![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
1
|
|

|
2
|
|
|
3
|
|

|
4
|
|

|
5
|
|
|
6
|
|

|
7
|
|

|
8
|
|

|
9
|
|

|
10
|
|
|
11
|
|

|
12
|
|

|
13
|
|
|
14
|
|
|
15
|
|
|
16
|
|
|
17
|
|
|
18
|
|

|
19
|
|
|
20
|
|

|
21
|
|

|
22
|
|
|
24
|
|
|
25
|
|
|
26
|
|

|
27
|
|
|
28
|
|

|
29
|
|

|
23
|
|
|
What radiologic plain film criteria are useful for determining malignant versus benign?
|
Standard textbooks give four aspects of a lesion to be examined:
(1) cortical destruction (2) periostitis (3) orientation or axis of the lesion (4) zone of transition. -These are plain film criteria and do not apply to CT or MR imaging in many instances. -Only the last one—the zone of transition—is accurate to a 90% plus rate. |
|
|
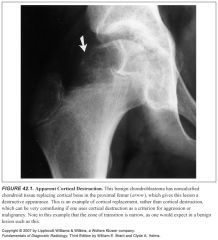
Talk about some lesions that demonstrate cortical destruction but are benign:
|
-Benign fibro-osseous lesions and cartilaginous lesions often have part of their noncalcified matrix (fibrous matrix or chondroid matrix, both of which are radiolucent on plain films) replacing cortical bone, which can give the false impression of cortical destruction on plain films
-Also, benign processes such as infection and EG can cause extensive cortical destruction and mimic a malignant tumor -It is well known that aneurysmal bone cysts cause such thinning of the cortex as to make the cortex radiographically undetectable -For these reasons, cortical destruction can occasionally be misleading. -Cortical destruction always makes one think of a malignant lesion when using the “gestalt approach,” but the lesion must also have other criteria for a malignant process, such as a wide zone of transition |
|
|
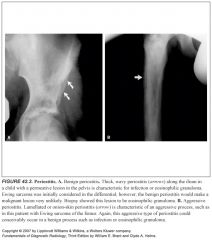
What sorts of things cause periosteal reaction?
|
Periosteal reaction occurs in a nonspecific manner whenever the periosteum is irritated, whether by a malignant tumor, a benign tumor, infection, or trauma.
Callus formation in a fracture is actually just periosteal reaction of the most benign type. |
|
|
Explain the difference between benign and malignant periosteal reaction:
Can benign things cause aggressive periosteal reaction and vice versa? |
-Periosteal reaction occurs in two types: benign or aggressive, based more on the timing of the irritation than on whether it is a malignant or benign process causing the periostitis.
-For example, a slow-growing benign tumor will cause thick, wavy, uniform, or dense periostitis because it is a low-grade chronic irritation that gives the periosteum time to lay down thick new bone and remodel into more normal cortex. -A malignant tumor causes a periosteal reaction that is high grade and more acute; hence, the periosteum does not have time to consolidate. -It appears lamellated (onion-skinned) or amorphous or even sunburst-like. -If the irritation stops or diminishes, the aggressive periostitis will solidify and appear benign. -Therefore, when periostitis is seen, the radiologist should try to characterize it into either a benign (thick, dense, wavy) type or an aggressive (lamellated, amorphous, sunburst) type. -Many benign lesions cause aggressive periostitis, such as infection, EG, aneurysmal bone cysts, osteoid osteomas, and even trauma. -Detection of benign periostitis, however, can be very helpful because malignant lesions will not cause benign periostitis. -Some investigators state that the only way benign periostitis can occur in a malignant lesion is if there is a concomitant fracture or infection. -Exceptions to this are extremely uncommon. |
|
|
What is the typical axis of a Ewing's sarcoma?
|
Ewing sarcoma usually has its axis along the shaft of a long bone.
|
|
|
Define "zone of transition":
What's the difference between a narrow and wide zone of transition? |
-The zone of transition is the border of the lesion with the normal bone.
