![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
282 Cards in this Set
- Front
- Back
|
What does GERD stand for? |
Gastroesophageal reflux disease |
|
|
What is the cause of GERD? |
the esophagus is exposed to gastric acid for prolonged periods due to malfunction of the lower esophageal sphincter OR impaired peristalsis (motion that pushes food down) |
|
|
What bacteria may be present in GERD? |
Heliobacter Pylori |
|
|
Where is the pain of GERD felt? |
chest or epigastric |
|
|
What does the pain of GERD feel like? What is this pain also known as? (2) |
burning aka "heartburn" and regurgitation |
|
|
When does GERD typically occur? |
After meal, especially fatty foods |
|
|
Three factors that aggravate GERD. |
Lying down bending over physical activity |
|
|
Two prescriptions and one OTC someone with GERD can take to feel better. |
Antacids
selected drugs like: theophylline, or Calcium channel blockers |
|
|
Three things people with GERD should avoid. |
alcohol avoidance avoid fatty meals avoid chocolate |
|
|
Seven associated symptoms you might see in a GERD PT. |
wheezing chronic cough shortness of breath hoarseness choking sensation halitosis sore throat |
|
|
GERD increases the risk of what two conditions? |
1. Barrett's esophagus (lining of the esophagus is damaged by stomach acid; changed to a lining similar to the stomach)
2. esophageal cancer |
|
|
Where are peptic ulcers usually located? |
duodenum or stomach |
|
|
What is the difference between peptic ulcers and dyspepsia? |
Dyspepsia has similar symtpoms with no ulceration. |
|
|
Bacteria present in peptic ulcers and dyspepsia. |
H. Pylori |
|
|
Location and radiation of Peptic ulcers/dyspepsia |
Epigastric, radiates to back |
|
|
What kind of pain might a peptic ulcer/dyspesia PT describe to you? |
gnawing, burning, aching, pressing, hungerlike |
|
|
How might you distinguish the pain of duodenal ulcers from the pain of gastric ulcers or dyspepsia? |
the pain: 1. wakes them in the middle of the night 2. occurs, disappears for months and recurs |
|
|
2 Factors that may relieve peptic ulcers/dyspepsia. |
food, antacids |
|
|
Six associated symptoms you might see in a peptic ulcer/dyspepsia PT. |
Nausea vomiting belching bloating heartburn (more indicative of duodenal) weight loss (more indicative of gastric)
|
|
|
Name the age groups that dyspepsia, gastric ulcers and duodenal ulcers are most commonly seen in. |
Dyspepsia: young, 20-29 gastric ulcers: 50+ duodenal ulcers: 30-60 |
|
|
The majority (90-95%) of stomach cancers are what type? |
adenocarcinoma |
|
|
Name three places that stomach cancer is found. |
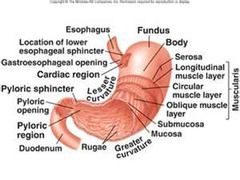
1. cardia (opening near top of stomach for food to pass down; connects esophagus to stomach) 2. distal stomach 3. gastroesophageal junction |
|
|
What might a PT with stomach cancer tell you their pain feels like? |
persistent, slowly progressive |
|
|
What aggravates stomach cancer pain? |
food
|
|
|
What makes stomach cancer pain from GERD and peptic ulcer/dyspepsia (in terms of what makes it feel better)? |
Stomach cancer is not relieved by antacids or food (peptic ulcers/dyspepsia are relieved by both GERD is relieved by antacids) |
|
|
Name 5 associated symptoms a stomach cancer PT might present with. |
Anorexia nausea early satiety weight loss bleeding |
|
|
What age range is stomach cancer common in? |
50-70 |
|
|
What is the cause of acute appendicitis? |
inflammation of the appendix with distention or obstruction |
|
|
Which two places might a PT with appendicitis point to when asked where they feel pain? |
pain is poorly localized general belly button area right lower quadrant pain |
|
|
1. If an appendicitis PT tell you that they have periumbilical pain, what would you expect that pain to feel like?
2. What if it is in the right lower quadrant? |
1. mild but increasing cramping
2. steady and more severe than that in the navel region
|
|
|
1. How long does the pain of appendicitis located in the periumbilical area last?
2. And in the right lower quadrant? |
1. 4-6 hours
2. depends on the intervention |
|
|
What causes acute cholecystitis? |
gallstone obstructing a cystic duct
|
|
|
Where would a PT point to for pain if they have acute cholecystitis? |
right upper quadrant or upper abdomen |
|
|
Where does the pain of acute cholecystitis radiate to? |
Right scapular area |
|
|
How would a PT describe the pain of acute cholecystitis? |
Steady, aching pain |
|
|
What two things make the pain of acute appendicitis in the right lower quandrant worse? |
Movement and cough |
|
|
What might a PT tell you about their pain that clues you in to perforation of the appendix? |
the pain has temporarily subsided |
|
|
1. Name three associated symptoms that present with the more severe form of appendicitis (right lower quadrant).
2. What can you expect these symptoms will usually be followed by? |
1. anorexia, nausea, vomiting
2. onset of pain and a low fever |
|
|
When does the pain of acute cholecystisis usually occur? |
gradual onset |
|
|
What makes acute cholecystitis worse? |
deep breathing (described as jarring in text) |
|
|
Name four associated symptoms of acute appendicitis. |
anorexia, nausea, vomiting, fever |
|
|
What causes biliary colic? |
Cystic duct or common bile duct is suddenly obstructed by a gallstone. |
|
|
1. Where would a PT with biliary colic point to for their pain? (two possible spots)
2. Where would it radiate to? |
1. epigastric OR right upper quadrant
2. radiates to right scapula and shoulder |
|
|
How would a PT likely describe the pain of biliary colic to you? |
steady, aching |
|
|
What is the "timing" for the pain of biliary colic? |
a recurrent pain that has a rapid onset over a few minutes, lasts for one to several hours and then gradually subsides |
|
|
Name four associated symptoms that biliary colic may present with. |
anorexia, vomiting, nausea, restlessness |
|
|
what is acute pancreatitis? |
acute inflammation of the pancreas |
|
|
1. Where is the pain of acute pancreatitis felt?
2. Where does it radiate to? |
1. epigastric
2. to the back or other parts of the abdomen |
|
|
What is the pain of acute pancreatitis like? |
steady |
|
|
What is the "timing" of the pain of acute pancreatitis? |
acute onset that is persistent |
|
|
What make the pain of acute pancreatitis worse? |
lying supine |
|
|
What makes the pain of acute pancreatitis better? |
leaning forward with the trunk flexed |
|
|
Name four associated symptoms of acute pancreatitis. |
nausea, vomiting, abdominal distention, fever |
|
|
What past medical history and social history items might indicate an increased risk for acute pancreatitis? |
history of previous attacks, alcohol abuse and gallstones |
|
|
What is the cause of chronic pancreatitis? |
fibrosis of the pancreas, caused by recurrent inflammation |
|
|
Where would a PT with chronic pancreatitis feel their pain?
|
epigastric, radiating to back |
|
|
How does the pain of chronic pancreatitis feel? |
steady, deep |
|
|
Name two factors that make chronic pancreatitis worse. |
alcohol, fatty, heavy meals |
|
|
What position might you find a chronic pancreatitis PT in that is trying to lessen the pain? |
learning forward with the trunk flexed |
|
|
Name three associated symptoms of chronic pancreatitis. |
1. pancreatic enzyme insufficiency 2. diarrhea with fatty stool (steatorrhea) 3. diabetes mellitus
|
|
|
The majority (95%) of pancreatic cancers are what kind? |
adenocarcinomas |
|
|
Where is the pain of pancreatic cancer felt?
Where does it radiate to? |
epigastric, radiates to the back |
|
|
How would a PT with pancreatic cancer most likely describe the pain? |
steady, deep, persistent pain |
|
|
What position might alleviate the pain of pancreatic cancer? |
learning forward with trunk flexed |
|
|
Name six associated symptoms of pancreatic cancer. |
anorexia nausea vomiting weight loss jaundice depression |
|
|
What is acute diverticulitis? |
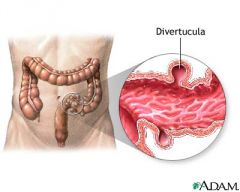
inflammation of the colonic diverticulum (a saclike mucosal outpouching through the colonic muscle) |
|
|
Where is the pain of acute diverticulitis felt? |
lower left quadrant |
|
|
What does the pain of acute diveritculitis feel like? |
may be cramping at first, but then becomes steady |
|
|
What is the onset of acute diverticulitis usually like? |
gradual |
|
|
Name 3 possible associated symptoms of acute diverticulitis. |
fever, constipation, brief diarrhea |
|
|
Name two causes of obstruction of the bowel lumen in acute bowel obstruction. Also, name their locations. |

