![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
174 Cards in this Set
- Front
- Back
|
What are some problems with peptides as drugs?
|
Hard to identify initially
Expensive to purify Immune reactions if animal products used Human form often required Difficult to synthesize chemically Ineffective orally (poor absorption and rapidly hydrolyzed) Require injection (unpleasant and still rapid hydrolysis) |
|
|
Technical advances in peptides as drugs
|
Available due to Human Genome Project
Produced by recombinant DNA technology (important for GH and insulin) Novel amino acids to prevent hydrolysis (desmopressin, octreotide) Route of admin: nasal, inhaled, transdermal, needle-free delivery devices, one oral drug = desmopressin) |
|
|
Other technical advances in peptides as drugs
|
Optimize AA sequence for potency/specificity, onset/duration of action, oral non-peptide mimetics etc.
|
|
|
Growth hormone uses
|
Promoting growth in children
Body maintenance in adults |
|
|
Growth hormone preparations
|
Only human hormone works
Human cadaver product used but not anymore b/c Creutzfeldt-Jakob |
|
|
Growth hormone recombinant hormone preparations (used now)
|
Somatropin (exact human sequence)
-Depot preparation 1-2/month Somatrem (human sequence plus extra methionine) Give these drugs IM or SC (2-7/week |
|
|
Growth hormone effectiveness
|
Increased linear growth (until epiphyseal closure)
Decreased fat, increased muscle and bone Increased sense of well-being Maintenance of adult physiology EXPENSIVE |
|
|
Growth hormone approved uses
|
GH deficiency in children and adults
Turner's and Prader-Willi syndromes "Idiopathic short stature" - controversial b/c not deficient Renal insufficiency AIDS cachexia Short bowel syndrome |
|
|
Growth hormone efficacy and safety
|
Delayed growth and wound healing in severe burns
Abuse by athletes/body-builders Laron dwarfism (patients have GH receptor defect) - not responsive to GH agonist - require IGF = "end organ hormone" |
|
|
Sermorelin
|
Works at hypothalmic level
Synthetic human GHRH Stimulates release of GH Requires pituitary function IV, SC, nasal administration Cheaper than GH and may be less effective More diagnostic than therapeutic and side effects not known |
|
|
Octreotide
|
Growth hormone inhibitor
Somatostatin analog with an 8-amino acid cyclin peptode Hypothalmic SS: inhibits GH release and inhibits TSHG and prolactin release Pancreatic SS: inhibits release of insulin and glucagon Gut SS: inhibits release of VIP SS not useful clinically because action too short and too much insulin effect |
|
|
Octreotide uses
|
Inhibit GH secretion (acromegaly)
Metastatic carcinoid (5HT-secreting tumor) VIP-secreting tumors Inhibit TSH and glucagon secretion Treating GI secretion disorders |
|
|
Key properties of Octreotide
|
Longer acting than SS
Less effect on insulin than SS (10-20x more selective) Some SS receptor subtype selectivity) - prefers SSTR-2 and 5 receptors which are expressed on hormone-secreting tumors |
|
|
Octreotide administration
|
Given SC 2-3/day
Newer long-acting depot preparations |
|
|
Octreotide side effects
|
GI side effects
Diarrhea, nausea, flatulence, malabsorption, gallstones EXPENSIVE |
|
|
Prolactin
|
No drug preparations
|
|
|
Dopamine
|
Endogenous inhibitor of PRL release
Numerous DA drugs alter prolactin DA agonists = inhibit prolactin release (anti-Parkinson's drugs) DA antagonists = cause hyperprolactinemia (anti-psychotics and anti-depressants) Dopamine itself not useful so use analogs |
|
|
Cabergoline
|
Effects D2 dopamine receptor agonism
Relatively D2 selective Inhibits prolactin release |
|
|
Uses of cabergoline
|
Hyperprolactinemia (infertility)
Decrease prolactinoma tumor mass Suppression of lactation Acromegaly (inhibits GH too in acromegaly patients, stimulates in normals) |
|
|
Cabergoline side effects and preparations
|
Non-peptide drug is orally effective and also has a vaginal preparation
Side effects = nausea, dizziness, hypotension Tolerance usually develops |
|
|
Other dopamine agonist analgogs
|
Good D2 action but also D1, shorter half-lives, multiple doses daily
Bromocriptine acts on D2 receptors Cabergoline preferred because of long action |
|
|
Posterior pituitary hormones
|
Vasopressin (ADH)
Released in response to increased osmolarity or a decrease in blood pressure Actions: increase renal water absorption and vasoconstriction to increase blood pressure |
|
|
Actions of vasopressin
|
Acts on G-protein coupled receptors
V1 receptors: vascular smooth muscle increases constriction V2 receptors: kidney increaes water reabsorption, and acts on endothelial cells increasing clotting factors U |
|
|
Uses of vasopressin
|
V2: Diabetes insipidus
V1 and V2: bleeding disorders |
|
|
Arginine vasopressin
|
Synthetic human vasopressin
IV, IM, SC, nasal Short-acting Acts on both V1 and V2 receptors but agent of choice for V1 effects |
|
|
Arginine vasopressin uses
|
Agent of choice for short term uses (whether V1 or V2)
Local bleeding artery (V1) Temporary diabetes insipidus following pituitary surgery (V2) |
|
|
Desmopressin acetate
|
Stable peptide analog
Long-acting (10-20 hours) Highly V2 selective IV, SC, Inaled First oral peptide drug |
|
|
Desmopressin acetate uses
|
Treatment of choice for diabetes insipidus (nasal has been but oral may be soon)
Increase clotting factor synthesis in hemophilia, von Willebrand's Nocturnal enuresis (to concentrate urine) (nasal prep no longer used for this) All V2 effects |
|
|
Side effects of vasopressin analogs
|
V1 receptors: increased BP, GI cramps, headaches
oxytocin receptor: uterine contractions, cramps Occur with AVP, little with DDAVP |
|
|
Oxytocin
|
Used to control labor, post-partum bleeding, and lactation
|
|
|
Thyroid drugs general information
|
Not peptides
