![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
216 Cards in this Set
- Front
- Back
|
Ischemic Heart Disease:
Stable Angina Pectoris |
Clinical Presentation: pressure; radiation to jaw or arm; reproducible with exertion; relieved with rest; “stable”
Management: RISK REDUCTION: statins & aspirin ANGINA ↓: nitrates, Ca2+ blockers BOTH: beta blocker, ACE inhibitors Prognosis: overall increased mortality |
|
|
Ischemic Heart Disease:
Unstable Angina Pectoria/NSTEMI |
Clinical Presentation: subacute/acute reduction in blood flow with INCOMPLETE occlusion; chest pain (at rest, new onset, crescendo); often >20 min in duration; DX with ST segment ↓ or T wave inversions; CK or troponin ↑
>increase in frequency of pain Management: oxygen; aspirin; heparin; beta blockers; nitrates >conservative tx = 24-48 hrs medical therapy, stress testing, cardiac cath >early invasive tx = early cardiac cath Prognosis: outcomes similar for both tx: pts with MI have 3-5X ↑ in risk of CV death or MI 25% men, 38% women die w/in 1 yr of MI w/in 6 yrs: 18% M, 35% W – another MI 22%M, 46% W – disabled from CHF mortality rates are lower than STEMI; 1.4 million ppl/yr |
|
|
Ischemic Heart Disease:
STEMI (ST Elevated Myocardial Infarction) |
Clinical Presentation: SAME PATHOPHYSIOLOGY AS USA/NSTEMI but COMPLETE arterial occlusion; infarction = cell death; AKA Q wave MI, acute MI/transmural MI
Management: **REPERFUSION** time = muscle thrombolytic agents (streptokinase), coronary angiography (preferred) Meds, balloon angioplasty, stent placement (w/in 90 minutes) aspirin; heparin; beta blockers; ACE inhibitors; oxygen, morphine, nitrates (PAIN) Prognosis: affects 540,000 pts/yr 50% die w/in first HOUR (arrhythmia) 50-60% of ppl who die suddenly of MI have had NO previous SX |
|
|
Ischemic Heart Disease:
Variant Angina |
Clinical Presentation: common in young ischemic pain that occurs at rest coronary artery spasm transient ST elevation on EKG
Management: nitrates, CCB Prognosis: can lead to arrhythmias >acute “active” phase for about 6 months, then becomes more stable; good prognosis |
|
|
Describe the atherosclerotic process
|
Endothelial Injury → oxidized LDL (by free radicals) → inflammatory cells (WBC) → inflammatory mediators (try to absorb oxidized) → smooth muscle cell migration → become inflamed and form fibrous cap
|
|
|
Discuss the role of endothelial dysfunction in the pathogenesis of CAD
|
The loss of normal endothelial defenses leads to inappropriate constriction, luminal thrombus formation, and abnormal interactions between blood cells, (*especially monocytes and platelets)* and the activated vascular endothelium. All of these changes ultimately result in the subintimal collections of fat, smooth muscle cells, fibroblasts, and intercellular matrix that define the atherosclerotic plaque. This process develops at irregular rates in different segments of the epicardial coronary tree and leads eventually to segmental reductions in cross-sectional area, i.e., plaque formation.
|
|
|
Discuss the epidemiology and prevalence of CAD.
|
o 62 million Americans have some form of CVD
o CVD is the leading cause of death in the US o 40% of all deaths are due to CVD (54 % - CAD) o 2600 people die each day from CVD o By 2010, CVD will be the leading cause of death in the world o More people die of CVD than next 5 causes combined o 30/24% of M/F whites, 41/40% of M/F blacks, 29/26% of M/F Hispanics o 80% of death in pts with DM is due to CVD o 40-50% of pts with CAD have HTN (30% of adults have HTN) |
|
|
List the risk factors associated with the development of atherosclerosis.
|
o MAIN
• Dyslipidemia • High LDL (100 is optimal) *** most closely associated with CV disease*** • Low HDL (40 is optimal) • High Triglycerides •Smoking *** biggest modifiable factor*** • HTN • DM o OTHER • FH • Obesity • Metabolic Syndrome • Homocysteine • Lp(a) |
|
|
Dx studies used in the evaluation of stable, unstable and variant angina
(my version) |
*Resting EKG*: normal in pts with stable angina. If normal proceed to exercise stress test.
