![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
361 Cards in this Set
- Front
- Back
|
Normal Gass Exchange Unit in the Lung.
Hypoxemic or Hypercapnic |
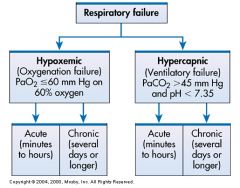
What is this image reprensenting? Respiratory Failure can be classified as _____________ or _____________
|
|
|
PaO2 is less than or equal to 60mm HG on 60% oxygen
PaCo2 is greater than 45mm HG and pH is less than normal 7.35 which makes is acidic pH. |
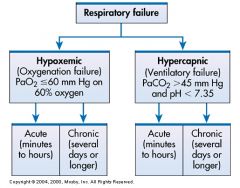
Memorize this and know that in Respiratory Failure with Oxygenation Failure you have ________________________ and with Ventilatory Failure you have _____________________________
|
|
|
3.3
1.0 0.63 Higher Lower Opposite |
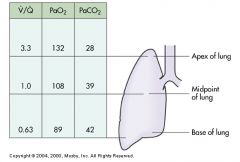
Regional V/Q differences in the normal lung. At the lung apex, the V/Q ratio is _____ at the midpoint ____, and at the base _____. This difference causes the PaO2 to be ____________ at the apex of the lung and _________ at the base. Values for PaCo2 are the __________. Blood that exits the lung is a mixture of these values
|
|
|
Major function of the respiratory system is ________________
|
Gas Exchange
|
|
|
Gas exchange involves the transfer of O2 and CO2 between the _________ and __________
|
Atmosphere
Blood |
|
|
Results when one or both of these gas exchanging functions are inadequate (O2 or Co2)
|
Respiratory Failure
|
|
|
Clinical states that interfere with adequate O2 transfer result in ____________
|
Hypoxemia
|
|
|
Hypoxemia is manefested by a/an ___________ in arterial O2 tension (PaO2) and a/an _________ in arterial O2 saturation
|
decrease
decrease |
|
|
Insufficient removal of CO2 results in
|
hypercapnia
|
|
|
Hypercapnia is manifested by an ___________ in Arterial Co2 tension PaCO2
|
Increase
|
|
|
Respiratory Failure can be classified as __________ or __________-
|
Hypoxemic
Hypercapnic |
|
|
Hypoxemic respiratory failure is also reffered to as _______________ becasue the primary problem is inadequate O2 transfer between the alveoli and the pulmonary capilliary bed
|
oxygenation failure
|
|
|
Hypoxemic Respiratory Failure is commonly definned as a PaO2 of _____ or less when the patient is receiving an inspired O2 concentration of _____% or greater
|
60mmHg 60% also known as the 60/60 club
|
|
|
The PaO2 of 60mmHg is at a level that indicates
|
inadequate O2 saturation of hemoglobin
|
|
|
the PaO2 level exists despite administration of supplemental O2 at a percentage _____% that is about three times that in room air (____%)
|
60%
21% |
|
|
Disorders that interfere with O2 transfer into the blood are:
|
pneumonia
pulmonary edema pulmonary embolism alveolar injury related to inhalation of toxic gases (smoke) Inaddition low cardiac output states congestive heart failure shock anatomical shunt |
|
|
Hypercapnic respiratory failure is also referred to as ______________. Its primary problem is insufficient _______ _________
|
ventilatory failure
Co2 removal |
|
|
Hypercapnic Respiratory Failure is commonly defined as a PaCo2 __________ in combination with acidemia _________
|
above normal greater than 45
a pH less than 7.35 |
|
|
Three important concepts to remember about Hypercapnic Respiratory Failure:
1. 2. 3. |
1. the Paco2 is higher than normal
2. there is evidence of the body's inability to compensate for this increase (Acidemia) 3. the pH is at a level where a further decrease may lead to severe acid base imbalance |
|
|
Disorders that compromise lung ventilation and subsequent Co2 removal include:
|
drug overdoses with CNS depressants
neuromuscular diseases (myasthenia gravis) trauma or diseases involving the spinal cord and its role in lung ventilation |
|
|
Hypoxemic Respiratory Failure Common Causes for the Respiratory System
1. 2. 3. 4. 5. |
1. ARDS
2. Pneumonia 3. Toxic Inhalation Smoke 4. Hepatopulmonary Syndrome 5. Massive Pulmonary Embolism |
|
|
Hypoemic Respiratory Failure common causes for the cardia system:
1. 2. 3. |
1. Anatomic Shunt (ventricular septal defect)
2. Cardiogenic Pulmonary Edema 3. Shock (decreaseing blood flow through pulmonary vasculature) |
|
|
Hypercapnic Respiratory Failure common causes related to the Respiratory System:
1. 2. 3. |
1.Asthma
2.COPD 3.Cystic Fibrosis |
|
|
Hypercapnic Respiratory Failure Common Causes related to the CNS
1. 2. 3. 4. |
1. Brainstem Infarction
2. Sedative and Narcotic Overdose 3. Spinal Cord Inury 4. Severe Head Injury |
|
|
Hypercapnic Respiratory Failure Common Causes related to the Chest Wall:
1. 2. 3. 4. |
1. Thoracic Trauma Flail Chest
2. Kyphocoliosis 3. Pain 4. Massive Obesity |
|
|
Hypercapnic Respiratory Failure Common Causes related to the Neuromuscular System:
10 of them |
1. myasthenia gravis, 2. critical illness polyneuropathy, 3. Acute myopathy, 4. Toxic ingestion 5. Amyotrophic lateral sclerosis 6. Phrenic nerve injury 7. Guillain-Barre syndromw, 8. Poliomyelitis 9. Muscular dystrophy 10. Multiple Sclerosis
|
|
|
Four physiologic mechanisms may cause hypoxemic and subsequent hypoxemic respiratory failure:
1. 2. 3. 4. |
1. V/Q Mismatch
2. Shunt 3. diffusion limitation 4. Hypoventalation |
|
|
The most common causes of Hypoxemic Respiratory failure are:
1: 2: |
V/Q mismatch and shunt
|
|
|
Amount of blood perfusing the lungs each minute is
|
4-5 liters
|
|
|
Amount of fresh gas that reaches the alveoli each minute
|
4-5 liters
|
|
|
At the lung _______ V/Q ratios are greater than 1: more ventilation than perfusion
|
apex
|
|
|
At the lung _______ V/Q ratios are less than 1: less ventilation than perfusion
|
base
|
|
|
Many diseases and conditions alter overall V/Q matching and thus cause a V/Q mismatch. The most common are those in which increased secretions are present in the airways such as
|
COPD
|
|
|
Many diseases and conditions alter overall V/Q matching and thus cause a V/Q mismatch. The most common are those alveoli:
|
pneumonia
|
|
|
Many diseases and conditions alter overall V/Q matching and thus cause a V/Q mismatch. The most common are those in bronchospasm is present
|
asthma
|
|
|
V/Q mismatch may also result from alveolar collapse _______ or as a result from ____
|
atelectasis
Pain |
|
|
Unrelieved or inadequately relieved pain interferes with chest and _________________ compromising ____________
|
abdominal wall movement
lung ventilation |
|
|
Pain increases ______ and _____ tension, producing generalized muscle rigidity, causes _________ __________and activation of the stress response; and _______ O2 consumption and Co2 Production
|
muscle
motor systemic vasoconstriction increases |
|
|
What affects the perfusion portion of the V/Q relationship by limiting blood flow and not having an effect on airflow to the alveoli.