Small, lipid-soluble hormones (but made as part of a large protein) Both suppressive and replacement therapy Larged stored reservoir of thyroid hormones in the colloid cells (3 month supply) |
|
|
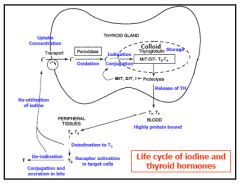
Life cycle of iodine and thyroid hormones
|
|
|
|
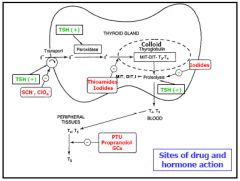
Sites of drug and hormone action
|
|
|
|
Life history of thyroid hormones
|
Iodide uptake
Oxidation of iodide, iodination of tyrosines, and coupling on TG, all by peroxidase Stored as part of TG in colloid T3, T4 released by proteolysis of TG, secreted Highly protein bound--TBG, transthyretin Metabolism -deiodination, iodine reutilized -conjugation, excretion in bile and urine True for drug forms too |
|
|
T3 vs. T4
|
5X more T4 secreted than T3
T3 is mainly from peripheral deiodination of T4 T4 = 99.9% bound in plasma, half-life = 6-7days T3 = 99% bound in plasma, half-life = 1-2days Protein binding of T4 slows its metabolism T3 is 5-10X more potent than T4 Most of hormone in plasma is T4 while most of effect is T3 |
|
|
Thyroid hormone receptor
|
Nuclear Transcription factor
Maybe cell surface and mitochondrial TH-Rs to explain more rapid "non-genomic" effects |
|
|
Thyroid hormone effects
|
Stimulation of growth and development (both physical and mental)
Stimulation of metabolism (both synthesis and degradation) -Carbohydrate, fat, protein Increased O2 consumption, heat production Increased sympathetic nervous system activity Increased production and degradation of other hormones (ex. insulin, glucocorticoids) |
|
|
Thyroid hormone targets
|
Nearly all tissues (heart, liver, muscle, fat)
Exert long-term effects (not minute to minute) -hormones have long half-life and effect protein synthesis |
|
|
Hypothyroidism
|
Primary--thyroid gland failure (95%)
-Hashimoto’s thyroiditis--anti-thyroid Abs -low iodine in diet -goitrogens in diet -prior treatment of hyperthyroidism -congenital defect Secondary--pituitary or hypothalamic failure |
|
|
Hypothyroidism types - infant, adult, myxedema coma
|
Hypothyroidism
Infant hypothyroidism--cretinism -dwarfism, mental retardation -↓ 3-5 IQ pts/mo -routine neonatal screening (~1/6000) Adult hypothyroidism--myxedema -symptoms listed, follow from TH effects -slowed metabolism, decreased SNS, cold, tired -symptoms often minimal; lab detection Myxedema coma -endstage of untreated hypothyroidism -usually a precipitating stress -medical emergency; symptoms listed |
|
|
Treatment of hypothyroidism
|
Dietary changes
-if due to goitrogens or inadequate iodine Replacement thyroid hormones -usually oral, except IV in emergency -usually lifelong, but some remissions -effective, cheap, easy, painless, safe -avoid animal extracts if synthetic available |
|
|
Levothyroxine (T4)
|
Major drug used
Longer duration, 1/day dosing (or less) Slowly converted to T3 in body Steady, predictable response Even preferred in myxedema coma over T3 |
|
|
Liothyronine (T3)
|
Effect too rapid and short for long-term replacement therapy
Limited specific uses for T3 in thyroid cancer: -to maintain suppression and support while tapering off of T4 prior to surgery or RAI -for more rapid onset of TH effects while restarting T4 after surgery or RAI -when a short effect is desired -rarely for depression or to supplement T4 |
|
|
Liotrix
|
T4 + T3 (don't use)
|
|
|
Thyroid hormone preparations
|
Product variability:
-up to 20% differences among brands, suppliers -"similarly" effective, but avoid switching -FDA working on standardization, consistency -3 specific generics recently FDA approved Slow onset and reversal of effects: -days to weeks(time required to fill binding sites; new protein synthesis; resetting metabolism; long half-life of TH) -small and gradual dose changes, careful monitoring, esp. cardiac function |
|
|
Thyroid hormone special preparations - elderly/cardiac, pregnancy, myxedema coma
|
Be cautious when using in elderly and cardiac patients because they may need these drugs for their health, but they strain the heart
Continue use in pregnancy -to maintain pregnancy -requirements increase -early fetus needs maternal TH Myxedema coma -IV bolus to fill plasma binding sites -supportive therapy |
|
|
Thyroid hormone side effects and drug interactions
|
Hyperthyroid symptoms due to overdosage
Interacts with drugs that alter thyroid function/effects & drugs that alter TH absorption/binding/metabolism |
|
|
Suppressive thyroid therapy
|
Thyroid cancer
–suppress release of TSH which can stimulate growth of thyroid tumor cells Non-toxic goiter -for mild hypothyroidism with obvious goiter –to suppress the elevated TSH that is causing thyroid enlargement –both suppressive and replacement |
|
|
Hyperthyroidism: types, causes, symptoms
|
Graves’ disease (diffuse toxic goiter)
-antibodies with TSH-like activity -no feedback regulation Toxic thyroid adenomas (nodular goiters) Symptoms follow from TH effects -increased metabolism, SNS activity; insomnia Thyroid storm -crisis hyperthyroidism -usually triggered--illness, thyroid surgery, 131I therapy -medical emergency |
|
|
Hyperthyroidism therapy
|
Symptomatic relief with sympatholytics
-Propranolol (beta-blocker and also inhibits T4 conversion to T3) Disease modifying treatment: -antithyroid drugs that are non-destructive (thioamides and iodides) -antithyroid drugs that are non-surgically destructive destructive (radioactive iodine) -partial thyroidectomy = surgical destruction |
|
|
Thioamides (effective inhibitors of TH synthesis)
|
Propylthiouracil
Methimazole First line therapy and non-destructive Average therapy about 1 year with some patients experiencing remission Most progress to radioiodine or surgery |
|
|
Pharmacokinetics of thioamides
|
oral, well absorbed
concentrated in thyroid – effective t½ 4-5X longer than plasma t½ methimazole 10X more potent than PTU methimazole longer half-life than PTU – 1/d dosing increases compliance – PTU 2-4/d dosing metabolism – conjugation, excretion in urine |
