![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
Obstructive lung disease is characterized by loss of _________ or increased _______.
|
loss of lung elasticity; increased airway resistance
|
|
|
The hallmark of obstructive lung disease is _______________, as a result __________ occurs, causing an __________.
|
Reduction of expiratory flow rate; air trapping; increase in resting lung volume and end-expiratory volume.
|
|
|
Draw a graphical output of a spirometer during normal ventilation. Include volumes and capacities.
|
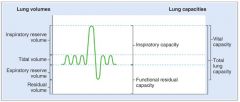
|
|
|
FEV1 is normally ____________ of the FVC.
|
80% (FEV1/FVC = 0.8)
|
|
|
________ and _________ are the two pathologic entities that comprise COPD.
|
Emphysema; chronic bronchitis
|
|
|
Emphysema and chronic bronchitis can often coexist, what does this mean?
|
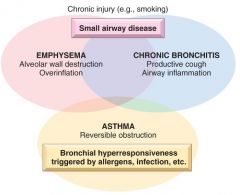
The patient exhibit features of both. There is clinical overlap.
|
|
|
Emphysema is caused by ________________________________.
|
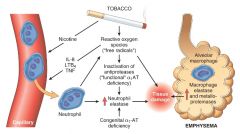
Alveolar wall destruction as a result of excessive protease activity.
|
|
|
The present hypothesis in emphysema is that activated neutrophils ___________________.
|
Release proteases that destroy interstitial elastin and collagen type IV.
|
|
|
In emphysema, alveolar wall destruction leads to a loss of pulmonary capillaries and a reduction in ___________.
|
capillaries; oxygen diffusing capacity
|
|
|
In emphysema, loss of pulmonary capillaries lead to a secondary increase in ____________ and ________.
|
pulmonary artery pressure; right heart failure
|
|
|
Interstitial elasticity help remain patency of _________ and __________.
|
terminal bronchioles; respiratory bronchioles
|
|
|
In emphysema, when patients exhales, many of their _______ has a tendency to ________, creating a _______ to air outflow.
|
bronchioles; collapse; obstruction
|
|
|
Chronic bronchitis is defined clinically as ___________.
|
productive cough for ≥ 3 months in at least 2 consecutive years, in the absence of any other identifiable cause.
|
|
|
Chronic bronchitis is characterized by __________ in the bronchial tree.
|
excessive mucus
|
|
|
Airway obstruction seen with chronic bronchitis is primarily due to ___________ and __________, both of which are triggered by inhaled __________ or ___________.
|
bronchiolar inflammation; bronchospasm; irritants; acute respiratory infection.
|
|
|
In cases of exacerbations in chronic bronchitis, it is helpful to employ ______ (3).
|
1. Systemic corticosteroids
2. Inhaled beta-2 agonists 3. Inhaled anticholinergics This is because bronchiolar inflammation is a cardinal feature. |
|
|
What is the pathogenetic background of chronic bronchitis?
|
Long-standing inhalation of toxins and irritants → Submucosal hypertrophy in trachea & bronchi (early) → Increased # of goblet cells in small airways (small bronchi & bronchioles) (late).
|
|
|
Compliance is [...]
|
The amount of change in volume achieved by a certain pressure change (ΔV/ΔP).
|
|
|
In interstitial fibrosis, the lungs are ______, and expand _____ for a given amount of pressure change; therefore, they have a ____ compliance.
|
stiff; less; low
|
|
|
As lung volume increases, interstitial elastin becomes ______, and compliance ________.
|
taut; decreases
|
|
|
In COPD, as FRC _______, lung expansion becomes more difficult because of ________ compliance at _______ resting volumes. This leads to ______ work of breathing.
|
increases; lower; higher; increased
|
|
|
What is the compliance of alveoli at the base of the lung?
|
They are MORE compliant because the intrapleural pressure being more POSITIVE there due to effects of gravity on the lungs. They are less distended and more compliant.
|
|
|
Emphysema is defined _______ and chronic bronchitis is defined ________.
|
morphologically; clinically
|
|
|
There is a difference in distribution of pure chronic bronchitis and pure emphysema. How is the distribution?
|

|
|
|
The collapse of alveoli and airways occurs preferentially at the ________ because of their _________.
|
bases; relatively higher compliance than at the apices.
|
|
|
Similar to the regional variation in ventilation, pulmonary capillary perfusion is _________ at the lung base compared with the apex.
|
greater
|
|
|
At the apex of the lung, where the _______ exceeds _______, described as zone __, there is ___________ flow.
|