|
Pulmonary embulous
|
|
|
What affects the the airflow to the alveoli but have not affect on the blood flow to the gas exchange
|
Unrelieved or inadequate Pain control
|
|
|
What is the first step to reverse hypoxemia caused by a V/Q mismatch becasue not all gas exchange units are effected
|
Oxygen Therapy
|
|
|
Explain how Oxygen Therapy works as the first line treatment in hypoxemia?
|
O2 increases the PaO2 in the blood leaving normal gas exchange units causing a higher than normal PaO2.
|
|
|
What happens to the well oxygenated blood when it mixes with poorly oxygenated blood?
|
It raises the over all PaO2 of blood leaving the lungs.
|
|
|
The optimal approach to hypoxemia caused by a V/Q mismatch is one directed at the _______
|
Cause
|
|
|
A shunt occurs when ________________________
|
blood exists the heart without having participated in gas exchange
|
|
|
A __________ is viewed as an extreme V/Q Mismatch
|
Shunt
|
|
|
There are two types of shunts:
1. 2. |
1. Anatomic
2. Intrapulmonary |
|
|
An anatomical shunt occurs when:
|
blood passes through an anatomic channel in the heart and there for does not pass throught the lungs
|
|
|
An intrapulmonary Shunt occurs when:
|
blood flows through the pulmonary capilliaries without participating in gas exchange
|
|
|
Intrapulmonary Shunts are seen in conditions in which the alveoli fill with fluid as seen in these diseases:
1. 2. 3. |
ARDS
Pneumonia Pulmonary Edema |
|
|
If hypoxemia is due to a shunt, what is ineffective in increaseing PaO2
|
Oxygen therapy
|
|
|
Why would oxygen be ineffect for an anatomic shunt?
|
Becasue blood passes from the right to the leftside of the heart without passing through the lungs
|
|
|
Why would oxygen be ineffective for an intrapulmonary shunt?
|
because the alveoli are filled with fluid, which prevents gas exchange
|
|
|
What is an example of an anatomic shunt
|
(A Ventricular septal Defect)
|
|
|
Patients with shunt are usually more ___________ than patients with V/Q mismatch
|
hypoxemic
|
|
|
Patients with Shunts may require:
1. 2. to improve gas exchange |
1. Mechanical Ventilation
2. FIO2 (high fraction of inspired oxygen |
|
|
Diffusion limitation occurs when gas exchange across the alveolar-capillary membrane is :
|
compromised by a process that thickens or destroys the membrane
|
|
|
Diffusion limitation can also be worsend by conditions that affect the pulmonary vascular bed such as severe ____________ or recurrant ______________.
|
emphysema
pulmonary embuli |
|
|
Some disease cause the alveolar capilliary machine to become thicker (fibrotic) which would slow gas transport. Such disease are:
1. 2. 3. |
1. pulmonary fibrosis
2. interstitial lung disease 3. ARDS |
|
|
Diffusion limitation is more likely to occure during _________ than at ________
|
excercise
rest |
|
|
During excercise blood moves more rapidly through the lungs. Because transit time is increased, red blood cells are in the lings for a shorter time, decreasing the time for _________________ across the alveolar-capilliary membrane.
|
diffusion of O2
|
|
|
Classical sign of diffusion limitation is:
|
hypoxemia that is present during excercise and not during rest
|
|
|
ALveolar hypoventilation is a generalized decrease in __________ that results in an increase in the ________
|
ventilation
PaCo2 |
|
|
Alveolar hypoventilation may be the result of:
1. 2. 3. 4. |
restrictive lung disease
CNS disease Chest Wall Dysfunction Neuromuscular Disease |
|
|
Alveolar Hypoventilation is primarliy a mechanism of ______________respiratory failure it can also cause __________
|
hypercapnic
hypoxemia |
|
|
What are the four ways hypoxemic respiratory failure can occur:
1. 2. 3. 4. |
V/Q mismatch
Shunt Diffusion Limitation Hypoventilation |
|
|
A patient with acute respiratory failure scondary to pneumonia may have a combination of V/Q mismatch and shunt becasue inflammation, edema, and hypersecretions of exudate within the bronchioles and terminal respiratory units:
1. 2. |
1. obstruct the airways V/Q
2, Fill the alveoli with exudate Shunt |
|
|
Shunt may occur becasue of
|
improper positioning
|
|
|
if you had a patient with an affect lung which way should you position the affect lung
|
the affected lung should always be up allowing it to drain down
|
|
|
WHat causes the affected lung up to drain down?
|
Gravity
|
|
|
A shunt may be increased as with Endogenous vasodilator mediators as is the case with
|
Pneumococcal pneumonia
|
|
|
A patient may have a combination of shunt and V/Q mismatch because some alveoli are completely filled from edema (shunt) and others are partially filled with fluid (V/Q) Mismatch in these 2 situations:
1. 2. |
Cardiogenic Pulmonary Edema
ARDS |
|
|
Hypercapnic respiratoyr failure results from an imbalance between ____________ and ___________
|
ventilatory supply
ventilatory demand |
|
|
Ventilatory supply is:_____________________that the patient can sustain without developing respiratory muscle fatigue
|
the maximum ventilation (gas flow in and out of the lungs)
|
|
|
Ventilatory Demand is:
|
the amount of ventilation needed to keep the PaCO2 with in normal limits
|
|
|
Why can normal individuals can engage in strenous excercise, which greatly increases CO2 production without an elevation in PaCo2
|
becasue the ventilatory supply far exceeds the ventilatory demand
|
|
|
Patients with lung disease can not effectivly increase lung ventilation in response to excercise or metabolic needs. Name an example of the lung disease that this would be
|
emphysema
|
|
|
What is typically present before ventilatory demand exceeds ventilatory supply
|
considerable dysfunction of the lung
|
|
|
When Ventilatory demand does exceed ventilatiry supply, the PaCo2 can no longer be sustained within normal limits and __________ occurs
|
hypercapnia
|
|
|
Hypercapnia reflects sustained
|
lung dysfunction
|
|
|
Hypercapnic respiratory Failure is sometimes called
|
ventilatory failure
|
|
|
Ventilatory failure's primary problem is the inability of the respiratory system to: _______________ to maintain a normal PaCo2
|
ventilate out CO2
|
|
|
Many different diseases can cause a limitation in ventilatory supply. Name the four categories:
1. 2. 3. 4. |
1. airways and alveoli
2. Abnormalities of CNS 3. Abnormalities of the Chest Wall 4. Neuromuscular Conditions |
|
|
Patients with asthma, emphysemia, chronic bronchitis and cystic fibrosis are at high risk for hypercapnic respiratory failure becasue the underlying pathophysiology of these condition result from:
|
airflow obstruction and air trapping
|
|
|
What is a common example of a problem that my suppress the drive of the CNS to breathe?
