![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
125 Cards in this Set
- Front
- Back
|
Dysphagia |
Difficulty swallowing Inability to initiate swallowing Sensation that swallowed solids/liquids "stick" in esophagus |
|
|
Dysphagia Type 1 |
Problems in delivery of food/fluid into the esophagus |
|
|
Dysphagia Type 1 Symptoms |
May cough and expel the ingested food/fluid through mouth or nose Aspirate when attempting to swallow Worse with liquids than solids |
|
|
Dysphagia Type 2 |
Problems in transport of bolus down esophagus |
|
|
Dysphagia Type 2 Symptoms |
Sensation food is "stuck" behind sternum May have impaired passage of liquids |
|
|
Dysphagia Type 3 |
Problems in bolus entry into stomach |
|
|
Dysphagia Type 3 Symptoms |
Tightness or pain in substernal area during swallowing process |
|
|
Esophageal Pain: Heartburn (Pyrosis) |
Reflux of gastric contents into esophagus High acidic contents are an irritant to sensory afferent nerve endings in mucosa Causes spasms of esophageal muscle |
|
|
Heartburn Symptoms |
Substernal burning sensation that may radiate to neck or throat |
|
|
Esophageal Pain: Chest Pain |
Esophageal Distention or Obstruction |
|
|
Esophageal Pain: Chest Pain Symptoms |
Similar to angina pectoris (radiates to neck, shoulder, arm, and jaw) Brought on by swallowing |
|
|
Abdominal Pain |
May be first sign of GI tract disorder Three types: visceral, somatic, and referred pain |
|
|
Abdominal Pain: Visceral Pain |
Stretching or distending an abdominal organ Inflammation |
|
|
Abdominal Pain: Visceral Pain Symptoms |
Diffuse, poorly localized Gnawing, burning, or cramping |
|
|
Abdominal Pain: Somatic Pain |
Injury to abdominal wall, parietal peritoneum, root of the mesentery of the diaphragm |
|
|
Abdominal Pain: Somatic Pain Symptoms |
Sharp, intense pain Well localized to area of irritation |
|
|
Abdominal Pain: Referred Pain |
Felt at a location distant from source of pain In the same dermatome or neurosegment |
|
|
Abdominal Pain: Referred Pain Symptoms |
Sharp and well localized May be felt in skin or deeper tissues |
|
|
Abdominal Pain: Acute |
Instantaneous onset Perforated ulcer or ruptured organ |
|
|
Abdominal Pain: Chronic |
Diverticulitis Ulcerative colitis |
|
|
Vomiting |
Forceful expulsion of gastric contents through mouth Accompanied by nausea Characteristics of vomitus suggest nature of disorder |
|
|
Vomiting Causes |
Coordinated sequence of abdominal muscle contraction with reverse esophageal peristalsis Alteration in the integrity of the GI tract wall Alterations in motility |
|
|
Intestinal Gas |
Results from altered motility or lack of digestive enzymes Belching: eructation of swallowed air |
|
|
Belching Causes |
Motility disorder Gastric outlet obstruction preventing passage of air from stomach to small intestine Swallowing of air Bacterial and digestive action or intestinal contents Diffusion from the blood Neutralization of acids by bicarbonate in upper GI tract |
|
|
Intestinal Gas: Abdominal Distention |
Causes: Failure to adequately digest nutrients such as lactose Excess gas resulting from defect in intestinal motility |
|
|
Intestinal Gas: Flatus |
Causes: Increased amounts of gas produced by action of bacteria on gas-producing nutritional substrates |
|
|
Bowel Pattern Alterations: Constipation |
Small, infrequent, or difficult bowel movements Causes: Dietary (low in fiber) Lack of exercise Pathologic conditions (ex. diverticulitis, obstruction) |
|
|
Bowel Pattern Alterations: Diarrhea |
Increased frequency and fluidity of bowel movements caused by decreased transit time in SI |
|
|
Diarrhea: Acute |
