![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back
|
Name five functions of the peripheral circulatory system.
|
1) Carry blood
2) Exchange nutrients 3) Transport 4) Regulate blood pressure 5) Direct blood flow |
|
|
Endothelium
|
the innermost lining of blood vessels;
composed of simple squamous epithelial cells, continuous with the endocardium of the heart |
|
|
Pericapillary cells
|
cells scattered throughout the length of the blood vessel, associated with the endothelial cells;
generally fibroblasts, macrophages, or undifferentiated smooth muscle cells |
|
|
Continuous capillaries
|
approx. 7-9 micrometers in diameter and their walls exhibit no gaps between the endothelial cells;
less permeable to large molecules than other vessels; found in muscle, nervous, and other tissues |
|
|
Fenestrated capillaries
|
endothelial cells with numerous fenestrae;
found in tissues where capillaries are highly permeable |
|
|
Fenestrae
|
areas approximately 70-100 nm in diameter in which the cytoplasm is absent and the plasma membrane consists of a porous diaphragm that's thinner than the nromal plasma membrane
|
|
|
Sinusoidal capillaries
|
larger in diameter than either continuous or fenestrated capillaries, and basement membrane is less prominent;
occur in such places as endocrine glands, where large molecules cross their walls |
|
|
Sinusoids
|
large-diameter sinusoidal capillaries;
structure suggests that large molecules and sometimes cells can move readily across their walls between the endothelial cells; common in liver and bone marrow |
|
|
Venous sinuses
|
similar in structure to the sinusoidal capillaries but are larger in diameter;
occur primarily in the spleen, and they have large gaps between the endothelial cells that make up their walls |
|
|
Arterial capillaries
|
the ends of capillaries closest to the arterioles
|
|
|
Venous capillaries
|
ends of capillaries closes to the venules
|
|
|
Metarterioles
|
vessel through which blood flows from arterioles into a thoroughfare channel;
have isolated smooth muscle cells along their walls |
|
|
Thoroughfare channel
|
a vessel that extends in a relatively direct fashion from a metarteriole to a venule, capillaries branch off of thoroughfare channel;
blood flow through thoroughfare is usually continuous |
|
|
Precapillary sphincters
|
smooth muscle cells located at the origin of capillary branches that regulate the flow of blood through the capillaries
|
|
|
Tunica intima
|
the inner layer of a blood vessel wall;
consists of endothelium, a delicate connective tissue membrane, a thin layer of connective tissue (lamina propria), and the internal elastic membrane |
|
|
Internal elastic membrane
|
a fenestrated layer of elastic fibers that separates the tunica intima from the tunica media
|
|
|
Tunic media
|
the middle layer of a blood vessel wall;
consists of smooth muscles cells arranged circularly around the blood vessel, and variable amounts of elastic and collagen fibers, as well as an external elastic membrane; smooth muscle in this layer helps regulate blood flow through vasomotion |
|
|
Vasoconstriction
|
a decrease in blood vessel diameter caused by smooth muscle contraction;
results in a decrease of blood flow |
|
|
Vasodilation
|
an increase in blood vessel diameter because of smooth muscle relaxation ;
results in an increase of blood flow through the vessel |
|
|
External elastic membrane
|
a fenestrated layer of elastic fibers which separates the tunica media from the tunica adventitia
|
|
|
Tunica adventitia
|
the outer layer of a blood vessel wall;
composed of connective tissue of varying thickness |
|
|
Elastic arteries
|
blood vessels with the largest diameter, relatively high pressure and a greater amount of elastic tissue and less smooth muscle tissue
|
|
|
Medium arteries
|
include most of the smaller unnamed arteries;
walls are relatively thick compared to their diameter; large numbers of smooth muscle cells that allow these vessels to partially regulate blood supply to different regions of the body |
|
|
Arterioles
|
vessels that transport blood from small arteries to capillaries;
the smallest arteries in which the three tunics can be identified; capable of vasodilation and vasoconstriction |
|
|
Venules
|
vessels composed of endothelium resting on a delicate basement membrane;
|
|
|
Small veins
|
veinous vessels in which a continuous layer of smooth muscle surrounds the vessel, and a tunica adventitia composed of collagenous connective tissue
|
|
|
Medium veins
|
collect blood from small veins and deliver it to large veins;
|
|
|
Large veins
|
transport blood from the medium veins to the heart;
tunica intima is thin and composed of endothelial cells, a thin layer of collagenous connective tissue, and a few scattered elastic fibers |
|
|
Valves
|
present in veins with a diameter greater than 2 mm;