|
an overdose of a narcotic or respiratory depressant drug
|
|
|
A ____________ or ___________- may also interfere with the normal function of the respiratory center because the __________ does not alter the respiratory rate in response to a change in PaCo2
|
brainstem infarction
severe head inury Medulla |
|
|
the respiratory center is located in the
|
medulla
|
|
|
CNS dysfunction may also include ________________ that limit innervation to the respiratory muscles
|
spinal cord injury
|
|
|
In patients with a flain chest __________ prevent the rib cage from expanding normally becasue of
1. 2. 3. |
FRACTURES
pain mechanical restriction muscle spasm |
|
|
In patients with Kyphoscoliosis the change in _____________ compresses the lungs and prevents normal expansion of the chest wall.
|
spinal configuration
|
|
|
In patients with massive obesity the weight of the chest and abdominal contents may:
|
limit lung expansion
|
|
|
Patients with chest wall conditions are at risk for respiratory failure becasue
1. limits 2. limits 3. limits |
limits lung expansion
limits diaphramatic movement limits gas exchange |
|
|
Certian diseases make patients at risk for respiratory failure becasue it may result in muscle weakness or paralysis. Patients with such risks are those with
1. 2. 3. Therefore unable to maintain a normal PaCo2 |
Guillian Barre Syndrome
Muscular Dystrophy Multiple Sclerosis |
|
|
Bottom line is that respiratory may occur because the medulla, chest wall, peripheral nerves, or respiratory muscles are not functioning normally. Patient may have no damage to tissue but may be unable to :
|
inspire a tidal volume sufficient to expel CO2 from the lungs
|
|
|
What determines the definition of respiratory failure
|
Paco2 and the PaCo2
|
|
|
What is the major threat of respiratory failure
|
the inability of the lungs to meet the oxygen demands of the tissues
|
|
|
What determines Tissue O2 delivery?
1. 2. |
the amount of O2 carried by the Hemoglobulin, and the Cardiac output
|
|
|
The inability of the lungs to meet the oxygen demands of the tissues may occur as a result of:
1. 2. 3. 4. |
1. inadequate tissue O2 delivery
2. Tissues unable to use the O2 3. Stress response 4. Increase in tissue O2 consumption |
|
|
Respiratory failure places the patient at greater risk if there are coexisting:
1. 2. |
cardiac problems
anemia |
|
|
Failure of O2 utilization most commonly occurs as a result of
|
septic shock
|
|
|
Adequate O2 may be delivered to the tissues, but an abnormally high amount of O2 returns in the venous blood, indicating that it is not being extracted and used at the tissue level. This is what we would classify as
|
septic shock
|
|
|
A sudden decrease in PaO2 or a rapid increase in PaCo2 implies a serious condition and may be considered a life-threatning emergancy. A clinical example of this would be a patient with ________ who develops severe ________ and a marked decrease in __________ resulting in respiratory arrest
|
asthma
bronchospasm airflow |
|
|
A more gradual change in PaO2 and PaCo2 is better tolerated because compensation can occur. An example of of this would be a patient with COPD who develops a progressive in PaCo2 over several days following the onset of a
|
respiratory infection
|
|
|
Becasue the respiratory infection happened over a couple of days there was time for renal compensation (retention of bicarbonate) which will minimize the change in _______ compensating from ________
|
arterial pH
respiratory acidosis |
|
|
Manifestations of respiratory failure are related to the extent of change :
1. 2. 3. |
1. Pao2 or Paco2
2. Rapidity of change acute vs chronic 3. ability to compensate for this change |
|
|
When the patients compensatory mechanism fails then this happens:
|
respiratory failure
|
|
|
Becasue clinical manifestations are variable it is important to monitor trends in _______ and or _________ to evaluate the extent of change
|
ABG's
Pulse Oximetry |
|
|
The initial indication of respiratory failure is a change in the patients
|
mental status
|
|
|
becasue the cerebral cortex is so sensitive to variations of oxygenation and acid-base imbalances __________changes will occurearly and frequenty before the ABG results are obtained
|
mental status
|
|
|
Restlessness, confusion, agitation, and combative behavior suggest _________ to the brain and should be fully investigated
|
inadequate O2 delivery
|
|
|
Nurse may detect manifestations of respiratory failure that are specific (arise from the __________ system) and nonspecific (arise from the _______ system)
|
respiratory
body |
|
|
___________ and __________ can also be early signs of respiratory failure
|
tachycardia
mild hypertension |
|
|
Tachycardia and hypertension may indicate an attept by the heart to _________ for the decreased O2 delivery
|
compensate
|
|
|
A severe morning _________ may indicate that hypercapnia may occured at night, increaseing cerebral blood flow by ___________ and causing a morning __________
|
headache
vasodilation headache |
|
|
Rapid shallow breaths may indicate that the _________ may be inadequate to remove CO2 from the lungs.
|
Tidal Volume
|
|
|
__________- is an unreliable indicator of hypoxemia and is a late sign of respiratory failure becasue it does not occur until hypoxemia is severe (Pao2 is less than or equal to 45 mm Hg
|
Cyanosis
|
|
|
__________ occurs when the PaO2 has fallen sufficiently to cause signs and symptoms of inadequate oxygenation
|
Hypoxia
|
|
|
If hypoxia or hypoxemia is severe the cells shift from ______ to ______ metabolism.
|
aerobic.
