![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
Organization of Respiratory system |
Nasal cavity/mouth turbinates/conchea pharynx (air and food) larynx trachea (can stretch but rigid w muscles to accomodate for esophagus (when bolus presses on the back of trachea) and allow coughing) 2 lungs bronchus --> 2 bronchi (20+ generations of branching) contain alveoli (300 million in adult) where gas exchange happens |
|
|
Trachea mucous escalator & smoking effects |
-covered in mucous and moves particles up while air is breathed in; cilia on the epithelial cells beat in one direction propelling in one direction towards mouth - smoking irritates cilia and they disappear, changing the epithelial cells into tougher/shorter cells
|
|
|
lung muscles |
Diaphragm: squeezes blood into thorax helps breathing Intercostal muscles: most muscle work is inhale and exhale is recoil (little effort) |
|
|
Protective sacs of lungs |
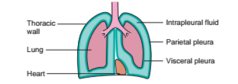
Parietal pleura (outside lining) Fluid (Intrapleural) sac (green) Visceral pleura Double membrane w water in between lubricant helps prevent tearing between organs |
|
|
Alveoli at the ends |
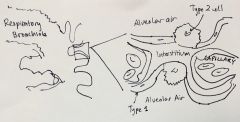
-capillaries surround numerous alveolus in sac to optimize surface area -Type 1 cell thin as possible to minimize air/O2 travel -Type 2 Secretory cells not included in gas exchange --> secretes surfactant |
|
|
Tidal Ventilation |
-air goes in and out the same tubes |
|
|
Bronchoconstriction causes |
mechanical irritant triggers closing off of bronchioles (also neighboring alveoli) ---> asthma has hyperactivity |
|
|
Purpose for surfactant |
air + water --> surface tension makes the alveoli collapse (intermolecular bonds on water). surfactant breaks this. because phospholipids that form a layer between water and air. greater effect on smaller alveoli and increases w deep breaths No equal and opposite electrostatic tension at surface --> the force --> surface tension surfactant prevents this and is produced in late fetal life |
|
|
Surfactant production |
cortisol --> surfactant --> premature baby in order to encourage production: give glutocorticoid to mother or synthetic surfactant(from animal) no surfactant: respiratory distress syndrome of the newborn |
|
|
Ventilation |
exchange of air between atmosphere and alveoli --> air moves through bulk flow from high to low pressure Flow = Change in pressure (p gradient)/ resistance change in pressure is (P-alveolar - P-atmosphere) Inspiration: P-alv < P-atm Expiration: P-alv > P-atm |
|
|
Inspiration |
intiated neurally through phrenic nerves that are innervating the diaphragm ----> diaphragm and inspiratory intercostals contract --> thorax expands --> interpleural pressure becomes more sub atmospheric ---> transpulmonary pressure increases --> lungs expand --> alveolar pressure becomes subatmospheric --> Air flows into alveoli |
|
|
Expiration |
end of inspiration --> motor neurons for inspiration stop firing then muscles relax, contraction stops --> chest wall start recoiling inward --> transpulmonary pressure decreases back to pre inspiration value lung recoil to preinspiration size --> alveoli air becomes compressed --> P-alv > P-atm --> air flows out of lungs passive but active during exercise |
|
|
Determinants of Lung compliance |
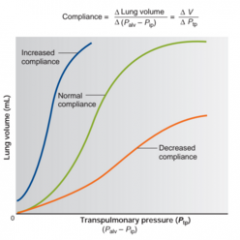
-stretchability of lung tissues; elastic connective tissues -- thickening of lung tissues decreases lung compliance -surface tension at the air-water interfaces within alveoli.
