![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
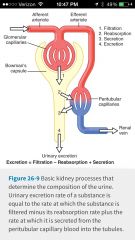
What is the urine excretion formula? |
Excretion = filtration |
|
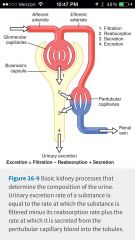
What is the calculation for tubular reabsorption? Under what conditions this happen? How do we find filtration and excretion?
|
This happens when excretion is less than filtration.
Reabsorption = filtration - excretion Filtration equals GFR x the plasma concentration of the solute. Excretion = the urine concentration of a solute x Urine flow rate |
|

|
S
|
|

|
G
|
|

|
G
|
|
|
Transport maximum define
What happens when max transport is reached for all nephrons? Define threshold... Why is this not the same as transport maximum of the whole kidney? What are examples? |
Transport maximum is concept that some substances have a maximum rate of tubular transport due to saturation of carriers, limited ATP etc.
Once the transport maximum is reach for all nephrons, further increases in tubular load are not reabsorbed and are excreted. Threshold is the tubular load at which transport maximum is exceeded in some nephrons. This is not exactly the same as transport maximum of the whole kidney because some nephrons have lower transport maximums than others. Examples would be glucose amino acids phosphate and sulphate |
|

|

|
|

|
G
|
|

|
G
|
|
|
The thin descending loop of Henle is very permeable to what?
In the thick ascending loop Of Henle what percentage of the load is filtered? What electrolytes get reabsorbed and what is secreted here? Is this area permeable to H2O? |

The descending loop of Henley is permeable to H2O
The ascending loop of Henley is more thick therefore it's not as permeable to h20. The Ascending loop filters 25% of the load. It reabsorbs sodium, chloride, potassium, bicarbonate , calcium and magnesium. It Secretes hydrogen |
|
|
Early distal tubule:
Usually sodium and chloride are transported from the Tubular lumen into the cell by: cotransport. This is inhibited by what? How is sodium pumped out of the cell and how does chloride leave the cell? |

|
|
|
Early distal tubule:
Usually sodium and chloride are transported from the Tubular lumen into the cell by: cotransport. This is inhibited by what? How is sodium pumped out of the cell and how does chloride leave the cell? The early tubule is functionally similar to what? Is it permeable to water? What four electrolytes does it actively reabsorb and what does it contain ? |

The early distal tubule is functionally similar to the ascending loop. It is not permeable to water which is why it's called the diluting segment. It actively reabsorbs sodium, chloride, potassium , and magnesium. It is well contains the macula densa
|
|
|
G
|
G
|
|
|
Early distal tubule: how much of a percentage of the filter load is reabsorbed? Is this area permeable to H2O or urea?
|

The early distal tubule is is not permeable to h2o nor is it permeable to urea. Only 5% of filtered load NACL is reabsorbed.
|
|
|
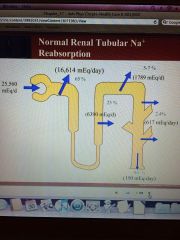
Late distal tubule and collecting tubule:
It's permeability to H2O depends on what? Is it permeable to be URea? |

Permeability to H2O depends ADH .It is also not very permeable to urea.
|
|
|
Late distal and cortical collecting tubules principal cells secrete what?
|

These principles cells secrete potassium ion.
|
|

What is the mechanism of sodium chloride reabsorption and potassium secretion in the late distal tubule's and cortical collecting tubules?
|

Sodium enters the cell thru special channels and is transported out of the cell by the sodium potassium pump. Aldosterone Antagonists compete with aldosterone for binding sites in the cell. This inhibits the effects of aldosterone and stimulates sodium reabsorption and potassium secretion. Sodium channel blockers directly inhibit the entry of sodium into the cell.
|
|

Late distal and cortical collecting tubule intercalated cells secrete what?
|
These intercalated cells secrete hydrogen ion.
|
|

Transport characteristics of medullary collecting ducts: this collecting duct actively reabsorbs what and secretes what? Is it permeable to urea? The reabsorption of water in the Medullary collecting ducts is controlled by the concentration of what?
|
These ducts actively resorb water and are permeable to urea so they resort that as well. Hydrogen is secreted. The Reabsorption of water is dependent upon the concentration of ADH
|
|
|
G
|
|
|
Concentrations of solutes in the different parts of the tubule depend on relative resorption of what compared to what?
If H2O is reabsorbed to a greater extent than the solute what happens to the concentration of solute within the tubule? Give two examples. If the opposite happens and water is reabsorbed to a lesser extent than the solute what will happen to the concentration of the solute with in the tubule? Give two examples . |
Concentrations of solutes in the different parts of the tubule will depend on relative reabsorption of the solutes compared to water.
If h2o is reabsorbed to a greater extent than the solute, the solute will be more concentrated in the tubule . Examples creatinine and inulin If H2O is reabsorbed to a lesser extent than the solute, solute will become less concentrated in the tubule. Examples of glucose and amino acids. |
|
|
Six things that regulate tubular reabsorption:
|
Glomerulotubular balance, peritubular physical forces, hormones, sympathetic nervous system, arterial pressure, osmotic factors,
|
|
|
What are the five hormones that regulate tubular reabsorption
|
Aldosterone ,angiotension II, ADH, natriuretic hormone, parathyroid hormone.
|
|
|
Aldosterone actions on late distal, cortical and medullary collecting tubules:
What are its effects on sodium potassium and hydrogen? And what cells achieve this? |
Principal cells cause both increases in sodium reabsorption and potassium secretion.
Intercalated cells cause increase in hydrogen secretion. |
|
|
G
|
|
|
Define primary aldosteronism/conns syndrome-what does this result in? four things....
Define Addison's disease. What does this result in? Three things.... |
Primary Aldosteronism/cons syndrome is excess aldosterone release. This results in sodium retention, hypokalemia, alkalosis, hypertension,
Addison's disease is an aldosterone deficiency. This causes sodium wasting ,hyperkalemia , hypotension |
|
|
What three things increase aldosterone secretion? What things decrease Aldosterone secretion?
|
Aldosterone can be increased by angiotensin II, increased potassium or adrenocorticotropic hormone.
It can be decreased by atrial natriuretic factor, or increased sodium concentration (Osmolality) |
|
|
Angiotensin II increases resorption of what two things? And also stimulates what? What four places does it directly increase sodium reabsorption? On which arterioles does it to constrict? What effect does this have on peritubular capillaries hydrostatic pressure? What effect does this constriction have on the filtration fraction?
|

