![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
71 Cards in this Set
- Front
- Back
|
What receives the signal in most cases of cell communication?
|
a receptor protein on the target cell
|
|
|
What are the 4 mechanisms of cell communication?
|
1. Contact Dependent Signaling
2. Paracrine Signaling 3. Synaptic Signaling 4. Endocrine signaling |
|
|
What is contact dependent signaling?
|
-relatively rare
-no chemical released - cells have to come into very close contact - Important during embryonic development |
|
|
What is paracrine signaling?
|
-common
- can target multiple, neighbouring cells - doesn't go very far (local) -signal is released by exocytosis and acts on multiple neighbouring targets (paracrine) - or on the signaling cell itself (autocrine) - acts as a feedback mechanism that allows the cell to control the signal |
|
|
What is the difference between Paracrine and autocrine?
|
Paracrine- in paracrine signaling, when the signal acts on multiple neighbouring targets
Autocrine: when the signal acts on the cell itself. - feedback mechanism that allows the cell to control the signal |
|
|
What is synaptic signaling? Where does it function?
|
- Only functions on cells of the nervous system
- equivalent to "face to face conversation" - signal is produced by a neuron and released at a synapse; acts on a single postsynaptic target |
|
|
What is endocrine signaling?
|
- When a hormone is released by exocytosis, it is released into the blood stream and can reach cells that are far away
- acts on multiple cells |
|
|
What kind of cell produces hormones?
|
an Endocrine cell
|
|
|
What types of signaling target multiple cells? What kind target single cells?
|
Multiple cells
- Paracrine Signaling -Endocrine Signaling Single cell - Synaptic signaling -Contact dependent signaling (I'm only 90% sure about this) |
|
|
- What are the types of signaling molecules? Which is most common? Least common?
|
-hydrophilic (most common)
-hydrophobic -gases(least common) |
|
|
List examples of hydrophobic signaling molecules. What are they generally?
|
generally, they are proteins, peptides, derivative amino acids, and small organic molecules
Acetylcholine - a neurotransmitter Adrenaline - small, organic molecule that functions as a hormone Growth factors - most often used in paracrine signaling |
|
|
In what kind of signaling are growth factor proteins commonly used?
|
Paracrine signaling
|
|
|
Signaling molecules are _________ in animal phyla
|
conserved
|
|
|
Give an example of a hydrophobic signaling molecule
|
Steroid hormone
|
|
|
Give an example of a gas signaling molecule
|
Nitric oxide
|
|
|
How does a hydrophobic signal or gas signal bind to a receptor?
|
-since it is hydrophobic, it can permeate the target cell and bind to either cytosolic receptors or nuclear receptors
-goes right through the cell membrane |
|
|
what kind of signal type are protein kinases (usually)?
|
Hydrophobic
|
|
|
How does a hydrophilic signal bind to a receptor?
|
-hydrophilic signals cannot permeate the membrane.
- bind to cell surface receptor, making them an extracellular receptor 1. binds to surface receptor 2. alters the intracellular protein, which acts like an intermediate protein (cascade effect) 3. Target protein is then affected |
|
|
How is the target protein effected in extracellular signaling? What type of signal does extracellular signaling
|
1. binds to surface receptor
2. alters the intracellular protein, which acts like an intermediate protein (cascade effect) 3. Target protein is then affected - signal type: hydrophilic |
|
|
If the target protein of extracellular signaling is a metabolic enzyme, what happens?
If it's a gene regulatory protein? if it's a cytoskeleton protein? |
Metabolic enzyme- would alter metabolism
Gene regulatory protein- altered gene expression cytoskeletal protein- altered cell shape or movement |
|
|
What determines the response that an extra cellular signal will cause (i.e. Acetylcholine)?
|
Determined by type of cell-surface receptor on diff. cells
ex. A) in a heart muscle cell - Acetylcholine binds, causes muscle to elongate then relax. -decreased rate and force of contraction B) Salivary gland cell - Acetylcholine binds, causes secretion C) Skeletal muscle cell - Acetylcholine binds to receptor on muscle - contraction |
|
|
What are the properties of fast and slow responses in cell signaling?
In other words, what makes a fast response fast, and a slow response slow? |
Fast response: involves changes in existing proteins
Slow response: requires new protein synthesis |
|
|
Steroid Hormone:
- What is it derived from? -how does it reach the target cell? -what are its important functions? |
-Derived from cholesterol
- dispersed through blood, (endocrine signaling) -Functions: controls metabolism, immune function, development of male/female sexual characeristics |
|
|
What is the process of a steroid hormone causing translation of a gene? (general, from receptor binding to translation)
|
-Steroid binds to receptors in the cytosol, then moves to nucleus
OR - steroid binds straight to nucleus receptors - in nucleus, steroid receptor complex binds to DNA, which turns on gene expression (that is a slow response) - binding causes genes to be transcribed -leads to translation |
|
|
What type of protein are steroid Receptors?
|
DNA=binding proteins
|
|
|
What part of steroid receptors is highly conserved?
