![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
113 Cards in this Set
- Front
- Back
|
Blood Vessels - arteries, capillaries and veins constitute a closed system for distribution of blood throughout body. |
Components of the Circulatory System - Pulmonary Circulation allows exchange of oxygen and carbon dioxide in the lungs; systemic circulation provides exchange of nutrients and wastes between blood and cells - Arteries: provide transport of blood away from heart and into lungs or to body tissues - Arterioles: smaller branches of arteries that control the amount of blood flowing into capillaries (thru degree of contraction of smooth muscle in vessel walls (vasoconstriction of dilation) - Capillaries: very small vessels organized in numerous networks that form the microcirculation. Blood flows very slowly and precapillary spincters determine amount of blood flow from arterioles into capillaries (depend on metabolic needs of tissue) |
|
|
Components of the Circulatory System - Small venules conduct blood from capillary beds toward heart- - larger veins collect blood draining from venules (approx 70% blood) located in veins at one time (veins are called capacitance vessels) blood flow depends on skeletal muscle action, respiratory movements and gravity. Valves in larger veins (arms and legs) keep blood flowing through heart. |
Walls of Arteries and Veins are made up of 3 layers 1. Tunica Intima (endothelial layer) inner layer 2. Tunica Media (layer of smooth muscle) that controls diameter and lumen size (diameter) of blood vessel (middle layer) 3. Tunica Adventitia (externa) outer connective tissue layer and contains elastic and collagen fibers. |
|
|
Vasa Vasorum - consist of tiny blood vessels supply blood to tissue of wall itself - normally large arteries highly elastic adjust changes in blood volume during cardiac cycle Ex: aorta must expand during systole to prevent systolic pressure rising too high - diastole: walls must recoil to maintain adequate diastole pressure - veins: have thinner walls than arteries and less smooth muscle |
Autoregulation - reflex adjustment in small area of tissue or an organ (varies depending on needs of cell in area) - controls localized vasodilation or vasoconstriction in arterioles Ex: decrease in pH, increase CO2 or decrease in O2 leads to Local Vasodilation - cause by release of chemical mediators (histamine or increase in temperature) cause vasodilation |
|
|
Norepinephrine and Epinephrine - increase systemic vasoconstriction - by stimulating alpha1-adrenergic receptors in arteriolar walls - Angiotensin (another powerful systemic vasoconstrictor) |
Capillary Walls - consist of single endothelial layer: facilitate exchange of fluid, oxygen and carbon dioxide, electrolytes, glucose and other nutrients and wastes between blood and interstitial fluid. - exchange abnormal electrolyte shifts |
|
|
TA 10-1 a) Explain why a high elastic content is required in the wall of aorta = A high elastic content is needed for expansion during systole, recoil during diastole, and prevention of extreme high or low blood pressures. b) Explain function of smooth muscle in arteries = controls peripheral resistance by vasoconstriction, the capacity of the cardiovascular system, blood pressure, and distribution in the body. |
TA 10-1 c) Predict those organs that would be expected to have a large capillary network what criteria did you use in making this prediction = Skeletal muscle requires more blood when exercising; the large surface area for liver allows exchange of nutrients and removal of wastes. d) Explain how venous return increases with exercise and purpose of action = Skeletal muscle activity and increased respirations promote movement of blood up through the veins to the heart. |
|
|
Blood - major transport system of body for essentials (oxygen, glucose and other nutrients, hormones, electrolytes and cell wastes) - serves as critical part of body's defenses carrying antibodies and WBCs for rapid removal of any foreign material - promote homeostasis, control body temp thru peripheral tissue. - blood is medium which body fluid levels and blood pressure measured (adjusted by hormones) - clotting factors available for hemostasis - buffer system in blood maintain stable pH 7.35 to 7.45 |
Composition of Blood - Adult body: approx 5 liters of blood - consist of water, dissolved solutes (55% of whole blood volume), remaining 45% (cells or formed elements (erythrocytes, leukocytes, thrombocytes or platelets) - Hematocrit: proportion of cells (essentially erythrocytes) in blood - indicates viscosity of blood Females 37% to 47% |
|
|
Composition of Blood - elevated hematocrit = dehydration (loss of fluid) or excess RBCs - low hematocrit: blood loss or anemia - Plasma = clear yellowish fluid remaining after cells removed - Serum = fluid and solutes remaining after cells and fibrinogen removed Plasma protein include albumin (maintains osmotic pressure in blood), globulins or antibodies; and fibrinogen (essential formation of blood clots) |
Blood Cells and Hematopoiesis - all blood cells originate from red bone marrow - Adult bone marrow: found in flat and irregular bones, ribs, vertebrae, sternum and pelvis. (iliac crest in pelvic bone common site for bone marrow aspiration biopsy) - During hemopoiesis or hematopoiesis: various blood cells develop from a single stem cell (pluripotential hematopoietic stem cell) - differentiation of this process commit to stem cells for each type of blood cell - then theses cells proliferate and mature = specialized functional cells |
|
|
Dyscrasia: pathological condition of blood usually refer to disorders (abnormality of blood or bone marrow; abnormal cell characteristics or numbers |
RBCs and Hematopoiesis - Erythrocytes or RBCs: biconcave, flexible discs that are non-nucleated when mature and contain hemoglobin - size and structure are essential for easy passage thru small capillaries - Hormone Erythropoietin (originate from kidney) stimulates erythrocyte production in red bone marrow in response to Hypoxia (insufficient oxygen available to cells. - Normally RBCs (4.2 to 6.2 million.mm^3) constitute most of cell volume in blood - adequate RBC production and maturation depend on availability of many raw materials (aa, iron, vit B12, vit B6, and folic acid) |
|
|
Hemoglobin = globin portion, two pairs of amino acid chains + 4 heme groups (each contain a ferrous iron atom, which O2 attaches to) - Heme provides the red color - normally hemoglobin become fully saturated with oxygen in lungs |
Oxyhemoglobin (bright red color) distinguishes arterial blood from venous blood, as blood circulates thru body, O2 dissociates from hemoglobin Deoxygenated hemoglobin (deoxyhemoglobin or reduced hemoglobin) = dark or bluish-red in color (found in venous blood) |
|
|
Small portion of CO2 in blood carried by hemoglobin (carbaminohemoglobin) attached to nitrogen in AA group at DIFFERENT site from that for O2. - most CO2 transported in blood as bicarbonate ion = Fatal hypoxia: oxygen easily displaced from hemoglobin by carbon monoxide (which binds tightly to iron) Carbon monoxide poisoning can be recognized by bright cherry color lips and face |
Lifespan of RBCs - approx 120 days - as it ages, cell becomes rigid and fragile - finally succumbs to phagocytosis in spleen or liver, (broken down into globin and heme) - Globin broken down into AA - recycled in AA pool - Iron (recycled) returned to bone marrow and liver (reuse in synthesis of more hemoglobin - excess iron can be stored as Ferritin or Hemosiderin in liver, blood, and other body tissues. |
|
|
Hemochromatosis - genetic disorder (iron overload) results in large amounts of hemosiderin accumulating in liver, heart and other organs causing serious organ damage |
Balance of heme component is converted to Bilirubin and transported by blood to liver where it is conjugated (or combined) with glucuronide to make it more soluble - excreted in bile - excessive hemolysis (destruction of RBCs may cause elevated serum bilirubin levels = Jaundice (yellow color in sclera of eye and skin) |
|
|
Hematopoiesis - Leukocytes (5 to 10,000/mm3) make up only about 1% of blood volume - subdivided into 3 types of granulocytes and 2 types of agranulocytes *all types of development and differentiate from original stem cell in bone marrow - Leukocyte (production of WBCs) stimulated by colony-stimulating factors (CSFs) produced by macrophages and T lymphocytes |
Ex: granulocyte CSF or multi-CSF (interleukin-3 [IL-3]) may be produced to increase certain WBCs during inflammatory response. - WBCs may leave capillaries and enter tissues by diapedesis (ameboid action) - movement thru intact capillary wall = needed for defense |
|
|
5 Types of Leukocytes 1. Lymphocytes (30 to 40% of WBCs) - B and T lymphocytes in immune response - some T cells designate as natural killer cells (significant in immunity) |
2. Neutrophils (polys, segs or PMNs) - most common leukocytes (50-60% of WBCs) but survive only 4 days. - First to respond to tissue damage and commence phagocytosis - an immature neutrophil is called a band or stab (increased in numbers by bacterial infection) = Lab: "shift to the left" pattern of luekoytes |
|
|
Basophils - migrate from blood and enter tissue to become mast cells (release histamine and heparin) - may be fixed in tissues or wandering |
Eosinophils - combat effects of histamine - increased by allergic reactions and parasitic infections |
|
|
Monocytes - can enter tissue to become macrophages = act as phagocytes when tissue damage occurs |