<--- 1. adhesions (scar tissue) or hernias in the small bowel
2. cancer or diverticulitis in the colon |
|
|
A PT with acute bowel obstruction in the small bowel would localize their pain to where? |
periumbilical or upper abdomen |
|
|
A PT with acute bowel obstruction in the colon would localize their pain to where? |
lower abdominal or generalized |
|
|
Regardless of the location of the obstruction, the pain in acute bowel obstruction will likely be described as? |
cramping |
|
|
What is the onset of acute bowel obstruction pain in both the small bowel and colon? |
paroxysmal - sudden attack or increase of symptoms |
|
|
Which kind of the acute bowel obstruction (small bowel or colon) pain is decreased as bowel motility is impaired? |
small bowel |
|
|
Which kind of the acute bowel obstruction (small bowel or colon) pain is generally milder? |
colon |
|
|
Based on the associated symptoms, how might you differentiate between small bowel or colon acute bowel obstruction? |
Note: Obstipation = complete or severe constipation
The symptoms occur in opposite order:
small bowel presents with: vomiting of BILE and MUCUS or FECAL material early, then obstipation develops
colon: Obstipation occurs early, there is not likely to be vomiting but if there is it's a late symptom |
|
|
What causes mesenteric ischemia? |
A thrombosis or embolus is blocking blood supply to the mesentery (called acute arterial occlusion)
OR
the blood supply is reduced from hypoperfusion |
|
|
Where would a PT with mesenteric ischemia probably tell you the pain is? |
periumbilical at first, then more diffuse |
|
|
What might a PT with mesenteric ischemia describe their pain as? |
cramping at first, then steady |
|
|
What is the onset of mesenteric ischemia? |
abrupt, then persistent |
|
|
Name four associated symptoms of mesenteric ischemia. |
Vomiting, diarrhea (can be bloody), constipation, shock |
|
|
Do you see mesenteric ischemia in younger aged PTs or older? |
older aged |
|
|
What is oropharyngeal dysphagia caused be? |
motor disorders that affect the pharyngeal muscles |
|
|
What is the "timing" of oropharyngeal dysphagia |
acute or gradual onset and variable progression depending on the underlying disorder |
|
|
What makes the pain of oropharyngeal dysphagia worse? |
trying to swallow |
|
|
In PTs with oropharyngeal dysphagia, what might happen when they attempt to swallow? |
Aspiration into the lungs or regurgitation into the nose |
|
|
What are three conditions that can cause oropharyngeal dysphagia? |
stroke, bulbar palsy, other neuromuscular conditions |
|
|
What causes the pain in esophageal dysphagia? |
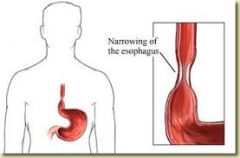
"mechanical narrowing"
|
|
|
In esophageal dysphagia:
if the mechanical narrowing is in the mucosal rings and webs, what is the "timing" of the pain? |
intermittent |
|
|
In esophageal dysphagia:
if the mechanical narrowing is in the mucosal rings and webs, what factor may aggravate the pain? |
solid foods |
|
|
In esophageal dysphagia:
if the mechanical narrowing is in the mucosal rings and webs, what might alleviate the pain? |
regurgitation of the bolus of food |
|
|
In esophageal dysphagia:
if the mechanical narrowing is due to an esophageal stricture, what is the "timing" of the pain? |
intermittent, may become slowly progressive |
|
|
In esophageal dysphagia:
if the mechanical narrowing is due to an esophageal stricture, what factor may aggravate the pain? |
solid food |
|
|
In esophageal dysphagia:
if the mechanical narrowing is due to an esophageal stricture, what might alleviate the pain? |
regurgitation of the bolus of food |
|
|
In esophageal dysphagia:
if the mechanical narrowing is due to an esophageal stricture, what might you see in the PT's PMH/CHS? |
long history of heartburn and regurgitation |
|
|
In esophageal dysphagia:
if the mechanical narrowing is due to esophageal cancer, what is the "timing" of the pain? |
may be intermittent at first, then progressive over months |
|
|
In esophageal dysphagia:
if the mechanical narrowing is due to esophageal cancer, what may aggravate the pain? |
solid foods, and then eventually liquids |
|
|
In esophageal dysphagia:
if the mechanical narrowing is due to esophageal cancer, what may alleviate the pain? |
regurgitation of the bolus of food |
|
|
In esophageal dysphagia:
if the mechanical narrowing is due to esophageal cancer, what are three associated symptoms? |
pain in the chest pain in the back weight loss (late-stage) |
|
|
What is the timing of the pain of diffuse esophageal spasm? |
intermittent |
|
|
What factors may aggravate diffuse esophageal spasm? |
solid or liquids |
|
|
What factors may alleviate diffuse esophageal spasm? |