anaerobic |
|
|
The waste product of anaerobic metabolism is ________ which is much harder to remove from the body than CO2 because _________ has to be buffered with ________
|
lactic acid
lactic acid sodium bicarbonate |
|
|
When the body does not have adequate amounts of sodium bicarbonate to buffer the lactic acid produced by anaerobic metabolism, ___________ results and cell death may occur
|
metabolic acidosis
|
|
|
Hypoxia and metabolic acidosis have adverse effects on the body especially in the:
1. 2. |
Heart
CNS |
|
|
The heart tries to compensate for the decreased O2 level in the blood by increasing the :
1. 2. |
heart rate
cardiac output |
|
|
As the PaO2 decreases and acidosis increases, the heart muscles may become dysfunctional and _________ may decrease. In addition
1. 2. May occur |
cardic output
Angina Arrythmias |
|
|
Permanent _________- may occure due to the decrease of oxygenation
|
brain damage
|
|
|
Renal function may also be impaired such as:
1. 2. 3. 4. |
sodium retention
edema formation acute tubular necrosis and Uremia |
|
|
GI alterations include
1. 2; 3. |
1. tissue ischemia
2. increased permability of intestinal wall 3. possible translocation of bacteria from Gi into circulation |
|
|
The changes that dispose to insufficient CO2 removal in respiratory failure are:
1. 2. |
1. rapid shallow breathing pattern
2. respitory rate slower than normal |
|
|
A common position to be in that will help decrease he work of breathing becasue propping the arms increases the anterior-posterior diameter of the chest and changes pressure in the thorax
|
tripod position
|
|
|
This technique may be used in which causes an increase in SAO2 becasue it slows respirations and allows for more time for expiration and prevents the small bronchiles from collapsing thus facilitating air exchange
|
purse lip breathin
|
|
|
Another assessment parameter is the number of pillows that the patient requires to breathe comfortably when resting, this is termed
|
orthopnea
|
|
|
When a patient is experiencing dyspnea a patient my speak with out pausing. This is an indication of the severity. Patient is speaking in sentences ___________ distress
Patient is speaking words _____ distress, Patient is speaking in phrases ______ distress. |
mild or no
severe moderate |
|
|
The normal I:E ration is ____ which means the expiration is twice as long as inspiration
|
1:2
|
|
|
With patients in respiratory distress the ratio may increase to ________--
|
1:3-1:4
|
|
|
The change of I:Es signifies _________ and that more time is required to empty the lungs
|
aifflow obstruction
|
|
|
The nurse may observe _________ (inward movement) of the intercostal spaces or the supraclavicular area and use of the accessory muscles during inspiration and exhalation
|
retraction
|
|
|
use of the accessory muscles signfies _________ distress
|
moderate
|
|
|
paradoxal breathing signifies _________- distress
|
severe
|
|
|
During Paradoxal breathing the abdomen and chest move in the opposite manner- _________- during exhalation and _________ during inhalation
|
outward
inward |
|
|
Normal breathing the thorax and abdomen move ________ on inspiration and _________ exhalation
|
outward
inward |
|
|
This results from maximal use of repiratlory muscles in respiration
|
paradoxal breathing
|
|
|
_________ and _________ may indicate pulmonary edema or emphysema
|
crackles or Rhonchi
|
|
|
absent or diminished breath sounds may indicate
1. 2. |
atelaectasis
pneumonia |
|
|
Crackles and Rhonchi may indicate :
1. 2. |
pulmonary edema
emphysema |
|
|
The presence of bronchial breath sounds over the lung periphery often results from lung consolidation that is seen with _________---
|
pneumonia
|
|
|
a __________ may also be heard in the presence of pneumonia that has involved the pleura
|
pleural friction rub
|
|
|
Patients with end stage severe chronic lung disease may have low PaO2 values or elevated PaCo2 levels and _________- in their normal baseline
|
crackles
|
|
|
It is especially important to monitor specific and nonspecific changes in patients with ______ becasue a small change can cause significant decompensation
|
COPD
|
|
|
Any deterioration in mental status such as agitation, combative behavior, confusion, or decreased level of consciousness must be reported immediately because the change may indicate a rapid deterioration in clinical status and the need for _______-
|
Mechanical ventilation
|
|
|
After physical assessment the most common diagnostic study used to determine respiratory failure is __________-
|
ABG Analysis
|
|
|
AN _______________ may be inserted into a peripheral artery for monitoring systemic blood pressure and obtaining blood for ABGS
|
indwelling cathether
|
|
|
__________ frequently used for monitoring oxygenation status, but tells little regarding lung ventilation
|
pulse oximetry
|
|
|
Diagnostic studies that may be done include:
1. 2. 3. 4. 5. |
Chest X-Ray
CBC Serum Eletrolytes Urinalysis ECG |
|
|
This may be used to assess tube placement within the trachea immediately following intubation:
|
End tidal Co2 EtCO2
|
|
|
EtCO2 may also be used during ventilator management to assess trends in ________ as determined by expired CO2
|
lung ventilation
|
|
|
In severe respiratory failure a pulmonary artery cathether may be inserted to measure
1. 2. 3. This information is helpfull at determining the adequacy of tissue perfusion and the patients response to treatment |
heart pressures
cardiac output mixed venous oxygenation saturation |
|
|
Pulmonary artery, pulmonary artery wedge, and left atrial pressures are monitored to determine whether the accumulation of fluid within the lungs is a result or _________ or _______ problems
|
cardiac
pulmonary |
|
|
The overal goals for a patient with respiatory failure is :
1. 2. 3. 4. |
1. ABG Valueswithin the patients baseline
2, breath sounds wth in patients baseline 3, no dyspnea or breathing sounds wiithin the patients baseline 4. effective cough and ability to clear secretions |
|
|
The most important plan of care for any patient who might be At Risk for respiratory failure is to:
1, 2, |
1, prevention
2,early recognition |
|
|
Prevention involves
1. 2. 3. |
1. Throughal Physical assessment
2. Health History to identify risk factors 3. initation of interventions 3. |
|
|
Patient at risk with respiratory failure should receive appropriate patient teaching regarding:
1. 2, 3. 4. |
1. coughing
2, deep breathing 3. incentive spirometry 4. ambulation |
|
|
What can decrease the risk of respiratory failure in the acutely or critically ill patient?
1. 2. 3. 4. |
1. Education of PREVENTION OF ATELECTASIS
2. education of prevention of pneumonia 3. Education on Optimizing hydration and nutrition |
|
|
The majory goals for acute respiratory failure include
1. 2. |
1. maintaing adequate o2
2. maintaing adequate ventilation |
|
|
Interventions usedin respiratory therapy are
1. 2. 3. |
O2 therapy
mobilization of secretions positive pressure ventilation |
|
|
Primary goal of oxygen therepy is to
|
correct hypoxemia
|
|
|
Hypoxemia is secondary to V/Q mismatch what will you do?
|
supplemental O2 administered 1-3 L min by nasal canula or by 24% to 32% SIMPLE FACE MASK or venturi mask
|
|
|
Hypoxemia secondary to an intrapulmonary shunt is usually not responsive to high O2 concentrations and the patient will usually require ___________--
|
PPV Positive Pressure Ventilation
|
|
|
PPV offers a means of :
1. 2. 3. |
1. Proving O2 and Humidification
2. Decreases work of breathing 3. Reduces respiratory fatigue |
|
|
Positive pressure may assist in ________________and and decreasing the shunt
|
opening collapsed airways
|
|
|
How is PPV provided?