|
|
Mechanism of action of thioamides
|
inhibit peroxidase:
-iodination, coupling do not inhibit release of preformed TH –latent period for effects (1-2 weeks) PTU inhibits T4 conversion to T3 –more rapid effect in thyroid storm –methimazole does not do this possibly anti-autoimmune mechanisms –basis for the remissions? |
|
|
Adverse effects of thioamides
|
agranulocytosis
–rare (1/500) but can be fatal –usually in first few months of therapy –warn patient to watch for signs of infection: sore throat, fever, flu-like -discontinue the drug -treat infection with antibiotics -don’t use thioamides again skin rash, drug fever, arthralgia, myalgia hypothyroidism, goiter –adjust dose |
|
|
Using thioamides during pregnancy or breast-feeding
|
treat mild hyperthyroidism in mother
–mother can tolerate a little too much TH –to avoid any hypothyroidism in infant –both PTU and methimazole readily cross placenta and into breast milk –PTU preferred here, because more highly protein-bound definitive therapy prior to pregnancy best |
|
|
Iodide uses
|
Inhibit synthesis and release of THs
-effect on release gives more rapid effect -useful in treating thyroid storm -limited duration of effect (gland adapts to inhibition and "escapes", increased iodide then increases TH, so only short-term use) Decrease size and vascularity of thyroid gland -major use is last 10 days prior to thyroidectomy, for cleaner, safer surgery -vasoconstrictor effect to "firm up" the gland |
|
|
Iodide cautions and side effects
|
Do not use prior to radioactive iodine
-will decrease uptake, concentration of 131I Sometimes used to reduce TH release and symptoms following radioiodine Used in radiation emergencies -to decrease uptake of radioactive iodine into thyroid which could cause thyroid destruction or cancers (e.g., very effective after Chernobyl) Side effects: sore throat, burning mouth, rash, diarrhea |
|
|
Iodide preparations
|
Potassium iodide
oral, either solutions or tablets |
|
|
Radioactive iodide
|
131I = most
Properties: -half-life ~ 8 days 15% gamma radiation –thyroid diagnostic and imaging use 85% weak beta radiation –therapeutic use –travels 1-2 mm in tissue –localized destruction |
|
|
131I uses and contraindications
|
Easy, effective, cheap, relatively painless
Often the treatment of choice Small (μCi) doses for diagnosis Larger (5-15 mCi) doses for non-surgical destruction of thyroid -given orally, concentrated in thyroid -local beta radiation destroys thyroid cells over course of several weeks -minimal radiation danger to other organs (no thyroid or other cancers induced) Contraindicated in pregnancy, breastfeeding, young children |
|
|
Adverse effects of radioactive iodine
|
Some radiation thyroiditis, salivary adenitis
Often results in hypothyroidism –transient or permanent –treat with replacement levothyroxine |
|
|
Partial thyroidectomy
|
This is surgery, but drugs still very important!
1. thioamides for 5-6 wks to make euthyroid 2. iodides last 2 wks to decrease size and vascularity of gland 3. surgical removal of bulk of thyroid 4. drugs to reduce and/or treat surgery induced thyroid storm 5. replacement levothyroxine for hypothyroidism that may result |
|
|
Specific uses of partial thyroidectomy
|
thyroid cancer
anti-thyroid drug failure during pregnancy patient who refuses radioiodine |
|
|
Treatment choice for hyperthyroidism
|
Patient’s age
-young: methimazole -older: radioactive iodine Pregnancy, breast-feeding -propylthiouracil safer than methimazole -surgery prior to pregnancy preferred -avoid radioiodine Other factors -size, severity, duration, pathophysiology -surgical risk |
|
|
Treatment for thyroid storm
|
Propylthiouracil
-to decrease conversion of T4 to T3 Iodide -to decrease release of preformed TH Glucocorticoids -prevent shock -also slows conversion of T4 to T3 Symptomatic relief of sympathetic effects -propranolol (beta blocker) –also inhibits T4→T3 -diltiazem (calcium channel blocker) |
|
|
Insulin
|
Peptide, pancreatic B cells
Stored complexed with zinc (2 zinc:6 insulin) Released in response to elevated glucose Short half-life (3-5 min) Degraded by proteolysis in liver and kidney |
|
|
Metabolic actions of insulin
|
Decrease blood glucose
-increase uptake, utilization, storage -decrease synthesis -multiple effects on transporters and metabolic enzymes for sugars, amino acids, lipids Growth factor effects |
|
|
Insulin receptor
|
Tyrosine kinase activity
Mediates insulin internalization for degredation |
|
|
Insulin therapy
|
Pharmacological replacement therapy:
-highly purified insulins -required for Type 1, often used for Type 2 A peptide, requires injection -inhaled prep available briefly but gone now Goal: mimic normal physiologic insulin levels -which vary with meals, activity Things to avoid -hyperglycemia from inadequate insulin, either post-prandial (after meal) or chronic (acute and chronic dangers) -hypoglycemia from excess insulin, delayed or missed meal, or excess physical activity (acute danger, including death) |
|
|
Insulin preparations
|
All equal "efficacy"
-i.e. full agonists at insulin receptors Formely 6 preparations: only 2 still in use -Others used excess Zn2+ to precipitate insulin(to slow absorption and prolong action) -Cloudy suspensions that could not be used IV -Complications with mixing preparations (order of drawing into the syringe) New synthetic insulins have replaced these |
|
|
Regular insulin
|
-rapid-acting and short-acting
-readily soluble and rapidly absorbed (physiological level of zinc, no added protein to slow action) -onset ½-1 hr, peak 2-4 hr, duration 5-8 hr -a clear solution, can be given IV |
|
|
Isophane insulin suspension (NPH)
|
-complexed with protein protamine at neutral