allow blood to flow toward the heart but not in the opposite direction; consist of folds in the tunica intima that form two flaps that are shaped and function like the semilunar valves of the heart |
|
|
Vasa vasorum
|
small blood vessels that supply nutrients to thick blood vessel walls by penetrating from the exterior of the vessel and forming a capillary network in the tunica adventitia and the tunica media
|
|
|
Arteriovenous anastomoses
|
allow blood to flow from arterioles to small veins without passing through capillaries;
present in large numbers in soles of feet, palms, terminal phalanges, and nail beds; function in temperature regulation |
|
|
Glomus
|
an arteriovenous anastomosis that consists of arterioles arranged in a convoluted fashio surrounded by collagenous connective tissue
|
|
|
Pathologic arteriovenous anastomoses
|
can result from injury or tumors;
can cause direct flow of blood from arteries to veins, and if sufficiently large, lead to heart failure because of tremendous venous return to the heart |
|
|
Portal veins
|
veins that begin in a primary capillary network, extend some distance and end in a secondary capillary network;
two portal vein systems in humans, the hepatic and hypothalamohypophyseal portal systems |
|
|
Arteriosclerosis
|
a term used to describe degenerative changes in arteries that make them less elastic
|
|
|
Atherosclerosis
|
refers to the deposition of material in the walls of arteries to form plaques
|
|
|
Laminar flow
|
flow in a streamlined fashion, with the outer layers of blood flowing more slowly and the innermost layers flowing the fastest
|
|
|
Turbulent flow
|
results when the rate of flow exceeds a critical velocity or when the fluid passes a constriction, a sharp turn, or a rough surface;
occurs primarily in the heart and to a lesser extent where arteries branch |
|
|
Blood pressure
|
a measure of the force blood exerts against blood vessel walls
|
|
|
Cannula
|
a tube used to measure blood pressure by placing it into a blood vessel and connecting it to a manometer or an electronic pressure transducer
|
|
|
Auscultatory method
|
used to measure blood pressure without surgical procedures or causing discomfort;
used under most clinical conditions |
|
|
Korotkoff sounds
|
vibrations produced by turbulent blood flow during systolic surges of blood through a constricted vessel that can be heard through a stethoscope
|
|
|
Systolic pressure
|
the pressure at which Korotkoff sounds can first be heard
|
|
|
Diastolic pressure
|
the pressure at which continuous laminar blood flow is reestablished and Korotkoff sounds can no longer be heard
|
|
|
Rate
|
the volume that passes a specifc point per unit time, usually measured in L/min
|
|
|
Mathematically describe the rate of blood flow
|
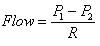
P1 and P2 are the pressures in the vessel at points one and two, respectively, and R is the resistance to flow
|
|
|
Viscosity
|
a measure of the resistnace of a liquid to flow;
as viscosity increases, the pressure required to force it to flow increases; when above its normal range, increases the workload of the heart and can result in heart failure |
|
|
Hematocrit
|
the percentage of the total blood volume composed of red blood cells;
as the hematocrit increases, the viscosity of blood increases logarithmically |
|
|
Critical closing pressure
|
the pressure, specific to each vessel, below which the vessel collapses and blood flow through the vessel stops;
during shock, if blood pressure decreases below this value, the vessel will collapse |
|
|
Laplace's law
|
states that the force that stretches the vascular wall is proportional to the diameter of the vessel times the blood pressure;
|
|
|
Aneurysm
|
a bulge of the vascular wall in weakened blood vessels;
in danger of rupturing |
|
|
Compliance
|
the tendency for blood vessel volume to increase as the blood pressure increases;
the more easily a vessel stretches, the greater is its compliance, the less easily is stretches, the smaller is its compliance |
|
|
Pulse pressure
|
the difference between systolic and diastolic pressures;
about 40 mm Hg; stroke volume of the heart and vascular compliance both affect pulse pressure |
|
|
Capillary exchange
|
the movement of substances into and out of capillaries;
the process by which cells receive everything they need to survive and to eliminate metabolic waste products; must be maintained for cells to survive |
|
|
Diffusion
|
the passive movement of substances from a high concentration to a lower concentration;
primary method of capillary exchange |
|
|
Net filtration pressure (NFP)
|
the force responsible for moving fluid across capillary walls;
the difference between net hydrostatic pressure and net osmotic pressure; 13 mm Hg at arterial end of capillary; -7 mm Hg at venous end of capillary |
|
|
Net hydrostatic pressure
|
the difference in pressure between the blood and interstitial fluid
|
|
|
Interstital fluid pressure
|
the pressure of interstitial fluid within tissue spaces;
