balance of other ions as well.
|
|
|
Bone Disorders
|
Abnormalities of bone growth and development:
1. Pituitary growth failure 2. Achondroplasia 3. Marfan syndrome 4. Gigantism 5. Acromegaly 6. Fibrodysplasia ossificans progressiva (FOP) |
|
Pituitary growth failure =
|
or dwarfism, results from inadequate production of growth hormone which leads to reduced epiphyseal cartilage activity and abnormally short bones. Rare in the United States because children can be treated with synthetic growth hormone.
|
|
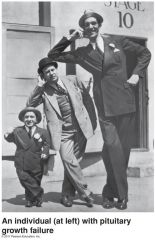
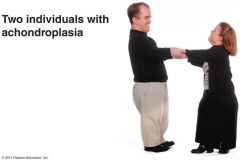
Achondroplasia =
|
results from abnormal hyaline cartilage development. Because hyaline cartilage forms the model for long bone formation, the individual will have short, stocky limbs but the torso and head are of normal size.
|
|

Marfan syndrome =
|
very tall with long, slender limbs due to excessive cartilage formation at the epiphyseal plates. Other defects in the structure of connective tissues commonly cause life-threatening cardiovascular problems.
|
|
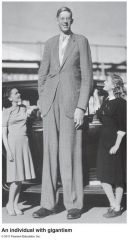
Gigantism =
|
results from an overproduction of growth hormone before puberty. Puberty is often delayed. The most common cause is a pituitary tumor which may be treated by surgery, radiation, or drugs that suppress the release of growth hormone.
|
|
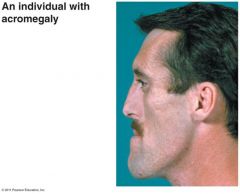
Acromegaly =
|
result from too much growth hormone after the epiphyseal plates close so that the bones do not grow longer but instead get thicker (especially the bones of the face, hands, and jaw). This leads to changes in their physical appearance.
|
|
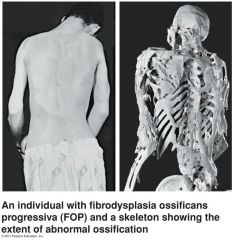
Fibrodysplasia ossificans progressiva (FOP) =
|
a rare gene mutation that causes the deposition of bone around skeletal muscles and the normally soft tissues of the body. There is not effective treatment for this painful and debilitating condition, and patients seldom survive into their 40’s.
|
|
A fracture
|
is a crack or a break in a bone.
|
|
Fractures are classified on the basis of:
|
a. Whether the bone penetrates the skin.
b. Orientation of the break. c. Position of the bone ends after the fracture. |
|

Whether the bone penetrates the skin.
Simple (closed) = |
bone breaks cleanly, but does not penetrate the skin.
|
|
Whether the bone penetrates the skin.
Compound (open) = |
broken ends of bone protrude through the tissue and skin.
|
|
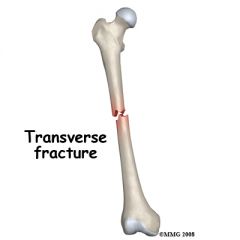
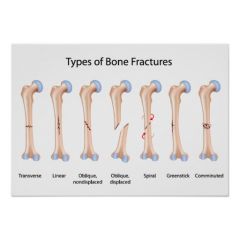
Orientation of the break.
Transverse= |
break occurs perpendicular to the long axis of a bone.
|
|
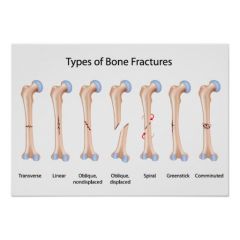
Orientation of the break.
Linear= |
breaks parallel to the long axis of the bone.
|
|
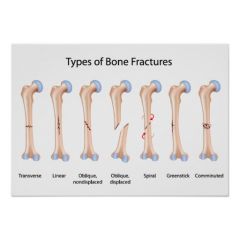
Position of the bone ends after the fracture.
Non-displaced= |
the bone ends retain their position.
|
|
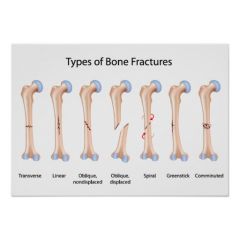
Position of the bone ends after the fracture.
Displaced= |
the bone end are out of normal alignment.
|
|
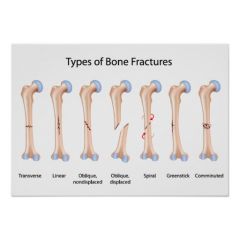
Types of Fractures:
Comminuted = |
bone fragments into many pieces.
|
|
|
Types of Fractures
Compression = |
bone is crushed from upward and downward forces
|
|
|
Types of Fractures
Depressed = |
broken bone is pressed inward (skull)
|
|
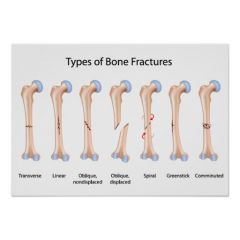
Types of Fractures
Spiral = |
raged break as a result of excessive twisting of the bone.
|
|
Types of Fractures
Epiphyseal = |
break occurring along the epiphyseal plate
|
|
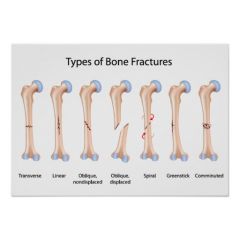
Types of Fractures
Greenstick = |
bone breaks incompletely
|
|

Types of Fractures
Colle’s = |
distal part of the radius breaks
|
|
|
Perichondrium:
|
A dense membrane that is composed of fibrous connective tissue that closely wraps all cartilage except the cartilage in joints, which is covered by a synovial membrane.
|
|

Types of Fractures
Pott’s = |
malleolus of tibia and fibula break
|