Acute infection Emotional stress Leakage of stool around impacted feces |
|
|
Diarrhea Chronic |
Chronic GI tract infection Alteration in motility or integrity of GI tract Malabsorption Certain endocrine disorders Food allergy Ingestion of irritants Caffeine |
|
|
Pathophysiologic Mechanisms: Osmotic |
Increased amounts of poorly, absorbed solutes in the intestine |
|
|
Pathophysiologic Mechanisms: Secretory |
Due to toxins that stimulate intestinal fluid secretion and impair absorption |
|
|
Pathophysiologic Mechanisms: Exudative |
Mucus, blood, protein Results from inflammatory processes |
|
|
Pathophysiologic Mechanisms: Diarrhea Related to Motility Disturbances |
Dumping syndrome |
|
|
Stomatitis |
Inflammation of oral mucosa Causes: Pathogenic organisms Trauma Chemical irritants Chemotherapy, radiation Nutritional deficiencies |
|
|
Acute Herpetic Stomatitis |
"Cold sores" Signs and symptoms: Fever Pharyngitis Prodromal tingling and itching Vesicles on erythematous base that rupture, leaving a painful ulcer |
|
|
Acute Herpetic Stomatitis Treatment |
Use adequate oral hygiene Medications: antiviral meds (famciclovir, valacyclovir) |
|
|
Gastroesophageal Reflux Disease (GERD) |
Backflow of gastric contents into esophagus through LES Inflammation caused by reflux or highly acidic material Progression can lead to ulceration, fibrotic scarring, strictures, Barrett esophagus |
|
|
Gastroesophageal Reflux Disease (GERD) Causes |
Any condition or agent that alters closure strength of LES or increases abdominal pressure Fatty foods Caffeine Large amounts of alcohol Cigarette smoking Sleep position Pharmacologic agents Anatomic features (ex. hiatal hernia) |
|
|
Esophagitis: Barrett Esophagus |
Complication when columnar tissue replaces normal squamous epithelium of the distal esophagus Carries a significant risk for esophageal cancer |
|
|
Hiatal Hernia |
Defect in diaphragm when a portion of the stomach passes through the diaphragmatic opening into the thorax Risk increases with age Women more than men Can be life threatening if large portion of stomach becomes caught above diaphragm and becomes incarcerated |
|
|
Hiatal Hernia Signs and Symptoms |
Similar to GERD Heartburn Chest pain Dysphagia |
|
|
Hiatal Hernia: Sliding Hernia |
Most common Portion of stomach and gastoesophageal junction slip up into thorax above diaphragm |
|
|
Hiatal Hernia: Paraesophagal Hernia (Rolling) |
Part of greater curvature of stomach rolls through the diaphragmatic defect |
|
|
Mallory-Weiss Syndrome |
Bleeding caused by a tear in mucosa or submucosa of the cardia or lower portion of esophagus Tear is usually longitudinal Primary cause is forceful or prolonged vomiting |
|
|
Mallory-Weiss Syndrome: Other Factors or Contributions |
Excessive ingestion of alcohol and salicylates Coughing Straining during bowel movements Trauma Hiatal Hernia Esophagitis Gastritis |
|
|
Esophageal Varices |
Complication of portal hypertension resulting from alcoholic or posthepatits cirrhosis Affects more than half of cirrhotic patients 30% have variceal hemorrhage within 2 years of diagnosis High mortality rate |
|
|
Gastritis: Acute |
Precipitated by ingestion of irritating substances Example: alcohol and aspirin |
|
|
Gastritis: Acute Signs and Symptoms |
Anorexia Nausea Vomiting Postprandial discomfort Hematemsis |
|
|
Gastritis: Chronic |
Helicobacter pylori is nearly always a factor Complications: Peptic ulcer disease Gastric adenocarcinoma Mucosa-associated lymphoid tissue lymphoma |
|
|
Gastroenteritis |