Differential Count - indicates proportions of specific types of WBCs in blood - frequently assist in making diagnosis Ex: bacterial infection or inflammatory condition stimulates increases in neutrophils - allergic reactions or parasitic infections increase the eosinophil counts |
|
|
Thrombocytes (platelets) - essential part of blood-clotting process or hemostasis - are not cells; very small, irregularly shaped, non-nucleated fragments from large megakaryocytes - platelets stick to damaged tissue and to each other to form platelet plug that seals small breaks in blood vessels or adhere to rough surfaces and foreign material - Common drug ASA (aspirin) reduce this adhesion and lead to increased bleeding tendency. - thrombocyte can initiate the coagulation process |
Blood Clotting - Hemostasis: consist of 3 steps 1. immediate response of blood vessel to injury = vasoconstriction or vascular spasm - in small blood vessels (decrease blood flow and may allow platelet plug to form) 2. thrombocytes tend to adhere to underlying tissue at site of injury, if blood vessel is small = form platelet plug in vessel 3. blood-clotting or coagulation mechanism required in larger vessels clotting factors are present in inactive forms in circulating blood are activated thru sequence of reactions - recent evidence indicates additional overlap in factor activity between intrinsic and extrinsic pathways but cascade reactions is basis for coagulation |
|
|
Clot formation (Coagulation) - requires sequence or cascade of events 1. damaged tissue and platelets release factors that stimulate a series of reactions involving numerous clotting factors = produce prothrombin activator (PTA) 2. Prothrombin or factor II (inactive in plasma) is converted into thrombin 3. Fibrinogen (factor I) converted into fibrin threads 4. Fibrin mesh forms to trap cells, making up a solid clot (thrombus) and stopping flow of blood 5. Clot gradually shrinks or retracts, pulling edges of damaged tissue closer together and sealing site |
Circulating clotting factors produced primarily in Liver - Vitamin K (fat-soluble) required in synthesis of most clotting factors - Calcium ions essential for many steps in clotting process |
|
|
Other measure can be used to faciliate clotting proces: Apply pressure and cold (vasoconstrictor) to site reduce blood flow in area or thrombin solution applied directly to speed up clotting |
Fibrinolysis - enzymatic breakdown of Fibrin in blood clots - delicate balance is always necessary between tendency to clot to prevent blood loss and tendency to form clots unnecessarily and cause infarctions. - prevent inappropriate thrombus formation, coagulation inhibitors (anti-thrombin III circulate in blood) - thru Thrombin, prostaglandin released to prevent platelets sticking nearby undamaged tissue. - Heparin (anticoagulant) released from basophils or mast cells in tissues = exert blocking thrombin - Heparin (drug) may be administered intravenously to patients at risk for thrombus formation. - does not dissolve clots but prevent further growth of thrombus. |
|
|
Natural Fibrinolytic process break down newly formed clots - Inactive plasminogen circulates in blood - following injury, converted by tissue plasminogen activator (tPA) and streptokinase thru sequence of reactions into plasmin. - plasmin breaks down fibrin and fibrinogen - localized fibrinolysis event - plasmin quickly inactivated by plasmin inhibitor - Application of this mechanism with "clot-buster" drugs (streptokinase (streptase)) minimize tissue damage resulting from blood clots |
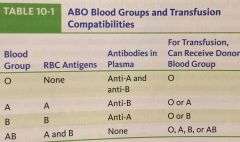
Antigenic Blood Types - individual's blood type determined by presence of pacific antigens on cell membranes of that person's erythrocytes - ABO groups are inherited depends on presence of type A or B antigens or agglutinogens - after birth, antibodies can react with different antigens on another person's RBCs form in blood of newborn infant - result in Agglutination (clumping) and hemolysis of recipient's RBCs, when incompatible blood transfusion |
|
|
Person's with Type O blood, lack A and B antigens = Universal Donors Persons with Type AB blood are Universal Recipients |
|
|
Signs of a transfusion reaction include - feeling of warmth in involved vein, flushed face, headache, fever and chills, pain in the chest and abdomen, decreased blood pressure and rapid pulse |
Another inherited factor in blood is Rh factor - may cause blood incompatibility if mother is Rh-negative and fetus is Rh positive Plasma or colloidal volume-expanding solutions can be administered without risk of reaction because they are free of antigens and antibodies |
|
|
Diagnostic Tests - complete blood count (CBC) includes total RBCs, WBCs, platelet counts and morphology (size and shape), a differential count for WBCs, hemoglobin and hematocrit values Ex: Leukocytosis = increase in WBCs in circulation is often associated with inflammation or infection Leukopenia = decrease in leukocytes occur with some viral infections as well as with radiation and chemotherapy |
Increase in Eosinophils = common with allergic responses |
|
|
Hematocrit shows % of blood volume composed of RBCs indicate fluid and cell content - may be indicator of anemia (low RBC count) - hemoglobin is measured and amount of hemoglobin per cell is shown by mean corpuscular volume (MCV) MCV indicates oxygen-carrying capacity of blood |
Bone Marrow Function can be assessed by - reticulocyte (immature non-nucleated RBC) count plus bone marrow aspiration and biopsy |
|
|
Blood-clotting disorders Diagnostic Tests - differentiated by tests such as bleeding time (measure platelet function, the time to plug a small puncture wound); prothrombin time or INR International Normalized Ratio (measures extrinsic pathway) and partial thromboplastin time (PTT- intrinsic pathway) measure function of various factors in coagulation process. = also used to monitor anticoagulant therapy |
Blood Therapies - whole blood, packed RBCs or packed platelets may be administered when severe anemia or thrombocytopenia develops - plasma or colloidal volume-expanding solutions can be administered without risk of a reaction = free of antigens and antibodies - Artificial blood products available- but non can perform all complex functions of normal whole blood, compatible with all blood types, Hemolink made of human Hemoglobin, Hemopure made from cow hemoglobin. Oxygent is synthetic (genetically engineered blood substitute. - Epoetin alfa (Procrit, Eprex) form of erythropoietin produced thru use of recombinant DNA technology- administered by injection to stimulate production or RBCs before certain surgical procedures (hip replacement) and patients with anemia related to cancer or chronic renal failure = reduces risk of infection or immune reaction associated with multiple blood transfusions |
|
|
Bone marrow or stem cell transplants - treat some cancers, severe immune deficiency or severe blood cell disease. For success: close match in tissue or human leukocyte antigen (HLA) type required. (marrow stem cells extracted from donor's pelvic bone, filtered and infused into recipient's vein) - For patients suffering from lack of blood clotting capability, drugs available to aid clotting process. Nplate drug stimulates platelet production of bone marrow. NovoSeven drug treat hemophiliacs but has been adapted to treat combat trauma. |
TA 10-2 a) state function of each type of cell in blood Erythrocytes contain hemoglobin to transport oxygen to cells; leukocytes form part of the defense system, participating in phagocytosis, the inflammatory response, and immune response; and thrombocytes are essential for blood clotting. |
|
|
TA 10-2 b) State 3 major functions of plasma proteins and list component responsible for each Albumin is primarily responsible for the osmotic pressure of the blood; globulins act as antibodies and fibrinogen is a clotting factor. |
TA 10-2 c) What is the normal pH range of blood? Why is it important to maintain this pH? = The normal pH range of blood is 7.35 to 7.45. A normal range is required for enzyme and metabolic functions; blood is a medium for the exchange of body fluids and for maintaining homeostasis. |
|
|
TA 10-2 d) Describe the 3 stages of hemostasis The stages of hemostasis are as follows: (1) transient vasoconstriction to reduce blood flow into the site; (2) thrombocytes stick to the site, attempting to form a plug; and (3) the clotting cascade takes place to form a fibrin mesh. |
Blood Dyscrasias (pg 193) The Anemias - cause a reduction of oxygen transport in blood due to decrease in hemoglobin content - low hemoglobin level may result from declining production of protein, decrease number of erythrocytes, or combo of these factors |
|
|
Anemia: oxygen deficit leads to sequence of events - less energy is produced in cells; cell metabolism and reproduction are diminished - compensation mechanisms improve oxygen supply including tachycardia and peripheral vasoconstriction - lead to general signs of anemia- fatigue (excessive tiredness), pallor (pale face), dyspnea (increased effort to breathe) and tachycardia (rapid heart rate) - decreased regeneration of epithelial cells cause digestive tract to become inflamed and ulcerated - stomatitis (ulcer in oral mucosa) inflamed and cracked lips, and dysphagia (difficulty swallowing) hair and skin may show degenerative changes - severe anemia may lead to angina (chest pain) during stressful situations if oxygen supply to heart is sufficiently reduced. Chronic severe anemia may cause congestive heart failure |