1. 2. |
1. Endotracheal Tube Most common
2. noninvasive tight fitting mask |
|
|
Type of O2 delivery system chosen for the patient in acute respiratory failure should be 1. tolerated by the patient because :
_____________________ and 2. Maintain PaO2 at ________ mm Hg or more and the SaO2 at ____% or more at the lowest O2 concentration possible |
anxiety caused by feelings of claustroophobia related to the face mask or dyspnea may prompt the patient to remove the mask
2. 55-60, 90% |
|
|
High O2 concentration replaces the nitrogen gas normally present in the alveoli causing instability and ________--
|
atelectasis
|
|
|
In intubated patients, exposure to 60% or greater O2 for longer than 48 hours poses a significant risk for O2 ________---
|
Toxicity
|
|
|
In nonintubated patients the risk is less clear, the effects of prolonged exposure to be high levels of O2 include increased pulmonary microvascular permability, decreased surfactant production, and surfactant inactivation and fibrotic changes in the _______
|
alveoli
|
|
|
Chronic Hypercapnia may blunt the response of chemoreceptors in the medulla, and condition known as _________
|
Co2 narcosis
|
|
|
In Co2 Narcosis respirations are stimulated by _________
|
hypoxia
|
|
|
Patients with chronic hypercapnia should receive O2 through a
1. 2. |
1. low flow nasal cannula at 1-2 liters/min
2. venturi mask at 24% to 28% |
|
|
______________ may cause or exacerbate acute respiratory failure by blocking movement of O2 into the alveoli and pulmonary capilliary blood and removal of Co2 during the respiratory cycle.
|
Retained Pulmonary Secretions
|
|
|
Secretions can be mobilized through:
1. 2. 3. 4. |
1. effective coughing
2. adequate hydration and humidification 3. chest physical therapy 4. tracheal suctioning |
|
|
If secretions are obstructing the airway patient should be encouraged to
|
cough
|
|
|
This type of coughing may be benefit for patients with neuromuscular weakness from disease or exhaustion may not be able to generate sufficient airway pressures to produce an effective cough
|
Augmented Breathing
|
|
|
Explain what Augmented Coughing is and how it is done:
|
performed by placing the palm of the hand on the abdominal musculature below the xiphoid process. As the patient ends a deep inspiration and begins the expiration the hand shoud be moved forcefully downward increasing abdominal pressure resulting in a forceful cough
|
|
|
What does the Augmented Coughing actually do?
|
It helps increase expiratory flow and thereby facilitate secretion clearance
|
|
|
What kind of coughing is a series of coughs while saying a specific word
|
Huff coughing stating the word Huff
|
|
|
What does Huff coughing prevent
|
It prevents the glottis from closing during the cough
|
|
|
Patients with _____ generate higher flow rates with a huff cough than is possible with a normal cough
|
COPD
|
|
|
the Huff cough is effective in clearing only the _________- airways but it may assist in moving secretions upward
|
central
|
|
|
the Staged cough helps
|
move secretions upwards
|
|
|
Explain how the staged cough is done:
|
the patient sits in a chair breathes three to four times in and out through the mouth, and coughs while bending forward and pressing a pillow inward against the diaphram
|
|
|
What will maximize the thoracic expansion, therby decreasing dyspnea and improving secretion mobilization?
1. 2. |
positioning the patient
1. elevating the head of the bed at least 45 degrees 2. reclining chair or chair bed |
|
|
A sitting position improves pulmonary function and assists in venous pooling in dependant body areas such as the
|
lower extremities
|
|
|
What kind of positioning may be used in patients with disease in one lung
|
sidelying position
lateral position |
|
|
This position termed down with the good lung, allows for ________ in the affected lung
|
Improved V/Q mismatch
|
|
|
What is optimal in dependent lung areas?
1. 2. |
pulmonary blood flow and ventilation
|
|
|
Optimal positioning would be to place the patient on their _______ to maximize ventilation and perfusion in the good lung and facilitate secretion removal from the affected lung. This is also called
|
left side
Postural drainage |
|
|
All patient must be __________ if there is any posibility that the tongue will obstruct the airway ot that aspiration may occur
|
side lying
|
|
|
An _____ or ____ airway should be kept by the bed side for use if necessary
|
oral or nasal
|
|
|
Adequate fluid intake is necessary to keep secretions thin and easy to expel. What is normal?
|
2-3 Liters per day
|
|
|
Some assessment signs for fluid overload include:
1. 2. 3. |
crackles
dyspnea increased central venous pressure |
|
|
Aerosols of sterile normal saline may be administered through a _____ which may be used to liquify secretions
|
nebulizer
|
|
|
Mucolytic agents such as nebulized __________ mixed witha bronchodilator may be used to thin secretions but as a side effect it may also cause airway :
1. 2. |
acetylcysteine Mucomyst
erythemia bronchospasm |
|
|
what procedure do we use the mucolytic agent and bronchodilator for?
|
bronchoscopy
|
|
|
Chest Physical therapy is indicated in patients who produce more than _____ml or sputum per day or have evidence of severe _______ or pulmonary iniltrates
|
30
atelaectasis |
|
|
If a patient is unable to expectorate secretions what are we suppose to do?
|
blind sunctioning
|
|
|
Which trach may be used to suction patients who have difficulty mobilizing secretions and when blind suctioning may be difficult or ineffective
|
the mini trach
|
|
|
The mini trach is a 4mm indwelling plastic cuffless cannula inserted through the __________ membrane
|
cricothyroid
|
|
|
Contraindications for the mini-trach is
1. 2. 3. |
absent gag reflex
history of aspiration need for long term mechanical respiration |
|
|
__________ may be provided invasively through an endotracheal or nasotracheal intubation or non invasively through a nasal of facial mask
|
PPV Positive pressure ventilation
|
|
|
A ________ is a mask that is placed over a patients nose or nose and mouth and the patient breathes spontaneously.
