![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
acrocyanosis
|
Cyanosis of the extremities
It is not a reliable indicator of hypoxemia May be an indicator of cold stress pallor may indicate decreased cardiac output severe anemia ,hypothermia ,acidosis or hypovolemia |
|
|
atresia
|
Absence of a normal opening
|
|
|
choanal atresia
|
Never rang or blockage of one or both nearest by membranous or bony tissue
If obstruction is limited to one side is called unilateral atresia if the obstruction is both sides is called bilateral atresia Infant is unable to feed and breathe at same time retractions may be seen unless the infant is breathing through the mouth or crying Interventions Open airway size and insert an oral airway its replaced by Mcgovern nipple at hospital. its a large nipple with d end cut |
|
|
cleft lip
|
Incomplete closure of the upper lip
More common in males |
|
|
cleft palate
|
Incomplete closure of the hard and or soft palate of the mouth
More common in females in pierre robin sequence it occurs because the infants tongue prevents the two sided of the palate from joining in the midline |
|
|
congenital
|
Present at or before birth
Minor birth defects include birthmarks skin tags an extra fingers or toes Major birth defect tracheoesophageal fistula, diaphragmic hernia and choanal atresia |
|
|
diaphragmic hernia
|
Protrusion of the abdominal contents into the chest cavity through an opening in the diaphragm
During early pregnancy a very small hole is normally present in the diaphragm of the fetus this hole usually closes by the end of the first trimester in case of a defect it allows some of the stomach, small intestine or even the spleen to invade the chest cavity those long are small because they had to share the space with abdominal contents in the chest cavity during fetal development Physical findings Little too severe respiratory distress. breath sounds are decreased , bowel sounds can be heard in the chest cyanosis may be present. does not improved despite ventilation the abdomen is usually flat(scaphoid) Interventions Patient is at high risk for developing pneumothorax if positive pressure ventilation is needed To avoid this complication perform tracheal intubation first if positive pressure is required place an oral gastric or nasogastric tube to deflate the stomach or intestines |
|
|
esophageal trasia ( EA )
|
Condition in wich the section of you esophagus from the mouth and a section of the esophagus from the stomach end as a blind pouch without connecting to each other
Physical findings Drooling often is accompanied by chocking coughing and sneezing the newborn swallows normally but oral secretions and feeding pool in the esophageal pouch cough when the fluid returns through nose and mouth also if you're unable to advance and orogastric or nasogastric tube into stomach |
|
|
fistula
|
And abnormal passage from a body organ to the body surface or between two internal body organs
|
|
|
hydrocephalus
|
And abnormal build-up of cerebrospinal fluid in the brain
|
|
|
meningocele
|
A type of SB in which the spinal cord develops normally but a sac like cyst that contains the meninges and cerebrospinal fluid protrudes from an opening in the spine usually in the lumbosacral area neurologic deficit are not usually present
|
|
|
meningomyelocele
|
The Severest form of SB in which the meninges cerebrospinal fluid and a portion of the spinal cord protrude from an opening in the spine and are in case in a sec cover by yourself in membrane also called my called myelomeningocele, neurologic deficits are usually present
Interventions Do not place a pation on their back position the infant on the side Watch for early signs of icp as hydrocephalus is commonly associated with this condition Cover the spinal defect with sterile gauze pads soak at all times in warm sterile normal saline cover with pladtic,keep patient warm |
|
|
Neonatal abstinence syndrome
|
Withdrawal symptoms that occur in newborns born to opiate addicted mothers
Simpsons usually begin within 48 a 72 hours after birth but may be delayed up to 2 weeks Signs include you eat ability jitters tremors rapid breathing modttling of the skin tachycardia cardio respiratory distress wheezing vomiting diarrhea and the hydration seizures may also result |
|
|
Neonate
|
And infant from birth to one month of age also called newborn
|
|
|
Neural tube defects
|
Congenital anomalities that involve incomplete development of the brain spinal cord and or their protective coverings
|
|
|
newborn asphyxia
|
The inability of a newborn to begin and continue breathing at birth
Examples of conditions that may occur in newborns who survived asphyxia at birth: Cerebral palsy mental retardation speaking hearing visual and learning disabilities |
|
|
Newly born
|
An infant in the first minutes to hours after birth
|
|
|
omphalocele
|
Protrusion of abdominal organs into the umbilical cord
