![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
Gall bladder lies between what segements of the liver?
|
segments IV and V
|
|
|
Cystic artery branches off what artery?
|
right hepatic artery
|
|
|
Describe the triangle of Calot.
|
cystic duct lateral
common bile duct medial liver superior |
|
|
Arteries that supply the hepatic and common bile duct (9- and 3-o'clock positions
when performing ERCP); considered longitudinal blood supply |
Right hepatic (lateral) Retroduodenal branches of the gastroduodenal artery
(medial) |
|
|
Where do the cystic veins drain?
|
into the right branch of the portal vein and in to the liver
|
|
|
Location of lymphatic in relation to the CBD
|
Lymphatics are on the right side of the common bile duct
|
|
|
Parasympathetic and sympathetic fibers to the biliary system.
|
Parasympathetic fibers from left (anterior) trunk of the vagus
Sympathetic fibers from T7- T10 coursing through the splanchnic and celiac ganglions |
|
|
What layer is the gallbladder missing?
|
submucosa
|
|
|
What part of the billiary system has no peristalsis?
|
Common bile duct
hepatic duct |
|
|
Gallbladder normally fills by?
|
contraction of sphincter of Oddi at the ampulla of Vater
|
|
|
Normal sizes:
1. CBD 2. GB wall 3. Pancreatic duct |
1. CBD < 8 mm ( < 10 mm after cholecystectomy)
2. GB wall < 4 mm 3. Pancreatic duct < 4 mm |
|
|
Location of the Highest concentration of CCK and secretin cells
|
Duodenum
|
|
|
Def: invagination of the epithelium of the wall of the gall bladder; formed from increased gallbladder pressure
|
Rokitansky-Aschoff sinuses
|
|
|
biliary ducts that can leak after a cholecystectomy
|
Ducts of Luschka
|
|
|
Causes Increased bile excretion
|
CCK, secretin, and vagal input
|
|
|
Causes decreased bile excretion
|
VIP, somatostatin, sympathetic stimulation
|
|
|
Essential functions of bile
|
• Fat-soluble vitamin absorption
• Bilirubin excretion • Cholesterol excretion |
|
|
How does the GB concentrate bile?
|
active resorption of Na and water
|
|
|
Active resorption of conjugated bile acids occurs in the ________.
|
Terminal ileum (50%)
|
|
|
Where is Bile secreted from?
|
bile canalicular cells (20%) hepatocytes (80%)
|
|
|
Def: breakdown product of conjugated bilirubin in gut; gives stool brown color
|
Stercobilin
|
|
|
Def: breakdown product of conjugated bilirubin in gut; yellow; some gets reabsorbed and released in urine
|
Urobilin
|
|
|
Rate limiting step in cholesterol synthesis
|
HMG CoA reductase
|
|
|
Stones in obese people
|
overactive HMG CoA reductase
|
|
|
Stones in thin people -
|
underactive 7-alpha-hydroxylase
|
|
|
Name the type of stone. increased cholesterol insolubilization, decreased lecithin and bile acids,
Increased water reabsorption, caused by stasis |
Nonpigmented stones
Most common type of stone found in the United States |
|
|
Name the type of stone.
most common worldwide Caused by solubilization of unconjugated bilirubin with precipitation of calcium bilirubinate and insoluble salts |
Pigmented stones
Dissolution agents do not work on pigmented stones (monooctanoin) |
|
|
Name the type of stone.
• Can be caused by hemolytic disorders or cirrhosis • Can also occur in patients on chronic TPN and in patients with ileal resection • Important factors for the development of these stones - increased bilirubin load, decreased hepatic function, and bile stasis • Almost always form in gallbladder |
Black stones
• Tx: cholecystectomy |
|
|
Name the type of stone.
Infection causing deconjugation of bilirubin • Increased in Asians • E. coli most common - produces beta-glucuronidase, which deconjugates bilirubin, causes formation of calcium bilirubinate • Need to check for ampullary stenosis, duodenal diverticula, abnormal sphincter of Oddi • primary common bile duct stones • Almost all patients with primary stones need a biliary drainage procedure sphincteroplasty 90% successful |
Brown stones
|
|
|
Define secondary
common bile duct stones |
Cholesterol stones and black stones found in the CBD are considered secondary
common bile duct stones |
|
|
associated with frank purulence in the gallbladder can be associated with sepsis and shock
|
Suppurative cholecystitis
|
|
|
Most common organisms in cholecystitis
|
E. coli, Klebsiella, Enterococcus
|
|
|
Caused by obstruction of the cystic duct by a gallstone
• Results in gallbladder wall distention and wall inflammation |
CHOLECYSTITIS
|
|
|
List Stone risk factors
|
age >40, female, obesity, pregnancy, rapid weight loss,
vagotomy, TPN ( pigmented stones), ileal resection ( pigmented stones) |
|
|
What is the usual route for Bacterial infection of bile?
