![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
Wound
|
Any injury to the bodys tissue involving a break in the skin.
|
|
|
Nursing focus during postsurgical recovery phase
|
Promote wound healing
|
|
|
Wound classifications derive from
|
Derive from their cause, the severity of injury, amount of contamination, skins integrity
|
|
|
Incision
|
Cut produced surgically creating an opening into an organ
|
|
|
Puncture
|
Stab wound for a drainage system
|
|
|
Classifications of wounds
|
Clean wound
Clean contaminated Contaminated Dirty or infected wounds |
|
|
Four phases of wound healing
|
Hemostasis
Inflammatory phase Reconstruction Maturation |
|
|
Hemostasis
|
Termination of bleeding
|
|
|
What happens during the hemostasis phase
|
Fibrin in the clot begins to hold the wound together, and bleeding subsides.
|
|
|
What happens during the inflammatory phase
|
Initial increase in the flow of blood elements. This process causes cardinal signs and symptoms of inflammation: erythema, heat, edema, pain, and tissue dysfunction
|
|
|
During what phase do cells in the injured tissue migrate divide and form new cells
|
Inflammatory phase
|
|
|
Collagen formation occurs during what phase
|
Reconstruction
|
|
|
During the reconstruction phase, encourage patients to consume foods rich in
|
Protein & vitamin A & C
|
|
|
Wound dehiscence most frequently occurs during which phase?
|
Reconstruction
|
|
|
Keloid
|
Overgrowth of collageneous scar tissue at the site of a wound
|
|
|
Keloids form during which phase
|
Maturation
|
|
|
Keloids color range from
|
Red to pink to white
|
|
|
Primary intention
|
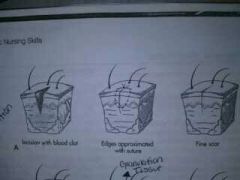
Skin edges close together and little tissue is lost. Minimal scarring. Healing begins during inflammatory phase
|
|
|
Granulation tissue
|
Soft, pink, fleshy projections consisting of capillaries surrounded by fibrous collagen
|
|
|
Tertiary intention
|
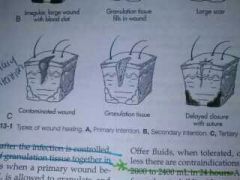
Contaminated wound left open and surgeon closes it later after infection is controlled.
|
|
|
Serous
|
Clear, watery plasma
|
|
|
Purulent
|
Thick, yellow, green, tan or brown
|
|
|
Serosanguineous
|
Pale, red, watery. Mixture of serous and sanguineous
|
|
|
Sanguineous
|
Bright red: indicates active bleeding
|
|
|
Phagocytosis
|
Cells engulf and dispose of microorganisms
|
|
|
Gauze dressings
|
Permit air to reach the wound
|
|
|
Semiocclusive dressings
|
Permit oxygen but not air impurities to pass
|
|
|
Occlusive dressing
|
Permit neither air nor oxygen to pass
|
|
|
Who does the initial dressing change?
|
Physician or surgeon
|
|
|
Dry dressing
|
Choice for management of a wound with little exudate or drainage
|
|
|
Does dry dressings debride the wound?
|
No. Not the proper selection for wounds requiring debridement
|
|
|
Because removal of a dressing can be painful, what should you do
|
Give an analgesic at least 30 minutes before exposing the wound
|
|
|
Primary purpose of wet to dry dressing
|
Debride a wound
|
|
|
Common wetting agents for wet to dry dressing
|
Normal saline, lactated ringers solution, isotonic solutions
|
|
|
Transparent dressings
|
Thin, self-adhesive transparent film that belongs in semiocclusive or occlusive categories.
|
|
|
Irrigation
|
Gentle washing of an area with a stream of solution delivered through an irritating syringe
|
|
|
Can irrigations introduce prescribed medications in solution form
|
Yes
|
|
|
What direction should irrigation fluid flow
|
From least contaminated to most contaminated
|
|
|
Eschar
|
Black, leathery crust
|
|
|
Solutions used for irrigation
|
Warm water, saline, and mild detergent
|
|
|
How far should the tip of the syringe be when irrigating
|
1 inch (2.5cm) above the wound or area your cleansing
|
|
|
With small wounds, what size syringe and gauge is best used
|
35 mL syringe with a 19 gauge needle
|
|
|
Wound bleeding usually indicates
|
A slipped suture, dislodged clot, coagulation problem, trauma to blood vessels or tissue.
|
|
|
Abscess
|
Cavity containing pus and surrounded by inflamed tissue.
|
|
|
Adhesion
|
Band of scar tissue that binds together two anatomical surfaces normally separated
|
|
|
Cellulitis
|
Infection of the skin characterized by heat, pain, erythema, and edema
|
|
|
Dehiscence
|
Separation of a surgical incision or rupture of a wound closure
|
|
|
Evisceration
|
Protrusion of an internal organ through a wound or surgical incision
|
|
|
Extravastation
|
Passage or escape into the tissues
|
|
|
Hematoma
|
Collections of extravasated blood trapped in the tissue or in an organ
|
|
|
Signs of hemorrhaging
|
Rapid, thready pulse; decreased blood pressure; decreased urinary output; and cool, clammy skin
|
|
|
When a skin suture breaks and dehiscence occurs, you will be able to close the wound effectively using
|
Steri-strips or butterfly strip
|
|
|
If evisceration occurs after dehiscence, what should the nurse do
|
Pt must remain in bed in a low fowlers position, knees flexed. Keep patient on NPO status. Cover the wound and contents with warm, sterile dressing. Notify the surgeon immediately.
|
|
|
The CDC labels a wound infected when it contains what?
|
Purulent (pus) drainage
|
|
|
A patient with an infected wound shows what type of signs
|
Patient displays fever, tenderness, and pain at the wound site, edema, and an elevated WBC count
|
|
|
Does purulent drainage have an odor
|
Yes. Purulent drainage is brown, yellow, or green
|
|
|
Normal wbc count
|
4,500-10,000 white blood cells
per microliter (mcL) |
|
|
How long are retention sutures left in place
|
14 days or more
|
|
|
Who removes wire sutures
|
Physician
|
|
|
Abnormal quantity of exudate or drainage is greater than how much the first 24 hour
|
300 mL. Report it immediately.
|
|
|
Normal bile drainage
|
250 to 500 mL/ 24 hours
|
|
|
Wound vac
|
Device that assists in wound closure by applying negative pressure to draw edges of a wound together
|
|
|
Acceptable negative pressure ranges
|
5 mmHg and 200 mmHg. The average is 125 mmHg
|
|
|
Maceration
|
Damage to wound edges.
|
|
|
Wound dessication
|
To cause to dry up
|
|
|
Bandage
|
Strip or roll of cloth that can be wound around a part of the body
|
|
|
Binder
|