-It is said to be “narrow” if it is so well defined that it can be drawn with a fine-point pen. -If it is imperceptible and cannot be clearly drawn at all, it is said to be “wide.” -Obviously, all shades of gray lie in between, but most lesions can be characterized as having either a narrow or a wide zone of transition. -If the lesion has a sclerotic border, it, of course, has a narrow zone of transition. -If a lesion has a narrow zone of transition, a benign process should be considered as the most likely possibility. -If a lesion has a wide zone of transition, it is aggressive, although not necessarily malignant. |
|
|
Why is cortical destruction sometimes tricky to evaluate in aneurysmal bone cysts?
|
Their walls can be so thin that they become imperceivable, thus mimicking cortical destruction
|
|
|
Define cortical replacement:
How can you tell a lesion that is replacing cortex from a lesion that is destroying cortex? |
-Benign fibro-osseous lesions and cartilaginous lesions often have part of their noncalcified matrix (fibrous matrix or chondroid matrix, both of which are radiolucent on plain films) replacing cortical bone, which can give the false impression of cortical destruction on plain films
-These benign lesions will often still demonstrate a narrow zone of transition |
|
|
What's the first thing out of your mouth when you see a malignant tumor in a patient age 1-30?
|
Ewing sarcoma, osteogenic sarcoma
|
|
|
What diagnoses are you thinking of when you see a malignant lesion in a patient age 30–40?
|
-Giant cell tumor
-Parosteal sarcoma, fibrosarcoma -Malignant fibrous histiocytoma -1° lymphoma of bone |
|
|
What are the most common malignant bone lesions in patients over 40?
|
-Chondrosarcoma
-Metastatic disease -Myeloma |
|
|
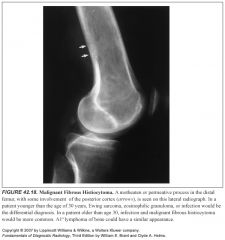
What lesions classically demonstrate a permeative appearance?
|
-Round cell tumors such as multiple myeloma, reticulum cell sarcoma (primary lymphoma of bone), and Ewing sarcoma are typical of this type of lesion.
-Infection and EG also can have this same appearance. |
|
|
How is the age of the patient helpful when discussing malignant bone lesions?
|
-Osteosarcoma and Ewing sarcoma are the only childhood primary malignant tumors of bone, and after the age of 40, only metastatic disease, myeloma, and chondrosarcoma are common.
-Although there are certainly outliers that are uncommon, these age guidelines are extremely useful. |
|
|
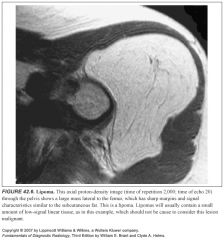
What does a lipoma look like on MR?
|
-Sharp margins
-Signal characteristics similar to the subcutaneous fat -Lipomas will usually contain a small amount of low-signal linear tissue, which should not be cause to consider this lesion malignant |
|
|
What does a hemangioma look like on MR?
|
-Hemangiomas typically have mixed fatty and vascular tissue, which gives high signal on both T1 and T2 sequences.
-They characteristically have low-signal serpiginous vessels visible. |
|
|
What does a schwannoma look like on MR?
|
-High T2 signal like a fluid collection
-Diffuse enhancement |
|
|
What is MR's role in assessing bone tumors?
|
-MR is without question the imaging procedure of choice for determining the extent of a lesion, both in the skeleton and in the soft tissues. For this reason, if resection of a tumor is contemplated, MR should be performed.
-In assessing benignity versus malignancy, MR is somewhat controversial |
|
|
What are benign features on MR?
|
Benign lesions tend to be well marginated, to have uniform and homogeneous signal, not to encase neurovascular structures, and not to invade bone.
|
|
|
What are malignant features on MR?
|
Malignant lesions tend to have irregular margins and inhomogeneous signal, and they may encase neurovascular structures or invade bone.
|
|
|
What are the usual signal characteristics of bony lesions?
What are the exceptions to this? |