Anemias occur when there is deficiency of a required nutrient, bone marrow function impaired or blood loss or excessive destruction of erythrocytes. |
|
|
Iron Deficiency Anemia - Pathophysiology - insufficient iron impedes synthesis of hemoglobin - reducing amount of O2 transported in blood = results in microcytic (small cell) = Hypochromic (less color) erythrocytes = low concentration of hemoglobin in each cell - very common, (mild to severe in all ages) est 1 in 5 women affected and increases for pregnant women. - also reduction in stored iron (indicated by decreased serum ferritin, decreased hemosiderin and decreased iron-containing histiocytes in bone marrow |
Etiology of Iron deficient Anemia (many reasons) - dietary intake of iron-containing vegetables or meat meat below minimum requirement (particular during adolescent growth spurt or pregnancy, breastfeeding = need to increase) (normally 5-10% ingested iron is absorbed but can increase to 20% when deficit) - Chronic blood loss from bleeding ulcer, hemorrhoids, cancer or excessive menstrual flow (cause of iron deficiency), continuous blood loss means less iron recycled to maintain adequate production of Hemoglobin |
|
|
Etiology of Iron deficient Anemia (many reasons) - Duodenal Absorption of ion may be impaired by disorders including malabsorption syndromes (regional ileitis and achlorhydria (lack of hydrochloric acid in stomach)) - Severe Liver disease may affect both iron absorption and iron storage (protein deficit would further impede hemoglobin synthesis) - Iron present but not well used = low hemoglobin levels but high iron storage levels (associated with some infections and cancers) |
Signs & Symptoms of Iron Deficiency Anemia -mild anemia frequently asymptomatic, hemoglobin drops, signs apparent - pallor of skin and mucus membranes (cutaneous vasoconstriction) - fatigue, lethargy, cold intolerance and cell metabolism decrease - irritability (CNS response to hypoxia) - degenerative change (brittle hair, spoon-shaped concave and ridged nails) - stomatitis and glossitis inflammation in oral mucosa and tongue (respectively) - menstrual irregularities - delayed healing - tachycardia, heart palpitations, dyspnea and perhaps syncope (fainting) as anemia severe |
|
|
Diagnostic Tests of Iron Deficient Anemia - lab test demonstrated low values of Hemoglobin, hematocrit, mean corpuscular volume and mean corpuscular hemoglobin, serum ferritin and serum iron and transferrin saturation. - microscopic exam: erythrocytes appear hypochromic and microcytic |
Treatment for Iron Deficient Anemia - depend on cause - iron-rich foods or iron supplements in the least irritation and easily absorbable forms - take iron with food to reduce gastric irritation and nausea - iron supplements lead to constipation - liquid iron stain teeth and dentures and straw should be used. |
|
|
TA 10-3 a) explain how chronic bleeding leads to iron deficiency anemia = Hemoglobin leaves the body, and iron is not recycled and returned to the bone marrow for the production of new hemoglobin in erythrocytes. Only a small proportion of iron in the diet is absorbed; therefore, an iron deficit results. |
TA 10-3 b) Explain the signs of anemia that indicate compensation for hypoxia is occurring = Signs of anemia are tachycardia and pallor (peripheral vasoconstriction). |
|
|
TA 10-3 c) explain how destruction of acid-producing cells in stomach can lead to iron deficiency anemia = Incomplete digestion in the stomach can lead to a decrease in the absorption of iron in the duodenum, thus limiting hemoglobin production. |
Pernicious Anemia - Vitamin B12 Deficiency (Megaloblastic Anemia) - very large, immature, nucleated erythrocytes - results from deficit of folic acid (Vitamin B 9) or cyanocobalamin (Vitamin B 12) Vit B 12 promotes maturation of erythrocytes - folic acid deficiency during first 2 months of pregnancy increases risk for spina bifida and other spinal abnormalities in child - recommended women pregnant take folic acid supplement - prototype of megaloblastic anemia is pernicious anemia, a vitamin B 12 deficiency |
|
|
Pathophysiology of Pernicious Anemia - Vitamin B12 Deficiency (Megaloblastic Anemia) - malabsorption of vitamin B 12 owing to lack of intrinsic factor (IF) produced in glands of gastric mucosa (parietal cells secrete IF into stomach) - IF must bind with Vitamin B 12 (in stomach) to enable absorption of vitamin in lower ileum. = Vit B 12 promotes maturation of erythrocytes - additional problem: atrophy of mucosa because parietal cells can no longer produce hydrochloric acid Achlorhydria interferes with early digestion of protein in stomach and absorption of iron = iron deficiency anemia may be present as well. |
Pathophysiology of Pernicious Anemia - Vitamin B12 Deficiency (Megaloblastic Anemia) - impaired maturation of erythrocytes owing to interference of DNA synthesis (RBCs large - megaloblasts or macrocyte) contain nuclei. - large erythrocytes are destroyed prematurely resulting in low erythrocyte count or anemia (hemoglobin in RBC is normal) but maturation of granulocytes affected resulting in development of abnormally large hypersegmented neutrophils. - Thrombocytes may be low - lack of VitaminB12 direct cause of demyelination of peripheral nerves and eventually spinal cord |
|
|
Etiology of Pernicious Anemia - Vitamin B12 Deficiency (Megaloblastic Anemia) - dietary insufficiency rarely cause this anemia (because very small amounts of Vit B12 are required) source of this vitamin is animal foods, vegetarians/vegans must ensure they take enough. - malabsorption (in older individuals) from chronic gastritis (common in alcoholics and cause atrophy of gastric mucosa or inflammatory condition (regional ileitis) - outcome of surgical procedures as gastrectomy (removal or resection of part of stomach) - parietal cells removed, resection of ileum (site of absorption) |
Signs & Symptoms Pernicious Anemia - Vitamin B12 Deficiency (Megaloblastic Anemia) 1. tongue is typically enlarged, red, sore and shiny 2. decrease in gastric acid leads to digestive discomfort often with nausea and diarrhea 3. neurologic effects: tingling or burning sensations (paresthesia) in extremities or loss of coordination and ataxia (loss of full control of bodily movements) |
|
|
Diagnostic Tests Pernicious Anemia - Vitamin B12 Deficiency (Megaloblastic Anemia) - erythrocytes appear macrocytic or megaloblastic and nucleated on microscope, reduced number in peripheral blood - bone marrow is hyperactive (increased # of megaloblast), Granulocytes are hypersegmented and decreased in # - Vit B 12 level below normal (Schilling's test, oral dose of radioactive vitamin B12 used to measure absorption) - Presence of hypochlorhydria or achlorhydria confirms presence of gastric atrophy |
Treatment of Pernicious Anemia - Vitamin B12 Deficiency (Megaloblastic Anemia) - oral supplements as prophylaxis for pregnant women and vegetarians - vit B12 administered injection as replacement therapy - prompt diagnosis and treatment prevents cardiac stress and neurologic damage |
|
|
TA 10-4 a) explain why individuals with pernicious anemia have a low hemoglobin level = The abnormally large erythrocytes are damaged in the capillaries and break down prematurely, resulting in a very low RBC count and thus a low hemoglobin value. |
TA 10-4 b) Explain how pernicious anemia can cause neurologic effect (tingling sensation in extremities or loss of coordination) = Demyelination of peripheral nerves occurs because of the lack of vitamin B12; this degenerative change interferes with nerve function, resulting in numbness or paresthesias and loss of coordination. |
|
|
TA 10-4 c) why is oral administration of vit B12 not effective as a treatment for pernicious anemia? = Oral vitamin B12 is not absorbed because of a deficit of IF. |
Aplastic Anemia Pathophysiology - results from impairment or failure of bone marrow = loss of stem cells and pancytopenia = (decreased numbers of erythrocytes, leukocytes and platelets in blood) - these deficits lead to many serious complications - bone marrow exhibits reduced cell components and increased fatty tissue |
|
|
Etiology of Aplastic Anemia (causes) - may be temp. or permanent depending - mostly middle-aged, cause is unknown (idiopathic - primary type) - Myelotoxins (radiation, industrial chemicals (e.g. benzene) and drugs (e.g. chloramphenicol, gold salts, phenylbutazone, phenytoin and antineoplastic drugs) may damage bone marrow if severe aplastic anemia due to cancer treatment is a risk - Viruses (particularly Hepatitis C) - Autoimmune Disease (systemic lupus erythesamtosus (SLE) may affect bone marrow - Genetic Abnormalities (myelodysplastic syndrome or Fanconi's anemia may affect bone marrow function) |
Signs and Symptoms of Aplastic Anemia - majority cases: onset is insidious (because entire bone marrow affected) manifestations include 1. Anemia (pallor, weakness, and dyspnea) 2. Leukopenia (recurrent or multiple infections) 3. Thrombocytopenia (petechiae: flat, red, pinpoint hemorrhages on skin and tendency to bleed excessively particularly in mouth) - as blood count diminish, (WBCS and platelets) = uncontrollable infection and hemorrhage |
|
|
Diagnostic Test Aplastic Anemia - Blood counts indicate pancytopenia - bone marrow biopsy may be required to confirm cause of pancytopenia (erythrocyte normal appearance) |