Inflammation of stomach and small intestine Usually a result of another GI disorder Acute is caused by direct infection of tract by pathogenic virus or bacterial toxin May be caused by imbalance in normal bacterial flora by introduction of usual bacteria (travel) |
|
|
Gastroenteritis Signs and Symptoms |
Diarrhea Abdominal discomfort and pain Nausea Vomiting Fever Malaise |
|
|
Gastroenteritis Treatment |
Replace fluid and electrolytes |
|
|
Peptic Ulcer Disease |
Causes: H. pylori Stress Smoking Alcohol Spicy foods Smoking Genetic |
|
|
Peptic Ulcer Disease: Gastric |
Due to breakdown of protective mucous layer that prevents diffusion of acids into gastric epithelia Barrier of epithelial layer and slightly alkaline layer of mucus interrupted with chronic irritations |
|
|
Peptic Ulcer Disease: Duodenal |
Inappropriate excess secretion of acid Increased basal activity of vagus nerve Stimulates pyloric antrum cells to release gastrin to act on gastric parietal cells to release HCl Results in high level of HCl |
|
|
Peptic Ulcer Disease Treatment |
H. pylori; antibiotics H2 antagonists Proton pump inhibitors Sucralfate Smoking cessation Avoidance of ASA and NSAIDs, caffeinated beverages, alcohol, and irritating foods |
|
|
Ulcerative Colitis |
Large ulcers form in mucosal layer of colon and rectum Associated with increased cancer risk after 8-10 years of disease Hallmark symptoms are bloody diarrhea and lower abdominal pain |
|
|
Ulcerative Colitis Treatment |
Corticosteroids Salicylate analogs Immunodulating agents: azathioprine and mercaptopurine |
|
|
Crohn Disease |
Affects proximal portion of the colon or terminal ileum Inflammation of all layers of the intestinal wall resulting from blockage and inflammation of lymphatic vessels Suggestive findings are ulcerations, strictures, and fistulas |
|
|
Crohn Disease Signs and Symptoms |
Intermittent bouts of fever Diarrhea RLQ pain (right lower quadrent) May have RLQ, tenderness |
|
|
Crohn Disease Treatment |
Smoking cessation, drugs similar to ulcerative colitis |
|
|
Antibiotic-Associated Colitis (AAC) (also called Pseudomembranous Enterocolitis) |
Acute inflammation and necrosis of small and large intestine Caused by clostridium difficle (exposure to antibiotics) |
|
|
Antibiotic-Associated Colitis (AAC) (also called Pseudomembranous Enterocolitis) Signs and Symptoms |
Diarrhea (often bloody), abdominal pain, fever, colonic perforation (rare) |
|
|
Antibiotic-Associated Colitis (AAC) (also called Pseudomembranous Enterocolitis) Treatment |
Stop current antibiotic (if possible), treat ischemia, oral antibiotics such as metronidazole or vancomycin |
|
|
Necrotizing Enterocolitis (NEC) |
Occurs in premature infants (<34 wks) and infants with low birth weight (<5 lb) Characterized by diffuse or patchy intestinal necrosis with sepsis |
|
|
Necrotizing Enterocolitis Signs and Symptoms |
Distended abdomen and stomach, intestinal perforation |
|
|
Necrotizing Enterocolitis Treatment |
Surgical with antibiotics |
|
|
Appendicitis |
Obstruction by fecalith or inflammation |
|
|
Appendicitis Signs and Symptoms |
RLQ pain ("McBurney's point") (classic, but may be anywhere), nausea, vomiting, fever, diarrhea, RLQ tenderness, systemic signs of inflammation |
|
|
Appendicitis Treatment |
Immediate surgical removal |
|
|
Diverticular Disease (Diverticulosis) |
Presence of diverticula in the colon Results in low intake of dietary fiber |
|
|
Diverticular Disease Signs and Symptoms |
Diverticulosis - Asymptomatic Diverticulitis - Fever, acute lower abdominal pain |
|
|
Diverticular Disease Treatment |
Antibiotics and surgery for complicated diverticulitis |
|
|
Irritable Bowel Syndrome |