The defect is usually covered by a sac of peritoneum the umbilical vessels are usually presentn within the sac Large cases include the stomach ,intestines ,liver and spleen And umbilical cord that looks you knew to be sent to be x_m in before clamping to make sure it is not a small omphalocele Rupture may occur immediately before or during delivery exposing the organs to a amniotic fluid resulting in intense inflammation Interventions position patient on their side cover exposed bowel with sterile gauze pads soaked at all times in warm normal saline cover with plastic to prevent loss of water and heat |
|
|
Pierre Robin sequence
|
A congenital anomaly characterized by a very small lower jaw (micognathia) a tongue that tends to fall back and downward
(glossoptosis) and cleft palate During week 7 to 11 of fetal development the mandible does not develop normally The shins are prone to airwaves truck shin intervention Verify airway is open if not size and insert an oral airway if airway is not open in urine able to insert an oral airway insert an oral gastric tube this will prevent the tongue from making a tight seal with the wall of the throat. Patients often have feeding problems and frequent ear infections caregivers may be instructed to nurse in a prone position allows the tongue to fall forward and keep the airway open |
|
|
Premature or preterm infant
|
Infant born before 37 complete weeks of gestation
Can be further classified according to their birth weight Low birth weight LBW 2500 grams 5.5 pounds Very low birth weight VLBW 1500 grams 3.3lbs or less Extremely low birth weight ELBW weighing less than 1000 grams |
|
|
Primary apnea
|
The newly born initial response to hypoxemia consisting of initial tachypnea then apnea, bradycardia and a slight increase in blood pressure is stimulated responds with resumption of breathing
|
|
|
Secondary apnea
|
When asphyxia is prolonged a period of gasping respirations with a simultaneous fall in blood pressure and heart rate gasping becomes weaker and slower and then ceases
You need to leave provide positive pressure ventilation The first sign of recovery after positive pressure ventilation is an increase in heart rate the blood pressure then rises and the skin becomes pink Bradycardia is almost always secondary to hypoxia has part changes in mental status |
|
|
Serious apnea
|
Cessation of breathing for longer than 20 seconds for any duration if accompanied by cyanosis and sinus bradycardia
Apnea in a newborn is usually caused by hypoxia or hypothermia Assessment may reveal newborn the doesn't breathe on his on after stimulation or the offend me have respiratory boss is that last more than 20 seconds if apnea is present bradycardia usually follows within 1 to 2 seconds |
|
|
spina bifida SB
|
a neural tube defect that affects the back portion of the vertebra which fail to close usually in need the area of the lower back; meningis, spinal cord or both may protrude thru this opening
This results during the first month of fetal development Folic acid is an important vitamin in fetal development defficiency of folic acid also called folate is believed to play a significant role in neural tube defects |
|
|
Spina bifida occulta
|
Mildest form of SB in which the spinal cord is intact but one or more their vertebrar fail to close in the lumbosacral area.
This time it's not you should be this awful and your loved that this is not typically present if prestons are limited too small temple in the lumbsacral area that is often associated with a tough hair |
|
|
thyrotoxicosis
|
A condition in which the thyroid gland produces excess thyroid hormone; also called hyperthyroidism or Graves disease
Instant usually has diarrhea tremors tachycardia and is very hungry |
|
|
Trachealesophageal fistula TEF
|
An abnormal opening between the trachea and esophagus
Fluid from the esophageal pouch or gastrointestinal secretions spill over into the trachea this results in cyanosis wheezing tachypnea and chemical pneumonitis Without EA may not have obvious symptoms at birth these babies may have chronic respiratory problems and or repeated episodes of pneumonia associated with feeding |
|
|
Vomiting
|
Forceful ejection of stomach contents through the mouth
|
|
|
paradoxic cyanosis
|
Cyanosis disappears when the infant cries and returns with rest
|
|
|
hypoglycemia
|
might develop in response to cold stress because the newborn rapidly uses glucose and glycogen reserves during anaerobic
metabolism signs and symptoms color changes respiratory distress apnea lethargy jitterness seizures |
|
|
suction interventions
|
careful not to insert suction catheter too far stimulation of the back of the throat can cause severe reflex bradycardia or apnea when performed within the first few minutes of delivery
if meconium stained fluid is present but newborn is vigorous ( strong ventilatory effort,good muscle tone heart rate >100 bpm) proceed with routine care. if newborn is depressed (the opposite from above) insert tracheal tube to suction apply as tube is slowly withdrawn repeat until little meconium is present. If heart rate or breathing is severely depressed positive pressure ventilation may be necessary despite the presence of some meconium in the airway |
|
|
Oxygen administration
|
Tissue damage may occur because of oxygen deprivation during and after asphyxia
