![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
Diastolic BP increases with age. At approximately what age does diastolic BP plateau? |
Around 70 years old |
|
|
Systolic BP increases with age at a constant rate until approximately what age? |
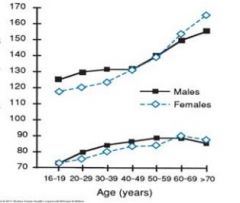
Trick question. Systolic BP continues to rise with age |
|
|
What measurements can differentiate the different stages of hypertension? |
Systolic BP and diastolic BP |
|
|
What systolic and diastolic BPs are needed to classify someone as normal, aka no HTN?
For pre-HTN? |
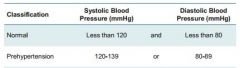
Normal - BP of 120/80 or less. Note that you must have a systolic of 120mmHg or less AND a diastolic of 80mmHg or less
Pre-HTN - a systolic of 120-139mmHg OR a diastolic of 80-89mmHg |
|
|
What systolic and diastolic BPs are needed to classify someone stage 1 HTN?
For stage 2 HTN? |
Stage 1 HTN - S-BP of 140-159mmHg OR D-BP of 90-99mmHg
Stage 2 HTN - S-BP of 160mmHg or greater OR D-BP of 100mgHg or greater |
|
|
For each of the following, determine if each patient is normal, pre-HTN, stage 1 HTN, or stage 2 HTN:
1) Systolic of 119mmHg and diastolic of 90mmHg 2) Systolic of 142mmHg and diastolic of 88mmHg |
1) Stage 1 HTN due to diastolic of 90mmHg 2) Stage 1 HTN due to systolic of 142mmHg |
|
|
T/F: The older you get the less you are able to lower your BP |
True |
|
|
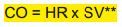
What was the given formula that relates SVR, BP, and CO? |
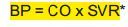
SVR = systemic vascular resistance. It's the total resistance of arterioles to the flow of blood
CO = cardiac output. It depends upon the heart rate and stroke volume (amount of blood pumped each cycle) |
|
|
What determines cardiac output (CO)? In other words, what's the equation for CO? |
HR = heart rate
SV = stroke volume which is the (amount of blood pumped each cycle) |
|
|
A patient has a sudden drop in BP. What is expected to happen to his/her:
Heart rate? Systemic vascular resistance? |
HR - should increase via the two equations SVR - should increase in resistance (BP = CO x SVR) |
|
|
Baroreceptors can detect drops in BP.
Where are they located? Where do baroreceptors signal to? What response would ultimately happen to fix this low BP? |
They can be found in the aorta and carotid arteries.
They send this decreased BP message to the CV center in the medulla of the brain stem.
The CV center's immediate response would be to increase CO and SVR. So vasoconstriction would happen, heart rate would increase, and the amount of blood pumped during each contraction of the heart should increase (via CO = HR x SV) |
|
|
BP = CO x SVR
HTN can be caused by an increase in CO. What mechanisms can cause this increase in CO? |
CO = HR x SV
1) Increase cardiac preload - fluid volume increases due to excess Na intake or less Na secretion through the kidneys. This gives a larger SV.
2) Sympathetic nervous activity can act on the heart and increase HR to increase CO |
|
|
BP = CO x SVR
HTN can be caused by an increase in SVR. What mechanisms can cause this increase in SVR? |
1) Increased stimulation of RAAS (renin-angiotensin-aldosterone system) can cause vasoconstriction
2) Increased sympathetic nervous system stimulation (vasoconstriction of blood vessels) |
|
|
What is hypertrophy?
How is hypertrophy related to HTN? |
Hypertrophy is the enlarging of muscles that are over-worked.
Hypertrophy can happen to the heart and blood vessels for hypertensive patients. |
|
|
Below is an analogue to hypertension mechanisms:
Suppose a balloon is losing air through a small hole (not the opening itself). What ways can you stop the balloon from deflating and keeping the air in? |

1) You can breathe more air into the balloon. (The body would increase CO via increased cardiac preload)
2) Pinch/cover the hole where the air is escaping (The body would increase SVR) |
|
|
Does angiotensin II directly affect CO, peripheral resistance, or both? |
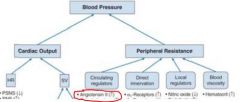
Angiotensin affects peripheral resistance and thus also affects BP
It has many other indirect actions due to this increased resistance |
|
|
Would a sensitized or desensitized baroreceptor possibly contribute to HTN? |
Desensitized
Since baroreceptors alert the CV center in the medulla to changes in BP, a desensitized receptor would no report that the BP has increased and no counter-mechanism would take place to lower the BP |
|
|
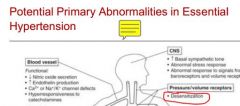
Which of the following ISN'T a possible contributor to high BP/HTN:
Decreased NO levels Desensitization to catecholamines RAAS dysfunction Desensitized baroreceptors
|

Desensitization to catecholamines
Catecholamines like epinephrine often increase BP, thus desensitization wouldn't be a likely cause of HTN |
|
|
T/F: HTN can cause injury to the eyes and kidneys |
True
They can cause damage to the retina and the nephrons |
|
|
What is/are the ideal "sweet spots" for systolic and diastolic BP to reduce mortality? |
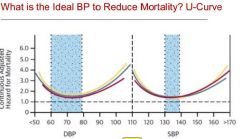
Systolic between 130-140mmHg (surprising as this is pre-HTN/stage 1 HTN range)
Diastolic between 60-80mmHg
Thus I'm not sure how practical this really is. |
|
|
Where/on what system does clonidine exert its main effect? (e.g. is it a diuretic?) |