*Exercise Stress Test*: test where before, during and after exercise treadmill EKG is recorded. Positive if pt has: ST segment depression, chest pain, hypotension, arrhythmias. *Stress Echocardiography*: peformed before & immediately after exercise. Exercise-induced ischemia evidenced by wall motion abnormalities. More sensitive to picking up on ischemia. *Cardiac Catheterization*: most accurate method for specific dx. Lets one see info on hemodynamics, intracardiac pressure measurements, cardiac output, oxygen sat,etc. Indications: 1 after positive stress test, 2 pts with angina that are difficult to recognize & 3 very symptomatic chest pain. **Coronary Angiography:** most accurate method of identifying CAD. Angiography is usually always performed at same time as cardiac cath to get view of the vessels too. |
|
|
Dx studies used in the evaluation of stable, unstable and variant angina
(their version) |
o Exercise Treadmill Test: ECG monitoring, graded protocols, Dx with ST depression, Prognosis = METS; Exercise capacity is one of the strongest prognostic markers
o Nuclear Perfusion Imaging – exercise or pharmacologic stress, then inject radiotracers (technetium-99 or thalium-201) after, take pictures; SHORT AXIS SHOULD LOOK SYMMETRIC; tracer won’t get into myocardium when there’s a blockage o Stress Echocardiogram – exercise or pharmacologic stress, inducible wall motion abnormalities – ischemia; more functional information o Coronary Angiography – inject dye into femoral artery, watch it perfuse the whole heard and coronary vessels; many risks, COMPLETELY DEFINES CORONARY ANATOMY *GOLD STANDARD* |
|
|
Discuss the role of acute plaque rupture in the pathophysiology of the acute coronary syndromes
|
Acute plaque rupture is the cause of acute coronary syndromes; causes a thrombus in the middle of a ruptured plaque which occludes the vessel
|
|
|
Discuss the diagnostic studies used to assess a pt with acute coronary syndrome
|
History!! ECG (ST segment depression, T wave inversions), Elevated cardiac enzymes (Creatine Kinase, Cardiac Troponin)
note: troponin can be falsely elevated in pts with renal failure |
|
|
When reading a 12 lead EKG, identify the most commonly seen myocardial infarction and ischemic patterns.
|
STEMI: ST elevation
NSTEMI: 1 mm horizontal or down sloping ST segment depression 0.06 or 0.08 msec after the J-point Infarction – ST elevation Ischemia – ST depression (with the exception of NSTEMI) |
|
|
Discuss the general indications and contraindications of thrombolytics and angioplasty in the tx of acute MI
|
Tx w/ O2, aspirin (break thrombus), heparin (break thrombus), Beta blockers (decrease HR), nitrates (vasodilate), possible glycoprotein inhibitors IIB/IIA (anti-platelet), possible urgent coronary angiography, angioplasty, stent placement.
>Thrombolytics are to re-establish coronary artery patency, angioplasty to salvage myocardium, and stent placement to improve survival. Choices in tx are made after considering pt. situation. (i.e. previous episodes, distance from hospital w/ cardiac care center, etc). Tx needs to be completed within 90 min of entering hospital. >>Give antiplatelet and antithrombin (heparin) during initial phase of STEMI – to establish and maintain patency |
|
|
Discuss indications for CABG and angioplasty and/or stenting in ischemic heart disease
|
PCI Indications: treatment of choice for majority of pts with SX CAD; must look at anatomy, risks
chronic stable angina >>In acute coronary syndromes: STEMI that present within 12 hours of onset CABG: →Tx of choice in pts with high-risk disease →indicated for: pts with Left Main disease, 3 vessel disease with reduced left ventricular function, 2 vessel disease with proximal LAD stenosis, OR severe ischemia for palliation of symptoms. |
|
|
Discuss the complications of acute myocardial infarction
|
V dysfunction (V remodeling), cardiogenic shock, RV infarction, ARRYTHMIAS, recurrent chest discomfort, pericarditis, thromboembolism (clot originating at site of infarction)
|
|
|
Discuss post myocardial infarction care and rehabilitation
|
>>No angioplasty: submax stress test after 5 days, complete stress test in 3-6 wks, light walking, regular activity OK (minority of pts now)
>>Angioplasty: daily walking OK, driving/sex OK in 1-2 wks, return to work in 2 wks >>Cardic Rehab: improves compliance, ↑exercise tolerance & functional capacity; ↓ cardio mortaliy; ↓emotional stress; ONLY 15% enrolled!!! |
|
|
Medical Tx post MI
|
Medical Therapy: →Aspirin, Beta blockers, ACE inhibitors, Statins, Oxygen, Nitrates, Morphine, Heparin.