Treatment of Aplastic Anemia - removal of any bone marrow suppressants to recover bone marrow - bone marrow transplantation (success depends on accuracy of tissue match using HLA) - chemotherapy and radiation used to prepare recipient's bone marrow - anti-rejection drug required for a year - common complication include damage to digestive tract from perp treatment, infection resulting from immune suppression and rejection reactions |
|
|
TA: 10-5 a) explain why bone marrow damage can result in multiple, recurring infections = Stem cells for leukocytes are not produced, decreasing the effectiveness of the body’s immune reaction to an infection. b) Explain why excessive bleeding occurs with aplastic anemia = Excessive bleeding occurs with aplastic anemia because of thrombocytopenia. |
TA: 10-5 c) Explain why it is necessary to treat bone marrow recipient with chemotherapy and radiation before transplant? - Treatment prepares the recipient’s bone marrow for the donor stem cells, preventing rejection. |
|
|
Hemolytic Anemias - result from excessive destruction of RBCs or hemolysis leading to low erythrocyte count and low total hemoglobin - causes: genetic defects affecting structure, immune reactions, changes in blood chemistry and presence of toxins in blood, infections (malaria, transfusion reactions and blood incompatibility in neonate (erythroblastosis fetalis) |
Examples of Hemolytic Anemias - Sickle Cell Anemia and Thalassemia Sickle Cell Anemia: Pathophysio: large # of similar hemoglobinopathies. - inherited characteristics leads to formation of abnormal hemoglobin, hemoglobin S (HbS) - one amino acid in pair of beta-globin chains have been changed from normal glutamic acid to valine. -when altered hemoglobin is deoxygenated, crystallizes and changes shape of RBC from disc to crescent or "sickle" shape - cell membrane damaged = hemolysis and have much shorter lifespan than normal (~20 days instead of 120 days) - initially: sickling maybe reversible when increased oxygen available but after several episodes, damage to RBC is irreversible and hemolysis occurs. - Hemoglobin S can transport oxygen normally but erythrocyte count is very low = low hemoglobin level in blood |
|
|
Sickle Cell Pathophysiology - obstruction of small blood vessels by elongated and rigid RBCs = thrombus formation and repeated multiple infarctions (areas of tissue necrosis) - deoxygenation of hemoglobin may occur in peripheral circulation as oxygen content of blood reduces, leading to repeated minor infarctions - serious crisis for people with lung infection or dehydration when basic oxygen levels are reduced - during sicking crisis: many larger blood vessels may be involved and multiple infarctions occur affecting brain, bones, or organs = significant damage and loss of function occur in organ systems - high rate of hemolysis = hyperbilirubinemia, jaundice and gallstones. |
Etiology of Sickle Cell Anemia - gene for HbS recessive and common in individuals from African and Middle East - homozygotes most normal hemoglobin (hemoglobin A [HbA] is replaced by HbS = clinical signs of sickle cell anemia - heterozygotes less than half the hemoglobin is abnormal HbS = clinical signs occur only with severe hypoxia = pneumonia or high altitudes this condition is termed sickle cell trait - carrier pop is Africa very high owing to a decreased incidence of malaria in those with HbS |
|
|
Sickle Cell Anemia - the effects of Sickling Fig 10-17 - Normal: RBCs containing HbS in presence of oxygen are flexible discs - Sickle cell: when O2 level is low, RBC sickle become elongated and rigid - as blood circulated thru body, oxygen levels may decrease - erythrocytes sickle and unable to pass thru small arteries - cell membrane damaged and RBC has short lifespan -1. increased hemolysis of RBC in spleen (decreased RBC, severe anemia) = Hyperbilirubinemia (Jaundice) or 2. Occlusion of Small Arteries - tissue damage and multiple infarctions, Pain, loss of function |
Signs & Symptoms of Sickle-Cell Anemia - do not appear until child is about 12 months (fetal HbF replaced by HbS) proportion of HbS in erythrocyte determines severity of condition. - severe anemia causes pallor, weakness, tachycardia and dyspnea - hyperbilirubinemia indicated by jaundice (yellowish color most obvious in sclerae of eyes) high bilirubin in bile may cause development of gallstones. - splenomegaly (enlargement of spleen) common in young people: sickled cells cause congestion - in adults: the spleen is smaller and fibrotic owing to recurrent infarction - vascular occlusions and infarctions lead to periodic painful crises and permanent damage to organs and tissues (ex: ulcers on legs and feet, areas of necrosis in bones or kidneys or seizures or hemiplegia = result from cerebral infarctions ( stroke), pain can be quite intense - in lungs: occlusions and infection cause acute chest syndrome with pain and fever (diagnosed with x-ray and frequent cause of death) - occlusions in smaller blood vessels of hands or feet cause hand-foot syndrome (pain and swelling early signs in children) - growth and development delayed: late puberty common. tooth eruption is late and hypoplasia common. Intellectual development usually impaired |
|
|
Signs & Symptoms of Sickle-Cell continued - congestive heart failure owing to efforts to improve supply of oxygen and increased peripheral resistance caused by obstruction - frequent infection = decreased defenses when spleen can no longer filter blood adequately, presence of necrotic tissues and poor healing capabilities. Pneumonia common cause of death in children. Infections lead to more sickling and vicious cycle develops |
Diagnostic Tests for Sickle Cell Anemia - carriers detected by simple blood test (hemoglobin electrophoresis) - useful in alerting those with sickle cell trait to avoid severe hypoxia and sickling episodes (e.g. with severe anemia, surgery or at high altitude) - prenatal diagnosis can be checked by DNA analysis of fetal blood (children more than 1 years: detect presence of sickled cell in peripheral blood and presence of HbS. Bone marrow is hyperplastic and more reticulocytes (immature RBCs) released into circulation |
|
|
Treatment for Sickle-Cell Anemia - hydroxyurea (Hydrea) reduced frequency of crises and prolonged lifespan for many but not effective for all. - dietary supplement folic acid (folate) recommended even during asymptomatic periods - avoid strenuous activity or high altitudes helpful. - prevent dehydration, acidosis, infection or exposure to cold (increase sickling tendency and painful crises) - children should be immunized against pneumonia, influenza and meningitis - continued prophylactic penicillin used for young children and adults with severe cases - bone marrow transplant effective but limited to number of African American donors on bone marrow registries |
TA 10-6 a) explain why vascular occlusions common in patients with sickle cell disease = Low O2 levels result in sickle-shaped RBCs that obstruct the arteries, causing thrombi to form. |
|
|
TA 10-6 b) Compare sickle cell trait and sickle cell anemia in terms of genetic factor, the amount of HbS present, and presence of clinical signs = Sickle cell trait occurs in heterozygotes (only one gene for HbS present), only a small amount of HbS is present, and sickling and clinical signs only occur when severe hypoxia is present. Sickle cell anemia occurs in homozygotes, who inherit the defective gene from both parents, resulting in blood containing primarily HbS; therefore, clinical signs occur frequently. |
Hemolytic Anemia: Thalassemia - pathophysio: anemia results from genetic defect when one or more genes for hemoglobin are missing or variant. - when two genes involved: thalassemia is moderate to severe. (abnormal: interferes with production of globin chains, = amount of hemoglobin synthesized and # of RBCs reduced) - normal: hemoglobin contains 4 globin chains, 2 alpha and 2 beta |
|
|
Thalassemia alpha = reduction in or lack of alpha chains - less normal hemoglobin can be made - missing chains: also accumulation of other available chains damaging RBCs. Ex: when beta chains missing, extra alpha chains collect in RBCs and damage cell membrane = lead to hemolysis and anemia - Homozygotes have thalassemia major ( Cooley's anemia) severe form of anemia: heterozygotes have thalassemia minor and exhibit mild signs of anemia - severe case: increased hemolysis of RBCs aggravates anemia and causes splenomegaly, hepatomegaly, and hyperbilirubinemia. - bone marrow is hyperactive trying to compensate |
Etiology of Thalassemia - most common genetic disorder in the world, occurs in 2 common forms - Thalassemia beta (autosomal dominant inheritance) occurs frequently in people from Mediterranean countries (Green or Italy) and (more common form) - Thaleassemia alpha: found in those of Indian, Chinese or Southeast Asian descent. because more than 1 gene involved, many possible gene mutations with varied effects on hemoglobin synthesis and severity of resultant anemia. |
|
|
Signs and Symptoms of Thalassemia - usual signs of anemia and increased hemolysis - child's growth and development impaired directly by hypoxia and indirectly by fatigue and inactivity. - hyperactivity in bone marrow: invasion of bone and impairs normal skeletal development - heart failure develops as a result of compensation mechanism increasing cardiac work load |
Diagnostic Tests for Thalassemia - RBCs microcytic (varying in size and hypochromic (low hemoglobin)) = increase in eyrthropoietin levels - often iron overload exists - prenatal diagnosis done by chorionic villus assay at 12 weeks or by amniocentesis at 16 weeks. |