|
|

|

G
|
|
|
What causes angiotensin II release? Angiotensin II causes constriction of what arterioles, causes sodium and water retention and maintains excretion of what? What effect does this have on the glomerular capillary pressure, renal bloodflow, peritubular capillaries pressure as well as on filtration fraction? What is angiotensin II release designed to prevent? two things
|

|
|
|
What 3 classes of meds block angiotensin II to decrease sodium and water reabsorption? Natriuresis and diuresis how what effect on blood pressure?
|

|
|
|
In what three ways do renin in inhibitors increase natriuresis and diuresis therefore equaling a lower blood pressure?
|
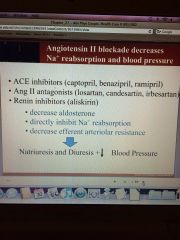
|
|
|
ADH is secreted by what gland? It increases what two things in the distal and collecting tubules? What three things does it allow for control of?
|
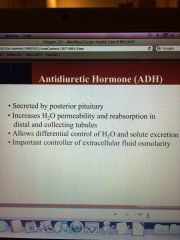
|
|
|
Where is ADH synthesized and released?
|
|
|

|
G
|
|
|
Feedback control of extracellular fluid osmolarity by ADH- high extracellular osmolarity causes what with ADH secretion, which does what to tubular H2O permeability which does what to H2O reabsorption which ultimately equals what with H2O excretion
|

|
|
|
Inappropriate ADH syndrome which is excess ADH, results in a decrease of what two things?
Central diabetes insipidus which is insufficient ADH results in what three things? |
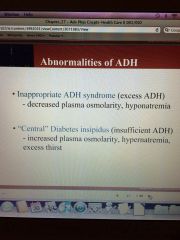
|
|
|
Atrial natriuretic peptide increases excretion of what? Where is it secreted and in response to what? What 3 things does it directly inhibit ? What effect does it have on GFR and blood volume expansion?
|
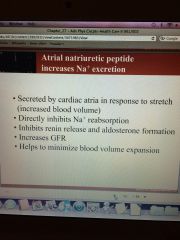
Anp Dialates afferent end constricts efferent end
|
|
|
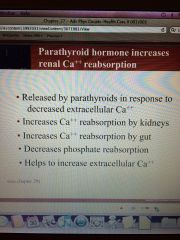
Para thyroid hormone increases what and decreases what? What stimulates this? It does these two things with what ultimate goal? Where does it increase this (2 places).
|
|
|
|
What is the effect of the sympathetic nervous system on sodium reabsorption? It therefore stimulates the release of what? And what is its effect on GFR and renal bloodflow? What is the only situation that we would see this happen to GFR and renal bloodflow?
|

|
|
|
What is the effect of increased arterial pressure on sodium reabsorption? What Ultimate effect does it have on peritubular capillaries hydrostatic pressure, renin aldosterone and intrarenal natriuretic factors ? What are the two intrarenal natriuretic factors?
|
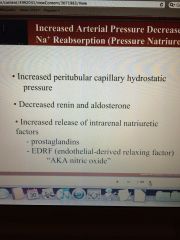
Then increased blood flow increases GFR and rbf
|
|
|
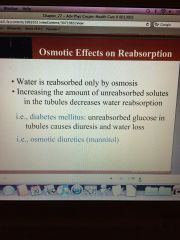
Osmotic effects on reabsorption:
What is the only way that water is reabsorbed? Increasing the amount of unabsorbed solutes in the tubules does what to water reabsorption ?name two examples of this |
|
|
|
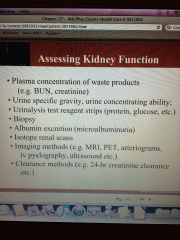
In what ways do we assess kidney function? How do we assess: plasma concentration of waste products, presence of protein or glucose in the urine, microalbinuria, clearance products?
|
|
|
|
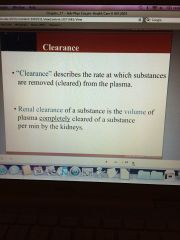
Define renal clearance. Does a volume of substance have to be completely cleared to be a part of our renal clearance value?
|
|
|
|
What is the renal clearance equation?
|

|
|

|
U
|
|
|
If clearance rate is above GFR than we have what ?
|
Secretion on top of filtration
|
|
|
If a person has decreased GFR and therefore has a buildup of creatinine and urea and then GFR increases in response to a buildup of urea then we can still actually filter at the same rate but we have a build up of urea in the plasma from the time they are GFR was decreased
|
T
|