pH (Neutral Protamine Hagedorn, Isophane) -slower onset, longer action than regular -onset 1-2 hr, peak 6-12 hr, duration 18-24 hr -a cloudy suspension, NOT given IV (because particles can clog IV line) |
|
|
Use of regular insulin
|
For glucose control after a meal due to rapid onset and short duration
Needs to be injected 30 minutes to a half-hour before a meal Available without prescription |
|
|
Use of isophane
|
Used for glucose control between meals and overnight due to slower onset and longer action
Available without prescription |
|
|
Biosynthetic modified insulin analogs
|
Rapid and short
-Insulin Lispro -Insulin Aspart -Insulin Glulisine Slow and long -Insulin Glargine -Insulin Detemir All synthetic insulins require a prescription |
|
|
Insulin lispro
|
Also called Humalog
Aggregates less so there is a more rapid effect Kinetics most closely resemble endogenous Can be injected immediately before meal Can be given IV like regular insulin Better control of glucose load and less post-meal hypoglycemia |
|
|
Insulin aspart
|
Novolog
Somewhat slower onset and longer duration than lispro Somewhat faster and shorter than regular insulin Injected immediately before meal and can be given IV |
|
|
Insulin glulisine
|
Same principle as insulin lispro and insulin aspart
Injected before or immediately after meal Marketed specifically for use with insulin glargine, to control post-prandial glucose surge (both are pH 4) |
|
|
Insulin glargine
|
Gly switch, plus two Arg retained from C peptide
-These substitutions alter the solubility properties, to slow absorption, increase duration Formulated with Zn at pH 4 to further slow absorption (cannot be mixed with other pH insulins, only glulisine) Absorption -soluble prior to injection -precipitates when injected SC (used 1/day) -very slow dissolution from injection site and somewhat variable absorption "Peakless" or "flat" -"opposite" properties from lispro, aspart -long, low, constant activity for >24 hr |
|
|
Insulin detemir
|
Levemir
Thr deleted, 14-carbon FA added (myristic) Fatty acid chain slows release, prolongs action Similar to glargine, but: -better and less variable absorption -somewhat shorter than glargine -may need 2 injections per day |
|
|
Duration of action of all the insulins
|
Ultrashort
-Lispro -Aspart -Glulisine Rapid/Short -Regular Intermediate -Isophane (NPH) Slow/Long -Detemir -Glargine |
|
|
Inhaled insulin (Exubera)
|
Withdrawn in 2007
Contained normal human insulin for inhalation Avoided injection, its major plus Had complications -limited dosing options were available -the inhalation device had problems -there were complications with lung delivery -concerns with smoking and asthma Not disapproved by FDA but voluntarily withdrawn by manufacturer |
|
|
Glucose monitoring and insulin delivery methods
|
Convenient personal glucose monitoring
-new subdermal implanted continuous monitor marketed this year Convenient injection devices -pens, cartridges, color-coded -pens require prescription -needle-free injection devices CSII (continuous subcutaneous insulin infusion) -open loop--manual control -closed loop--controlled by sensor -pumps now use lispro and glulisine rather than regular insulin Experimental delivery methods -transdermal, oral, better inhaler options |
|
|
Diabets control and complications
|
Diabets control and complications trial (DCCT)
-Major study, published 1993 -Compared "tight" control (intensive insulin therapy) vs "traditional" in Type 1 diabetics -Tighter control of glucose levels clearly reduces long-term complications -implicates hyperglycemia as major risk factor -requires more frequent monitoring and more frequent injections -may increase the risk of acute hypoglycemia UK Prospective Diabetes Study (UKPDS) -Tight control similarly important for Type 2 |
|
|
New issues in diabets control
|
Tighter control does a better job of controlling blood glucose and long-term complications
But appears to be INCREASING rather than decreasing mortality Similar issues arising with other drugs and what may be inappropriate "biomarkers" |
|
|
Insulin side effects of hypoglycemia
|
Dose too high, missed meal, exertion
Sympathoadrenal symptoms -sweating, weakness, hunger, tachycardia, anxiety, tremor CNS symptoms -headache, blurred vision, confusion, incoherent speech, convulsions, coma Or can occur without symptoms Treatment -glucose, juice, candy, honey -glucagon IM -glucose IV Wear warning bracelet -Patient, family and co-worker education |
|
|
Insulin side effects of immunologic actions
|
Insulin allergy
-immediate hypersensitivity, rare Insulin resistance -development of anti-insulin antibodies –occurs in most patients –even with human insulins -may also involve receptor subsensitivity Lipodystrophy at site of injection -rotate site of injection All less common with purified preparations, especially recombinant human insulins |
|
|
Insulin side effects - weight gain
|
Insulin therapy can cause weight gain, particularly in Type 2 diabetics
This is obviously counter-productive |
|
|
Drug interactions with insulin
|
Agents that increase glucose, decrease insulin, and/or inhibit insulin effectiveness:
-growth hormone, glucocorticoids -glucagon, beta agonists -estrogens, progestins, OCs -thiazide diuretics -calcium channel blockers -alpha-2 agonists, beta blockers -sulfonamides -MAO inhibitors -anabolic steroids -captopril, disopyramide -ethanol, salicylates Propranolol and other beta blockers dangerous -increase hypoglycemia risk -also mask symptoms of hypoglycemia Special precautions for surgery and pregnancy |
|
|
HYPERglycemic agents for treating HYPOglycemia
|
Glucose
-oral--candy, honey, syrup -gel -if patient remains conscious -IV in severe emergency Glucagon -IM or SC -if patient becomes unconscious -opposite effects of insulin, therefore counteracts insulin excess by multiple mechanisms Diazoxide -ATP-sensitive K+ channel opener |
|
|