|
|
Treatment of Thalassemia - blood transfusions only treatment available - iron chelation therapy may be necessary to remove excess iron from numerous transfusions - administration of folate recommended - bone marrow transplant have been curative in some children - mild patients form have normal lifespan and those with moderate to severe disease live into 30s with transfusions and chelation therapy. |
Blood- Clotting Disorders - spontaneous bleeding or excessive bleeding following minor tissue trauma - warning signs may be caused by other factors (infections, damaged or fragile blood vessels (e.g. Vitamin C deficit) |
|
|
Iron Deficiency Anemia - Microcytic, Hypochromic RBCs - Decreased Hemoglobin production - Etiology: decreased dietary intake, malabsorption, blood loss - Additional: only effects of anemia |
Pernicious Anemia - Megaloblasts (immature nucleated cells) RBCs - short lifespan - Etiology: deficit of intrinsic factor owing to immune reaction - Neurologic damage Achlorhydria |
|
|
Aplastic Anemia - Often normal RBCs - Pancytopenia - Etiology: Bone marrow damage or failure - Excessive bleeding and multiple infections |
Sickle-Cell Anemia - RBC elongates and hardens in "sickle" shape when O2 levels are low- short life span - Etiology: Recessive inheritance - Painful crises and multiple infarctions, Hyperbilirubinemia |
|
|
Warning signs of Excessive bleeding and possible blood-clotting disorders - persistent bleeding fro gums - Petechiae : pinpoint flat red spots on skin or mucous membranes, result from bleeding from capillary or small arteriole - frequent purpura and ecchymoses (large, purplish red or greenish areas on skin (bruises)- more persistent bleeding - coughing up blood (hemoptysis) bright red flecks in sputum - vomiting blood, hematemesis - blood in feces often black (tarry) or occult (hidden) - Anemia - feeling faint and anxious, Low blood pressure and rapid pulse |
Causes from Excessive Bleeding - Thrombocytopenia : may be caused by acute viral infections in children or autoimune reactions in adults (chronic idiopathic thrombocytopenic purpura) - chronic form usually in adults (young women) when thrombocytes are destroyd by antibodies. HIV infection, hepatomegaly and splenomegaly and certain drugs also lead to thrombocytopenia. - chemotherapy, radiation treatments and cancers (leukemia- also reduce platelet counts causing bleeding) |
|
|
Excessive bleeding has many causes - defective platelet function associated with uremia (end-stage kidney failure) and ingestion of aspirin (ASA), avoid ASA or ASA and NSAIDS containing drugs if bleeding disorder - Vitamin K deficiency may cause decreases in prothrombin and fibrinogen levels, occur in patients with liver disease (with decreased bile production and those with malabsorption problems) Vit K fat soluble produced by intestinal bacteria and present in some foods. * Vit K useful antidote when excess warfarin (Coumadin) oral anticoagulant causes bleeding |
Excessive bleeding has many causes - liver disease reduces available bleeding disorders resulting from deficiency of one of clotting factors, serum factor analysis and more specific tests useful Include PT to measure extrinsic pathway, activated partial thromboplastin time (APTT) measure intrinsic pathway and thrombin time for final stage, fibrinogen to fibrin. - Hemorrhagic fever viruses (Ebola virus) cause excessive bleeding and acute illness (affecting many organs) - anticoagulant drugs (warfarin (Coumadin) for long-term and patient's hemostatic ability requires close monitoring |
|
|
Patient with any bleeding disorder at risk for hemorrhage because of invasive procedure (prepare lab test to check current blood clotting status and administer prophylactic medications if needed) - app pressure, cold dressings and absorbable hemostatic packing agents (Gelfoam or Oxygel and styptics) |
Hemophilia A pathophysiology - classic hemophilia is deficit of abnormality of clotting factor VIII and most common inherited clotting disorder - 90% patients have TYpe A. - defect causing hemophilia A is transmitted as an X-linked recessive trait (manifest in men but carried in women- asymptomatic) - with improved treatment and longer lifespan of men (pattern could change) - an affected man and a carrier woman could produce female child who inherits gene from both parents |
|
|
Hemophilia B (Christmas disease) - similar and involves deficit of factor IX; Hemophilia C (Rosenthal's hemophilia) - milder form resulting from decrease in factor XI. *some cases of hemophilia result from spontaneous gene mutation in a person with no previous family history of disease |
Milder forms: more than 5% factor VIII activity, excessive bleeding occurs only after trauma, frequent spontaneous bleeding common in people with severe deficiencies (less than 1% factor III activity) ~ 70% of affected individuals have severe form. |
|
|
SIGNS & Symptoms of Hemophilia A - prolonged or severe hemorrhage occurs following minor tissue trauma - persistent oozing of blood after minor injuries and hematomas is common - spontaneous hemorrhage into joints (hemarthrosis) ay occur (causing painful and crippling deformities resulting from recurrent inflammation) - blood may appear in urine (hematuria) or feces (bleeding in kidneys or digestive tract) |
Diagnostic Test of Hemophilia A - bleeding Time and PT normal but PTT and APTT and coagulation time are prolonged - serum levels of factor VIII are low - thromboplastin generation time differentiates between deficits of factor VIII and factor IX |
|
|
Treatment of Hemophilia A - desmopressin (DDAVP) may raise clotting factor levels in some patients - stimulates endothelium lining of blood vessels to release stored factor VIII. - replacement therapy for factor VIII available for intravenous administration at regular intervals (esp before any surgical or dental procedure) - Hepatitis and HIV transmits thru blood products - risk of unknown infection - newer recombinant DNA product (Advate) produced through genetic engineering does not contain any material such as proteinf rom human or animal blood - Nplate stimulates platelet production in bone marrow |
von Willebrand Disease Pathophysio - most common hereditary blood clotting/bleeding disorder - caused by deficiency of the von Willebrand factor (clotting factor helps platelets clump and stick to walls of blood vessels where damage occurs) - 3 major types of disease (similar signs and symptoms but much milder than hemophilia) |
|
|
Signs & Symptoms of von Willebrand Disease - skin rashes, frequent nosebleeds, easy bruising, bleeding of gums and abnormal menstrual bleeding - |
Diagnostic tests of von Willebrand Disease - bleeding time, blood typing, factor VIII levels, platelet count and aggregation test, ristocetin cofactor test and von Willebrand factor specific test |
|
|
Treatment for von Willebrand Disease - required in cases like surgery, tooth extraction, or accident trauma. - manmade hormone desmopressin (treat mild cases) - injection or nasal spray of hormone causes increased release of von Willebrand factor and factor VIII into bloodstream - can be injected into vein (replacement therapy) - Antifibrinolytic drugs help prevent breakdown of blood clots (used after minor surgery or injury) - women with abnormal menstrual flow caused by this disease can be treated with birth control (cause increase in release of clotting factors) |
Disseminated Intravascular Coagulation Pathophysiology - Disseminated intraascular coagulation (DIC) is a condition (often life-threatening) involves both excessive bleeding and excessive clotting - complication of numerous primary problems which activate clotting process in microcirculation throughout body - clotting may be induced by release of tissue thromboplastin or by injury to endothelial cells causing platelet adhesion - cause multiple thromboses and infarctions but consumes available clotting factors and platelets and stimulate fibrinolytic process. - result consumption of clotting factors and fibrinolysis = leads to hemorrhage and hypotension or shock - Chronic DIC milder form- difficult to diagnose - blood counts may be normal or abnormal (usually caused by chronic infection and thromboembolism (dominant feature) |
|
|
Etiology of DIC - variety of disorders can initiate DIC - may result from obstetric complication (toxemia, amniotic fluid embolus or abruptio placenta (tissue thromboplastic released from placenta - infection (gram-negative) leads to endotoxins cause endothelial damage or stimulate release of thromboplastin from monocytes - many carcinomas release substance that trigger coagulation - major trauma (burns or crush injuries and widespread deposits of antigen-antibody complexes results in endothelial damage = release thromboplastin and initiating process. |
Signs and Symptoms of DIC - Obstetric patients usually manifest increased bleeding - cancer patients have more thromboses - hemorrhage is critical problem (low plasma fibrinogen level, thrombocytopenia and prolonged bleeding time, PT, APTT, and thrombin time - accompany hemorrhage effects of low blood pressure or shock - vascular occlusions frequently present in small blood vessels (affect large vessels, causing infarcts in brain or organ) - neurologic effects: seizures and decreased responsiveness - acute renal failure with oliguria often accompanies shock |
|
|