-Although almost all tumors will have low signal on T1WI, which become very high in signal intensity with T2 weighting (as will fluid collections)
-There are a few exceptions. Fibrosarcomas, malignant fibrous histiocytomas, and desmoid tumors can occasionally demonstrate low signal on both T1W and T2W sequences. -Any tumor with calcification will be low in signal on both T1 and T2 sequences. |
|
|
What benign things can look like soft tissue tumors (benign or malignant) on MR?
|
Intramuscular injection sites can mimic soft tissue tumors, as can any area of soft tissue trauma.
|
|
|
Which type of osteosarcoma is usually completely lytic?
|
These are usually telangiectatic osteosarcomas.
|
|
|
What is the most common malignant primary bone tumor?
|
Osteosarcoma is the most common malignant primary bone tumor.
|
|
|
Why is there a second peak incidence of osteosarcoma in patients older than 60?
|
This is probably because of secondary osteosarcoma in Paget disease and because of prior radiation.
|
|
|
Imaging characteristics of osteosarcoma (all modalities)?
|
-Although osteosarcoma typically occurs toward the end of a long bone, it may occur anywhere in the skeleton with enough frequency that location is not a helpful discriminator.
-These lesions are usually destructive, with obvious sclerosis present from either tumor new bone formation or reactive sclerosis -MR of an osteosarcoma generally reveals a large soft tissue component with heterogeneous high and low signal on both T1WIs and T2WIs |
|
|
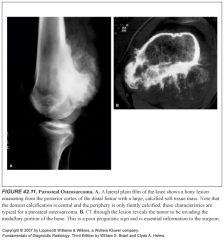
What is a parosteal osteosarcoma?
What does it look like? Why is it important to distinguish from central osteosarcomas? Where is a common place for these tumors to arise? |
-A parosteal osteosarcoma originates from the periosteum of the bone and grows outside the bone
-It often wraps around the diaphysis without breaking through the cortex at all. -It occurs in an older age group than the central osteosarcomas and is not as aggressive or as deadly as long as it has not extended into the medullary portion of the bone. -The radiologist needs to evaluate the lesion for invasion of the adjacent cortex to help determine treatment and prognosis. This is best done with CT or MR. -A common location from which parosteal osteosarcomas arise is the posterior femur, near the knee. |
|
|
What benign lesions can mimic a parosteal osteosarcoma both on imaging and histology?
|
-A lesion that can mimic an early parosteal osteosarcoma in the posterior distal femur is a cortical desmoid tumor.
-A cortical desmoid tumor is an avulsion injury that is totally benign but can appear somewhat aggressive. -Unfortunately, it can appear malignant histologically, so biopsy can lead to disastrous consequences. -Another lesion that can be confused with a parosteal osteosarcoma is an area of myositis ossificans. Like cortical desmoid tumors, areas of myositis ossificans can be histologically confused for malignancies, with disastrous consequences |
|
|
What is a cortical desmoid tumor?
|
-A cortical desmoid tumor is an avulsion injury of the posterior distal femur that is totally benign but can appear somewhat aggressive.
|
|
|
What are classic imaging features of Ewing's sarcoma?
|
-Ewing sarcoma is classically a permeative (multiple small holes) lesion in the diaphysis of a long bone in a child.
-Only about 40% of these tumors occur in the diaphysis, however, with the remainder being metaphyseal and diametaphyseal and in flat bones. -Although they are most often permeative in appearance, they can elicit reactive new bone that can give the lesion a partially sclerotic or “patchy” appearance. -Ewing sarcomas often have an onion-skin type of periostitis, but they can also have periostitis that is sunburst-like or amorphous in character |
|
|