Diazoxide
|
-inhibits insulin secretion
-binds and activates (opens) ATP-sensitive K+ channel -ATP from glucose, and some oral agents, inhibit this channel to increase insulin release -diazoxide activates the channel, thereby decreases insulin release, less hypoglycemia |
|
|
Type 2 Diabetes: The Problems
|
Obesity (sedentary, overeating)
Insulin resistance in liver and muscle (receptor subsensitivity) High glucose in spite of increased insulin from pancreas and excess dietary glucose to fight also Gut and fat hormones may be new targets for drugs |
|
|
Key points for Type 2 Diabetes Mellitus
|
Insulin is present, in fact often elevated
-so it is not really insulin that they need -they need their insulin to work better -or less glucose for insulin to work against But patients are often insulin "resistant" -sub-sensitive, not in-sensitive -giving more insulin, or increasing endogenous insulin release, may help overcome this relative resistance Insulin is used/required for many Type 2 diabetics, not only for Type 1 |
|
|
Approaches to treating Type II Diabetes
|
Synthesize and release more insulin
Make more insulin recptors or make them more senstive Increase glucose uptake and storage and decrease endogenous glucose production Bring less glucose into body and bloodstream from gut |
|
|
Oral anti-diabetic agents general information
|
Don't require injection
Only used for Type II Often used in combination with each other and with insulin *None used in Type I |
|
|
Global concepts of oral anti-diabetic agents
|
Always switch to insulin itself in pregnancy and for
surgery -for more direct control -using only a "natural" compound Increased hypoglycemia risk with some combos -drugs that increase insulin or its actions -caution in combining with insulin or each other Weight gain is a concern with several drugs -including insulin itself -counter-productive in Type 2 diabetes |
|
|
Sulfonylureas mechanism of action
|
Increase insulin secretion
–block ATP-sensitive K+ channels –same site of action as glucose insulin "secretagogues" increase tissue sensitivity –increase receptor number –increase post-receptor effects decrease glucagon secretion |
|
|
Blocking K+ Channel
|
Increases insulin release
Glucose -> ATP which blocks the K channel and stimulates release Sulfonylureas and meglitinides block ATP sensitive potassium channels and increase insulin secretion |
|
|
Second generation sulfonylureas
|
more potent, much safer
Glipizide (Glucotrol®) Glyburide (Diabeta®, Glynase®, Micronase®) Glimepiride (Amaryl®) - may be less prone to cause hypoglycemia than other two |
|
|
Pharmacokinetics, Side effects, and Contraindications of sulfonylureas
|
Pharmacokinetics
-multiple daily doses; or 1/d extended release -oral, well-absorbed, protein-bound -metabolized by liver and kidney -excreted in urine and bile Side effects -hypoglycemia, esp. together with insulin -often cause weight gain -rarely GI, skin, liver, blood cell problems -few drug interactions Contraindications -liver or kidney disease (because metabolized by liver and excreted by kidney) |
|
|
Meglitinides
|
Repaglinide (Prandin®)
Non-SU structure, but same mechanism of action and same effects as SUs (a SU "cousin") -bind a different component of the ATP-sensitive K channel than the "SU receptor" Rapid and short-acting -taken 30 min before meal for post-prandial control (faster than SUs) May be safer than SUs -hypoglycemic, but less likely than SUs -less danger in kidney disease |
|
|
Biguanides (Metformin)
|
Metformin (Glucophage®)
-first non-SU drug available -only metformin in USA -controversy because of lactic acidosis seen with earlier biguanide phenformin -less lactic acidosis risk with metformin Becoming a first line drug: -especially for obese patients who are insulin resistant -an interesting rise from "hard to get approved" up to "first-line therapy" Glucovance®: metformin-glyburide combo |
|
|
Metformin mechanism of action (biguanide class)
|
different from SUs; effects primarily in liver
-decreases glucose production and increases glucose uptake into cells -increases insulin effectiveness but not insulin secretion -acts by activating AMP-dependent protein kinase (AMP-K) involved in glucose regulation |
|
|
Metformin uses, advantages, and pharmacokinetics (biguanide class)
|
Uses
-together with insulin in insulin resistance -together with SUs (different mechanisms) -together with other oral agents Pharmacokinetics -oral, well-absorbed, not protein-bound -2-4 times per day; or 1/day extended release -renal excretion without metabolism -dangerous in patients with kidney disease or conditions that may compromise renal function Advantages -does not cause hypoglycemia because not increasing insulin secretion -does not cause weight gain |
|
|
Metformin disadvantages and side effects
|
Disadvantages, side effects
-risk of lactic acidosis –metformin inhibits lactic acid metabolism –rare but frequently fatal –alcohol and hypoxia also increase lactic acid (interactions) -metformin dangerous in kidney disease (since metformin secreted unmetabolized) -potential concern in liver disease also (liver required for lactic acid metabolism) -unpleasant GI side effects (metallic taste, diarrhea, nausea, vomiting, anorexia) |
|
|
Alpha-glucosidase inhibitors
|
Acarbose (Precose®)
Miglitol (Glyset®) Structure and mechanisms -microbial saccharides or analogs -inhibit α-glucosidase, amylase -block hydrolysis of disaccharides and complex sugars, mainly in GI tract -slow formation and absorption of glucose Use -in mild disease or together with other agents -taken 30 min before each meal -for post-prandial glucose control |
|
|
Alpha-glucosidase inhibitors names of drugs
|
Acarbose (Precose®)
-oligosaccharide, so poorly absorbed and remains in the gut Miglitol (Glyset®) -smaller monosaccharide from plants so does not get absorbed |