In other words, what is the same in all Steroid receptors? |
DNA binding domain
|
|
|
What is the DNA binding domain of steroid receptors consist of?
|
Two zing fingers that bidn to specific DNA sequences called Hormone Response Elements
|
|
|
What are Hormone Response elements?
|
DNA sequences to which the DNA binding domains of Steroid Receptors bind.`
|
|
|
What makes a steroid receptor inactive?
|
The nuclear localization signal is bound by an inhibitory protein ( a chaperone)
|
|
|
What are the parts of an empty steroid receptor?
|
Ligand binding domain
transcription activating domain DNA binding domain |
|
|
What does the steroid receptor look like as soon is it is activated?
|
-A ligand is attached
- Coactivator proteins are attached to the ligand-binding domain and transcription activating domain - Only the DNA binding domain is exposed |
|
|
Once the hormone is in the steroid receptor, how do Steroid hormones activate gene expression? (specific)
|
1. Receptor-steroid-hormone complex activates primary response genes.
2.Primary (early response) genes are transcribed 3. Proteins encoded by these genes (primary response proteins) turn on expression of secondary delayed response genes 4. Secondary response proteins synthesized |
|
|
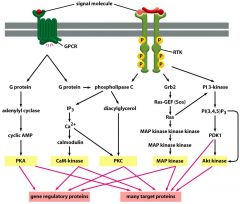
What are the three types of cell-surface receptors?
|
1. Ion-channel linked receptors
2. G protein-coupled receptors 3. Enzyme-linked receptors |
|
|
what are the structural characteristics of GPCRs?
|
7 transmembrane domains
N- terminal in extracellular matrix, C- terminal in side the cell 3 loop of intracellular loop is bigger than the others |
|
|
What part of GPCR is important for binding the extracellular signals? the intracellular signals?
|
extra-cellular: N-terminal
Intra-celular: Cterminal and 3rd intracellular loop |
|
|
What intermediate is needed for GPCR to activate a target?
|
a G-protein
|
|
|
What is an orphan receptor?
|
a receptor for which the gene exists, and it is expressed, but we don't know what activates it
many are probably activated by smell/taste |
|
|
What is the structure of a G-protein? What are its general physical properties?
|
-Trimeric, has three subunits (alpha,beta, gamma)
-has GTPase activity -lipid-anchored membrane protein |
|
|
what does the alpha subunit do in G-proteins?
|
it binds and hydrolyzes GTP and GDP
|
|
|
What are the three major classes of G proteins?
|
Gs
Gi Gq |
|
|
What does the inactive form of G protein look like compared to the active form?
|
Inactive is trimeric, and has GDP
Active has dissociated subunits, GTP |
|
|
How do the three subunits of the G protein dissociate?
|
Alpha splits from (beta and gamma), all three remain attached to the membrane
|
|
|
What is the first thing that happens when a signal binds to GPCR?
Then what? |
A conformational change in the receptor occurs, causing GPCR to have a higher affinity for G protein/binds more tightly to g protein
Then, G protein undergoes a conformational change, causing it to replace GDP with GTP After this, protein is fully activated? |
|
|
Which subunit(s) of g protein act like an on/off switch? How?
|
G alpha subunit, because it binds to a target protein which creates altered protein activity (on)
after a while, G alpha subunit hydrolyzes GTP and dissociates from the target (off) |
|
|
What happens to G alpha subunit once it dissociates from its target protein?
|
It re-associates with G beta/G gamma subunits, making the G protein inactive once more.
|
|
|
What is the most common target of G proteins?
|
Adenylate Cyclase enzyme
|
|
|
What activates adenylate cyclase? what inhibits it?
|
Gs alpha activates
Gi alpha inhibits |
|
|
what activates phospholipase c-beta?
|
Gq alpha
|
|
|
What produces cyclic AMP (cAMP)?
|
adenylate cyclase
|
|
|
When would you see cAMP in a cell? when would you not see it? Why would you start/stop seeing it?
|
you would see it when the enzyme Adenylate cyclase is activated.
you would stop seeing it once the signal for Adenylate cyclase activation has ceased (once GCPR is not binding to a signal) - because cAMP is quickly destroyed by phosphodiestherase |
|
|
What does cAMP activate?
|
Protein Kinase A (PKA)
|
|
|
What is the structure of Protein Kinase A (PKA)?