|
|
|
Arrhythmias:
Premature Atrial Contractions (PAC) |
>Etiology:normal; stress; hypoxemia; stimulant drugs (caffeine, tobacco, alcohol); valvular CVD; CAD
MstCmn in chain smokers >Pathophysiology: early beat from ectopic atrial pacemaker (NOT a sinus beat from SA node CP: asymptomatic palpitations – compensatory pause, extra time for V to fill, V pumps harder, feel harder beat |
|
|
Arrhythmias:
Supraventricular Tachycardia (SVT) |
>Etiology: stress; hypoxemia; stimulant drugs; valvular CVD; CAD; atrial septal defect; acute MI
>Pathophysiology: ectopic atrial focus: overrides SA node = extra pathway CONTINUOUS; up to 280 bpm >Clinical Presentation:“fast heart beat” palpitations (no pause) light-headedness near syncope/syncope |
|
|
Arrhythmias:
Atrial Flutter SAWTOOTH QUEEN – “FLUTTER” |
>Etiology: atherosclerotic CVD; MI; thyrotoxicosis; PE; mitral valve DZ; cardiac surg; COPD
>Pathophysiology: atrial impulses stuck in “short circuit” – AV node cannot handle all the impulses; rapid atrial rate of 280-340 bpm; 2:1, 3:1 ratio STILL HAVE ATRIAL CONTRACTION >Clinical Presentation: palpitations/SOB/ near syncope/syncope/ CVA/TIA |
|
|
Arrhythmias:
Atrial Fibrillation irregularly irregular cardiac nuisance RATE CONTROL!!!!!!! |
>Etiology: CAD; valvular CVD; thyrotoxicosis; PE; COPD; cardiomyopathy; alcohol; CO poisoning; pheochromocytoma; hypoxia; hypokalemia; sepsis; pneumonia; post-op
>Pathophysiology:TOTALLY chaotic atrial activity; simultaneous discharge of multiple atrial foci - “static” NO ATRIAL CONTRACTION NO P WAVES QRS without REGULAR RHYTHM >Clinical Presentation:palpitations fatigue dizziness/ lightheadedness >asymptomatic (60-70%) CVA/TIA (TIA - confusion, unilateral weakness) CHF/ volume overload |
|
|
Arrhythmias:
Premature Ventricular Contractions (PVC) |
>Etiology: idiopathic; stimulants; acute MI; valvular CVD; cardiomyopathy; cor pulmonale
>Pathophysiology:ectopic beat from ventricular focus; skips AV node; doesn’t use Purkinje system, so QRS is DOWN and WIDE (b/c the impulse is going up towards (-) electrode) NO P WAVE – not starting in atrium) >Clinical Presentation: palpitations |
|
|
Arrhythmias:
Ventricular Tachycardia regular – WIDE and fast |
>Etiology: ischemic CAD; S/P MI; cardiomyopathy; acute myocarditis; muscular dystrophies; electrolyte imbalances; hypoxia; drug toxicity
>Pathophysiology:SERIOUS DYSRRHYTHMIA irritable focus in ventricle indicates underlying CVD 3+ consecutive PVC = VTach >Clinical Presentation: syncope palpitations SCD (sudden cardiac death) CO can go to ZERO |
|
|
Arrhythmias:
Ventricular Fibrillation |
>Etiology:→Ischemic heart dz
→Antiarrhythmic drugs, esp those that cause torsade de points (prolonged Q-T intervals) →A-Fib with very rapid ventricular rate in pts with WPW >Pathophysiology:multiple irritable foci in the ventricles; no P or QRS waves; chaotic rhythm; irregular CP: cannot measure BP, no HS or pulse. Pt unconscious, if untreated death. >Clinical Presentation: NO CARDIAC OUTPUT EMERGENCY TX NEEDED • Immediate defibrillation • drug-shock-drug • CPR/ACLS |
|
|
Arrhythmias:
Idioventricular Rhythms regular – WIDE and slow |
>Etiology: infarction
medicine toxicity >Pathophysiology: ventricular escape rhythm (AKA slower VTach) >Clinical Presentation: as an irregular rhythm TX: atropine; pacing if hypotensive - atropine |
|
|
Arrhythmias:
First Degree Heart Block |
>Etiology:inferior MI; drug effect
>Pathophysiology: fixed, prolonged PR interval (> 0.2 s) >Clinical Presentation: usually asymptomatic |
|
|
Arrhythmias:
Second Degree Heart Block • Type 1 |
>Etiology:vagal stimulation
degen ∆ in upper AV conduction syst ischemic CVD drugs: BB, CCB, digitalis acute inferior MI >Pathophysiology: progressive prolongation or lengthening of PR interval until QRS dropped – P wave does NOT conduct >Clinical Presentation:usually asymptomatic irregular pulse with dropped beats |