1. nitroglycerin 2. repeated swallowing 3. straightening the back/raising the arms 4. Valsavla maneuver <--- straining down against closed glottis |
|
|
What does the pain of diffuse esophageal spasm mimic?
How long does it last? |
chest pain like angina pectoris or myocardial infarction
lasts minutes to hours |
|
|
What is the "timing" of scleroderma pain? |
intermittent; may progress slowly |
|
|
What factors may aggravate scleroderma? |
solids or liquids |
|
|
what is diffuse esophageal spasm? |
contractions of the esophagus are of normal amplitude but they are uncoordinated, simultaneous, or rapid |
|
|
what is scleroderma? |
connective tissue disorder that affects the skin; wall of the blood vessels; in this case, internal organs, such as the gastrointestinal tract |
|
|
what factors might alleviate scleroderma? |

1. repeated swallowing 2. straightening the back/raising the arms 3. Valsavla maneuver <--- straining down against closed glottis |
|
|
what are the associated symptoms of scleroderma? |
heartburn, other symptoms assocated with scleroderma (scleroderma is systemic) |
|
|
What is achalasia? |
increased pressure in lower esophageal sphincter (LES), diminished or absent peristalsis distal esophagus, and lack of a coordinated relaxation when swallowing |
|
|
what is the "timing" of achalasia? |
intermittent, may progress slowly |
|
|
what aggravates achalasia? |
solids or foods |
|
|
what alleviates achalasia? |