CNS effects |
|
|
Which of the following does not have anti-HTN effects:
Catecholamine inhibitors Vasodilators Angiotensin I blockers (ARBs) ACEi Aldosterone agonists Diuretics |
Aldosterone agonists
Aldosterone blockers would be a possible anti-HTN mechanism |
|
|
Regardless of the different classes of diuretics, how do diuretics work in general? |
They work by increasing the removal of sodium (Na+). Thus water follows (H2O - O is slightly negative). Less water = less volume in blood = lower BP |
|
|
What are the three classes of diuretics? |
Loop diuretics Thiazides Potassium-sparing diuretics |
|
|
Where do each of the following diuretics exert their MOAs:
Loop diuetics Thiazides K-sparing diuretics |
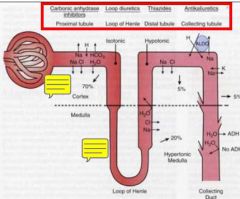
Loop - loop of Henle Thiazides - distal tubule K-sparing - collecting tubules/ducts |
|
|
Where is the majority of Na reabsorbed in the kidney? |
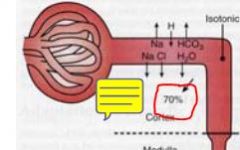
The proximal tubule in the cortex |
|
|
Ignoring the proximal tubule, where is the majority of the remaining Na reaborbed?
What diuretic class works here? |
Loop of Henle
Thiazides |
|
|
---Difficult FYI Q---
Thiazide and thiazide-type diuretics work in the distal tubule. What thiazide/thiazide-type drug is an exception? |
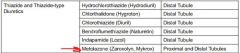
Metolazone - it works on both the proximal and distal tubules |
|
|
What is the MOA of thiazides to reduce BP? |
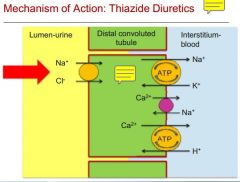
Thiazides inhibit Na/Cl transporter on the LUMEN-urine side to stop reabsorption of Na+
Thus more Na+ in urine and water follows. Less volume in blood means lower BP |
|
|
What other electrolyte besides sodium and chloride is affected by thiazides? |
Potassium
Since Na+ is being excreted, K+ is also affected to maintain an electrolyte balance |
|
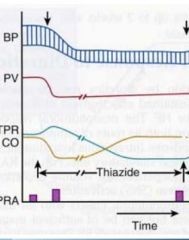
What are the immediate/short term effects of thiazides on BP?
What are the long term effects? |
Short/immediate - plasma volume is decreased and CO is increased (to make up for less plasma volume)
When maintained on thiazides, TPR is decreased while CO returns to baseline |
|
|
Which thiazide/thiazide-like diuretic comes in IV formulation? |
Chlorothiazide |
|
|
Which of the following thiazides has the shortest serum half-life:
Chlorothiazide Hydrochlorothiazide Bendroflumethiazide |
Chlorothiazide - 1.5h Hydrochlorothiazide - 2.5h Bendroflumethiazide - 3-4h |
|
|
Which thiazide/thiazide-like drug is the only one that is hepatically metabolized? |
Indapamide
Thus can be used in renal insufficiency |
|
|
What values should be monitored with chronic thiazide use? (e.g. electrolytes, etc.) |
Magnesium Sodium Glucose levels/tolerance Uric acid levels Calcium
Potassium is also affected, but we don't tend to monitor this one as much unless there is a reason to |
|
|
For each of the following, will values rise (hyper-) or lower (hypo-) with chronic thiazide use:
Mg Ca Uric acid Na K |
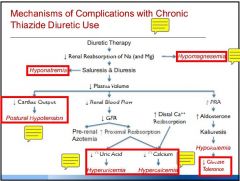
Hypo - Mg, Na, and K (Mg follows Na to be excreted)
Hyper - Ca and uric acid levels (Ca clearance is lowered) |
|
|
Why are thiazides to be used with caution in patients with gout? |
Increased uric acid levels from thiazides can worsen gout |
|
|
How do thiazides and loop diuretics greatly differ in their effects on calcium? |
Thiazides cause hypercalcemia
Loop diuretics increase Ca clearance, thus do not cause hypercalcemia |
|
|
Which class is more effective for HTN: loop diuretics or thiazides? |
Thiazides are superior anti-HTN drugs |
|
|
What population/disease-type are loop diuretics mostly used in? |
Patients with renal insufficiency (all loop diuretics in class are at least 33% hepatically eliminated) |
|
|
How do thiazides and K-sparing drugs differ in their effects on potassium? |
Thiazides cause hypo-K
K-sparing cause hyper-K |
|
|
K-sparing diuretics technically have two sub-classes. What are they and how do they differ in MOA? |
1) K-sparing agents (amiloride & triamterene) - work by inhibiting transporters in the collecting duct
2) Aldosterone antagonists (spironolactone & eplerenone) - work by inhibiting the aldosterone receptor which normally reabsorbs Na. (note spironolactone has a 100-fold greater affinity for androgen & progesterone receptors than eplerenone) |
|
|
Which K-sparing diuretic is eliminated by the kidneys? |
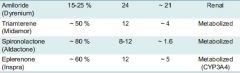
Amiloride |