|
|
Arrythmias:
Second Degree Heart Block • Type 2 • Fixed PR |
>Etiology: degen ∆ in upper His-Purkinje system
acute anterior wall MI calcific aortic stenosis >Pathophysiology: sudden interruption of AV conduction without prior prolongation; periodic non-conducted P wave; still fixed PR interval; MORE RARE/SERIOUS >Clinical Presentation: irregular pulse with occ. dropped beats sudden LossOfConsciousnes TX: pacing; (+/-) atropine |
|
|
Arryhthmias:
Third Degree Heart Block |
>Etiology: degen ∆ in upper conduction system
acute inferior wall MI calcific aortic stenosis cardiomyopathy trauma/CV surg >Pathophys:COMPLETE dissociation between atria and ventricles • Fixed P-P • Fixed Q-Q >CP: dizziness palpitations Stokes-Adams syncopal attacks CHF – SOB / angina TX: treat underlying cause, pacing |
|
|
Describe the potential complications of AFib
|
>Low CO from loss of “cardiac kick”
>Aggravate CHF (but CHF can promote A-fib as well) >Cardiomyopathy with “RV Rhythm” [dilation of the atrium] >CVA – stasis blood in left atrial appendage can form thrombus. Thrombus can embolize, causing CVA/TIA |
|
|
Discuss the management of acute and chronic AFib
Overview |
“CHF causes AFib, but AFib aggravates CHF”
>Slow HR to give ventricles time to fill – RATE CONROL LOWERS MORTALITY |
|
|
Acute AFib – Dx within 48 hours
|
• Cardioversion (back to NSR)
o Class III drugs – amiodarone, sotalol o Class I drugs – quinidine, procainamide o Flecainide |
|
|
Chronic AFib – longtime Dx
|
• BB
• CCB WITH COUMADIN • Digoxin |
|
|
Goals of TX of AFib
In general |
1. Abolish precipitants
2. Improve quality of life o ↓ symptoms o ↓ complications (anticoagulation and rate control) 3. Lengthen survival 4. Minimize tx-related adverse effects CHADS score – CHF, HTN, Age, DM, Secondary Embolic Event (2 pts) – assess prognosis, develop tx of AFib complications |
|
|
Identify the inheritance pattern, genetic abnormality, predictive testing and preventative treatment of long QT, Romano Ward, Andersen Brugada syndromes and arrhythmogenic RV cardiomyopathy.
|
-all are genetically inherited
Long-QT - delayed repoloarization leads to torsade de pointes Romano Ward - major variant of long QT syndrome Andersen Brugada - same as above Arrhythmogenic RV Cardiomyopathy - R ventricular ischemic cardiomyopathy |
|
|
General etiology of Valvular Disease
|
. Regurges: progressive V enlargement; impairs contraction → progressive V dysfunction; SX LATE IN DZ
|
|
|
Valvular Heart Disease:
Aortic Stenosis • Angina • Syncope • Failure |
>Etiology: degenerative
congenital (bicuspid) rheumatic fever *all cause calcific leaflets* >2% adults >65 yo have calcific aortic stenosis >Pathophys: LV pressure ↑ to maintain gradient and flow across aortic valve LV Hypertrophy develops, leading to D dysfunction and then S dysfunction >CP:SYSTOLC EJECTION MURMUR *time to peak ~ severity* Ejection click A2 decreased, delayed S4 common/ slow shuttering upstroke >Tx:surx – mod to severe (>=1.5 cm2) stenosis with SX [ECHO to show valve size] F/U – asymptomatic >Natural Hx: gradual progression over many years asymptomatic until mod to severe / prognosis poor once SX appear |
|
|
Valvular Heart Disease:
Aortic Regurgitation Just Etiology and Pathophysiology |
>Etiology: Leaftlet problems
o Endocarditis o Rheumatic fever o Bicuspid valve Annulus problems o HTN o Marfan’s o Aortic dissection >Pathophys: regurgitant flow causes volume load on LV, ↑ LV diastolic pressure in response to overload >passive ↑ in pulm venous pressure >LV dilates progressively to hold extra fluid & to maintain forward flow >coronary flow occurs during diastole, need pressure in aorta to keep coronary flow, so flow to coronary arteries may be compromised >high pressure with systole because of large volume, then drops off |