1. repeated swallowing 2. straightening the back/raising the arms 3. Valsavla maneuver <--- straining down against closed glottis |
|
|
what are three symptoms associated with achalasia? |
regurgitation at night when lying down nocturnal cough chest pain after eating |
|
|
Name three lifestyles habits that can affect bowel movements and lead to constipation. |
1. inadequate time or setting for defecation -ignoring the defecation reflex leads to inhibition of the defecation reflex; can be due to hectic schedules, unfamiliar surroundings, bed rest
2. False expectations of bowel habits -expectations of what is considered "regular" or more frequent stools than the person's norm; can be due to beliefs, treatments, ads for laxatives
3. diets deficient in fiber -leads to decreased fecal bulk; can be due to debilitation or constipating drugs |
|
|
Three patterns of irritable bowel syndrome. |
1. diarrhea-predominant 2. constipation-predominant 3. mixed |
|
|
What is Irritable Bowel Syndrome? What is it caused by? |
functional change in the frequency or form of bowel movements without known pathology; possibly due to change in intestinal bacteria |
|
|
What are the diagnostic critera of irritable bowel syndrome with respect to:
1. how long the abdominal pain has been present 2. how long the accompanying symptoms have been present 3. what symptoms and how many must be present |
1. pain must have onset of 3 months or longer 2. accompanying symptoms must have been present for 6 month or longer 3. 2/3 symptoms of the following must be present: -improvement w/defecation -onset with change in stool frequency -onset with change in stool form/appearance |
|
|
Name three types of mechanical obstructions of the bowels. |
1. cancer of the rectum or sigmoid colon 2. fecal impaction 3. obstructing lesions |
|
|
Why does the bowel become obstructed in cancer of the rectum or sigmoid colon? |
progressive narrowing of the bowel lumen from adenocarcinomas |
|
|
where is fecal impaction usually located? |
in the rectum |
|
|
What are some associated symptoms of sigmoid colon cancer? |
change in bowel habits, diarrhea, abdominal pain, bleeding, occult blood in stool |
|
|
what are some symptoms specific to rectal cancer? |
tenesmus - feeling of constantly needing to pass stool pencil-shaped stools weight loss |
|
|
what are some symptoms associated with fecal impaction? |
rectal fullness abdominal pain diarrhea around the impaction
|
|
|
What types of patients would you most likely find fecal impaction? |
debilitated bedridden elderly |
|
|
Name four types of lesions that can cause a mechanical obstruction of the bowel. |
1, diverticulitis 2. volvulus - tangled intestine 3. itussusception - part of intestine slides back into another section of intestine 4. hernia |
|
|
Name some symptoms associated with lesions that obstruct the bowel, ex. volvulus, intussusception, hernia, diverticulitis |
colicky abdominal pain abdominal distention red blood stools in intussusception |
|
|
The pain of painful anal lesions can cause what to occur? |
spasm of the external sphincter and voluntary inhibition of the defecation reflex. |
|
|
Name three associated symptoms with painful anal lesions. |
anal fissures painful hemorrhoids perirectal abcesses |
|
|
Name three kinds of drugs that can cause constipation. |
opiates anticholinergics antacids with calcium or aluminum |
|
|
Why do neurologic disorders cause constipation? |
interfere with the autonomic innervation of the bowel |
|
|
what are some associated symptoms of constipation from depression? |
fatigue anhedonia sleep disturbances weight loss (basically the typical depression symptoms) |
|
|
what are some neurologic disorders that can cause constipation? |
spinal cord injuries multiple sclerosis Hirschsprung's disease - missing nerve cells in the muscles of part or all of a baby's colon |
|
|
Name three metabolic conditions that can cause constipation. |
pregnancy hypothyroidism hypercalcemia |
|
|
Name the two types of diarrhea lasting NO LONGER THAN 14 days. |
secretory infection (non-inflammatory) inflammatory infection |
|
|
secretory infection diarrhea is caused by? |
viral infections, bacterial toxins
(S. aureus, B. cereus, C. perfringens, toxigenic E.coli, vibrio cholerae, cryptosporidium, Giardia lamblia, rotavirus) |
|
|
what kind of stool does secretory infection diarrhea cause? |
water, without blood, pus or mucus |
|
|
name the associated symptoms of secretory infection diarrhea. |
nausea vomiting diarrhea periumbilical cramping pain slightly elevated temperature |
|
|
name three risks for secretory infection diarrhea. |
travel common food source epidemic
|
|
|
what is the cause of inflammatory infection diarrhea? |
colonization or invasion of inestinal muscosa
(nonthyphoid Salmonella, Shigella, Yersinia, Camplylobacter, enteropathic E. coli, entamoeba, histolytica, C. difficile) |
|
|
what is the stool in inflammatory infection diarrhea like? |
watery, with blood, pus or mucus |
|
|
what are the associated symptoms of inflammatory infection diarrhea? |
lower abdominal cramping, pain and often rectal urgency aka tenesmus, fever |
|
|
what are some of the causes of inflammatory infection diarrhea? |
travel contaminated food or water frequent anal intercourse |
|
|
what are some drugs that cause diarrhea? |
magnesium-containing antacids antibiotics antineoplastic agents - aka anticancer laxatives |
|
|
Name two types of diarrheal syndromes that can cause diarrhea to last 30 days or more. |
Irritable bowel syndrome cancer of the sigmoid colon |
|
|
what are two possible characteristics of the stool in PTs with irritable bowel syndrome? |
loose, 50% with mucus, small to moderate volume OR
small, hard stools with constipation
can be mixed patterns |
|
|
when is diarrhea in irritable bowel syndrome the worst? (time of day) |
worse in the morning rarely at night
|
|
|
What are the associated symptoms of irritable bowel syndrome? |
crampy lower abdominal pain, abdominal distention, flatulence, nausea, urgency to defecate, relieves symptoms |
|
|
Who is at risk for irritable bowel syndrome? |
young and middle-aged adults |
|
|
what is the stool like in cancer of the sigmoid colon? |
blood-streaked |
|
|
what are some associated symptoms of cancer of the sigmoid colon? |
