![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
143 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Types of bone cells |
- Bones of the skeleton: axial & appendicular - Cartilages, ligaments & connective tissues
|
|
|
|
Axial skeleton includes: |
- skull - vertebral column - rib cage |
|
|
|
Appendicular skeleton includes: |
- pectoral girdle - pelvic girdle - arms - legs |
|
|
|
5 Primary functions of the skeletal system include: |
1. Support 2. Storage of minerals & lipids 3. Blood cell production (hemopoiesis) 4. Protection of internal organs 5. Leverage for muscular movement |
|
|
|
Composition of Bone |
39% Calcium
0.2% Potassium 0.7% Sodium 0.5% Magnesium 9.8% Carbonate 17% Phosphate TOTAL Inorganic components 67% |
|
|
|
Composition of bone
|
99% of body's calcium 4% of body's Potassium 35% of body's sodium 50% of body's magnesium 80% of body's carbonate 99% of body's phosphate |
|
|
|
What is the most abundant mineral in the body? |
Calcium |
|
|
|
Calcium ions are vital too... |
- membranes - neurons - muscle cells (especially heart cells) |
|
|
|
The skeleton is considered a calcium reserve b/c |
- bones store calcium & other minerals |
|
|
|
Bones are classified by their...
|
- shape/structure - internal tissue organization - bone markings (surface features; marks) |
|
|
|
6 bone shapes |
1. Long 2. Short 3. Flat 4. Sutural 5. Irregular 6. Sesamoid
|
|
|
|
- small, irregular bones - found b/w the flat bones of skull This describes what type of bone? |
SUTURAL BONES |
|
|
|
- complex shapesex. spinal vertebrae, pelvic bones |
IRREGULAR BONES |
|
|
|
- small & thick ex.) ankle & wrist bones
What type of bone is this?
|
SHORT BONES |
|
|
|
- long & thin - arms, legs, hands, feet, fingers & toes
What type of bone is this? |
LONG BONES |
|
|
|
- small & flat - develop inside tendons near joints of knees, hands & feet
What type of bone is this? |
SESAMOID BONE |
|
|
|
The following describe what characteristic of a bone?
- depressions / grooves - elevations / projections - tunnels |
BONE MARKINGS aka: surface features |
|
|
|
Depressions / Grooves are found... |
along bones surface |
|
|
|
What is the bone marking where...
- tendons & ligaments attach - at articulations w/ other bones
|
Elevations / projections
|
|
|
|
Bone marking where blood & nerves enter bone |
TUNNELS |
|
|
|
Structure of a LONG BONE |
- diaphysis - epiphysis - metaphysis |
|
|
|
What part of a bone does this describe?
- shaft of long bone
- heavy wall of COMPACT BONE / dense bone
-central space called MEDULLARY (marrow) CAVITY |
DIAPHYSIS |
|
|
|
What part of a bone does this describe? - wide part at each end
- articulation w/ other bones
- mostly SPONGY (cancellous) BONE
- covered w/ compact bone (CORTEX) |
EPIPHYSISE |
|
|
|
What part of a bone does this describe?
- where diaphysis & epiphysis meet
|
METAPHYSIS |
|
|
|
aka "dense bone" & is relatively solid |
COMPACT BONE |
|
|
|
The central space of long bone is called the... |
MEDULLARY CAVITY aka:"marrow cavity" |
|
|
|
What type of bone does this describe? aka: cancellous / trabecular bone
- consists of an open network of struts & plates that resembles latticework |
SPONGY BONE |
|
|
|
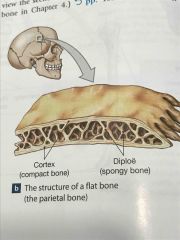
The structure of a FLAT BONE resembles a... |
"spongy bone sandwich" |
|
|
|
The sturcture of a FLAT BONE consist of... |
- compact bone - spongy bone - compact bone |
|
|
|
Within the cranium, the layer of spongy bone b/w the compact bone is called the_________ |
diploë |
|
|
|
– Dense,supportive connective tissue
– Contains specialized cells
– Produces solid matrix of calcium salt deposits around collagen fibers |
Osseous (bone) tissue |
|
|
|
Characteristics of BONE TISSUE include: |
- matrix - osteocytes - lacunae - canaliculi - periosteum |
|
|
|
The (dense) MATRIX contains... |
- calcium salt deposits - osteocytes (bone cells) w/in lacunae |
|
|
|
- form pathways for blood vessels - exchange nutrients & wastes |
CANALICULI |
|
|
|
- covers outer surfaces of bones - consists of outer fibrous & inner cellular layers |
PERIOSTEUM |
|
|
|
Bone matrix is made up of...
|
- Minerals - 2/3 calcium phosphate [Ca3(PO4)2] - Reacts w/ calcium hydroxide [Ca(OH)2] to formcrystals of hydroxyapatite [Ca10(PO4)6(OH)2], which incorporates other calcium salts & ions like calcium carbonate [CaCO3] - Matrix proteins - 1/3 is protein (specifically COLLAGEN FIBERS) |
|
|
|