|
NIPPV: non invasive positive pressure ventilation
|
|
|
With a NIPPV it is possible to ____________ with out the need for an endotracheal intubation
|
Reduce the work of breathing
|
|
|
A form of NIPPV is called ______ in which different possitive pressure levels are set for inspiration and expiration
|
BIPAP Bilevel positive airway pressure
|
|
|
A _________ is another form of NIPPV which is a constant positive pressure that is delivered to the airway during inspiration and expiration
|
CPAP continous positive airway pressure
|
|
|
What is the most useful in managing chronic respiratory failure in patients with chest wall and neuromuscular disease
|
NIPPV
|
|
|
Certian patients may refuse mechanical vetillation by intubation but will desire NIPPV with some palliative ventilatory support for example patients who may be in
|
end stage COPD
|
|
|
NIPPV is not appropriate for the patient who has:
1. 2. 3. |
absent respirations
excessive secretions decreased level of consciouness high o2 requirements facial trauma hemodynamic instability |
|
|
The goals of drug therapy for patients with acute respiratory failure include:
1. 2. 3. 4. |
Relief of bronchospasms
reduction of airway inflammation and pulmonary congestion treatment of pulmonary infection reduction in anxiety and restlessness |
|
|
Short acting bronchodillators such as
1. 2. ar frequently administered to reduce bronchospasm using either a hand held nebulizer or meter does inhaler with spacer |
metaproterenol Alupent
albuterol Ventolin |
|
|
During an acute bronchospasm these bronchodilators can be given how ofter?
|
30-60 minute intervals untila response has occured
|
|
|
What happend is several bronchospasms occur what can be given by IV for the patient
|
aminophylline
|
|
|
Bronchodilator effects may sometimes cause a worsening of arterial ________ by redistruibuting the inspired gas to areas of decreased perfusion
|
hypoxemia
|
|
|
What will alliviate the arterial hypoxemia. What could you give with the bronchodilators
|
O2-rich gas mixture
|
|
|
What type of medication should reduce an airway inflammation
|
corticosteriods
|
|
|
What corticosteriod may be used in conjunction with a brochodilator when inflammation if present
|
solumedrol methlyprednisolone
|
|
|
WHat kind of effect does corticosteriod have on the body when it is given by IV
|
immediate onset
|
|
|
What is the therapuetic effect of inhaled corticosteriods
|
4-5 days
|
|
|
Are inhaled corticosteriods used with acute respiratory failiure?
|
No becasue it takes too long to have a therapeutic effect
|
|
|
What type of drugs reduces pulmonary congestion
|
Diuretics
|
|
|
What can occur as a consequence of direct or indirect injury to the alveolar capilliary membrane, ARDS or from right or left side heart failure and therefore can be cardiac or non cardiac in orgion
|
pulmonary interstitial fluid
|
|
|
What happens when you have pulmonary interstitial fluid in the lungs?
|
You will have a decrease in ventilation and hypoxemia
|
|
|
What type of drug is given to reduce pulmonary congestion caused by heart failure
|
IV diurectis Furosemide Lasix
|
|
|
What may also be used if heart failure or atrial fibrilliation is present to increase contractility and decrease heart rate?
|
Digitalis
|
|
|
Pulmonary infections such as
1. 2. result in excessive mucus roduction, fever, increased O2 consumption, inflammed fluid filled or collapsed alveoli |
pneumonia
acute bronchitis |
|
|
Axniety, restlessness, and agitation result from what?
|
cerebral hypoxia
|
|
|
Fear caused by the inability to breathe and a sense of loss of control may exacerbate what?
|
anxitey
|
|
|
Anxiety, pain, and agitation ________ o2 consumption which may worsen the degree of hypoxemia
|
increase
|
|
|
Anxiety , pain, and agitation _________ CO2 production affects ventilator management, and increases morbitity
|
increases
|
|
|
Certian benzodiazepines may be used to decrease anxiety, agitation and pain.
1. 2. |
Ativan
Versed |
|
|
Some narcotics are used to reduce anxiety, agitation, and pain.
1. 2. |
morphine
fentanyl |
|
|
What kind of risk for injury related to continued agitation will increased the patients wor of breathing, o2 consumption and CO2 production
|
accidential extubation
|
|
|
What kinds of depression muct the patient be monitored for when using sedatives?
|
respiratory and cardiovascular depression
|
|
|
Patients who breathe asynchronously with mecanitcal ventilation may also benefit from titration of ventilator flow rates and other settings, as well as adressing treatable causes of agitation such as:
1. 2. 3. |
hypoxemia
pain hypercapnia |
|
|
Patients who remain asynchronous with mechanical ventilatio may require nueromuscular blockaid with agents such as Norcuron or Numbex to produce what effect on the body?
|
skeletal muscle relaxation and synchrony breathing on mechanical ventilation
|
|
|
_________ may also decrease the patients risk of lung injury related to excessive inspiratory/intrathoracic pressures.
|
Neuromuscular Blockade
|
|
|
What should patients receiving neuromuscular blockade receive?
|
sedatives and analgesic to the point of unconsciousness
|
|
|
Why is a patient suggested to be unconscious during neuromuscular blockade?
1. 2. 3. |
Comfort
eliminate awareness to terrifying experience and pain |
|
|
What is the medical supportive therapy primary goal?
|
treat underlying cause
|
|
|
What are two other goals that the medical supportive therapy try and accomplish
1. 2. |
maintain adequate cardiac output
maintain hemoglobin concentration |
|
|
What does cardiac output reflect?
|
BLOOD FLOW REACHING THE TISSUES
|
|
|
WHat is an important indicator of cardiac output?
|
blood pressure
|
|
|
Usually a systolic blood pressure of at least ____ is adequate to maintain perfusion to vital organs
|
90
|
|
|
How is decreased cardiac output treated?
|
by administration of IV fluids and medications or both
|
|
|
cardiac output may also decrease by changes in intrathoracic or intrapulmonary pressures from
|
PPV positive pressure ventilation
|
|
|
WHat is the primary carrier when delivering O2 to the tissues?
|
Hemoglobin
|
|
|
If the patient is anemic tissue O2 delivery will be ________
|
compromised
|
|
|
A hemoglobin of _______ or greater is typically ensures adequate O2 saturation of hemoglobin
|
9-10
|
|
|
If patient does not have an adequate hemoglobin concentration and it can not be maintained what should be monitored? _______ what should it be transfused with? ________
|
blood loss
Packed RBC |
|
|
Maintenance of _____ and _____ stores is especially important in patients who experience acute respiratory failure.
|
protein
energy |
|
|
Nutritional depletion causes a loss of ______ mass including those of the respiratory system
|
muscle
|
|
|
During acute manifestations of respiratory the risk of aspiration typically prevents ________
|
oral nutritional intake
|
|
|
WHat kind of nutrition will be administered to the respiratory failure patient
|
enteral or parenteral
|
|
|
What kind of diet should be avoided in patients who retian CO2?
|
High Carbohydrate
|
|
|
Why must the patient avoid carbs?
|
carbs metabolize into CO2 and increase the Co2 load on the patient
|
|
|
Older adults are at higher risk for developing respiratory failure becasue of the ?
|
reduction in ventilatory capacity that accompanies aging
|
|
|
Physiological aging of the lung may produce?