|
dissemination from portal system is usual route
|
|
|
Type of cholecystitis
• Thickened wall, RUQ pain, increased WBCs • Occurs most commonly after severe burns, prolonged TPN, trauma, or major surgery • Primary pathology is bile stasis (narcotics, fasting), leading to distention and ischemia • Also have increased viscosity secondary to dehydration, ileus, transfusions • US shows sludge, gallbladder wall thickening, and pericholecystic fluid |
ACALCULOUS CHOLECYSTITIS
|
|
|
• Can see on plain film
• Increased in diabetics; usually secondary to Clostridium perfringens • Symptoms: severe, rapid-onset abdominal pain, nausea, vomiting, and sepsis • Perforation more common in these patients |
EMPHYSEMATOUS GALLBLADDER DISEASE
• Gas in the gallbladder wall |
|
|
Fistula between gallbladder and duodenum that releases stone, causing small bowel
obstruction; elderly • Can see pneumobilia (air in the biliary system) on plain film • Terminal ileum - most common site of obstruction |
GALLSTONE ILEUS
|
|
|
When can you perform a primary repair for a CBD injury?
|
if < 5O% the circumference of the common bile duct,
in all other cases, will likely need hepaticojejunostomy or choledochojejunostomy |
|
|
most important cause of late postoperative biliary strictures
|
Ischemia
• Tx: ERCP with sphincterotomy and possible stent placement to decompress; PTC tube if that fails |
|
|
How would you Dx & Tx
• Patients classically present with UGI bleed, jaundice, and RUQ pain • Most commonly occurs with trauma ( 50% of all cases), infections, primary gallstones, aneurysms, and tumors |
HEMOBILIA
Dx angiogram Tx: resuscitation ; angiogram and embolization 1st; operation if that fails |
|
|
most common cancer of the biliary tract
Four times more common than bile duct CA; most have stones Liver - most common site of metastasis |
GALLBLADDER ADENOCARCINOMA
|
|
|
GALLBLADDER ADENOCARCINOMA first spreads to what part of the liver?
|
segments IV and V; 1st nodes are the cystic duct nodes (right side)
|
|
|
Risk of gallbladder CA in patients with Porcelain gallbladder these patients need
cholecystectomy |
10%-20%
|
|
|
Tumor Stages of GB CA
|
T1:invades lamina propria or muscular layer
T2:invades perimuscular connective tissue; no extension beyond serosa or into liver T3:Tumor perforates the serosa (visceral peritoneum) and/or directly invades the liver and/or one other adjacent organ or structure T4: invades main portal vein or hepatic artery or invades two or more extrahepatic organs or structures |
|
|
What percentage of patients present with stage IV GB Ca
|
90%
|
|
|
Name the cancer.
Occurs in elderly; males Risk factors: C. sinensis infection, typhoid, ulcerative colitis, choledochal cysts, sclerosing cholangitis, congenital hepatic fibrosis, chronic bile duct infection Sx: early - painless jaundice most common; can also get cholangitis; late -weight loss, anemia, pruritus Persistent increase in bilirubin and alkaline phosphatase |
BILE DUCT CANCER (CHOLANGIOCARCINOMA)
|
|
|
most common type of CHOLANGIOCARCINOMA
worst prognosis, |
Klatskin tumors - Carcinoma of the hepatic duct bifurcation
Tx: can try lobectomy and stenting of contralateral bile duct if localized t o either the right or left lobe |
|
|
CHOLANGIOCARCINOMA
Middle 1/3 - Lower 1/3 - Palliative stenting for unresectable disease • Overa l l 5-year s u rvival rate - 2 0% |
Middle 1/3- hepaticojejunostomy
Lower 1/3 - Whipple |
|
|
Most common type of CHOLEDOCHAL CYSTS.