change in usual bowel habits, cramply lower abdominal pain, constipation |
|
|
what group is at risk for sigmoid colon cancer? |
middle-aged and older adults, especially 55+ |
|
|
What is ulcerative colitis? |
inflammation of the mucosa and submucosa of rectum and colon |
|
|
what are two kinds of Inflammatory Bowel Disease? |
ulcerative colitis crohn's disease of the small bowel or colon |
|
|
two kinds of crohn's disease. |
crohn's of the small bowel: aka regional enteritis crohn's of the colon: granulomatous colitis |
|
|
what is crohn's disease? |
chronic inflammation of the bowel wall, usually in a skip pattern involving the terminal ileum and/or proximal colon |
|
|
what is the stool like in crohn's (small bowel/enteritis) and in crohn's (colon/granulomatous colitis) |
small bowel/enteritis: small, soft to loose or watery and free of blood
colon/granulomatous colitis: blood in stool, less bleeding than in ulcerative colitis |
|
|
Is crohn's chronic and/or recurrent? |
both chronic and recurrent |
|
|
What are the associated symptoms of crohn's in small bowel/enteritis and colon/granulomatous colitis? |
small bowel/enteritis: crampy around the navel or right lower quadrant
colon/colitis: diffuse with pain and anorexia, low fever, weight loss
may also present with perianal fistulas |
|
|
what is distinct about the stool in ulcerative colitis? |
there is blood in the soft to watery stool |
|
|
who is at risk for ulcerative colitis? and what does it put those who have it at risk for? |
those at risk: young people puts them at risk for: colon cancer |
|
|
who is at risk for crohn's disease? what does it put them at risk for? |
those at risk: young people, late teens, also in middle age, people of jewish descent
at risk for: colon cancer |
|
|
Name three conditions that can be classified as "voluminous diarrhea." |
Malabsorption syndrome osmotic diarrhea secretory diarrhea |
|
|
What is malabsorption syndrome? |
defective transport/absorption by intestinal epithelium
impaired luminal digestion
epithelial defects at brush border |
|
|
Name three types of malabsorption disorders that are caused by defective absorption by intestinal epithelium |
crohn's celiac disease surgical resection |
|
|
name a type of malabsorption disorder that is caused by impaired luminal digestion. |
pancreatic insufficiency |
|
|
name a type of malabsorption disorder that is caused by epithelial defects of brush border. |
lactose intolerance |
|
|
what are some of the characteristics of the stool in malabsorption syndromes? |
bulky, soft, light yellow to gray, mush, greasy or oily, frothy, especially foul-smelling, usually floats |
|
|
Name some associated symptoms of malabsorption syndrome. |
anorexia, weight loss, fatigue, abdominal cramping, abdominal distention, symptoms associated with the nutritional deficiencies brought on by malabsorption |
|
|
In malabsorption syndrome what nutritional deficiency leads to bleeding?
|
vitamin K |
|
|
In malabsorption syndrome what nutritional deficiency leads to bone pain and fractures? |
vitamin D |
|
|
In malabsorption syndrome what nutritional deficiency leads to glossitis? |
vitamin B |
|
|
In malabsorption syndrome what nutritional deficiency leads to edema? |
protein |
|
|
Two causes of osmotic diarrhea |
lactose intolerance and abuse of osmotic purgatives |
|
|
what is lactose intolerance? |
lack of the intestinal enzyme lactase |
|
|
what types of stool are produced by osmotic diarrhea and secretory diarrhea? |
watery, large volume |
|
|
What makes lactose intolerance worse? better? |
worse: ingestion of milk better: fasting |
|
|
what does the pain associated with lactose intolerance feel like? |
crampy, abdominal pain, abdominal distention and flatulence |
|
|
What percentage of the African American, Asian, Native American, Hispanic and Caucasian population are lactose intolerant? |
African Americans, Asians, Native Americans and Hispanics: over 50% Caucasians: 5-20% |
|
|
what is melena? |
black, sticky, shiny, tarry stool |
|
|
In melana, occult blood test results are positive or negative? |
positive |
|
|
How much blood is lost into the GI tract for an adult to produce melena? Where is it lost from? |
at least 60 mL
usually lost from the esophagus, stomach, or duodenum. |
|
|
How long does it take for blood lost from esophagus, stomach or duodenum to be excreted? |
7-14 hours. |
|
|
If transit time from esophagus, stomach or duodenum is more than 7-14 hours, what is the likely source of the blood? |
jejunum, ileum or ascending colon |
|
|
what is a common cause of melena in newborns? |
swallowing blood during birth |
|
|
Name four causes of melena. |
GERD/peptic ulcers
gastritis/stress ulcers
esophageal or gastric varices
reflux esophagitis/Mallory-Weiss tear in mucosa due to vomiting |
|
|
Black, non-sticky stools are negative or positive for occult blood tests? |
negative, no pathologic significance |
|
|
Name some causes of black non-sticky stools. |
ingestion of iron, bismuth salts, licorice or even chocolate cookies |
|
|
If a PT comes to you with:
melena has recently ingested aspirin had recent bodily trauma increased ICP
what might you consider as the diagnosis? |
gastritis or stress ulcers |
|
|
If a PT comes to you with:
melena cirrhosis of the liver
what might you consider as the diagnosis? |
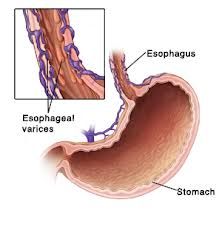
<--- esophageal - enlarged veins in the lower part of esophgus
(or gastric varices) |
|
|
If a PT comes to you with:
melena recent alcohol consumption states that they've been violently retching and vomiting
what might you consider as the diagnosis? |
Mallory-weiss tear to esophagus |
|
|
Hematochezia, what is it? And where does it usually originate from? |
red blood in the stool originating from the colon, rectum or anus
Note: can originate from jejunum or ileum, but less frequently |
|
|
What condition invovles large loss of blood into the stool, more than a liter? |
Upper gastrointestinal hemorrhage
|
|
|
Why does the blood stay red in hemtochezia as opposed to the black color in melena? |
Short transit time through the intestinal tract leaves little time for the iron in the hemoglobin to oxidate and turn black.
The longer the transit time through the GI tract - the darker the stool will be. |
|
|
Name some causes of hemetochezia. |

