![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
ICA branches |
Ophthalmic Artery and posterior communicating artery |
|
|
ICA terminates |
In middle cerebral artery and anterior cerebral artery |
|
|
ECA branches |
8 major branches 1st superior thyroid artery Facial artery, superficial temporal artery |
|
|
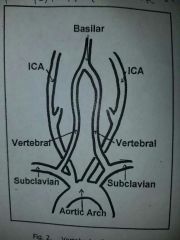
Vertebral Arteries form |
Basilar artery |
|
|
Basilar artery divides inti |
Posterior cerebral arteries |
|
|
Circle of Willis |
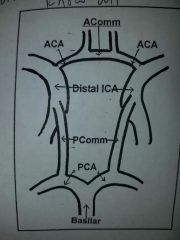
Largest intra-arterial connection |
|
|
Vertebrobasilar system |
|
|
|
Supraorbital artery arises from |
Ophthalmic Artery and joins with ECA via some of it's branches |
|
|
Frontal artery arises from |
Ophthalmic Artery; exits orbits medially to supply mid forehead;joins ECA via some of its branches |
|
|
Anastomoses include |
ECA-ICA via orbital and ophthalmic arteries Occipital branch of ECA w/ Atlantic branch of vertebral |
|
|
Bernoulli principle |
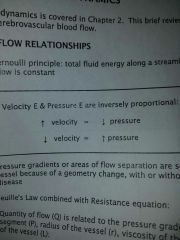
Total fluid energy along a streamline of fluid flow is constant |
|
|
Transient ischemic attack |
Fleeting neurological dysfunction;symptoms last <24 hrs;usually embolic from heart or carotid artery |
|
|
Resolving ischemic neurologic deficit |
(RIND) symptoms last >24hrs; complete recover usually occurs |
|
|
Cerebrovascular accident |
(CVA) symptoms last >24hrs; complete recovery does not occur |
|
|
Atheromatous |
Form of arteriosclerosis; localized accumulations |
|
|
Types of atheromatous |
Fatty streak:thin layer in intimal Fibrous plaque Complicated lesion Ulcerative lesion: deterioration of normally smooth surface; may result in emboli Intra-plaque hemorrhage: sonolucent area w/in plaque |
|
|
Types of atheromatous |
Fatty streak:thin layer in intimal Fibrous plaque Complicated lesion Ulcerative lesion: deterioration of normally smooth surface; may result in emboli Intra-plaque hemorrhage: sonolucent area w/in plaque |
|
|
Thromboembolic |
Obstruction of blood vessel by piece of thrombus |
|
|
Thrombus |
Large amounts of RBC's trapped w/in fibrin network |
|
|
Embolism |
Piece of thrombus breaks loose and travels distally until lodges in small vessel |
|
|
Aneurysm |
Localized dilation of blood vessel due to congenital defects or weakness of wall (trauma, infection or atherosclerosis) |
|
|
Dissection |
Results from sudden tear in intima; creates false lumen |
|
|
Fibromuscular dysplasia |
(FMD) most commonly caused by dysplasia of media along w/ overgrowth of collagen in mid/dist ICA; bead like appearance;often seen in young women |
|
|
Neointimal hyperplasia |
Intimal thickening from rapid production of smooth muscle cells; response to vascular injury/reconstruction (endarterectomy);significant stenosis may occur w/in 6-24 months |
|
|
Symptoms w/ ICA lesions |
Unilateral paresis, unilateral paresthesia, aphasia, amaurosis fugax |
|
|
Symptoms w/ MCA lesions |
Aphasia or dysphasia, more severe facial and arm hemiparesis or hemiplegia, behavioral changes |
|
|
Symptoms w/ ACA lesions |
More severe leg hemiparesis or hemiplegia, incontinence, loss of coordination |
|
|
Paresis |
Weakness or slight paralysis on one side of body |
|
|
Paresthesia |
Prickling or tingling of skin |
|
|
Aphasia |
Inability to speak |
|
|
Amaurosis fugax |
Temporary, partial or total blindness usually of one eye |
|
|
Dysphasia |
Impairment of ability to communicate |
|
|
Hemiparesis |
Weakness on one side of body |
|
|
Hemiplegia |
Paralysis on one side of body |
|
|
Symptoms w/ vertebrobasilar lesion |
Vertigo, ataxia, bilateral visual blurring or double vision, bilateral paresthesia or anesthesia, drop attack |
|
|
Symptoms w/ PCA lesion |
Dyslexia, coma |
|
|
Ataxia |
Muscular uncoordination |
|
|
ICA Doppler signal |
High pitched and continuous; rapid upstroke and down stroke with high diastolic component |
|
|
ECA doppler signal |
Pulsatile; rapid upstroke and down stroke with low flow diastole, dicrotic notch |
|
|
50-79% stenosis |
PSV >125 EDV <140 |
|
|
80-99% stenosis |
PSV >125 EDV >140 |
|
|
Surgery w/ ICA/CCA ratio |
>4 |
|
|
Criteria determining occlusion |
CCA mat have very low or absent diastolic flow; evidence of collateralization (ECA exhibit high flow in end diastole); absent ICA Doppler signal or pre-occlusive thump |
|
|
Ways to increase PRF/Nyquist limit |
Decrease baseline; increase scale; change frequency; alter angle; decrease depth; use CW |
|
|
Mirror imaging |
Doppler shifts above and below baseline; turn down gain or change angle of isonation |
|
|
Helical Flow |
Occurs when Flow moves into wider portion of vessel; Doppler shifts above and below baseline; spectral broadening present |
|
|
Intraoperative monitoring |
Identify defects secondary to surgery or areas of platelet aggregation; use >12 MHz transducer |
|
|
If flow in ACA is antegrade |
Getting flow from anterior communicating artery |
|
|
If increased flow in PCA |
Reversing direction of flow in posterior communicating artery |
|
|
Temporal arteritis |
Inflammation of arterial wall |
|
|
Calculating diameter reduction |
(1-(d/D)x100=% |