Chronic (>3 months) functional disorder Fluctuations in stool frequency and consistency (no nocturnal diarrhea) Cause: unclear but slow wave activity of bowel increased Often associated with anxiety or depression |
|
|
Irritable Bowel Syndrome Signs and Symptoms |
Diarrhea or constipation or alteration of both, abdominal cramping pain, mucus in stool, nausea, bloating |
|
|
Irritable Bowel Syndrome Treatment |
Antidiarrheal agents, antispasmodic medications, increased fiber in diet |
|
|
Intestinal Obstruction Mechanical |
Adhesions, hernia, tumors, impacted feces, volvulus, intussusception |
|
|
Intestinal Obstruction Functional |
Conditions that inhibit peristalsis such as narcotics, anesthesia, surgery, peritonitis, hypokalemia, spinal cord injuries |
|
|
Intestinal Obstruction Signs and Symptoms |
Depend on site and duration: dehydration, vomiting, electrolyte depletion, constipation, abdominal distention |
|
|
Intestinal Obstruction Treatment |
Surgical intervention or decompression with intestinal tube If left uncorrected may cause wall edema, ischemia, and necrosis leading to bowel gangrene, sepsis, and shock |
|
|
Volvulus |
Twisting of bowel on itself causing intestinal obstruction and blood vessel compression (ischemia) Results from anomaly of rotation, ingested foreign body, or adhesion; cannot always be determined Common sites are cecum and sigmoid colon Sudden, tight, twisting of bowel impedes blood flow to bowel Impeded blood flow lead to gangrene, necrosis, and perforation Life-threatening condition |
|
|
Volvulus Signs and Symptoms |
Depend on site and duration: dehydration, vomiting, electrolyte depletion |
|
|
Volvulus Treatment |
Varies according to severity and location: surgical intervention or decompression |
|
|
Intussusception |
Telescoping/invagination of a portion of bowel into adjacent (usually distal) bowel causing intestinal obstruction Males more than females |
|
|
Intussusception Signs and Symptoms |
Increased bowel sounds, abdominal pain, varies |
|
|
Intussusception Treatment |
Surgical treatment |
|
|
Hirschsprung Disease |
Familial, congenital disorder of the large intestine in which the autonomic ganglia are reduced or absent Occurs 1:5000 live births Most commonly found in infants and children Male more than females |
|
|
Hirschsprung Disease Signs and Symptoms |
Profuse diarrhea, hypovolemic shock, intestinal perforation |
|
|
Hirschsprung Disease Treatment |
Colonic lavage, surgical intervention |
|
|
Malabsorption Disorders |
Failure of GI tract to absorb or normally digest one or more dietary constituents |
|
|
Malabsorption Causes |
Enzyme abnormalities Infection Radiation enteritis |
|
|
Malabsorption Signs and Symptoms |
Diarrhea Passage of inappropriately processed intestinal contents |
|
|
Malabsorption Types |
Celiac disease and tropical sprue |
|
|
Celiac Disease |
Familial intolerance of gluten-containing foods Lead to inflammation and atrophy of the intestinal villi Impaired nutrient absorption: reduced surface area and decreased brush border enzymes 2x increase of intestinal malignancy |
|
|
Celiac Disease Diagnosis |
Intestinal biopsy Anti-tissue transglutaminase antibody (anti-ttg) Immunoglobulin A (IgA) endomysial antibody |
|
|
Celiac Disease Treatment |
Gluten-free diet Supplemental Fe, folate, B12, fat-soluble vitamins (A, D, E, K) |
|
|
Tropical Sprue |
Malabsorptive syndrome of unknown cause Prevalent in equatorial countries (living/visiting) Adults more than children |
|
|
Tropical Sprue Etiology |
Mucosa of small intestine atrophies resulting in malabsroption along with B12 and folic acid deficiency |
|
|
Tropical Sprue Signs and Symptoms |