|
|
Adverse effects of Alpha-glucosidase inhibitors
|
-don't cause hypoglycemia on their own, but… when combined with insulin or SU
–increases risk of hypoglycemia –sucrose NOT effective for hypoglycemia GI: flatulence, cramps, diarrhea -tolerance develops –additive with those of metformin |
|
|
Thiazolidinediones (glitazones)
|
Rosiglitazone (Avandia®)
(and fixed combo w/metformin (Avandamet®)) Pioglitazone (Actos®) -Appear to be less hepatotoxic -But much current concern about CV risk |
|
|
Effects of Thiazolidinediones
|
-do not increase insulin secretion
-do increase responsiveness to insulin -most insulin effects are enhanced liver: decreased glucose and triglyceride synthesis and release muscle: increased glucose uptake and utilization adipose: increased glucose uptake, decreased fatty acid production remember metformin mainly alters liver; these have more effect on muscle and fat |
|
|
Mechanism of Action of Thiazolidinediones
|
activate PPAR-γ
–peroxisome proliferator-activated receptor – a nuclear receptor/transcription factor –a PG-J2 is endogenous ligand –enhance transcription of insulin-responsive genes (which mostly code for glucose-handling enzymes, transporters, etc.) may act via AMP-Kinase also –the metformin target |
|
|
Use of Thiazolidinediones
|
sometimes alone, more often together with insulin, SUs, metformin
in patients with insulin resistance can reduce or eliminate insulin requirement the prototypical insulin "sensitizers" important tools for treating insulin resistance |
|
|
Pharmacokinetics of Thiazolidinediones
|
oral, taken with food
only once per day liver metabolism, excretion in bile dangerous in patients with liver disease relatively safe in patients with renal disease |
|
|
Side effects of Thiazolidinediones
|
-still concern with liver toxicity (liver function tests every 2 months)
EDEMA recent data on rosiglitazone CV toxicity –increased congestive heart failure –increasing evidence for ischemia, angina, myocardial infarction -recommended for use with insulin -not "powerful" drugs, risky, use decreasing |
|
|
Problem: Inadequate insulin secretion (pancreas)
|
sulfonylureas, repaglinide
"Releasers" |
|
|
Problem: Insulin resistance (muscle, fat)
|
thiazolidinediones
"Sensitizers" |
|
|
Problem: Too much endogenous glucose (liver)
|
metformin
"Reducers of glucose" |
|
|
Problem: Too much glucose coming in (gut)
|
acarbose, miglitol
|
|
|
Drug choice: Rationale for use
|
Newly diagnosed
-if thin, normal insulin levels (i.e. not insulin-resistant), start with a "releaser" to increase insulin (they also increase sensitivity some) -if obese (likely to be insulin-resistant) (start with a "sensitizer" to make insulin work better or metformin, to avoid weight gain and resistance) -liver or renal dysfunction must be considered! Ongoing -add second oral agents as needed, based on disease changes and drug effects -metformin to increase glucose use, sensitizer or releaser to increase insulin action, acarbose to decrease glucose uptake, etc Add insulin injections if necessary -continue oral agents -cut back on "releasers" (avoid hypoglycemia), use "sensitizers" and "glucose reducers" to "help" insulin |
|
|
Exenatide
|
analog of glucagon-like peptide-1 (GLP-1)
-an "incretin" –gut peptide released in response to food –exendin-4 (exenatide) in Gila monster saliva! multiple mechanisms –potentiates insulin secretion –decreases glucagon secretion –slows gastric emptying, promotes satiety clinical effects –moderate decrease in fasting glucose –major decrease in post-prandial glucose –no weight gain, may induce weight loss –non-diabetics "abusing" it for weight loss |
|
|
Use and concerns of exenatide
|
approved use
-only together with SUs or metformin –not for use with insulin or alone –a peptide, so requires injection –injected SC before breakfast and supper concerns –nausea –increases hypoglycemia, esp. with SUs –decreases absorption of some drugs contraceptives, antibiotics -take these 1 hr before exenatide –avoid in patients with renal disease |
|
|
Sitagliptin
|
di-peptidyl-peptidase-4 (DPP-4) inhibitor
-prevents degradation of the endogenous incretins such as GLP-1 -increasing concentrations of endogenous incretins orally is likely to be doubly preferable to injecting exogenous incretin analogs oral, once per day approved for use as monotherapy, or with metformin, or with thiazolidinediones no weight gain OR loss no major side effects (yet--still new!) |
|
|
Pramlintide
|
analog of amylin
-peptide hormone released with insulin from pancreatic beta cells –acts on amylin receptors effects –decreases post-prandial glucose and liver glucose formation –limits glucose fluctuations –decreases amount of rapid insulin needed –slows gastric emptying, increases satiety –so does not cause weight gain |
|
|
Pramlintide approved uses
|
Type 1 or 2 diabetics on insulin and not controlled by insulin alone
only use with insulin, not by itself injected SC before meals note this is two drugs injected each meal but clinicians say patients "love" these drugs in spite of injections; perhaps because they work and reduce weight |
|
|
Pramlintide concerns
|
mild nausea, headache
can increase risk of hypoglycemia (so reduce rapid insulin dose, which is the goal with this drug anyway) avoid with drugs that decrease GI motility or GI drug absorption renal excretion, so avoid in kidney disease |
|
|
General uses of cortisol and analogs
|
Endocrine replacement drugs:
-low "physiological" doses -effective, safe Anti-inflammatory drugs --high "pharmacological" doses --very effective, very toxic |
|
|
Glucocorticoid metabolism
|
Regulation is by synthesis
Metabolized by reduction, conjugation, urinary excretion |
|
|
Diurnal rhythm of glucocorticoids
|
High in the mornng and low at night
|
|
|
Effects of glucocorticoids - primary
|
increase in glucose