alveolar pressure; pulmonary arterial and venous pressure; 1; practically no flow
|
|
|
In lung zone 2, the capillary flow is proportional to the difference in ___________.
|
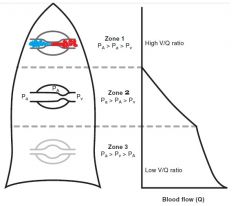
Pulmonary arterial pressure minus alveolar pressure. In zone 2, we do have capillary flow beceause Pa exceeds PA.
|
|
|
At the base, in zone 3, ____________ exceeds ___________ and flow is proportional to ____________.
|
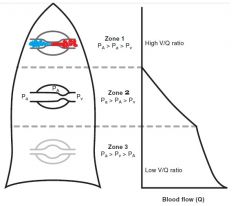
pulmonary venous pressure; alveolar pressure (it's like a column of fluid); difference of pulmonary arterial and venous pressures.
|
|
|
How is the V/Q ratio at the apex?
|
High. Perfusion is lower than ventilation at the apex.
|
|
|
The apex contributes ______ to the total
pulmonary capillary gas exchange because of _________. |
little; low perfusion
|
|
|
Why do we see a pathologic V/Q mismatch with hypoxemia in COPD (emphysema)?
|
The bases are more compliant, because at FRC they are stretched less. This is why we see a preferential collapse of alveoli in the base, and not (so much?) the apices. Ventilation is SHIFTED to the apex, which actually does not contribute a whole lot to total pulmonary capillary gas exchange due to its LOW PERFUSION. Gas exchange is therefore impaired and patients get hypoxemia.
|
|
|
In COPD, the inability to effectively _____________ results in _____ retention, increased _______, and respiratory _______.
|
expire alveolar CO2; CO2; arterial PaCO2; acidosis
|
|
|
What is the compensation for the acid-bace imbalance in long-standing COPD?
|
Compensation is renal. It consists of increased excretion of H+ as titratable acid (filtered HPO42- forms H2PO4-) and NH4+ (from glutamine), and increased reabsorption of "new" HCO3-.
|
|
|
What would be seen on a chest X-ray of a patient with COPD?
|
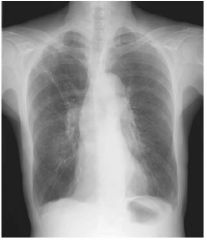
hyperinflated lungs, diaphragm flattening, and narrow cardiac silhouette.
|
|
|
Describe two important patterns of emphysema.
|

• Centriacinar (Centrilobular) emphysema:
- Seen in cigarette smokers. - The proximal parts ("central") of the acini, formed by respiratory bronchioles, are affected, while distal alveoli are spared (but in severe cases, distal become affected). - More common in upper lobes (particularly apical segments) • Panacinar (Panlobular) emphysema - Occurs in alpha1-antitrypsin deficiency - Acini are uniformly enlarged from the level of the respiratory bronchiole to the terminal blind alveoli. - Occurs more commonly in the lower lung zone |
|
|
In obstructive lung disease, such as asthma, FEV1 is ________ than FVC so the FEV1/FVC is ________.
|
reduced MORE than FVC; decreased
|
|
|
In COPD, in which airway R is increased, patients learn to expire ________________ to prevent the ______ that may occur with a forced expiration.
|
slowly with "pursed lips"; airway collapse
|
|
|
Why are people with a COPD primarily of emphysema, sometimes said to be "pink puffers"?
|
Pink because of absence of cyanosis.
Puffers because they puff air out with pursed lips to produce a positive end-expiratory pressure, allowing some alveoli/small airways to remain patent when expiring and not collapsing. |
|
|
Why are people with a COPD primarily of chronic bronchitis, sometimes said to be "blue bloaters"?
|
Blue because of cyanosis.
Bloaters because of systemic edema secondary to right ventricular failure. |
|
|
What pulmonary function abnormalities are expected in a patient with COPD?
|
Increased lung resting volume (FRC)
Increased RV Decreased FEV1 (collapse) Decreased VC "Loss of elasticity results in greater lung compliance, or distensibility. This hinders the ability for normal passive exhalation to occur, resulting in increased FRC and RV. Without the normal recoil mechanism, the thoracic cage expands, which increases TLC and results in the characteristic barrel chest." |
|
|
In COPD, air trapping occurs:
A. more in the upper lobes B. more in the lower lobes C. centrally greater than peripherally D. equally throughout E. Cannot be determined |
In COPD, air trapping occurs mostly at the bases, which results in shunting of ventilation to the apices where little perfusion occurs. This results in a ventilation/perfusion mismatch, which has a deleterious effect on gas exchange.
|
|
|
As lung volume increases, lung compliance ________?
|
Increasing lung volume results in stretching of alveoli and interstitial elastin, causing greater stiffness and recoil; therefore, compliance diminishes as lung volume increases
|