Cell and tissue injury may increase if hypoxic tissue is exposed to high concentration oxygen the infant's heart rate is lower than 60 beats per minute after 90 seconds of resuscitation with a lower concentration of oxygen increase the oxygen concentration to 100 %until recovery of a normal heart rate Blow by oxygen should be set to deliver at least 5 liters per minute and held close to the face to maximize oxygen flow to nose and mouth do not administer high flow rates more than 10 liters per minute if its unheated or dehumidified because convective heat loss can become a problem |
|
|
term newborn vitals
|
Normal heart rate 100 to 180 beats per minute during the first 12 hours of life
Ventilatory rate 40 and 60 breaths per minute in the first 12 hours of life Heart rate greater than 100 beats per minute will need no further emergency care if heart rate is less than 100 beats per minute begin positive pressure ventilation I f heart rate less than 60 beats per minute indicates that additional resucitate measures are needed Cardiac output is almost exclusively dependent on heart rate cardiac output requirements of 500 m_l for minute yet only physically have 300 m_l of blood the only way to meet this requirements is to circulating very fast Clinical assessment of skin color is very poor indicator of oxy hemoglobin saturation during the immediate neonatal period and that lack of cyanosis appears to be a very poor indicator of the state of oxygenation of an uncompromise newborn following birth It is normal for the oxygen saturation level to remain in the 70% to 80% range for several minutes following birth with the appearance of cyanosis |
|
|
apgar score
|
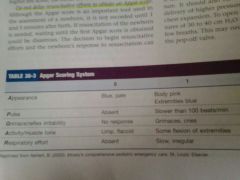
Numerical method of rating five specific signs pertaining to newborns condition after birth
its not recorded until 1 and 5 minutes after birth |
|
|
Ventilation
|
If bBM is required for more than 2 minutes consider placement of and or gastric tube to prevent respiratory compromise from gastric distention
Indications for positive pressure ventilation include apnea or gasping ventilations heart rate less than 100 beats per minute despite initial steps of estabilization Term newborn select bag with a minimum volume of 450 to 500 ml in a maximum volume of 750 ml Term newborn requires approximately 15 to 25 ml with each ventilation 528 ml per kilogram Preterm newborn requires less so much little as 5 to 10 ml per ventilation To open alveoli in a newborn pressures of 30 to 40 cm h2o may be needed during the first few breaths Ventilate newborn lungs at a rate of 40 to 60 breaths per minute to achieve or maintain a high rate of at least 100 beats per minute If newborn is are responsive to positive pressure ventilation and heart rate is less than 60 beats per minute continue positive pressure ventilation and begin chest compressions consider tracheal intubation |
|
|
bradycardia
|
Primary bradycardia is usually caused by structural heart disease
Secondary bradycardia it's a slow heart rate from a non-cardiac cause horses include increase vagal tone (parasympathetic) ( vomiting ICP suctioning or tracheal intubation procedure) hypothermia, hypothyroidism ,acidosis and hyperkalemia remember cardiac output= sttoke volume × heart rate Hypoxia is the most common cause of bradycardia in newborns infants and children correcting the hypoxia (if present) should increase the heart rate |
|
|
seizures
|

hypixic ischemia encephalopathy (most common cause)
icp meningitis drug withdrawal development abnormalities cns malformation metabolic disturbances ( hypoglycemia hypocalcemia, hypimagnesimia, pyridoxine deficiency) |
|
|
fever
|
newborn average normal temperature is 37.5 degrees celsius 99.5 degrees fahrenheit. fevers present if the rectal temperature is 38.0 celsius 100.4 fahrenheit or higher
Term infants who has a fever will have beads of sweat on the brow but usually not over the rest of the body Preterm infants will have no visible sweat To maintain normal body temperature of the newborn uses more glucose when blue color is depleted anaerobic metabolism results Infants in the first three months of life have an immature immune system |
|
|
hypothermia
|
body temperature be low 35 degrees celsius 95 degrees fahrenheit the whistle degrees and he production an increase in heat loss for a combination of these factors
It can be a sign of sepsis |
|
|
hypoglycemia
|
Hypoglycemia in a newborn is a blood glucose level of less than 40 mg/dl prolong low blood glucose levels can lead to irreversible brain damage
Newborns glycogen stores are adequate to meet glucose requirements for only 8 to 12 hours By 3 hours of life the glucose level rises to 50 to 80 mg DL I probably see me and mia car as early as 30 to 6 minutes of the birth and children of diabetic mother |
|
|
vomiting
|
My meeting in the first 24 hours of life just obstruction in the upper digestive trac pyloric stenosis or icp
Vomiting of non bile stain fluid suggest an anatomical or functional obstruction at or above the first portion of the duodenum or gastro esophageal reflux Vomiting of bile stain fluid suggests an obstruction below the opening of the bile duct |
|
|
diarrhea
|

|
|
|
brachial plexus injury
|
Peripheral nerve injury can occur when nerve roots are stretch during delivery this can occur when shoulder dystocia is present
|