–adrenal diabetes, insulin resistance increase in protein breakdown –muscle atrophy, weakness mobilization, redistribution of fat –buffalo hump, moon face |
|
|
Effects of glucocorticoids - cardiovascular
|
mineralocorticoid effects
glucocorticoid effects –increase cardiac output –potentiate epinephrine vasoconstriction |
|
|
Effects of glucocorticoids - additional effects
|
decrease body Ca2+
–decreased GI absorption stimulate gastric acid, pepsin secretion alter neuronal function inhibit growth induce fetal lung surfactant |
|
|
Feedback regulation of glucocorticoids
|
inhibit ACTH secretion
suppression of H-P-A axis inability to respond to physiological stress |
|
|
Glucocorticoid pathology
|
Cushing's: Hypercortisolism
-moon face, buffalo hump, muscle wasting,bruise easily, slow healing, osteoporosis, hypertension, diabetes, mental disturbances Addison's: Adrenal deficiency -hyperpigmentation, weakness, weight loss, hypotension, depression, low glucose Drug use to treat both conditions: -"Cushingoid" symptoms occur with GC toxicity -"Addisonian" crisis can occur on GC withdrawal |
|
|
Inflammation and glucocorticoids
|
Inflammation
-redness, swelling, heat, pain -GCs are most powerful anti-inflammatory drugs (but not first choice because of toxicity) -act via GC receptor, not MC receptor |
|
|
Anti-inflammatory mechanisms of GCs
|
-Decrease redness and swelling
(enhance vasoconstriction, decrease vascular permeability, decrease kinin and histamine release) -Decrease fever (heat) and pain (inhibit AA metabolism, decrease PGs and LTs, induce inhibitors of PLA2, decrease COX2 expression) Effects on leukocytes -decrease neutrophils at site of injury -T and B cells, monocytes, eosinophils, basophils sequestered in lymphoid tissue -decrease macrophage phagocytosis Effects on cytokines and other mediators -decrease IL-1,2,3,6, TNFα, GM-CSF, IFNγ, and degradative enzymes -decrease target cell responsiveness also |
|
|
Generalized suppression of immune system using glucocorticoids
|
dangerous side effect
therapeutic immunosuppression cytotoxicity useful in leukemia therapy |
|
|
Effects of mineralcorticoids
|
increase sodium and water retention
-reabsorption in distal tubule –increase blood volume and pressure –hypernatremia, edema, hypertension increase potassium and H+ excretion –hypokalemia, alkalosis |
|
|
Regulation of mineralcorticoids
|
primarily renin-angiotensin system
activated by low blood volume, high potassium |
|
|
Are glucocorticoids protein-bound?
|
YES
Some glucocorticoid drugs are not protein bound which leads to an increase in potency |
|
|
Glucocorticoid regulated genes
|
Both positive and negative GREs
nGREs seem most important for anti-inflammatory effects Similar mechanisms for mineralocorticoid receptor; but different hormone and drug selectivity, different cells, different genes, different proteins |
|
|
Cortisol and mineralcorticoid action
|
Cortisol: is both GC and MC and is rapidly degraded
Drugs: increase potency, duration, receptor selectivity -by adding side-chains/molecules |
|
|
Glucocorticoid preparations
|
All effective orally
-good for long-term replacement Water-soluble for parenteral use -emergency use, unable to swallow Poorly soluble suspension -sustained effect when given IM Local administration: avoid systemic toxicity -inhalers -nasal sprays -ointments and skin creams -ophthalmic preparations -enemas, suppositories -intra-articular injection |
|
|
Anti-inflammatory and immunosuppressive uses of glucocorticoids
|
Arthritis, bursitis
if other drugs fail; injection into joint Skin diseases, e.g., dermatitis, mycosis fungoides -skin creams particularly convenient Collagen vascular disease, e.g., lupus Hypersensitivity and allergic reactions -if antihistamines and other drugs fail Asthma -systemic preps were last resort -aerosol GC preps are now standard therapy –systemic in acute attacks Renal diseases, e.g., nephrotic syndrome Ulcerative colitis, inflammatory bowel disease -suppositories may be convenient Eye disease -eye drops used Prevention of organ or graft rejection |
|
|
Mineralcorticoids receptor toxicites
|
hypernatremia
hypokalemia alkalosis edema hypertension |
|
|
Glucocorticoids receptor toxicites
|
The more anti-inflammatory, the more of these side effects
since anti-inflammatoryeffect and toxic effect mediated by the same receptor Multiple receptor isoforms, conformations so hope to separate the side effects someday muscle wasting, weakness thin skin, easy bruising osteoporosis growth inhibition diabetes or insulin resistance weight gain fat redistribution activation of peptic ulcer CNS--euphoria, insomnia, psychosis cataracts, glaucoma poor wound healing –due to decreased fibrin, collagen increased risk of infection –due to immune suppression decreased response to stress –due to H-P-A axis suppression |
|
|
Contraindications of mineralcorticoid and glucocorticoids
|
CV disease, diabetes, ulcer, infections,osteoporosis, glaucoma, psychoses
|
|
|
Anti-inflammatory therapy general considerations
|
Short-term high dose "safe"
Long-term low dose "safe" Long-term high dose can be very toxic Generally only palliative, doesn't treat underlying disease May make disease worse May mask symptoms of disease progression May prevent irreversible tissue damage due to inflammation |
|
|
Clinical strategies of anti-inflammatory therapy
|
Usually used as last resort
Lowest dose for shortest time Reduce but maybe not eliminate symptoms Localized administration –systemic absorption can occur –caution switching from systemic to local Alternate day therapy 2/3 dose a.m., 1/3 p.m. –to mimic normal diurnal rhythm Increase dose during stress –infection, surgery, emotional Withdraw slowly, carefully (months) –return of disease or Addison's symptoms Wear warning bracelet Keep adequate supply |
|
|
Therapy of adrenal insufficiency
|