A bandage that is made of large pieces of material to fit a specific body part
|
|
|
When applying a binder, patient should flex their arm approximate at what angle
|
80 degree angle
|
|
|
Basic bandage turns
|
Spiral, figure of 8, recurrent, circular, spiral reverse
|
|
|
Circular bandage used
|
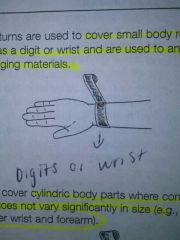
Cover small body regions (Digits or Wrist)
|
|
|
Spiral bandage use
|

Cover cylindrical body parts. Wrist or forearm
|
|
|
Spiral- reverse bandage use
|
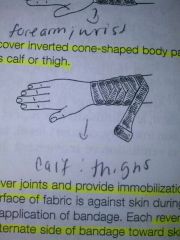
Use to cover inverted cone shaped body parts. Calf or thigh
|
|
|
Figure of 8 bandage use
|
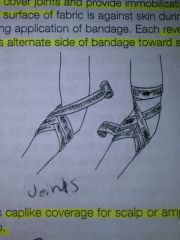
Used to cover joints and provide immobilization. Joints
|
|
|
Recurrent bandage use
|
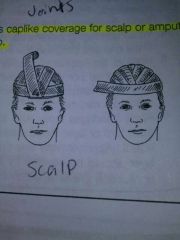
Provides caplike coverage. Scalp
|
|
|
Secondary intention
|

Wound must granulate during healing. Skin edges not close together,or when pus has formed.
|