What is the classic differential for a permeative lesion in a child? What characteristics help you narrow this differential?
|
-The classic differential diagnosis for a permeative lesion in a child is Ewing sarcoma, infection, and EG.
-These three entities can appear radiologically identical. -Ewing sarcoma should be removed from the differential diagnosis if definite benign periostitis or a sequestration is present. -The presence or absence of a soft tissue mass is not helpful in distinguishing between these three lesions. -The presence of symptoms is not helpful, because all three entities can be symptomatic. |
|
|
How can you tell a chondrosarcoma from an enchondroma?
|
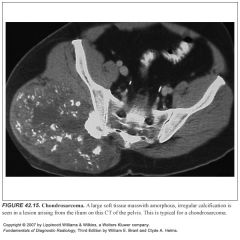
-The truth of the matter is neither radiologists nor pathologists can reliably distinguish between enchondromas and low-grade chondrosarcomas.
-For these reasons, the diagnosis of “possible chondrosarcoma” should be reserved for those lesions that are painful or that show definite aggressive characteristics, such as periostitis and destruction. -MR can be very useful in distinguishing a benign enchondroma from a chondrosarcoma. -If a soft tissue mass or edema is present, it is unlikely to be an enchondroma. |
|
|
What characteristics would make you suspicious of a chondrosarcoma?
|
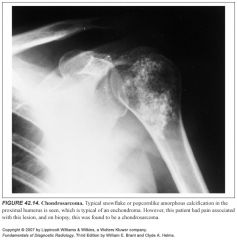
Chondrosarcoma should be considered in the diagnosis any time there is a bony or soft tissue mass with amorphous, snowflake calcification in an older patient (>40 years)
|
|
|
How can you tell the difference between a benign and malignant giant cell tumor?
|
-Radiologically, benign and malignant giant cell tumors appear identical.
-Histologically, benign and malignant giant cell tumors appear the same. -If metastases (usually to the lung) occur, the tumor is considered by most oncologists to be malignant. -This is quite rare. |
|
|
What does a fibrosarcoma look like?
|
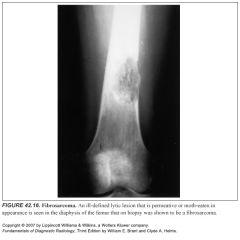
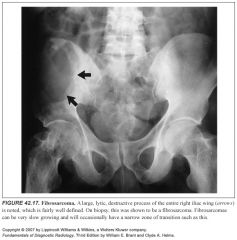
-Fibrosarcomas are lytic malignant tumors that do not produce osteoid or chondroid matrix.
-They usually do not cause reactive new bone and, therefore, are almost always lytic in appearance. -This lytic appearance may take any form, from permeative to moth-eaten to a fairly well-defined area of lysis. -The age range for fibrosarcoma is quite broad, but they tend to predominate in the fourth decade. -This is one of the few malignant tumors that can, on occasion, have a bony sequestrum. |
|
|
What malignant bony tumors can have a bony sequestrum?
|
Fibrosarcoma
MFH Desmoid tumor |
|
|
What do malignant fibrous histiocyytomas look like?
|
Radiologically, when they arise in bone, they appear identical to fibrosarcomas: lytic lesions with variations extending from permeative to fairly well defined. Like fibrosarcomas, they may, on occasion, have a bony sequestrum.
|
|
|
What is a desmoid tumor?
What does a desmoid tumor look like on imaging? |
-Desmoid tumor (not to be confused with a cortical desmoid) is a half-grade fibrosarcoma.
-They most commonly arise in the soft tissues and are uncommon in the bony skeleton. -These lesions, like fibrosarcoma, are lytic when in bone but are usually fairly well defined because of their slow growth. -They often have benign periostitis present that has thick spicules or “spikes.” -They usually have a multilocular appearance with thick bony septa -They are slow growing and do not metastasize, but they can exhibit inexorable tumor extension into surrounding soft tissues, with devastating results. -Like fibrosarcoma and malignant fibrous histiocytomas, these lesions can exhibit a bony sequestrum. |
|
|
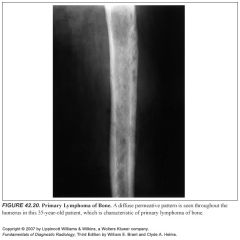
What does primary lymphoma of bone look like on imaging?
|
-Primary lymphoma of bone is a neoplasm with a radiologic appearance identical to that of Ewing sarcoma—that is, a permeative or moth-eaten pattern.