Bone contains 4 types of cells |
1. Osteocytes 2. Osteoblasts 3. Osteoprogenitor cells 4. Osteoclasts
|
|
|
|
2 major functions of OSTEOCYTES |
1. Maintain protein & mineral content of matrix 2. Help repair damaged bone |
|
|
|
– Mature bone cells that maintain the bone matrix
– Live in lacunae between layers (lamellae) of matrix – Connect by cytoplasmic extensions through canaliculi in lamellae
– do not divide |
OSTEOCYTES |
|
|
|
"bone building" cells |
OSTEOBLASTS |
|
|
|
Immature bone cells that secretes osteoid, the organic component of bone matrix, matrix compounds (OSTEOGENESIS) |
OSTEOBLASTS |
|
|
|
Matrix produced by osteoblasts, but not yet calcified to form bone is called an ______ |
OSTEOID |
|
|
|
Osteoblasts surrounded by bone become _____ |
OSTEOCYTES |
|
|
|
Mesenchymal stem cells that divide to produce osteoblasts are called________ |
OSTEOPROGENITOR CELLS |
|
|
|
Functions of Osteoprogenitor cells include: |
- assist in fracture repair
- Mesenchymal stem cells that divide to produce osteoblasts |
|
|
|
Osteoprogenitor cells are located in the... |
Endosteum- inner cellular layer of periosteum |
|
|
|
"bone recycling" cells are called what? |
OSTEOCLASTS |
|
|
|
- Giant, multi-nucleated cells that secrets acids & enzymes to dissolve bone matrix
- Derived from stem cells that macrophages |
OSTEOCLASTS |
|
|
|
Functions of Osteoclasts include: |
- secrete acids & protein-digesting enzymes
- dissolve bone matrix & release stored minerals (Osteolysis) |
|
|
|
Homeostasis of bone is maintained by... |
the equal building of bone (osteoblasts) & recycling of bone (osteoclasts)
|
|
|
|
bones become weak if.... |
there is more breakdown than building |
|
|
|
What can cause osteoblasts to build bone? |
exercise, especially weight-bearing exercise |
|
|
|
- Mature bone cells that make up most of the cell population
- Maintains the bone matrix |
OSTEOCYTES |
|
|
|
Stem cell whose divisions produce osteoblasts are called what type of cell? |
OSTEOGENIC CELL |
|
|
|
The basic functional unit of mature compact bone is called a... |
OSTEON |
|
|
|
In an osteon, the osteocytes are arranged in concentric lamellae around a ________ canal containing blood vessels. |
Central canal |
|
|
|
Function of PERFORATING CANALS include... |
Carrying blood vessels into the bone marrow |
|
|
|
Perforating canals run _______ to the central canal. |
PERPENDICULAR |
|
|
|
What is the main function of CIRCUMFERENTIAL LAMELLAE |
Binds osteons together |
|
|
|
Where is CIRCUMFERENTIAL LAMELLAE found? |
- found at the outer & inner surfaces of the bone |
|
|
|
Collagen adds ______ to bones. |
Strength |
|
|
|
Compact bone contains parallel ______ |
OSTEONS |
|
|
|
Spongy bone contains ______ |
Trabeculae |
|
|
|
Compact bone is covered w/ a _____ |
Membrane |
|
|
|
What membrane covers all the bones except parts enclosed in joint capsules?
*structure |
Periosteum |
|
|
|
A membrane made of a fibrous outer layer & a cellular inner layer. |
Periosteum |
|
|
|
3 Functions of PERIOSTEUM |
1. Isolates bone from surrounding tissues
2. Provides a route for circulatory (blood vessels) & nervous supply
3. Aides in bone growth & repair |
|
|
|
Compact bone is covered w/ a ________ membrane. |
Endosteum |
|
|
|
- an incomplete cellular layer - lines the medullary (marrow) cavity - covers traneculae of spongy bone - lines central canals - contains osteoblasts, osteoprogenitor cells & osteoclasts - active in bone growth / repair |
Endosteum |
|
|
|
What type of bone does not have osteons? |
Spongy bone |
|
|
|
The matrix of a ______ bone forms an open network of supporting bundle of fibers called TRABECULAE. |
Spongy bone |
|
|
|
The matrix or TRABECULAE of a spongy bone does not contain what? |
Blood vessels |
|
|
|
The space between trabeculae is filled with ______ bone marrow. |
RED |
|
|
|
What does RED BONE MARROW do? |
- contains blood vessels - forms red blood cells - supplies nutrients to osteocytes |
|
|
|
What does YELLOW BONE MARROW do? |
Stores lipids/fat |
|
|
|
Weight bearing bones |
The femur transfers weight from hip joint to knee joint.
Causes tension on the lateral side of the shaft & compression on the medial side. |
|
|
|
Human bones grow until about what age? |
25 |
|
|
|
Bone formation is called what? |
Osteogenesis |
|
|
|
Process of replacing other tissues w/ bone is called what? |
Ossification |
|
|
|
During development, most bones originate as _______ cartilages. |