|
type I - fusiform or saccular dilatation of extrahepatic ducts
|
|
|
Treatment of CHOLEDOCHAL CYSTS
|
• Tx: cyst excision with hepaticojejunostomy and cholecystectomy
• Type IV cysts are partially intrahepatic, and type V (Caroli' s disease) are totally intrahepatic will need partial liver resection |
|
|
Name the disease
• Men in 4th-5th decade • Can be associated with retroperitoneal fibrosis, Riedel's thyroiditis, pancreatitis, ulcerative colitis, and DM • Symptoms: fatigue, fluctuating jaundice, pruritus, weight loss, RUQ pain • Pruritus caused by bile acids • Dx: ERCP - multiple strictures and dilatations |
PRIMARY SCLEROSING CHOLANGITIS
|
|
|
TX for PRIMARY SCLEROSING CHOLANGITIS
|
• Tx: TXP needed long term for most; PTC tube drainage, choledochojejunostomy may
be effective for some; balloon dilatation of dominant strictures may provide some symptomatic relief • Cholestyramine - can decrease pruritus symptoms (decreased bile acids) • UDCA (urodeoxycholic acid ) - can decrease symptoms ( decrease bile acids) and improve liver enzymes |
|
|
Name the disease
• Women; medium -sized hepatic ducts • Cholestasis> cirrhosis>portal hypertension • Symptoms: fatigue, pruritus, jaundice, xanthomas • Antimitochondrial antibodies • No increased risk for cancer • Tx: TXP |
PRIMARY BILIARY CIRRHOSIS
|
|
|
Charcot's triad
|
RUQ pain, fever, jaundice
|
|
|
Reynolds' pentad
|
Charcot's triad plus mental status changes and shock (suggests sepsis)
|
|
|
most common organisms in CHOLANGITIS
|
E.coli and Klebsiella
|
|
|
Cholovenous reflux occurs at what pressure?
|
20 mmHg pressure > systemic bacteremia
|
|
|
#1 serious complication; related to sepsis with CHOLANGITIS
|
Renal failure
|
|
|
• Asia; recurrent cholangitis from primary CBD stones
• Caused by C. sinensis, A. lumbricoides, T trichiura, and E. coli infections • Tx: hepaticojejunostomy and antiparasitic medications |
ORIENTAL CHOLANGIOHEPATITIS
|
|
|
The causes of SHOCK FOLLOWING LAPAROSCOPIC CHOLECYSTECTOMY
Early (1st 24 hours) Late (after 1st 24 hours) |
Early (1st 24 hours)hemorrhagic shock from clip that fell off cystic artery
Late (after 1st 24 hours)septic shock from accidental clip on CBD with subsequent cholangitis |
|
|
• thickened nodule of mucosa and muscle associated with
Rokitansky-Aschoff sinus • Not premalignant; does not cause stones, can cause RUQ pain • Tx: cholecystectomy |
Adenomyomatosis
|
|
|
• benign neuroectoderm tumor of gallbladder
• Can occur in biliary tract with signs of cholecystitis • Tx: cholecystectomy |
Granular cell myoblastoma
|
|
|
Def: speckled cholesterol deposits on the gallbladder wall
|
Cholesterolosis
|
|
|
Gallbladder polyps when should you worry about malignancy
|
> 1 cm, worry about malignancy
|
|
|
Def: bound to albumin covalently, half-life of 18 days; may take a while to clear after long-standing jaundice
|
Delta bilirubin
|
|
|
Def: compression of the common hepatic duct by a stone in the infundibulum of the gallbladder or inflammation arising from the gallbladder or cystic duct extending to the contiguous hepatic duct, causing stricture and hepatic duct obstruction
|
Mirizzi syndrome
|
|
|
Abx that can cause gallbladder sludging and cholestatic jaundice
|
Ceftriaxone
|
|
|
Indications for asymptomatic cholecystectomy
|
in patients undergoing l iver TXP or gastric bypass procedure
|
|
|
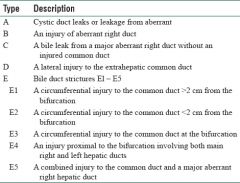
List the classification for CBD injuries |
|
|
|
What is the MC site of obstruction for gallstone ileus? |
terminal ileum |
|
|
Treatment of Bile Duct Ca |
|
|
|
GB adenocarcinoma TX T1 and T2 |
Stage 1a- T1 confined to mucosa + lamina propria TX: Cholecystectomy Stage 1b- T2 muscle invasion only TX: Wedge resection of segments IV and V w/ 2-3 cm margins and striping of portal triad LN
|
|
|
GB adenocarcinoma TX T3 and T4
|
Stage 2a- beyond muscle but resectable TX: Formal resection of segments IV and V w/ 2-3 cm margins, striping of portal triad LN, possible hepatico-Jejunostomy |