|
|
Valvular Heart Disease:
Aortic Regurgitation CP, TX and Natural Hx |
>CP: *Acute: acute illness /oTachycardia oHypotension oPulm Edema soft, absent A2; short, often soft D murmur
*Chronic: asymptomatic period, wide pulse pressure, laterally displaced PMI, Diastolic decreased murmur correlates with severity >waterhammer, traube’s, bobbing head, quincke’s pulses >uvular bobbing >Tx: Indications for surg: oSX due to severe AR oProgressive LV dilation oDeterioration of LV systolic function in aSX pts oRULE OF 55: operate before LVEF <55% or LV end-S dimension is >5.5 cm >ECHO or CATH to evaluate >Natural Hx: average mortality in aSX pts = 0.5%/year <5%/year develop SX of LV dysfunction >prognosis worse if LV size ↑ on serial echo studies >not a terrible DX, but need to watch for LV dilation |
|
|
Valvular Heart Disease:
Mitral Stenosis |
>Etiology: rheuMatic heart disease o Progressive valve destruction, fibrosis, SX after 10-30 years > rare causes
o Congenital >Pathophys: when valve area < 2cm, pressure gradient develops to maintain flow; LA pressure rises, LA dilates >pulmonary A pressure ↑ secondary to ↑ LA pressure >LV function normal >>CP:loud S1 > opening snap >DIASTOLIC MURMUR (low-rumble @ apex bc lower pressure) >signs of pulm HTN >Tx: goals: relief of SX, prevention of stroke o RATE control o Diuretics o Anticoagulants o Intervention for mod/sev MS with SX >consider surg: mod to severe with SX >Natural Hx: mild – aSX at rest, Sx with ↑ HR and CO >mod/sev - ↑ LA pressure, pulm HTN, pulm congestion, fatigue due to low CO >AFib Risk of LA thrombus/stroke |
|
|
Valvular Heart Disease:
Mitral Regurgitation |
>Etiology: leaflet problem chordate tendinae DZ [connective tissue DZ] /myocardial DZ/ ∆ LV shape / annular size ↑
>Pathophys: supranormal LV function and EF because there’s more blood because the V is constantly receiving blood from the atrium >but low forward SV because some of the blood is getting pumped back into the atria >CP:hyperdynamic PMI, classic MR murmur radiates to axilla >intensity does not ~ severity >Tx: acute: medical stabilization and urgent valve replacement >Surg – REPAIR rather than REPLACE >LVEF can ↓ after replacement >Natural Hx:Long aSX period with LV enlargement and loss of contraction >SX after LV dysfunction – SOB, fatigue, weakness |
|
|
Valvular Heart Disease:
Mitral Valve Prolapse |
>Etiology: aortic stenosis >acute MI that weakens wall close to insertion of papillary muscles >infective endocarditis
>Pathophys:during systole – flapping of mitral valve back into atrium > classic → symmetric and asymmetric >CP: mid systolic click >Tx: presents the same as mitral regurg |
|
|
Valvular Heart Disease:
Tricuspid Stenosis |
>Etiology: almost ALWAYS rheumatic mitral stenosisuncommon
>Pathophys: pressure gradient develops between RA and RV, leads to ↑ RA pressure, systemic venous congestion, low CO >CP: signs of systemic venous congestion, JVD, edema, hepatomegaly, Diastolic murmur, ↑ with inspiration, opening snap; often cardiac findings obscured by MS >Tx: >Natural Hx: mitral stenosis → tricuspid stenosis |
|
|
Valvular Heart Disease:
Tricuspid Regurgitation |
>Etiology: usually secondary to RV dilation and/or pulm HTN
(pulls valve leafs apart) >Pathophys: RA volume overload >CP: JVD, pulsatile liver, holosystolic mumur with ↑ in inspiration >Tx: surg occ required, annuloplasty ring vs. valve replacement >Natural Hx: |
|
|
Valvular Heart Disease:
Pulmonary Stenosis • thrills |
>Etiology: usually congenital
>Pathophys:pressure gradient develops between RV and pulm A > gradient < 50 = mild >CP: mild – aSX mod/sev – exertional fatigue, dyspnea, syncope >harsh systolic ejection murmur along LSB with thrill (pulmonic v in front) soft, absent P2 >Tx: intervention with mod/sev stenosis with SX balloon valvuloplasty preferred – good, permanent results >Natural Hx: |