Hyaline |
|
|
|
The process in which hyaline cartilages are replaced w/ bone. |
Endochondral ossification |
"Endo" (inside) "chondros" (cartilage) |
|
|
Endochondral ossification is the process of creating... |
LONG BONES |
|
|
|
Purpose of skeletal system |
- provides framework for body posture - allows for precise movements |
|
|
|
Purpose of Cartilages, ligaments & connective tissues |
- stabalize/connect the bones |
|
|
|
What cell is found in bone that: - located in lacunae - mature bone cells - adjacent osteocytes are interconnected by canaliculi |
OSTEOCYTES |
|
|
|
A bone cell that synthesizes the bony matrix by ossification is called... |
OSTEOBLASTS or OSTEOGENESIS |
|
|
|
A bone cell that dissolves the bony matrix through osteolysis is called... |
OSTEOCLASTS |
|
|
|
A cell that differentiate into osteoblasts are called... |
OSTEOGENIC CELLS |
|
|
|
COMPACT BONE contains... |
PARALLEL OSTEONS |
|
|
|
SPONGY BONE contains... |
trabeculae |
|
|
|
The basic functional unit of a COMPACT BONE is the... |
OSTEON |
|
|
|
An OSTEON contains OSTEOCYTES that are arranged around a central canal. |
|
|
|
|
PERFORATING CANALS |
extend perpendicularly to the bone surface |
|
|
|
located where stresses from a limited range of directions, such as along the DIAPHYSIS of long bones. Is this COMPACT/SPONGY bone? |
COMPACT BONE |
|
|
|
located where stresses are few or come from many directions, such as at the EPIPHYSES of long bones. Is this COMPACT/SPONGY bone? |
SPONGY BONE |
|
|
|
A bone is covered by a ______ & lined w/ an _____. |
PERIOSTEUM ENDOSTEUM |
|
|
|
Bones form through _____ & enlarge through _______ & remodeling. |
OSSIFICATION APPOSITIONAL GROWTH |
|
|
|
the process of bone formation |
OSSIFICATION or OSTEOGENESIS |
|
|
|
the process of depositing calcium salts within a tissue |
CALCIFICATION |
|
|
|
ENDOCHRONDRAL OSSIFICATION 1. Chondrocytes grow w/in calcifying matrix. Chrondrocytes cut off from nutrients die & disintegrate, leaving cavities w/in the cartilage |
ENDOCHRONDRAL OSSIFICATION |
|
|
|
ENDOCHRONDRAL OSSIFICATION 2. Blood vessels grow around edges of cartilage, & cells of the perichondrium covert to osteoblasts. Shaft of cartilage then becomes enclosed in a superficial layer of bone. |
ENDOCHRONDRAL OSSIFICATION
|
|
|
|
ENDOCHRONDRAL OSSIFICATION
3. development of primary ossification center, blood vessels allow fibroblasts to differienate into osteoblasts producing spongy bone @ primary ossification center. Bone formation then spreads along the shaft toward both ends of the former cartilage. |
ENDOCHRONDRAL OSSIFICATION
|
|
|
|
ENDOCHRONDRAL OSSIFICATION
4. Remodeling occurs, growth continues, creating medullary cavity. The osseous tissue of shaft becomes thicker & cartilage near each epiphysis is replaced by shaft of bone. Increases in length & diameter. |
ENDOCHRONDRAL OSSIFICATION
|
|
|
|
ENDOCHRONDRAL OSSIFICATION
5. Capillaries & osteoblasts move into epiphyses, creating secondary ossification centers. |
ENDOCHRONDRAL OSSIFICATION
|
|
|
|
ENDOCHRONDRAL OSSIFICATION
6. Epiphyses filled w/ spongy bone. Metaphysis separates the epiphysis from diaphysis. Epiphyseal cartilage |
ENDOCHRONDRAL OSSIFICATION
|
|
|
|
ENDOCHRONDRAL OSSIFICATION
7. Puberty, rate of epiphyseal cartilage production slows & rate of osteoblasts increase. Then epiphyseal cartilage gets smaller until it disapears (called epiphyseal closure) Epiphyseal line is distinct. |
ENDOCHRONDRAL OSSIFICATION
|
|
|
|
When long bone stops growing, after puberty the former location of the epiphyseal cartilage becomes a distinct _______ line. Visible on x-rays |
EPIPHYSEAL LINE |
|
|
|
As long bone matures ... |
Osteoclasts enlarge medullary (marrow) cavity
|
|
|
|
As long bone matures... |
Osteons form around blood vessels in compact bone. |
|
|
|
Compact bone thickens & strengthens long bone w/ layers of circumferential lamellae. This is called... |
APPOSITIONAL GROWTH |
|
|
|
Another term for Intramembranous Ossification |
Dermal Ossification |
|
|
|
Intramembranous Ossification (dermal Ossification) occurs in the... |
Dermis |
|
|
|
What type of bones does Intramembranous Ossification produces what type of bones? |
Dermal bones - mandible - clavicle |
|
|
|
What type of bones does Intramembranous Ossification produces what type of bones? |
Dermal bones - mandible - clavicle |
|
|
|
INTRAMEBRANOUS OSSIFICATION (5 Steps) |