1. Colon cancer 2. Adenomatous hyperplastic polyps (pictured) 3. Diverticula of the colon 4. Inflammatory conditions of the colon/rectum (crohn's, ulcerative colitis, etc.) 5. Ischemic colitis 6. Hemorrhoids 7. Anal fissures |
|
|
What is ischemic colitis? |
Blood flood to the colon is reduced by blocked artieries. |
|
|
What finding would correlate with ischemic colitis in your physical exam of the abdomen upon palpation? |
abdomen is soft to palpation |
|
|
A PT presents with:
hematochezia lower abdominal pain fever and a soft abdomen upon palpation
What might you consider as a diagnosis? |
ischemic colitis |
|
|
What are some signs and symptoms of hemorrhoids and anal fissures? |
blood on the toilet paper blood on the surface of the stool blood dripping into the toilet |
|
|
What is a cause of reddish but not bloody stool? What symptoms might lead you to rule this out as having a non-pathologic origin? |
ingestion of beets
pink urine preceding the reddish stool |
|
|
What are some mechanisms of increased frequency to urinate? (Think changes to structure rather than disease) |
1. decreased capacity of the bladder 2. increased sensitivity to stretch due to inflammation 3.decreased elasticity of wall of the bladder 4. decreased inhibition of bladder contractions 5. impaired emptying of bladder leaving some residual urine in bladder
|
|
|
What are some causes of increased frequency to urinate? |
Infection stones tumor/foreign body in the bladder scar tissue motor disorders of the nervous system (stroke)
|
|
|
If a PT presents with burning on urination, urgency to urinate and hematuria would you expect his condition to arise from:
a) infection, stones, tumor
b) scar tissue
c) motor disorder of the nervous system
|
both a) and b) are possible:
a) infection, stones or a tumor b) scar tissue |
|
|
If a PT presents with increased frequency to urinate accompanied by neurologic symptoms like weakness and paralysis would you expect his condition to arise from:
a) infection, stones, tumor
b) scar tissue
c) motor disorder of the nervous system
|
c) motor disorder of the nervous system |
|
|
Name some mechanisms that could cause the bladder to not empty fully. |
partial obstruction of the bladder neck or proximal urethra
loss of peripheral nerve supply to the bladder |
|
|
What can cause an obstruction in the bladder neck or proximal urethra? |
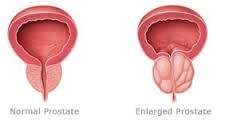
benign prostatic hyperplasia <---
urethral stricture
lesions of the bladder or prostate
|
|
|
If a PT presents to you with:
increased frequency of urination, hesistancy in starting the urinary stream, straining to void, reduced size and force of the stream and dribbling at the end
what diagnosis might you consider? |
an obstruction in the bladder of the neck or proximal urethra |
|
|
What condition is associated with a nerve disease that affects the sacral nerves and nerve roots and causes frequency to urinate? |
diabetic neuropathy |
|
|
Name some causes for nocturia wigh high output volumes. |
1.polyuria in general 2. decreased concentrating ability by kidneys and a loss of the normal decrease in nocturnal urinary output 3. excessive fluid intake before bedtime 4. fluid-retention/edematous states that accumlate during the day and excrete when the PT lies down at night |
|
|
Name some conditions that cause edematous states leading to nocturia. |
Heart failure nephrotic syndrome hepatic cirrhosis w/ascited chronic venous insufficiency |
|
|
Name two kinds of nocturia. |
Hight-volume nocturia low-volume nocturia |
|
|
Name a cause of low-volume nocturia. |
Insomnia in which the PT is up at night without a real urge to urinate |
|
|
Name four mechanisms of polyuria. |
1. antidiuretic hormone (ADH) deficiency 2. renal unresponsiveness to ADH 3. solute diuresis 4. excessive water intake |
|
|
what is solute diuresis? |
increased urination caused by the presence of certain substances in the small tubes of the kidneys
ex. electrolytes, nonelectrolytes |
|
|
A deficiency in antidiuretic hormone caused by a disorder of the posterior pituitary and hypothalamus is called?
|
diabetes insipidus
|
|
|
A condition in which the kidneys are unresponsive to antidiuretic hormone is called? |
nephrogenic diabetes insipidus |
|
|
What are some causes of nephrogenic diabetes insipidus? |
hypercalcemic and hypocalcemic nephropathy lithium toxicity |
|
|
In addition to polyuria what other associated factors would lead you to consider a diagnosis that is either diabetes insipidus or nephrogenic diabtetes insipidus? |
severe and persistent thirst/polydipsia
nocturia |
|
|
Name an electrolyte the can cause solute diuresis . And some causes of the imbalance.
|
Electrolyte: sodium salts large saline infusions, potent diuretics, some kidney diseases
Nonelectrolyte: glucose uncontrolled diabetes mellitus |
|
|
What is a symptom to check for to see if excessive water intake is the cause of your PT's polyuria? |
the polydipsia tends to be episodic and nocturia is usually absent |
|
|
What is stress incontinence (urinary)? |
the urethral spinchter is weakened so that it cannot fight the bladder pressure, urethral resistance is more easily exceeded |
|
|
Who often has stress incontinence (urinary)? |
Women: -who have a weakness in the pelvic flood and inadequate muscular support of the badder, -usually from childbirth or surgery. -postmenopausal atrophy of the mucosa -urethral infection
men : after prostatic surgery |
|
|
What are the symptoms of stress incontinence (urinary)? |
momentary leakage of small amounts of urine with coughing, laughing or sneezing |
|
|
What are some physical findings of someone with stress incontinence (urinary)? |
the bladder is NOT detected in physical exam
PT may exhibit during the exam, especially if sitting upright and has not voided before exam
atrophic vaginitis - thinning, drying and inflammation of the vaginal walls due to your body having less estrogen |
|
|
What is urinary urge incontinence? |
The detrusor contractions are so strong that they exceed the normal urethral resistance. |
|
|
Name some conditions urinary urge incontinence is caused by. |
stoke, brain tumor, demetia, spinal cord lesions (decreased inhibition of detrusor contractions)
bladder infections, tumors, fecal impaction (sensory pathways are hyperexcitable)
deconditioning of voiding reflex due to frequently voiding at low bladder volumes
|
|
|
In cases where the urge incontinence is due to a DECREASE in inhibition of detrusor contractions, what are some signs and symptoms you might expect? |
moderate volume of involuntary urine loss preceded by an urge to void
mental deficits and motor signs of CNS disease are often present |
|
|
What are some clues to tell you that a PT's urge incontinence is probably arising from hyperexcitability of the sensory pathways (ex. bladder infection, tumor, fecal impaction) |
urgency, frequency and nocturia with small to moderate volumes and acute inflammation or pain while urinating may be present
other local pelvic problems are present |
|
|
What are some clues to tell you if a PT's urge incontinence is likely based off us a deconditioning of the void reflex? |
they void within seconds after positional changes, or going up/down stairs
|
|
|
What is overflow incontinence? |
the detrusor contractions are insufficient to overcome urethral resistance and the bladder becomes large even after an effort to void |
|
|
What are detrusor contractions? |
When the bladder is stretched, the parasympathetic nervous system signals to contract the detrusor muscle. This encourages the bladder to expel urine through the urethra |
|
|
What are three causes of overflow incontinence? |
obstruction of the bladder outlet such as in benign prostatic hyperplasia
weakness of the detrusor muscle due to peripheral nerve disease at sacral level
interruption of the reflex arc from impaired bladder sensation (such as in diabetic neuropathy) |
|
|
How would you narrow down the cause of overflow incontinence to either: a) obstruction b) peripheral nerve disease c) impaired bladder sensation |
obstruction - continuous dripping
peripheral nerve disease - decreased force of the stream
impaired bladder sensation - PT is diabetic |
|
|
What is functional incontinence? |
inability to get to the toilet in time because of impaired health or environmental conditions |
|
|
Name some health conditions that cause functional incontinence. |
problems in mobility such as weakness, arthritis, poor vision |
|
|
Name some environmental factors that cause functional incontinence. |
unfamiliar settings, distant bathrooms, bed rails, physical restraints |
|
|
In overflow incontinence what is a common physical exam finding? |
enlarged bladder that is tender |
|
|
Name some drugs that may cause incontinence. |
sedatives tranquilizers anticholinergics sympathetic blockers potent diuretics |
|