|
|
Valvular Heart Disease:
Pulmonary Regurgitation |
>Etiology: Pulm HTN/ endocarditis/ congenital
>Pathophys: RV volume overload (well-tolerated) >CP: soft, diastolic decrescendo murmur at LUSB, ↑ with inspiration >decrescendo: loudness correlates with pressure max velocity right after valve closes, decreases after >Tx: Surg RARE >Natural Hx: |
|
|
easy way to remember diastolic murmurs from regurgitation
|
BAD ARMS: Diastolic Murmurs = aortic regurg or mitral stenosis
Decrescendo Diastolic = regurg |
|
|
Dx studies used in the evaluation of valvular heart Disease:
ECHO |
• Identify valve path, mechanism, severity (valve PMS)
• LV size • Systolic function (ejection fraction) • Wall motion • Flow – how fast, which direction |
|
|
Dx studies used in the evaluation of valvular heart Disease:
Catheterization |
• Severity of regurgitation
• LV size, systolic function, pressure (because of dye) • Coronary anatomy • Samples for biopsy • Can put in stents/do angioplasty |
|
|
Discuss the indications for surgical repair of valvular Disease
|
>MITRAL REGURG: SX attributable to severe MR; progressive ↓ in LV function in aSX pts (LVEF <60% or LVESD > 4.5 cm)
>AORTIC REGURG: SX attributable to severe AR; progressive LV dilation or deterioration of LV systolic function in asymptomatic pts; RULE OF 55 >AORTIC/MITRAL/PULMONIC STENOSIS: Mod/Sev with SX; with pulmonic, balloon valvuloplasty (pliable valve with minimal calcification) |
|
|
Cardiac Enzymes:
CK |
total CK ↑ at some time in 90-100% of acute MI; in heart, skeletal, brain
sensitive but not specific |
|
|
Cardiac Enzymes:
CK-MB Isoenzyme |
cardiac muscle
MOST SENSITIVE FOR Acute MI serial measurement q6-8 hrs x3 (many measurements, not just one) ↑ at 4 hrs post MI; peaks at 18 hours; normal in 24-48 hours ↑ without total CK ↑ still = acute MI Also: there are many things can give false positive: pericarditis, drugs, myositis, skeletal trauma etc |
|
|
Cardiac Enzymes:
Troponin I |
smaller molecule / most common
↑ in 4-6 hrs; peaks in 10-24 hrs serial levels at 2,4,6 hrs returns to normal in 4-10 days |
|
|
Cardiac Enzymes:
Troponin T |
larger molecule
↑ in 4-6 hrs; peaks in 10-24 hrs returns to normal in 10 days+ |
|
|
Cardiac Enzymes:
Myoglobin |
↑ in 2-6 hrs; peaks in 6-12 hours
returns to normal in 1 day limitation: doesn’t distinguish cardiac from non-cardiac |
|
|
Discuss the usefulness of the CXR in the screening/detection of CVD
|
PA (posterioanteror) & lateral views to check for:
• overall heart size • fluid in the pericardium (pericardium should be directly adhered to heart) • size/location of aortic arch and pulmonary vessels • calcifications in aorta walls • heart failure • lung/bone DZ associated with heart DZ • normal heart silhouette should be less than 50% of thoracic cavity • “water bottle heart” = pericardial effusion |
|
|
clinical usefulness of the Holter in the evaluation of cardiac arrhythmias
|
• Graphic recording
• Gives 24 hour picture • Indications o Palpitations/Syncope o Efficacy of anti-arrhythmic drugs o Painless ischemia • CAN CATCH SINUS ARRYTHMIAS!!!! (aka Second-degree heart block) |
|
|
clinical usefulness of the Event monitor in the evaluation of cardiac arrhythmias
|
• Size of pager
• Wear 3-6 weeks • Arrhythmias are detected by the monitor and prompt the user to download the electrical activity to the doctor’s office |
|
|
Explain the concept of pretest probability in determining the clinical usefulness of exercise testing in the evaluation of cardiac disease
|
Population with high prevalence will be the best population to screen – will have the least false positives. Don't order a stress test unless you are pretty sure the pt has cardiac disease.... meaning they should probably have risk factors, signs and/or symptoms before deciding to do the test.