Severe diarrhea with blood-tinged stools, abdominal distention, steatorrhea |
|
|
Tropical Sprue Treatment |
Predictability depends on area Antidiarrheals, prolonged antimicrobial therapy |
|
|
Dumping Syndrome |
Dumping of stomach contents into small intestine due to impaired gastric emptying Common after gastrectomy Large volume of hyperosmolar food is dumped rapidly into small intestine leading to increased bowel motility Rapid absorption of large amount of glucose leads to an excessive rise in plasma insulin |
|
|
Dumping Syndrome Signs and Symptoms |
Diarrhea, abdominal pain Rapid fall in blood glucose level 1-3 hr after meal (rebound hypoglycemia) |
|
|
Dumping Syndrome Treatment |
Eating small meals throughout day instead of large meals, carbohydrate restriction, medications to reduce bowel motility |
|
|
Short-Bowel Syndrome |
Severe diarrhea and significant malabsorption Develops after surgical removal of large portions of SI Rapid transit time and reduced surface area for absorption Diminished ability to absorb H20, electrolytes, protein, fat, carbohydrates, vitamins, and trace elements |
|
|
Short Bowel Syndrome Signs and Symptoms |
Diarrhea and malabsorption |
|
|
Short Bowel Syndrome Treatment |
Temporary or indefinite intravenous nutritional support |
|
|
Esophageal Cancer |
Accounts for 1%-2% of all cancers Men more than women Survival rate of <20% in men older than 60 years |
|
|
Esophageal Cancer Risk Factors |
Genetic, diet high in nitrosamine content, chronic severe reflux (Barrett esophagus), environmental, smoking, alcohol |
|
|
Esophageal Cancer Prognosis |
Poor; spreads extensively to surrounding organs Very high degree of metastasis |
|
|
Esophageal Treatment |
Stent placement, tumor ablation through heat probe and laser |
|
|
Gastric Carcinoma |
Prevalence in Japan 10x higher than U.S. Men > 30 years |
|
|
Gastric Carcinoma Stages (early and advanced) |
Determined by penetration into major muscle layer of stomach, involvement of lymphatic system and surrounding organs |
|
|
Gastric Carcinoma Risk Factors |
H. pylori infection, genetic, dietary habits, environmental factors, smoking |
|
|
Small Intestinal Neoplasms |
Benign or Malignant Unusual: accounts for <5% GI tumors >50 years Causes partial or complete obstruction Depending on extent and type |
|
|
Small Intestinal Neoplasms Signs and Symptoms |
Depends on type and extent; partial or complete obstruction of small bowel may occur |
|
|
Small Intestinal Neoplasms Treatment |
Surgical removal of tumor and affected portion of SI |
|
|
Colonic Polyps |
Any protrusion into the lumen of the GI tract Benign or malignant |
|
|
Colonic Polyps Signs and Symptoms |
Usually none; may cause occult or gross bleeding, abdominal pain |
|
|
Colonic Polyps Treatment |
Varies according to size, type, and location |
|
|
Colon Cancer Risk Factors |
Increases after age 40 High fat, low fiber diet Polyps, chronic irritation or inflammation |
|
|
Colon Cancer Warning Signs |
Black, tarry, or pencil shaped stool Change in bowel habits Urgent need to defecate on awakening in morning Alternating constipation and diarrhea Sensation of rectal fullness Dull ache may be felt in rectum/sacral region |
|
|
Colon Cancer Prognosis |
Early detection, better prognosis Depends on extent of tumor invasion, cell type, degree of dysplasia, tumor genetics, presence or absence of metastasis TNM classification used for metastasis |
|
|
Colon Cancer Treatment |
Surgical removal Chemotherapy, radiation, or both |
|
|
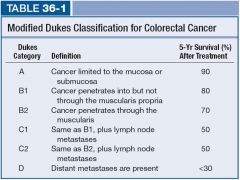
Modified Dukes Classification for Colorectal Cancer |
|