1. 2. 3. |
larger air spaces
loss of surface area dilated alveoli |
|
|
There are a few other things that happens with aging what are they?
1. 2. 3. |
diminished Elastic recoil within the airways
decreased chest wall compliance decreased respiratory muscle strength |
|
|
What is a big risk factor for respiratory failure in the older adult that their PaO2 falls further and the PaCo2 rises to a higher level before the respiratory system is stimulated to alter the rate and depth of breathing
|
smoking
|
|
|
A sudden and progressive form of acute respiratory failure is called
|
ARDS: Acute respiratory Distress syndrome
|
|
|
When ArDS happens the alveolar capilliary membrane becomes damaged and more permeable to __________
|
intravascular fluid
|
|
|
The alveoli fill with fluid resulting in:
1. 2. 3. 4. |
Severe dyspnea
hypoxemia reduced lung compliance infuse pulmonary infiltrates |
|
|
Mortality rate is about ___% Patients with both gram negative septic shock and ARDS you will have a mortality rate of ___% to ___%
|
50%
70-90% |
|
|
Direct Lung Injury: Common casues are:
1. 2. |
Aspiration
Pneumonia |
|
|
Less Common Causes of Direct Injury to the lungs are:
1. 2. 3. 4. 5. |
embolism
trauma near drowning O2 toxicity Radiation Pneumonitits Inhalation of toxic substances |
|
|
Indirect lung injury common causes include
1. 2. |
Sepsis
Trauma |
|
|
Less Common causes of indirect lung injury are:
1. 2. 3. 4. 5. 6. 7. |
pancreatitis
anaphylaxis cardiopulmonary bipass disseminated intravascular coagulation blood transfusions overdose narcotics nonpulmonary system distress head injury shock states |
|
|
Injury to the alveolar capilliary membrane is by two main events
1. Damage to the Type ____ alveolar cell and by 2. release of _________ mediators |
II
Inflammatory |
|
|
Most common cause of ARDS is
|
SEPSIS
|
|
|
Direct lung inury my cause ARDS or ARDS may develop as a consequence of the _____
|
SIRS Systemic inflammatory response syndrome
|
|
|
SIRS may have an infectious or a noninfectious etiology and is characterized by _____________ or clinical responses to _____________ following a ariety of Psysiologic insults including:
1, 2. 3. 4. |
severe trauma
gut ischemia lung injury sepsis |
|
|
ARDS may also develop from _____which results from Organ system dysfunction that progressively increases in severity and ultimately results in multisystem organ failure
|
MODS multiple organ dysfunction system
|
|
|
Pathophysiology changes of ARDS are though to be due to stimulation of the ________ and ________ systems which causes an attraction of neutraphills to the pulmonary interstituim
|
inflammatory and immune systems
|
|
|
Neutraphils cause a release of humeral, biochemical, and cellular __________-
|
mediators
|
|
|
These changes such as : increased pulmonary apilliary membrane permeability, destruction of elastin and collagen, formation of pulmonary microemboli, and pulmonary artery vasoconstriction is by the
|
neutrophilsbiochemical, humeral and cellular mediators
|
|
|
There are three pathophysiology changes in ARDS that are divided into three phases. These phases are
1. 2. 3 |
injury or exudative phase
reparative or proliferative phase fibrotic phase |
|
|
in the earliest phase of injury there is engorgement of the peribronchial and perivascular interstitial space which produces ______________
|
interstitial edema
|
|
|
Neutrophils adhere to the pulmonary microcirculation causeing damage to the ____________ and increased capillary permeability
|
vascular endothilium
|
|
|
Intrapulmonary shunt develops after the fluid from the interstitial space crosses the alveolar epithelium and enters the alveolar space why??
|
alveoli become filled with fluid and the bloodpassing through them cannont be oxygenated
|
|
|
Alveolar type I and type II cells do what?
|
produce surfactant
|
|
|
the function of surfactant is to maintain alveolar stability by
|
decreasing alveolar surface tension and preventing alveolar collapse
|
|
|
Decreased synthesis of surfactant and inactivation of existing surfactant cause the alveoli to become unstable which is know also as
|
atelectasis
|
|
|
Wide spread atelectasis further does what?
|
decreases lung compliance,
compromises gas exchange contributes to hypoxemia |
|
|
this type of membrane is composed of necrotic cells, protein, fibrin, and lies adjacent to the alveoli wall
|
hyaline
|
|
|
Hyaline membranes contribute to the development of _____ and ______ leading to a decrease in gas exchange capability and lung compliance
|
atelectasis
fibrosis |
|
|
Primary pathopghysiology changes that characterize in the injury or exudative phase or ARDS is
1. 2. |
edema
atelectasis |
|
|
this is the termed used for a severe V/Q mismatch and shunting of pulmonary capilliary blood result in hypoxemia unresponsive to increasing concentrations of O2
|
refractory hypoxemia
|
|
|
Reduced lung compliance greatly increases the patients what?
|
work of breathing
|
|
|
Hypoxemia and the stimulation of juxtacapilliary receptors in the stiff lung parenchyma (J reflex) initially cause an
|
increase in respiratory rate and a decrease in tidal volume
|
|
|
When you have a breathing pattern that increases the CO2 removal what kind of state would you be in that you would be in stated from ABGS?
|
respiratory Alkalosis
|
|
|
Cardiac Output increases in response to hypoxemia a compensatory mechanism to increase what
|
pulmonary blood flow
|
|
|
Second phase reparative or proliferative phase of ARDS begins 1-2 weeks after initial lung injury. During this phase there is an influx of neutrophils, monocytes and lymphocytes and fibroblast proliferation as part of the
|
Inflammatory response
|
|
|
The proliferated phase is complete when the diseased lung becomes characterized by dense _______
|
fibrious tissue
|
|
|
Hypoxemia worsens becasue of thickened alveolar membrane, causing diffusion limitation and ______
|
shunting
|
|
|
The third phase is the fibrotic phase which occurs 2-3 weeks. by this time the lung is completely what
|
remodeled by sparsely collagenous and fibrous tissues
|
|
|
There is a diffuse scarring and fibrosis, resulting in
|
decreased lung compliance
|
|
|
This results from pulmonary vascular destruction and fibrosis
|
pulmonary hypertension
|
|
|
Several factors seem to be important in determining the course of ARDS including
1. 2. 3. |
nature of the initial injury
extent and severity of the coexisting diseases pulmonary complication |
|
|
Some symptoms that the patient may experience at first would be :
1. 2. 3. 4. |
dyspnea
tachynpnea cough restlessness |
|
|
Chest auscultation may be normal or reveal fine, scattered what
|
crackles
|
|
|
ABGS usually indicate mild hypoxemia and respiratory alkalosis casued by ______
|
hyperventillation
|
|
|
This results from hypozemia and stimulation of J receptors
|
respiratory alkalosis
|
|
|
Pulmonary function tests in ARDS reveal decreased compliance and decreased lung volumes particularily a decrease in _______
|
functional residual capacity FRC
|
|
|
As ARDS progresses chest auscultation will reveal scattered to diffuse
|
crackles and rhonchi
|
|
|
X-Ray demonstrates diffuse and extensive ?