|
|
|
|
ENDOCHONDRAL OSSIFICATION (7 steps) |

|
|
|
|
Endochondral Ossification (7 steps) |

|
|
|
|
Bone STRUCTURE |

|
|
|
|
Flat bone structure |
Spongy bone sandwich |
|
|
|
Types of bone cells |

Back (Definition) |
|
|
|
Types of Bones Cells |

Back (Definition) |
|
|
|
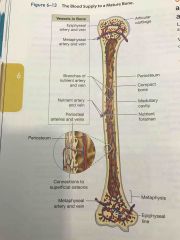
Blood supply of mature bone |
|
|
|
|
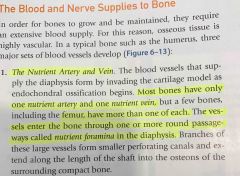
Nutrient Artery & Nutrient Vein |
|
|
|
|
Metaphyseal vessels |
Back (Definition) |
|
|
|
Periosteal Vessels function |
|
|
|
|
Process of remodeling |
Back (Definition) |
|
|
|
Process of remodeling |
Back (Definition) |
|
|
|
Effects of exercise on bone |
- mineral recycling allows bones to adapt to stress
- heavily stressed bones become thicker & stronger |
|
|
|
Bone degeneration |
- bones degenerate quickly
- up to 1/3 of bone mass can be lost in a little as a few wks of inactivity |
|
|
|
Normal bone growth/maintenance depend on NUTRITIONAL/HORMONAL factors: |
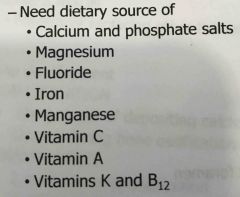
|
|
|
|
Fractures are... |
- Cracks / breaks in bones
- caused by physical stress |
|
|
|
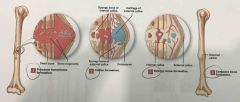
Fracture Repair STEPS |
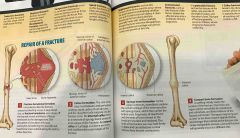
1. Bleeding (hematoma) 2. Cells of endosteum & periosteum 3. Osteoblasts 4. Osteoblasts & osteocytes remodel the fracture for up to 1 year |
|
|
|
Composition of Bone |

|
|
|
|
Step 1. Fracture Repair Bleeding |
- produces a clot (fracture hematoma)
- estb a fibrous network
- bone cells in the are die |
|
|
|
Step 2. Fracture Repair Cells of the endosteum / periosteum |
- divide & move into fracture zone
- calluses stabilize the break
EXTERNAL CALLUS of a cartilage & bone surrounds break
INTERNAL CALLUS develops in medullary cavity |
|
|
|
Step 3. Fracture Repair Osteoblasts |
- replace central cartilage of external callus w/ spongy bone |
|
|
|
Step 4. Fracture Repair Osteoblasts & osteocytes remodel the fracture for up to a year |
- reduces bone calluses |
|
|
|
Age related changes to bones: |
- bones become thinner / weaker with age
OSTEOPENIA begins between ages 30 & 40
- women lose 8% of bone mass per decade, men 3% |
|
|
|
Age related change |
The epiphyses, vertebrae & jaws are most affected.
- Results in fragile limbs - reduction in height - tooth loss |
|
|
|
Osteoporosis |
- severe bone loss - affects normal function - over age 45, occurs in: 29% of women 18% of men |
|
|
|
4 Steps of Fracture Repair |
Back (Definition) |
|
|
|
Weight bearing bones: |
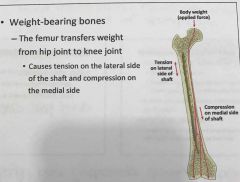
|
|
|
|
Vessels in Bone |
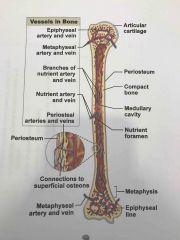
Back (Definition) |
|