-Primary lymphoma of bone tends to occur in an older age group than Ewing sarcoma, and, whereas Ewing sarcomas are typically systemically symptomatic, patients with primary lymphoma of bone are often asymptomatic. -It is said to be the only malignant tumor that can involve a large amount of bone while the patient is asymptomatic. |
|
|
Which cancer almost always produces lytic bony metastases?
|
Although nearly every metastatic bone lesion can be either lytic or blastic, the only primary tumor that virtually never presents with blastic metastatic disease is renal cell carcinoma.
-The classic differential diagnosis for an expansile, lytic metastasis is renal cell or thyroid carcinoma |
|
|
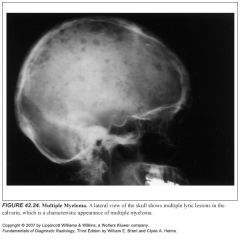
What does multiple myeloma look like on imaging? Bone scans?
|
-Myeloma typically has a diffuse permeative appearance that can mimic a Ewing sarcoma or primary lymphoma of bone.
-Rarely, myeloma can present with multiple sclerotic foci, thus resembling diffuse metastatic disease. -Myeloma is one of the only lesions that is not characteristically hot on a radionuclide bone scan; therefore, radiologic “bone surveys” are performed in place of radionuclide bone scans when evidence of myeloma is found clinically. -Occasionally, myeloma will present with a lytic bone lesion called a plasmacytoma. This lesion can mimic any lytic bone lesion, benign or aggressive, in its appearance; it can precede other evidence of myeloma by up to 3 years. |
|
|
What are the two most common soft tissue tumors?
|
The two most common soft tissue tumors, malignant fibrous histiocytoma and liposarcoma, should be mentioned as the most likely possibilities for any soft tissue tumor, but any cell type can produce a benign or malignant tumor and mimic any other soft tissue tumor.
|
|
|
What two types of soft tissue tumors are so homogeneously T2 bright that they can be mistaken for fluid collections?
|
Synovial sarcomas are one of two types of tumors (along with neural tumors) that are typically homogeneously bright on T2WIs—to the extent that they can be mistaken for a fluid collection.
|
|
|
What does synovial sarcomas look like on imaging?
|
-Synovial sarcomas or synoviomas, only rarely originate in a joint. They are often adjacent to joints.
-They are so homogeneously T2 bright that they could be mistaken for fluid collections |
|
|
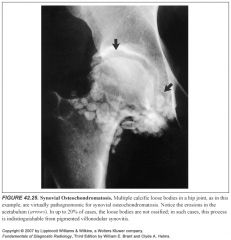
What exactly is synovial osteochondromatosis? What lesion can it mimic?
|
-Synovial osteochondromatosis is a benign joint lesion that probably occurs from metaplasia of the synovium and leads to multiple calcific loose bodies in a joint.
-This can histologically mimic a chondrosarcoma and therefore is best diagnosed radiographically, as it has a pathognomonic radiographic appearance. -Up to 20% of the time, the loose bodies do not calcify, however, and the osteochondromatosis then can mimic pigmented villonodular synovitis. |
|
|
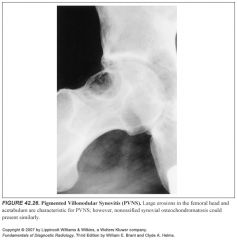
What exactly is pigmented villonodular synovitis? What other condition can mimic PVNS?
|
-Pigmented villonodular synovitis is a benign synovial soft tissue process that causes joint swelling and pain and, occasionally, joint erosions.
-It virtually never has calcifications associated with it. -The MR appearance of pigmented villonodular synovitis is characteristic. -Marked low signal lining the synovium is seen on T1WIs and T2WIs because of the hemosiderin deposits -Chronic bleeding into a joint, so-called hemosiderotic arthritis, can have a similar appearance but is encountered uncommonly. |
|
|
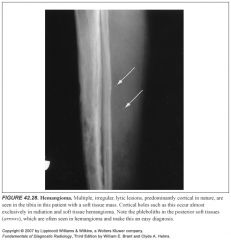
What do hemangiomas look like on plain films?
|
Hemangiomas will often have phleboliths associated with them and often cause cortical holes in adjacent bone that can mimic a permeative or moth-eaten pattern in a pseudopermeative pattern.
|