|
bilateral interstitial and alveolar infiltrates
|
|
|
HALLMARKS of ARDS include
1. 2. ____ ratio below 200 |
hypoxemia
PaO2/FIO2 |
|
|
ARDS progresses it is associated with profound respiratory distress requiring :
1. 2. |
Intubation or PPV ventillation
|
|
|
A chest X-Ray at this stage is usually termed :
|
white out or white lung
|
|
|
Diagnostic Findings in ARDS:
PaO2<50mm Hg on FIO2>40% with PEEP.5 cm H20 PaO2/FIO2 ration<200 |
Refractory Hypoxemia
|
|
|
Diagnostic Findings in ARDS:
New bilateral interstitial and alveolar infiltrates are found by |
chest x ray
|
|
|
Diagnostic Findings in ARDS:
<18mm Hg and no evidence of heart failure is the |
Pulmonary Artery Wedge Pressure
|
|
|
Complications associated with ARDS include:
Infection: 1. 2. 3. |
catherter related infection
nosocomial pneumonia sepsis |
|
|
Complications associated with ARDS include:
Respiratory Complications 1. 2. 3. 4. 5. |
O2 oxicity
Trauma Emboli Fibrosis |
|
|
Complications associated with ARDS include:
Gastrointestinal 1. 2. 3. |
Paralytic Ileus
Pneumoperitoneu, Stress Ulceration and Hemorrhage |
|
|
Complications associated with ARDS include:
Renal 1. |
Acute Renal failure
|
|
|
Complications associated with ARDS include:
Cardiac 1. 2. |
arrhythmias
decreased cardiac output |
|
|
Complications associated with ARDS include:
Hematologic 1. 2. 3. |
Anemia
disseminated intravascular coagulation Thrombocytopenia |
|
|
Complications associated with ARDS include:
ET intubation 1. 2. 3. 4. |
laryngeal ulceration
tracheal malacia Tracheal stenosis Tracheal ulceration |
|
|
The major cause of death in ARDS is often accompanied with sepsis
|
MODS
|
|
|
The vital organs most commonly involved are :
1. 2. 3. |
Kidneys
Liver Heart |
|
|
the organ systems most commonly involved are
1. 2. 3. |
CNS
Hematologic gastrointestinal |
|
|
These are all risk factors for what?
host defenses contaminated medical equipment invasive monitoring aspiration prolonged mechanical ventilation well colonization of respiratory tract |
nosocomial Pneumonia
|
|
|
In order to prevent nosocomial pneumonia we must :
1. 2. |
Infection control
elevation of head of bed 45 degrees |
|
|
This may result from rupture of overdistended alveoli during mechanical ventillation
|
Barotrauma
|
|
|
Barotrauma results in the presence of alveolar ____in locations where it is not usually found
|
air
|
|
|
TO avoid barotrauma patient with ARDS is sometimes ventilated with smaller _______ volumes resulting in higher PaCo2. This method of ventilation is called _______________
|
tidal
permissive hypercapnia |
|
|
this can occur in patients with ARDS when large tidal volumes results in alveolar fractures and movement of fluids and proteins fo in to the ________--
|
Volu-pressure trauma
alveolar spaces |
|
|
To limit Volu-pressure trauma it is reommended that smaller ______- volumes or pressure ventilation are used with these patients with ARDS
|
tidal
|
|
|
Stress ulcers occure and management strategies include correction of predisposing conditions such as
1. 2. 3. |
hypotension
shock acidosis |
|
|
Prophylactic management includes antiulcer agents such as
1. 2. 3. |
Pepcid
Prilosec Carafate |
|
|
Renal failure can occur from decreased ________ as a result from hypostension hypoxemia or hypercapnia
|
tissue oxygenation
|
|
|
Renal failure may also be because of administration of nephrotic drugs such as _____
|
aminoglycosides
|
|
|
The overall goals for a patient with ARDS is
1. 2. 3. |
PaO2 of at least 60
good lung ventilation normal pH |
|
|
There are three main respiratory therapies for the patient with ARDS
1. 2. 3. |
Oxygen Administration
Mechanical Ventilation Positioning Strategies |
|
|
Primary goal of O2 thereapy is to
|
correct hypoxemia
|
|
|
This is commonly used to monitor and assess the effectiveness of O2 therapy
|
Pulse Ox
|
|
|
during mechanical ventilation PEEP at 5 cm H20 is to compensate for loss of ______ from et tube
|
glottic function
|
|
|
ECMO and ECCO2R pass blood across a gas-exchanging membrane outside the body and then returned oxygenated blood where?
|
back to the body
|
|
|
ECCO2R with low frequency PPV allws the lungs to do what while the lung is not functioning
|
heal
|
|
|
Positioning is also a good way what position to what position is commonily used
|
supine to prone
|
|
|
what position is usually reserved for patients with refractory hypoxemia
|
prone
|
|
|
lateral rotational therapy provides continous rotation allowing 2 things
1. 2. |
postural drainage
mobilize pulmonary secretions |
|
|
If cardia output fails it is necessary to administer
1. 2. |
crystalloid fluids
colloid solutions |
|
|
Inotropic drugs such as may be necessary
|
dobutrex
intropin |
|
|
this is a serious acute respiratory infection caused by a coronavirus spread through air droplets in the air
|
SARS severe acute respiratory syndrome
|
|
|
SARS begins with ________--
|
fever greater than 100.4
|
|
|
Other manifestations include
|
headache and discomfort
|
|
|
Patient should be placed where in the hospital
|
isolation
|
|
|
Medications given to a patient with SARS is
1. 2. 3. |
antiviral meds ribavirin
antibiotics corticosteriods |
|
|
Hypercapnic respiatory failure can be casued by
|
asthma
|
|
|
Early sign of acute respiratory failure is
|
restlessness
|
|
|
O2 delivery system chosen for a patient in acute respiratory failure should be
|
maintain the PaO2 at 60 mm Hg or greater at the lowest O2 concentration possible
|
|
|
Most common early clinical manifestations of ARDS that the nurse may observe are
|
dyspnea and tachypnea
|
|
|
Maintenance of fluid balance in the patient with ARDS involves
|
mild fluid restriction and diuretics as necessary
|
|
|
Which of the following interventions is designed to prevent or limit barotrauma in the patient with ARDS who is mechanically ventillated?
|
the use of permissive hypercapnia
|