Name this bulge in the abdominal wall.
Define it. |
Umbilical hernia.
protrusion through a defective umbilical ring, typically in infants but can be in adults. |
|

Name this bulge in the abdominal wall.
Define it. |
Incisional hernia.
protrusion through an operative scar |
|
|
How is an umbilical hernia usually resolved in infants? |
On its own within 1 to 2 years. |
|
|
When you palpate an incisional hernia what must you determine?
Why is it important to determine this? |
Detect the length and width.
A large hernia that passing through a small defect has a greater risk for complications than a large defect.
|
|

Name this bulge in the abdominal wall.
Define it. |
Epigastric hernia.
Small midline protrusion through a defect in the linea alba. Occurs between the xyphoid process and the umbilicus. |
|
|
How do you palpate an epigastric hernia? |
With the patient's head and shoulders raised, run your fingerpad down the linea alba to feel it.
|
|

Name this bulge in the abdominal wall (vs. the normal chest on the bottom).
Define it. |
Diastasis recti.
Separation of the two rectus abdominus muscles, through which the abdominal contents form a midline ridge when the PT raises his head and shoulders. |
|
|
Name three common causes for diastasis recti. |
pregnancy obesity chronic lung disease
|
|

Name this bulge in the abdominal wall.
Define it. |
Lipoma.
Common, benign, soft, lobulated, fatty tumors usually in subcutaneous tissues almost anywhere on the body, including the abdominal wall. |
|
|
How would you palpate a lipoma? |
Press your finger down on the edge of the lipoma, it should slip out from under. |
|