|
4 subunits, 2 catalytic, 2 regulatory
|
|
|
What role do the subunits of PKA play?
|
they bind to cAMP (4 cAMP are needed to activate a protein kinase)
once cAMP is bound, it causes the dissociation of PKA complex, which releases the catalytic subunits that can phosphorylate other proteins |
|
|
how many cAMP are needed to activate a PKA?
|
4
|
|
|
What's an example of a serine-thrionine protein kinase?
|
PKA
|
|
|
What enzyme has broad specificity and catalyzes reactions at serine/thrionine residues?
|
PKA
|
|
|
is cAMP fast or slow? why?
|
fast, doesn't need to do protein synthesis
|
|
|
Give an example of an intracelllular second messenger. What makes it an intracellular second messenger?
|
cAMP, because the 1st messenger would be the extracellular signal that causes the formation of cAMP
- then cAMP is the second, because it then activates PKA -cAMP necessary because the hydrophilic 1st signal cannot get in the cell |
|
|
When would cAMP be considered fast response?
slow response? what happens here? |
cAMP is fast during its regular activity in activating PKA, because no proteins need to be synthesized.
cAMP is slow when it stimulates gene expression - less common - happens when PKA can get into the nucleus via nuclear pores - causes the nuclear protein CREB to be phosphorylated -CREB is a gene regulatory protein, which causes new proteins to be syntehsized when it is phosphorylated |
|
|
What is a CREB?
|
a nuclear, gene-regulatory, protein that is phosphorylated by PKA via slow response (when PKA goes straight into nucleus, stimulated by cAMP)
|
|
|
What are the 4 ways a cell can stop the response to a signal in G-protein coupled receptor signaling?
|
1) no more signal is made, means no more G-protein is made, which causes a cascade
2) If the G-alpha subunit turns itself/g-protein off by hydrolyzing GTP 3)if the enzyme that destroys cAMP (phospho-diestherase) becomes active 4) if the protein phosphatases that remove phosphates become active |
|
|
how does signal desensitization occur? Why does it occur?
|
Occurs in response to a signal that continuously keeps being delivered (for example by a stress related hormone)
- receptor is constantly full of signal, keeps being activated, needs to be "quieted" - after some time, receptor becomes desensitized by repeated ligand stimulation -if the signal is present in the receptor for too long, the receptor will be phosphorylated, causing a conformational change |
|
|
What does Adrenaline stimulate in the muscle and liver?
|
- glycogen phophorylate
|
|
|
What mediates the effect of Adrenaline stimulus? Why?
|
a GPCR called beta-adrenergic receptor
- Because the hormone is outside of the cell, it needs a GPCR to send the signal inside |
|
|
what is the path of the Adrenaline signal in turning on Glycogen Phosphorylase?
|
1. Adrenaline binds to beta-adrenergic GPCR (associated with Gs
2.G protein activated 3.Adenylate cyclase activated 4.causes production of cyclic AMP 5. Makes PKA active -PKA, although it has broad specificity, does not recognize Glycogen phosphorylase, so there needs to be an intermediate 6.PKA activates phosphorylase kinase (PK) - via phosphorylation -PK specifically phosphorylates Glygogen phosphorylase 7. PK phosphorylates GP, activates it 8. Glycogen brokedown into Glu-1-P |
|
|
What breaks down cAMP immediately after it is produced (pretty much immediately after)?
|
cAMP phosphodiestherase
|
|
|
How does signal amplification occur?
|
it is the by-product of signal cascade
- everytime a reaction step occurs, you intensify teh signal because more and more molecules are involved ex. PKA activated - 1 molecule PKA, phosphoryaltes many PK - each PK phosphporylates many GP |
|
|
what are several examples of intracellular second messengers?
|
cAMP
Calcium inositol triphosphate, GMP |
|
|
explain how Calcium acts as a an intracellular second messenger.
|
Calcium increases rapidly in stimulated cells, proteins activated
ex. Calcium/calmodulin-dependent protein kinases (CaM kinases) ex. Protein Kinase C (PKC) ex. Calcineurin (Phosphatase) ex. Troponin (actin-binding proteins) Gq and phospholipase C-beta signaling pathway - uses inositol phospholipid.Calcium pathway - used in control of regulated secretion/exocytosis -phospholipases c-beta cleaves phosphoinositol biphosphate (PIP2) - reaction produces inositol triphosphate (IP3) and Diacylglycerol |
|
|
What is IP3 (Inositol triphosphate)? What does it do?
|
a product of the Phospholipase C-Beta signaling pathway
- IP3 travels to ER and opens channel of ER membrane - ligand gated channel -Calcium released into cytosol |
|
|
what are all thre major pathways in eukaryotic intracellular communication?
|
|