Treatment of DIC - difficult depend on whether hemorrhages or thromboses are dominant - infection must be treated successfully (excessive clotting or hemorrhage) prognosis depends on severity of primary problem |
Thrombophilia pathophysiology - group of inherited or acquired disorders that increase risk of development of abnormal clots in veins or arteries - abnormal clotting events can result in conditions (deep venous thrombosis, pulmonary embolism or peripheral vascular disease) - inherited thrombophilias result of mutations among genes responsible for producing coagulation proteins in blood - commonly occur during surgery, injury or other medical conditions allow for increase of amount of clotting factors in blood or accumulation of antibodies |
|
|
Signs & Symptoms of Thrombophilia - can affect any organ or system in which clot may lodge and cut off blood supply - clot lodges in heart or vessels of lungs result can be myocardial infarction or acute stroke |
Diagnosis of Thrombophilia - blood testing for clotting factor levels and abnormal antibody levels |
|
|
Treatment of Thrombophilia - treat causative condition to decrease potential of acquired thrombophilia - anticoagulants (warfarin- Coumadin) prescribed to reduce risk of abnormal clot formation - use of these meds must be weighed with risks for excessive bleeding due to interruption of normal coagulation capability of blood |
TA 10-7 a) state the probability that a child with a carrier mother will have hemophilia A The probability that a male child will have hemophilia A with a carrier mother is 50% affected; a female child's probability is 50% carrier. |
|
|
TA 10-7 b) Describe briefly 3 causes of excessive bleeding other than hemophilia = Excessive bleeding may be caused by a vitamin K deficit, which impairs production of clotting factors, liver damage, thrombocytopenia resulting from ITP, and certain toxins, infections, and drugs. |
TA 10-7 c) Explain how a deep vein thrombosis in a large vein in leg can result in a life-threatening condition (stroke or myocardial infarction? = A clot in a large vein can break loose, travel to the heart, and block the blood supply, causing a stroke or infarction of the heart muscle. |
|
|
Myelodysplastic Syndrome MDS - excludes disorders such as aplastic anemias and deficiency dyscrasias - may be idiopathic or occur following chemotherapy or radiation treatment for other cancers. - diagnosis based on patient's history, standard blood tests and bone marrow biopsy. - treatment measure depends on type of deficiency and include transfusion replacements, chelation therapy to reduce iron levels and supportive therapies to prevent complications |
Low level chemotherapy may be used to reduce iron levels and supportive therapies to prevent complication - low level chemotherapy may be used with growth factors to stimulate more normal bone marrow function - bone marrow transplants are curative but often patient's health will not allow this treatment - prognosis for patients with MDS dependent on age of onset, past treatment with chemotherapy or radiation and response to treatment. |
|
|
Sickle cell Anemia and Thalassemia are caused by - inherited defects in hemoglobin synthesis - result in excessive hemolysis and low erythrocyte count |
Polycythemia may occur as primary or secondary problem - increased RBCs cause vascular congestion |
|
|
Myelodysplastic syndrome is comprised of a number of conditions which bone marrow does not produce adequate cellular elements for blood, may be related to prior history of chemo or radiation |
Leukemias may be acute or chronic - named by specific neoplastic cell that is proliferating excessively in bone marrow - malignant cells are immature and nonfunctional (increasing risk of infection) Thrombocytopenia and anemia present. |
|
|
WHy are multiple opportunistic infections common in patients with leukemia? = Multiple opportunistic infections are common in patients with leukemia because of impaired defenses caused by immature, nonfunctional WBCs. |
Compare contrast characterisitics of acute and chronic leukemias (age groups, onset and typical blood cell characteristics) = Acute leukemias—children and young adults, sudden onset, high WBC count, many blast cells Chronic leukemias—older adults, insidious onset, WBC count elevated, some blast cells |
|
|
Chapter 11 |
Lymphatic System Disorders |
|
|
Lymphatic System - Return of excess interstitial fluid to the cardiovascular system - Vessels empty into the subclavian veins. - Filter and destroy foreign materialInitiate the immune response - Absorb lipids from the GI tract |
Lymphatic Vessels Originate as capillaries in contact with blood capillary bed in tissues Lymph collected by lymphatic trunks Lymphatic trunks empty into ducts Ducts empty into the subclavian veins |
|
|
Lymph = Clear, watery, isotonic fluid Circulates in lymphatic vessels Resembles blood plasma, with a lower protein content Returned to the cardiovascular system |
Lymphomas (disorder) Malignant neoplasms involving lymphocyte proliferation in lymph nodes Specific causes not identified - Higher risk in adults who received radiation during childhood Two main disorders: Hodgkin’s lymphoma and Non-Hodgkin’s lymphoma Distinguished by multiple node involvement Nonorganized, with widespread metastases |
|
|
Hodgkin's Lymphomas Initially involves a single lymph node Cancer spreads to adjacent nodes - To organs via lymphatics - T lymphocytes seem to be defective; lymphocyte count decreased - Presence of Reed-Sternberg cells - Giant cells present in lymph node - Four subtypes - Based on cell found at biopsy |
Hodgkin's Lymphomas Symptoms First indicator—usually a painless enlarged lymph node Later—splenomegaly and enlarged lymph nodes General signs of cancer: Weight loss, anemia, low-grade fever, night sweats; fatigue may develop. Treatment: Radiation, chemotherapy, surgery Staging and prognosis dependent on: Number of nodes involved Location of nodes involved |
|
|
Non-Hodgkin's Lymphoma Increasing in incidence Partially caused by HIV infection Similar to Hodgkin’s lymphoma Clinical signs and symptoms are similar. More difficult to treat when tumors are not localized Initial manifestation—enlarged, painless lymph node |
Multiple Myeloma Neoplastic disease that involves increased production of plasma cells in bone marrow - Unknown cause: Occurs in older adults - Production of other blood cells is impaired - Multiple tumors in bone - Loss of bone - Severe bone pain Prognosis poor, with short life expectancy |
|
|
Signs and Symptoms of Multiple Myeloma Onset usually insidious Malignancy well advanced before diagnosis Pain caused by bone involvement Anemia and bleeding tendency Impaired kidney function and eventually failure Chemotherapy to encourage remission Median survival, 3 years |
Lymphedema Obstruction of lymphatic vessels Most common form is congenital Extremities swell because of lymph accumulation Treatment: - Diuretics - Bed rest - Massage of affected area Elevation of affected extremity |
|
|
Elephantiasis = Lymphedema Caused by blockage because of parasitic infection - Significant swelling of affected extremity - Extreme swelling of legs, breast, and/or genitalia - Thickening of subcutaneous tissue - Frequent infections - Skin ulcerations - Fever Treatment—medication regimen to kill parasite |
Castleman's Disease Rare illness Involves overgrowth of lymphoid tissue Two types: Unicentric form = Affects a single lymph node Multicentric form = Affects multiple lymph nodes and tissue—may have severe effects on the immune system Signs, symptoms, and treatment depend on the type of the disease |
|
|
In which blood does pancytopenia develop? = Aplastic anemia |
What is the cause of oral ulcerations and delayed healing occurring with any severe anemia? = Deficit of oxygen for epithelial cell mitosis and metabolism |
|
|
What causes numbness and tingling in the fingers of individuals with untreated pernicious anemia? = Vitamin B12 deficit causing peripheral nerve demyelination |
Why is excessive bleeding a common occurrence with acute leukemia? = Decreased platelets |
|
|
The function of the hormones secreted by the thymus gland is to: = enable lymphocytes to develop into mature T cells. |
A rare illness that involves the overgrowth of lymphoid tissue, although not itself considered a cancer is: = Castleman disease. |
|
|
The spleen has a number of important functions, which include: = hematopoiesis, destruction of old erythrocytes, blood reservoir. |
Multiple myeloma is a neoplastic disease of unknown etiology occurring in older adults and involving: = plasma cells. |
|
|
The staging system typically used in determining the stage of the Hodgkin's lymphoma is the: = Ann Arbor system. |
One of the reasons non-Hodgkin's lymphomas are harder to treat than Hodgkin's lymphomas is that they: = involve multiple nodes and widespread metastases. |
|
|
Malignant neoplasms involving lymphocyte proliferation in the lymph nodes are called: = lymphomas |
Anemias may be caused by - dietary deficits - malabsorption syndromes - genetic defects - damage to bone marrow - blood loss |
|
|
Name 6 substances that are transported in blood and function of each - Substances transported in the blood and their functions follow: oxygen: cell metabolism and energy; hormones: cell metabolism; glucose, amino acids, and other nutrients: cell growth and reproduction; cells—red blood cells: oxygen, white blood cells: defense, thrombocytes: clotting; clotting factors (e.g., prothrombin): hemostasis; wastes (e.g., carbon dioxide, urea, lactic acid): to be removed; buffers: maintain serum pH; electrolytes (e.g., sodium): fluid balance, metabolism; and antibodies and phagocytic cells: remove foreign material. |