Name this cause of a protruberant abdomen.
Where is it thickened? |
Fat.
Fat thickens the abdominal wall, the mesentery and omentum.
|
|
|
What is a pannus? |
apron of fatty tissue that may exten below the inguinal ligaments |
|
|
When inspecting a pannus what should you look for? |
Lift the pannus to look for inflammation in the skin folds or even a hidden hernia. |
|

Name this cause of a protruberant abdomen.
What would you expect it to sound like when percussed? |
Gas.
caused by certain foods, or more serious conditions like intestinal obstruction and adynamic (paralytic) ileus.
tympanic percussion note |
|

Name this cause of a protruberant abdomen.
What would you expect it to sound like when percussed? |
a large, solid tumor that is usually rising out of the pelvis
dull to percussion |
|
|
Name some causes of a tumor in the abdomen. |
ovarian tumors uterine myomata |
|

Name this cause of a protruberant abdomen.
How might you distinguish this from another cause? |
Pregnancy.
Listen for the fetal heart. |
|
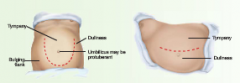
Name this cause of a protruberant abdomen.
How might you distinguish this from another cause?
|
Ascitic fluid.
Ascitic fluid seeks the lowest point in the abdomen, if you turn the PT on their side and the fluid shifts to the lowest point. |
|
|
What are you listening for at this spot on the abdomen. (general) |
bowel sounds |
|
|
Bowel sounds can be described as increased or decreased.
Which would you expect in early intestinal obstruction?
In adynamic ileus and peritonitis? |
Increased - early intestinal obstruction
decreased - adynamic ileus and peritonitis |
|
|
What is recommended you do before you decide that bowel sounds are absent? |

sit down and listen at the "x" for 2 or more minutes. |
|
|
If you hear a high-pitched tinkling sound in the bowels what does this suggest? |
intestinal fluid and air under tension in a dilated bowel |
|
|
If you hear rushes of high-pitcheded sounds in the bowels what does this suggest? |
intestinal obstruction, especially those that coincide with an abdominal cramp |
|

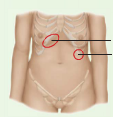
If you hear a soft humming noise with both systolic and diastolic components where indicated, what is this called?
What is this sound caused by?
Ex. of a condition that would cause this? |
Venous hum.
Caused by increased collateral circulation between portal and systemic venous systems.
hepatic cirrhosis |
|
|
What kind of sound does bruits make? |
turbulent flow
sound of blood rushing past an obstruction |
|
|
What is a hepatic bruit indicative of? |
carcinoma of the liver or alcoholic hepatitis |
|
|
What is arterial bruits suggestive of? |
partial occlusion of the aorta or large arteries |
|
|
Partial occlusion of a renal artery can lead to? |
hypertension |
|
If you hear a grating sound at either of the indicated spots what would you consider is the cause?
What does this sound indicate? |
friction rub.
inflammation of the peritoneal surface of an organ such as in liver cancer or splenic infarct.
|
|
|
When a systolic bruits accompanies a hepatic friction rub what condition is likely? |
carcinoma of the liver |
|

Explain how you would localize the tenderness in a PT's abdomen, deep or superficial? |
Ask the PT to raise their head and shoulders, if the tenderness persists it is more superficial, whereas if the tendernesss is from a deeper lesion it will be protected by the tightened muscles and the pain will decrease. |
|

If a PT is concerned about pain in these structures and states that the discomfort is dull and you find that there is no muscular rigidity or rebound tenderness what would you conclude? |
That these structures are normally tender to deep palpation and that this is normal. |
|

A PT experiencing abdominal pain and tenderness in the area denoted by the red line (unilaterally or bilaterally) with rebound tenderness and rigidity what diagnosis might you consider further? |
acute pleurisy |
|

If a PT states that they are experiencing pain in the red areas of the picture and you find that they hve rebound tenderness and motion of the uterus causes pain what diagnosis might you consider? |
acute salpingitis |
|

What condition is likely when a PT tells you they have pain in the red area and upon palpation you find that it hurts when they breathe in (Murphy's sign.) |
acute cholecystitis |
|

What condition is likely when the pain is "almost like a left-sided appendicitis?" |
acute diverticulitis |
|
|
If a PT states that they have a severe amount of pain in their whole abdomen and you see guarding (boardlike muscle rigidity) what condition would you consider? |
generalized peritonitis |
|
|
Does a palpable liver always indicate hepatomegaly? |
No, more often it results from a change in consistency (soft to firm). |
|
|
Explain the significance of palpating a liver that seems to extend far past the lower costal margin than normal BUT, is determined by percussion to be normal dimensions for a liver. |
Downward displaced liver
It is likely a low diaphragm, the upper border is also low (due to the low diaphragm) so the bottom liver edge is past the costal margin, common in COPD. |
|

An elongation in the right lobe that is easily palpable is called?
What does this finding suggest? |
Riedel's Lobe
It is a normal variation, typically in those who are lanky in build, it is not an increase in liver volume or size. |
|

If you palpate a smooth, non-tender, large liver what would you consider as a possible diagnosis?
What if it is tender? |
Cirrhosis may produce an enlarged liver with a firm, non-tender liver.
Tender: suggests inflammation such as in hepatitis, venous congestion of right-sided heart failure |
|

An enlarged liver that is firm or hard and has irregular edges suggests what?
Would you expect the liver to be tender or non-tender? |
Hepatocellular carcinoma
The liver may be tender or non-tender. |