negative because of the suction effect of excess fluids being pulled from the interstital spaces by lymphatic vessels |
|
|
Net osmotic pressure
|
the difference in osmotic pressure between the blood and the interstital fluid
|
|
|
Blood colloid osmotic pressure (BCOP)
|
the osmotic pressure caused by the plasma proteins;
several times larger than the ICOP; remains relatively constant across capillary bed |
|
|
Interstitial colloid osmotic pressure (ICOP)
|
the osmotic pressure caused by proteins in the interstitial spaces
|
|
|
Venous tone
|
a contiual state of partial contraction of the veins as a result of sympathetic stimulation; increased sympathetic stimulation increases venous tone; decreased sympathetic stimulation decreases venous tone
|
|
|
Vasodilator substances
|
chemicals such as carbon dioxide, lactic acid, adenosine, AMP, ADP, K+, H+ that are produced as metabolism increases, diffuse from the tissues supplied by the capillary to the areas of the precapillary sphincter, the metarterioles, and the arterioles, to cause vasodilation
|
|
|
Vasomotion
|
periodic contraction and relaxation of the precapillary sphincters in response to conc. of nutrients in the interstitial fluid;
results in a cyclic blood flow through capillaries |
|
|
Autoregulation
|
the maintenance of blood flow by tissues; mechanisms operate in response to conc. of nutrients in the interstitial fluid;
utilizes same mechanisms as vasomotion |
|
|
Vasomotor center
|
an area of the lower pons and upper medulla oblongata that is tonically active and contributes to vasomotor tone;
can be stimulated or inhibited by areas throughout the brain |
|
|
Vasomotor tone
|
a condition of constant partial constriction;
produced in response to tonic stimulation from the vasomotor center |
|
|
Chemoreceptor reflex
|
a relfex that helps maintain homeostasis when oxygen tension in the blood decreases or when carbon dioxide and hydrogen ion conc. increase;
chemoreceptors found in the carotid and aortic bodies produce afferent APs that travel to the medulla and result in increased vasomotor tone |
|
|
Central nervous system ischemic response
|
elevation of blood pressure in response to a lack of blood flow to the medulla oblongata;
functions in response to emergency situations in which blood flow to the brain is severely restricted |
|
|
Renin-angiotensin-aldosterone mechanism
|
a long-term blood pressure regulatory system that helps regulate kidney function and can also influence peripheral resistance by causing vasoconstriction
|
|
|
Renin
|
an enzyme released by the kidneys into the circulatory system;
acts angiotensinogen to split a fragment off of one end |
|
|
Angiotensinogen
|
a plasma protein produced by the liver which is acted on by renin to produce angiotensin I
|
|
|
Angiotensin I
|
a fragment cleaved off of angiotensinogen by renin;
a protein that is about 10 amino acids long |
|
|
Angiotensin-converting enzyme
|
an enzyme found primarily in small blood vessels of the lung;
cleaves two additional amino acids from angiotensin I to produce angiotensin II |
|
|
Angiotensin II (active angiotensin)
|
a fragment of angiotensin I that has been cleaved by ACE to produce an 8 amino acid fragment;
causes vasoconstriction in arterioles and to some degree in veins, thereby increasing PR and venous return to the heart, raising blood pressure; also stimulates aldosterone release from the adrenal cortex; also increases salt appetite, thirst, and ADH secretion |
|
|
Aldosterone
|
a mineralocorticoid released from the adrenal cortex that acts on kidneys to increase the reabsorption of Na+ and Cl- from the filtrate into the extracellular fluid;
with ADH, dereases urine production, raising blood volume and pressure |
|
|
Vasopressin mechanism
|
a blood pressure regulatory mechanism that works in harmony with the renin-angiotensin-aldosterone mechanism in response to changes in blood pressure;
decreases in blood pressure detected by baroreceptors results in ADH seretion by post. pit.; ADH acts directly on blood vessels to cause vasoconstriction |
|
|
Atrial natriuretic hormone
|
a polypeptide hormone that is released from cells in the atria of the heart in resposne to increased venous return, stretching cardiac muscle cells;
acts on kidneys to increase the rate of urine production and Na+ in the urine, causing blood volume and venous return and vasodilation decreases PR |
|
|
Fluid shift mechanism
|
a blood pressure regulatory mechanism that occurs in response to small changes in pressures across capillary walls, allowing fluid to move to and from interstitial spaces;
begins to act within a few minutes but requires hours to achieve its full functinoal capacity |
|
|
Stress-relaxation response
|
a response characteristic of smooth muscle cells; in which dereases of blood volume cause a decrease in the force applied to the vessel by the blood, the vessel responds by contracting to decrease vessel volume and maintain blood pressure
|