Explain importance/function of each a) high elastic fiber content in aorta High elastic content in the aorta allows for expansion during systole and recoil during diastole and prevents extreme high or low blood pressure. b) Smooth muscle in arterioles Smooth muscle controls peripheral resistance by vasoconstriction, capacity of the cardiovascular system, blood pressure, and distribution of blood in the body. |
|
|
c) Extensive capillaries in liver and lungs - The large surface area for the liver allows for exchange of nutrients and removal of wastes; in the lungs, extensive capillaries permit gas exchange; valves in veins prevent back flow and assist venous return. |
Explain the cause of incompatible blood transfusion = Individual blood type depends on which antigens are on the red blood cells. The plasma contains antibodies, which may not be compatible with another person’s blood. For example, a person with type A blood (with A antigens on the red blood cells) has anti-B antibodies in the plasma and therefore would have an antigen-antibody reaction if the person received type B blood. Rh incompatibility is also possible. |
|
|
4. List 3 types of clotting problems = Blood clotting is impaired by a deficit of platelets or other clotting factors, - lack of vitamin K, liver failure, or interference with the clotting process by drugs or other agents. |
5. Explain how pernicious anemia may develop from chronic gastritis = Gastritis leads to atrophy of the gastric mucosa and glands and less secretion of intrinsic factor in the stomach. Vitamin B12 is not absorbed in the ileum unless intrinsic factor is available for transport. |
|
|
6. For which conditions could secondary polycythemia develop as compensation? VSD, CHF, chronic lung disease, aplastic anemia, multiple myeloma = Secondary polycythemia could develop as compensation in cases of VSD, CHF, and COPD. |
7. Explain how DIC develops and state two signs of its development = DIC develops as a complication when the clotting process is activated, using up available clotting factors, eventually resulting in hemorrhage. Signs are purpura, decreased BP, and thrombocytopenia. |
|
|
8. Explain why severe bone pain occurs with leukemia Proliferation of malignant cells in the bone marrow causes pressure on nerves in the surrounding rigid bone. |
Lymphatic System Disorders |
|
|
Lymphatic system consists of - lymphatic vessels, lymphoid tissue (palatine and pharyngeal tonsils, lymph nodes, the spleen and thymus gland) |
Lymphatic vessels - originate as microscopic capillaries direct contact with tissue cells and interstitial fluid surrounding cell - capillaries form branches, then trunks and finally ducts - ducts empty into left and right subclavian veins - have thinner walls than veins, more valves and contain nodes at certain intervals (thinner walls allow increased permeability allowing large molecules and some particulate matter to be removed from interstitial space) |
|
|
Proteins that eventually accumulate in interstitial fluids can only be returned to blood system through lymphatic vessels - dramatic effect on blood protein concentration and osmotic pressure (serious or fatal results) affect normal return from lymphatic vessels to blood vessels |
Lymph capillaries in villi (small intestines) = Lacteals - absorption of fats and other nutrients that are produced as a result of digestion |
|
|
Lymph nodes and lymphoid tissue act as a defense system - removing foreign or unwanted material from lymph fluid before it enters general circulation |
During Infection - regional lymph nodes often swollen and tender Ex: upper respiratory infection causes enlarged nodes in neck area -lymph nodes containing many lymphocytes and macrophages are situated along all lymphatic and blood vessels = ensuring constant filtration and surveillance of body fluids - lymph nodes are essential to immune response and sensitization of B and T lymphocytes |
|
|
Palatine and Pharyngeal Tonsils - composed of: lymphoid tissue located in a ring under mucous membrane of mouth and at back of throat - tonsils function as protection against bacterial infection (area of openings between nasal and oral cavities)= first line of defense from invasion by external organisms and subject to infections (tonsillitis) |
Spleen - located on left side of abdominopelvic activity below diaphragm - surrounded by a fibrous capsule and internally divided into compartments - blood passes thru spleen (macrophages remove microorganisms from blood and destroy them thru phagocytosis) - in hematopoiesis: monocytes and lymphocytes mature and become activated in spleen (before birth erythrocytes formed - in spleen) - after birth, the spleen responsible for RBC formation (in extreme cases of hemolytic anemia) |
|
|
function of RBC and platelet destruction - carried out by macrophages and destroy old blood cells and platelets thru phagocytosis - also break down hemoglobin molecules from destroyed RBCs and salvage iron and globin portion of hemoglobin, returned to blood circulation for storage in liver and bone marrow |
Spleen - blood reservoir contains large amounts of blood in pulp and venous sinuses (large reservoir damages spleen: severe trauma) - this blood can be quickly returned to circulatory system if needed |
|
|
Thymus gland - 2 lobes (located in mediastinum) - lying in front of the top half of heart and extending up the neck to bottom of thyroid gland - covered by fibrous capsule extends inward and subdivide lobes into small lobules - critical role in immunity mechanism against infection = 2 primary functions: final site of lymphocyte development before birth and secretion of hormones after birth (enable lymphocytes to develop into mature T cells *T cell functions to attack foreign or abnormal cells and regulators of immune function (extremely important) |
Composition and Production of Lymph - Lymph: clear, watery, isotonic fluid circulate in lymphatic vessels - Lymph & ISF almost chemically identical when taken from same part of body (closely resemble blood plasma) but contain lower protein % than plasma except in thoracic duct |
|
|
In thoracic duct - lymph is protein rich - outflow into duct from liver and small intestine - ISF not absorbed by cells/capillaries tends to accumulate in Interstitial spaces and fluid builds it will drain into lymphatic vessels and become lymph |
Lymphatic Circulation 1. Begins with blind-ending capillaries containing one-way minivalves at terminus into excess interstitial fluid flows as pressure builds up in tissues 2. Lymphatic capillaries join to form larger vessels with valves to ensure a one-way flow of fluid, similar to network of veins - flow depends on pressure arising from movement of surrounding skeletal muscle and organs 3. Lymphatic vessels are interrupted periodically by more lymphocytes (enter lymph en route to general circulation) |
|
|
Lymphatic Circulation 4. Vessels of upper right quadrant empty into right lymphatic duct which returns lymph into general circulation via right subclavian vein 5. Remainder of lymphatic vessels drain into thoracic duct in upper abdomen and thoracic cavity (duct drains into left subclavian veins) 6. Lymphatic capillaries in intestinal villi absorb and transport most fluids as chylomicrons |
TA 11-1 a) Explain 2 purposes of lymphatic system = The lymphatic system is a defense, filtering lymph, removing foreign material, and activating the immune system when necessary. It also helps in the return of excess fluid and protein from the interstitial compartment through the open-ended lymphatic capillaries. Protein cannot pass back into vascular capillaries. |
|
|
11-1 b) predict the result of destruction of lymph nodes in specific region Edema is likely because excess fluid is not returned to the lymphatics. |
11-1 c) Under what circumstances might lymph nodes be surgically removed Removal may be required to check for the presence of malignant cells or if confirmed as malignant. |
|
|
Lymphatic Disorders - common infection involving lymphatic system, infectious mononnucleosis |
Lymphomas - malignant neoplasms involving lymphocyte proliferation in lymph nodes 2 main disorders: - Hodgkin's Lymphoma and Non-Hodgkin's Lymphoma (differentiated by lymph node biopsy) - how rapidly growing or aggressive tumor is * higher incidence in those who receive radiation treatments during childhood |
|
|
Hodgkin's disease/Hodgkin's Lymphoma Pathophysio - malignancy involves single lymph node (frequently in neck area) - later cancer spreads to adjacent nodes in orderly fashion then to organs via lymphatics - T- lymphocyte appear to be defective and lymphocyte count decreased - Atypical cell used as marker for diagnosis of Hodgkin's lymphoma = Reed-Sternberg Cell (giant cell present in the lymph node) |
4 subtypes of Hodgkin's disease based on cells found in biopsy (use diaphragm as differential landmark) - Ann Arbor Staging System: defines a - stage 1 cancer affecting a single lymph node or region and - stage II affecting two or more lymph node regions on same side - stage III cancer involves nodes on both sides of diaphragm and spleen - stage IV: diffuse extralymphatic involvement (bone, lung or liver) |
|
|