|
|
|
Surface tension in alveoli |
prevents alveoli from stretching further . energy needed to overcome surface tension and stretch connective tissue |
|
|
Law of Laplace |
relationship btwn pressure surface tension and radius of alveolus. P = 2T/r |
|
|
Air mixture |
78% Nitrogen 21% oxygen 1% CO2 (only important one is oxygen) all pressurized |
|
|
Atmospheric Pressure |
P-atm ~760 mmHg -in higher altitudes --> pressure decreases because density or air decreases the higher you are and gravity |
|
|
Partial pressure of oxygen |
0.21 ~160mmHg in boston This force will drive the oxygen throught the alveolar wall (type I) |
|
|
How does gas move within the body? |
Pressure gradients formed in the body (high to low) |
|
|
Gases in solution |
-gases dissolve in solution but have a solubility limit -gases are resistant in their state in a pressurized state -the move by diffusion through the pressure gradient P1V1 = P2V2 if pressure goes up volume goes down (viceversa) |
|
|
Neural inputs of breathing |
-neural inputs, signal generated in brain stem (2 major sets from the brain stem) - one goes from b stm down to spinal cord, innervates the rib muscles(intercostal) -- intercostal nerves -another does down to the spinal cord and innervate diaphragm -- phrenic nerves |
|
|
Rhythm centre of brain |
brain has rhythm built into it, no SA node like structure and no electrical stimulation within the organ. neural network w number of nuclei involved scattered around pons and medulla |
|
|
Breath frequency |
12-15 breaths a minutes, higher in women and children, and babies. Higher in sickness Rhythm modulated by SNS PSNS and other factors |
|
|
What can slow down breathing |
Sleep - metabolism slows down and doesn't need much O2 Drugs- ethanol inhibits the centre, barbituates act like GABA, all supress respiration and opiates conscious control for a limited time Pulmonary stretch reflex- when stretch sensitive cells near alveoli, connective lung tissue and chest wall --> activate sensitive neurons which go to brainstem and negative feedback to slow (from vagus nerve) |
|
|
What stimulates breathing |
Progesterone increases breaths exercise stretching skeletal muscles (independent of exercise) reflex --> stretch a muscle and triggers a measurable increase in ventilation conscious control for a limited time |
|
|
Chemoreceptors |
- detect chemicals in respiratory system (blood gases: O2 CO2 and H - located in arch of aorta: cortid and aortic bodies (derived from neural system) -detect how much blood gases are in the blood and monitor at all times what is the partial pressure of O2/CO2 in the blood and ion conc of hydrogen -influence speed of breathing -holding breath - more CO2 in blood and build up --> chemoreceptors will eventually force you to breathe |
|
|
CO2 in blood |
CO2 + water in presence of enzyme(carbonic anhydrase) mediate reaction forms short lived compound (carbonic acid) spontaneously dissociates into bicarbonate ions and H ions --CO2 has limited solubility --> lots of waste and formation of safer form --> creates H ion and increases acidity. 2/3 of CO2 does through this (some dissolves into solution or bind to hemoglobin) CHEMORECEPTORS: interpret H ions as imbalance of CO2 |
|
|
Acidosis |
when breath is held and H+ ions increase, blood becomes more acidic . low blood pH. |
|
|
Respiratory Acidosis |
Occur if there is a respiratory problem: -over dose on CNS depressants (barbituates or opiates) -depressed brainstem --> slowed breathing --> build up of CO2 because not disposing of it effectively -Pulmonary edema -anything that influences the ability of gases to move back or forth btwn alveoli and blood (could cause CO2 build up) -Emphysema (progressive/chronic) Chest surgery -painful after surgery -- shallow breaths build up of CO2 - need to be coached to increase surfactant and keep alveoli partially inflated YOU'RE NOT DOOMED TO HAVE ACIDOSIS FOREVER -KIDNEYS CAN HELP COMPENSATING FOR H+ (more excretion in urine) |
|
|
Metabolic Acidosis |
From lactic acid (more produced -> more in blood) blood gets more acidic respiratory system saves the day --> chemoreceptors pick up levels of acidity --> breathe faster and deeper respiration and kidneys regulate pH This is why you breathe so hard |
|
|
Keto Acidosis |
Ketones (fragments of fat ketones) are a useful form of energy w glucose (acetate) acidic |
|
|
Respiratory Alkalosis |
H+ ions decreases -- breathing more CO2 out than put into blood net CO2 decreases Hyper ventilation (decreasing CO2 increases pH) -happens from stress alertness anxiety (remnant of flight/fight) Hypoventilation (acidosis) |
|
|
Metabolic Alkalosis |
Alkali ingestion Vomiting |
|
|
Hemoglobin and New equilibrium |
equilibrium change because only unbound hemoglobins stay in solution and can move only in solution molecules matter O2 released from hemoglobin Hb +O2 <-> HbO2 ---> through association |
|
|
Cooperativity |
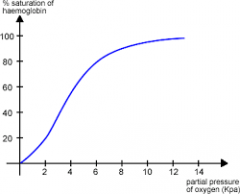
Protein with ligand units when one O2 ligand binds the iron, warps the heme(subunit + changes tertiary structure) triggering the change of other subunits--> heme more available for O2 to bing to Hb in curve the heme has a limit (100%) and reaches it as partial pressure increases |
|
|
Bohr effect |
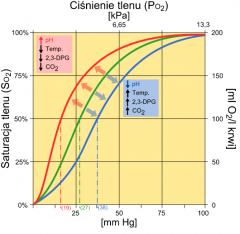
Shift of saturation v PO2 curve Hemoglobin bind w CO2 or H+ (different places) decreases the affinity temporarily for oxygen and so does heat more active --> more O2 --> more favor in unloading more active--> more waster products --> less hold on O2 by hemoglobin |
|
|
O2 pathway (inspired O2 in atmosphere to mitochondria) |
(lungs) inspired O2 -> alveolus ->dissolves through pulmonary capillary wall and in blood (most in hemoglobin >2% in plasma)-> O2 in Hb -> blood makes it to tissue capillary and oxygen goes through capillary wall -> interstitial fluid and then use diffusion gradient into cell -> mitochondrion consumes O2 |
|
|
CO2 pathway (mitochondria to expired CO2 in atmosphere) |
CO2 produced in cell -> dissolved in interstitial fluid through capillary wall ->either stay in plasma or dissolved in Erythrocyte (rbc) -> +Hb or turned into bicarbonate (out of cell) -> CO2 dissolves into lung and alveolus out as expired CO2 |