|
|
|
clinical usefulness and contraindications to:
Adenosine Thallium Scan obtained pre/post exercise |
• Women < 50 yo with Chest Pain (angina)
• Post MI to detect size, location of infarct • Post PTCA, CABG to assess result • Evaluate false + stress test • Area of ↓ cardiac perfusion more likely to be seen >No Contraindications listed. |
|
|
clinical usefulness and contraindications to :
Exercise Stress Testing Exercise Tolerance Test ETT |
Usefulness: • Dx myocardial ischemia
• Assess efficacy of anti-angina drugs • Identify pts likely to have severe CAD • Serially assess degree of conditioning • Stage valve replacement → False (+) more likely in women → True (-) more likely in women >>Contraindications: • Acute phase of MI • Unstable angina • Decompensated HF, severe HTN • Serious arrhythmias • Sx with aortic valve DZ • AFib with rapid ventricular response • Dilated/Hypertrophic cardiomyopathy • R/L bundle branch block • Hypokalemia • Non-cardiac debilitating DZ |
|
|
clinical usefulness and contraindications to :
Multi-gated Acquisition Scan (MUGA) exercise radionuclide scan |
• Pts about to have chemo
• LV function estimated for several minutes – accurate • Estimates systolic function & EJECTION FRACTION – GOLD STANDARD (tagging RBCs) • Assess LV wall motion & diastolic compliance No contraindications listed. Limitation: gives only info about ejection Fraction |
|
|
clinical usefulness and contraindications to :
Dobutamine Echocardiogram |
• IONOTROPIC AND CHRONOTROPIC
• Pts unable to exercise • Increases cardiac work Contraindications: • Aflutter • AFib |
|
|
clinical usefulness and contraindications to :
Electron Beam CT Scan |
• Detects calcium deposits in artery walls
• Calcium = good indicator of plaque burden • Early indicator of athero No contraindications listed: |
|
|
clinical usefulness and contraindications to :
CTA |
• Calcium scoring/burden
• Cardiac structures • Similar limitations to electron beam CT No contraindications listed: |
|
|
clinical usefulness and contraindications to :
MRI |
• High-resolution
• Hypokinetic: “stunned” vs dead • Valve structure • Aortic dissection • Pericardial DZ • Thrombi/masses • Adult congenital heart DZ • Pulm HTN • >Contraindications: Pacemakers/AICD/stents • Must slow HR, so AFib is contraindicated • Pts with renal DZ (due to contrast) |
|
|
clinical usefulness and contraindications to :
ECHOcardiography |
• Gold standard to r/o thrombus in heart
• Cross sectional: visualize moving heart chambers, tomographic image of heart • Doppler: direction & velocity of blood flow • >>Contraindications: COPD (emphysema) • Thick chest wall |
|
|
clinical usefulness and contraindications to :
Electrocardiography (EKG) |
• Heart’s electrical activity
• Acute cardiac events: acute vs evolving MI • Hypertrophy and chamber enlargement • Conduction abnormalities • HTN, COPD, electrolyte abnormalities, drug effects No contraindications listed. |
|
|
clinical usefulness and contraindications to :
Cardiac Catherization |
• Visualize vessels, valves, chambers
• Measure pressures • >Contraindications: Dye rxn • Concurrent infection • GI bleeding • Severe anemia • Recent stroke • Advanced noncardiac DZ |
|
|
Kinds of Cardiac
Imaging |
• Chest X-Ray
• Echocardiogram • Cardiac catheterization • MRI/CT |
|
|
Kinds of Cardiac
Perfusion Evaluation |
• Cardiac catheterization
• Exercise tolerance test • ETT with imaging adjunct (ex thallium) • Pharmacologic stress testing • PET scan |
|
|
Kinds of Cardiac:
Cardiac Function |
• Echocardiogram
• MUGA |
|
|
clinical usefulness of
Electrophysiology Study |
• Arrhythmias
• Palpitations • Heart DZ; HF; HCM; abnormal ambulatory monitoring • Can induce dysrhythmias to dx |
|
|
clinical usefulness of
Tilt-table Testing |
• To check bp problem
• Lay down, measure BP and HR, then stand up • (+) test is 20 mmHg decrease in SBP, increase in 10 in DBP and HR (20/10/10 rule) • R/O hypovolemia [as in dehydration, OD of BB] |
|
|
clinical usefulness of
B-Type Natiruretic Peptide (BNP) |
• Characterizes volume overload
• Released by ventricle - promotes water loss • Dx of CHF (also HTN) because body is trying to get rid of water |
|
|
clinical usefulness of
C-Reactive Protein (CRP) |
• Inflammation!!!!
|
|
|
clinical usefulness of
Lipoprotein-a |
• Associated with elevated risk of atherosclerotic DZ, but there is not a widely available drug that specifically targets it & testing for it is also not widely available
|
|
|
Describe how the electrical current is generated throughout the heart
|
The resting polarity is maintained by a membrane pump. The inside of the cell is normally negative. In depolarization, sodium and calcium is released, allowing actin and myosin to interact or contract. During repolarization, the membrane returns to resting polarity. The heart is automatic, excitable and conductive. The heart’s automaticity is highest in the SA node.
|
|
|
Discuss how the electrical movement throughout the heart produces predictable wave patterns on the EKG
|
Electricity towards a (+) electrode will be a positive deflection on the EKG. Remember that electrode at feet is (+), so when Purkinjes repolarize, it will be a (-) deflection because the impulse is going towards a (-) electrode.