Signs & Symptoms of Hodgkin's Lymphoma 1. lymph node (cervical) large, painless and nontender 2. splenomegaly and enlarged lymph nodes at other locations may cause pressure effects: Ex: enlarged mediastinal nodes compress esophagus 3. General signs of cancer(weight loss, anemia, low-grade fever and night sweats, fatigue may develop. 4. Generalized pruritus common 5. Recurrent infection common because abnormal lymphocytes interfere with immune response |
Treatment of Hodgkin's lymphoma - radiation, chemotherapy, and surgery used with greater success - new drugs combos ABVD most effective |
|
|
Non-Hodgkin's Lymphomas - increasing incidence due to numbers associated with HIV infection - similar to hodkin's in some ways ~80% cases involve B lymphocytes - initial manifestation : enlarged painless lymph node - clinical signs, staging and treatment similar to hodgkin's lymphoma |
Non- Hodgkin's Lymphoma - distinguished by multiple node involvement scattered throughout body - non-organized pattern of widespread metastases (present at diagnosis) - Intestinal nodes and organs frequently involved in early stage - difficult to treat tumors not localized |
|
|
Multiple Myeloma or Plasma Cell Myeloma Pathophysiology - neoplastic disease of unknown etiology occurring in older adults - involve plasma cells (mature B lymphocytes produce antibodies) - increased # of malignant plasma cells replace bone marrow and erode bone - blood production impaired and production of antibodies - multiple tumors with bone destruction develop in vertebrae, ribs, pelvis and skull - pathologic or spontaneous fractures at weakened sites in bone common - hypercalcemia develops as bone is broken down - tumor cells spread throughout body into lymph nodes and infiltrating many organs |
Signs & Symptoms of Multiple Myeloma - onset usually insidious malignancy well advanced before diagnosis - frequent infections - pain (bone involvement) common and present at rest - pathologic fractures occur as bone weakened - anemia and bleeding tendencies common because blood cell production affected - kidney function (tubules) affected leading to proteinuria and kidney failure |
|
|
Treatment of Multiple Myeloma - chemotherapy used to encourage remission (median survival 3 years) - analgesic for bone pain and treatment for kidney impairment - blood transfusions required later stage |
TA 11-2 a) explain why infections occur frequently in patients with lymphomas = Infections occur frequently in patients with lymphoma because lymphocytes are abnormal, decreasing the immune response, and there is a lack of normal filtration and removal of foreign material. |
|
|
11-2 b) state prognosis for person with stage I and stage IV hodgkin's lymphoma and explain A person with stage I Hodgkin's lymphoma has a localized tumor that is easy to treat, and therefore prognosis is good. A person with stage IV Hodgkin's lymphoma has widespread disease that is difficult to treat in all locations, and there are probably some secondary tumors not detected; prognosis is poor. |
Lymphedema - tissues in extremities swell due to obstruction of lymphatic vessels and subsequent accumulation of lymph |
|
|
Etiology of Lymphedema - most common disorder: congenital may involve vessels and lymph nodes (often seen in women between 15-25 years) - caused by blockage of lymph vessels by infestation of parasitic worms - result in condition called Elephantiasis |
Signs & Symptoms of Lymphedema - extremities swell as lymph accumulates - swelling may be soft but progresses more firm, painful and unresponsive to treatment - chronic lymphedema may lead to frequent infections (high fever and chills) |
|
|
Treatment of Lymphedema - diuretics to reduce swelling - strict bed rest - massage of affected area - elevation of affected extremity if edema is severe, infection set in, or patient's mobility has been severely impaired, surgical removal of affected tissue and surrounding fascia may be required - other implant drainage shut to drain lymph from superficial to deep lymphatic circulation |
Elephantiasis (Filariasis) - type of lymphedema caused primarily by infestation and blockage of lymph vessels of extremities by parasitic worm (Filaria) |
|
|
Etiology of Elephantiasis - parasitic worms infest small lymph vessels blocking lymph flow and result in significant swelling of affected extremity - severe: swelling and extremity may resemble an elephant's limb - nonfilarial elephantiasis caused by chemicals entering body thru cuts on feet (chemicals in ash irritate lymph vessels causing swelling)- block lymph vessels, causing excessive swelling of affected area. |
Signs & Symptoms of Elephantiasis (manifestations) - extreme swelling of legs, breasts or genitalia - thickening of subcutaneous tissue - frequent infections - skin ulceration - fever |
|
|
Diagnosis and Treatment of Elephantiasis - positive diagnosis of lymphatic filariasis by detection and identification of parasitic worms in blood - urine can reveal presence of parasites and exam of hydrocele fluid - primary treatment for lymphatic filariasis : medication regimen to kill parasite - treatment for elephantiasis: surgery to perform fluid shunting |
Castleman Disease - rare illness involves overgrowth of lymphoid tissue (not cancer) but high risk of lymphoma |
|
|
Pathophysio and Etiology of Castleman Disease - giant lymph node hyperplasia and angiofollicular lymph node hyperplasia (classified as lymphoproliferative disorder) 2 types of Castleman disease -unicentric (affects single lymph node) - multicentric (affects multiple lymph nodes and tissue may lead to severe weakening of immune system) |
Signs & Symptoms of Castleman Disease (unicentric) - difficulty breathing or eating due or fullness or pressure in chest or abdomen - large lump on neck, armpit or groin - unexplained weight loss and anorexia - persistent cough - |
|
|
Signs & Symptoms of Castleman Disease (Multicentric) - fever and night sweats - nausea and vomiting = loss of appetite and weight loss - weakness and overal fatigue - enlarged spleen, liver and or peripheral lymph nodes in neck, groin or armpits - numbness or weakness in hands and feet due to nerve damage |
Diagnosis of Castleman Disease - physical exam of lymph nodes - blood and urine test for anemia (associated with disease) - imaging tech - xray, computed tomography scans or MRI detect presence and # of any enlarged lymph noes and enlargement of organs (spleen or liver) - lymph node biopsy |
|
|
Treatment of Castleman Disease - Unicentric form: surgical removal of diseased and enlarged lymph node is preferred - if cannot remove node, take meds: corticosteroids or radiation treatment to shrink or destroy node - Multicentric form: more difficult: surgical removal of affected nodes (not practical because #s of nodes), use medications to target affected nodes or organs (corticosteroids, monoclonal antibodies, antiviral drugs, immune modulators and some anticancer drugs) |
Why might absence of parasitic nematode in blood not be a definitive proof that patient is not suffering from elephantiasis The elephantiasis may be a nonfilial form caused by a reaction to chemicals. |
|
|
Function of Spleen - defense, hematopoiesis, and red blood cell and platelet destruction (serving as reservoir for blood) |
Study Questions 1. Describe function of lymph nodes, thymus gland, tonsils and spleen The lymph nodes ensure constant filtration and surveillance of body fluids, removing foreign or dangerous materials. They are essential to the body’s immune response. The thymus gland is the final site of leucocyte development before birth and is responsible for the secretion of hormones after birth, which enables lymphocytes to develop into mature T cells. Tonsils function as protection against bacterial infections in the area of the openings between the nasal and oral cavities. The spleen functions in body defense— its macrophages remove microorganisms in the blood; monocytes and lymphocytes mature in the spleen; before birth, erythrocytes are formed in the spleen; old red blood cells and platelets are broken down and recycled in the spleen; and finally the spleen serves as a large reservoir for blood, which can be quickly returned to the circulatory system if needed. |
|
|
2. Trace the basic path of lymphatic circulation = Interstitial fluid flows into blind-ending capillaries with one-way valves; these capillaries form larger vessels with valves; these vessels are periodically interrupted with lymph nodes; the vessels of the upper right quadrant of the body empty into the right lymphatic duct, which returns lymph to the general circulation via the right subclavian vein. The remainder of the lymphatic vessels drains into the thoracic duct, which drains into the left subclavian vein. |
3. Compare Hodgkin's and non Hodgkin's lymphomas = Hodgkin’s lymphoma is characterized by T lymphocyte and Reed Sternberg cells and painless nontender cervical lymph nodes; it spreads to adjacent lymph nodes. Non-Hodgkin’s lymphoma is characterized by multiple involvement of scattered lymph nodes. Multiple myeloma is characterized by plasma cells (B lymphocytes) in the bone marrow, multiple tumors in vertebrae, skull, ribs, pain, and pathologic fractures. |
|
|
4. What are two forms of Castleman disease and characteristics distinguishes one from another = The two types of Castleman disease are unicentric and multicentric. The unicentric type involves a single lymph node with more local effects and is usually more easily treated with surgery. The multicentric type involves multiple lymph nodes, displaying more serious systemic manifestations; surgery is not a practical treatment because multiple sites are involved. |
THE END |