Primary, secondary, acute
Replacement therapy -Hydrocortisone -Add fludrocortisone if needed |
|
|
Congenital adrenal hyperplasia
|
Defects in cortisol production
–21(OH)ase: ↑ androgen, ↓ MC –11(OH)ase: ↑ androgen, ↑ MC –17(OH)ase: ↓ androgen, ↑ MC Hydrocortisone to suppress ACTH and MC or androgen excess –both suppressive and replacement Add fludrocortisone or androgen replacement therapy as needed |
|
|
Additional specific uses of glucocorticoids
|
Stimulate surfactant secretion
-For lung maturation in premature infants -Betamethasone is drug of choice (less bound) Hypercalcemia due to excess vitamin D -Sarcoid, granuloma, overdose, malignancy -Prednisone commonly used Malignancies -Leukemia, lymphoma, myeloma (for cytotoxic effects) -Breast, prostate cancer –to reduce adrenal sex steroids -Prednisone commonly used Myasthenia gravis, multiple sclerosis Minimize cerebral edema after brain surgery or in spinal cord injury -Dexamethasone used |
|
|
Mineralcorticoid agonists
|
Aldosterone
-natural hormone, not useful as drug Deoxycortisone -aldosterone precursor, IM use Fludrocortisone (Florinef®) -oral, potent MC, also GC -major drug used for MC replacement |
|
|
Mineralcorticoid antagonists
|
Spironolactone (Aldactone®)
-mineralocorticoid antagonist -a K+-sparing diuretic -for aldosterone-secreting tumors -also an androgen antagonist – can cause gynecomastia, etc. |
|
|
Adrenalcorticoid inhibitors
|
Metyrapone (Metopirone®)
-inhibits cortisol synthesis -diagnosis of adrenal insufficiency and Cushing's -treatment of adrenal carcinoma or ectopic ACTH production Above drugs used therapeutically primarily in cancer, because of toxicity |
|
|
Angina pectoris
|
Primary symptom of ischemic heart disease caused by transient episodes of ischemia that occur when oxygen supply can't meet oxygen demand
|
|
|
Chronic stable angina
|
pressure/heavy discomfort
occasionally indigestion exertion, emotion, eating, cold weather, lying down stopping effor and sublingual nitro can relieve see transient S-T segment depression |
|
|
Variant angina
|
coronary artery spasm (rare)
|
|
|
Unstable angina
|
pattern of increased frequency and duration; angina at rest
|
|
|
Silent ischemia
|
asymptomatic
|
|
|
Pharmacological therapy for angina
|
Reduce myocardial oxygen demand
Increase myocardial oxygen supply Organic nitrates, calcium channel blockers, beta blockers |
|
|
Treatment of underlying CAD to prevent MI and death
|
Antihyperlipidemics, antihypertensives, antidiabetic agents
Antiplatelet therapy Reduction of other risk factors |
|
|
Determinants of myocardial oxygen demand
|
Heart rate
Contractility Ventricular wall stress (preload/afterload) Oxygen demand can be reduced buy reducing preload/afterload and reducing HR and contracility |
|
|
Determinants of myocardial oxygen supply
|
Most of available O2 is xtracted by myocardium at rest
Increased O2 demand met by increasing coronary blood flow via arteriolar dilation When exertion occurs, no way to increased CBF CBF negligible during systole; duration of diastole bbecomes limiting factor for myocardial perfusion during tachycardia |
|
|
How is increase myocardial oxygen supply
|
Reducing HR and thus increasing time spent in diastole
Dilating coronary arteries (preventing vasospasm) |
|
|
Organic nitrates (nitroglycerin) - mechanism of action
|
Prodrug metabolized to NO by ALDH2
No-induced VSM relaxation produces arterial/venous dilation Venous dilation predominates over arterial so affects the PRELOAD -decreased venous return reduces oxygen demand Effective for relief of symptoms, doesn't prevent MI |
|
|
Organic nitrates (nitroglycerin) - effects on coronary blood flow
|
Vasodilator action on large (epicardial) arteries and promotes redistribution of blood to endocardium
Effects minimal on small resistance vessels (arterioles) Resistance vessels may already be maximally dilated (autoregulation) Direct vasodilating effects on spastic coronary arteries (increases oxygn supply) |
|
|
Organic nitrates (nitroglycerin) - cardiac effects
|
No direct inotropic/chronotropic effects
Reflex tachycardia (if dose is high enough to dilate systemic arteries) |
|
|
Organic nitrates (nitroglycerin) - ALDH2 polymorphism
|
Esterase activity of this enzyme forms glyceryl dinatrate plus nitrate; reductase activity forms NO from nitrate
Low activity polymorphism - ALDH2*2 (Asians) =get less NO formation |
|
|
Organic nitrates (nitroglycerin) - route of administration
|
Oral - low bioavailability due to rapid liver metabolism
Sublingual - therapeutic blood effects in minutes (no first pass metabolism) Transdermal - slow release and longer duration for angina prophylaxis IV: intensive care, unstable angina This drug has a short duration of action (5 minutes) |
|
|
Organic nitrates (nitroglycerin) - Tolerance
|
Sulfhydryl hypothesis: depletion of SH-groups (GSH, cysteine) required to form NO
New explanation: inactivation of ALDH2 by nitroglycerin Cross tolerance occurs to all other nitrates Tolerance can be avoided by using medication intermittently or stopping drug administration overnight |
|
|
Organic nitrates (nitroglycerin) - Adverse effects
|
Headache - arterioles in face and neck and CNS are sensitive to vasodilating properties
Orthostatic hypotenstion Reflex tachycardia which can increase oxygen demand (defeats purpose) -beta blocker or calcium channel blocker can negate this effect Long-term use = endothelial cell dysfunction |
|
|
Organic nitrates (nitroglycerin) - Drug interactions
|
Phosphodiesterase (PDE5) inhibitors (viagra) - severe refractory hypotension can precipitate myocardial infarction
Alcohol (ALDH2 inhibition by acetaaldehyde) |
|
|
Organic nitrates (nitroglycerin) - Other uses
|
CHF and pulmonary hypertension
|
|
|
Calcium channel blockers - two subclasses
|
Dihydropyridines: nifedipine
Non-dihydropyridines: verapamil |