|
|
|
Describe what the horizontal axis and vertical axis on the EKG paper measures
|
Time (X axis) vs. Voltage (Y axis)
|
|
|
Correlate each of the 12 leads with the region of the heart it is recording
|
Anterior : V1-V4
Lateral: I, aVL, V5-V6 Inferior: II, III, aVF |
|
|
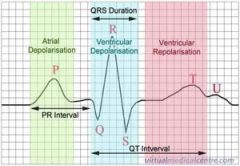
P wave:
|
Atrial Depolarization (less than 0.10 seconds)
|
|
|
QRS complex:
|
Ventricular Depolarization & Atrial Repolarization (less than 0.12 seconds)
|
|
|
T wave:
|
Ventricular Repolarization (1/3 to 2/3 of R wave)
|
|
|
U wave:
|
Repolarization of Purkinje fibers
|
|
|
PR interval:
|
the length of beginning of ventricular depolarization to the beginning of V repolarization (0.3 – 0.44 sec)
|
|
|
ST segment:
|
end of V depolarization to beginning of repolarization (0.08 to 0.12 sec)
|
|
|
ekg
|
|
|
Describe the criteria that define Normal Sinus Rhythm
|
• Pathway: SA node → AV node → Bundle of His → Purkinje Fibers
• 60-100 bpm • 1 P wave for every ORS |
|
|
Discuss the incidence and prevalence of HTN in the US
|

|
|
|
Discuss the mechanisms that control blood pressure
|
Blood Pressure = function of CO and PVR, balance between vasoconstrictors & vasodilators
Influence of local factors Sodium homeostasis RAA system ANS Genetic predisposition Environment |
|
|
Discuss the classification of BP, including normal, prehypertensive and stage 1 & 2 hypertension
|
CLASSIFICATION SBP DBP
Normal <120 < 80 PreHTN 120-139 80-89 Stage 1 HTN 140-159 90-99 Stage 2 HTN ≥ 160 Or ≥ 100 |
|
|
Recognize non-reversible and reversible risk factors for CVD
|
• Cigarette smoking
• Obesity (BMI > 30) • Physical Inactivity → HTN → Dyslipidemia → DM → Microalbuminemia → Age → FH of premature CVD |
|
|
Discuss the difference between essential and secondary HTN
|
>Essential: no medical cause can be found for high blood pressure (90-95% of cases)
>Secondary: HBP is secondary to another condition |
|
|
Define accelerated HTN
|
Significant elevation from previous levels with fundoscopic changes (Grade3, 4 Retinopathy) or renal insufficiency
|
|
|
Define Labile HTN
|
Abrupt and repeated fluctuations in blood pressure levels (ex high BP)
|
|
|
Define Malignant HTN
|
greater than or equal to 200/140 with optic nerve swelling!
|
|
|
What are some of the identifiable causes of HTN?
|
>Kidney Disease
>Endocrine Disease >Coarctation of the Aorta >Obstructive Sleep Apnea >HTN-causing substances |
|
|
Causes of HTN elaborated:
Kidney Disease |
→ Renal Artery Stenosis: abdominal bruits, heavy smoker, < 30 or > 50 yo, scleroderma
→ Renal Paryenchymal DZ: MC due to chronic DM, 2-5% of cases of HTN, ↓ functioning nephrons, sodium retention → Polycystic Kidney DZ: abdominal/flank masses that impinge on arteries |
|
|
Causes of HTN elaborated:
Endocrine Disease |
→ Hyperthyroidism
→ Primary Aldosteronism: adrenal adenoma, unexplained severe hypokalemia, patients 30-50 yo, 1/200 cases of HTN → Cushings: Na+ retaining from cortisol causing hypervolemia → Pheochromocytoma: adrenal medulla tumor, headache, palpitations, pallor, paroxysmal or persistent HTN |
|
|
Causes of HTN elaborated:
Coarctation of the Aorta |
→ Young patient with ↓ femoral pulse, BP, CXR reveals post-stenotic dilation of the aorta; HTN in upper right arm
|
|
|
Causes of HTN elaborated:
Obstructive Sleep Apnea |
→ 10 obstructions/hour
→ Tissues collapse, obstruct airway, BP can’t decrease because pt becomes ischemic |
|
|
Causes of HTN elaborated:
HTN causing substances |
→ Decongestants, cocaine, alcohol, NSAIDS, BC, corticosteroids, ephedra, feverfew, licorice
|
|
|
Discuss the approach to the physical exam in a pt with suspected/known HTN
|
o History
o PE: funduscopic changes, auscultation for bruits, palpation of thyroid, palpate kidneys, peripheral vascular exam, neuro exam (if indicated) o Lab: HCT, potassium (renal function), creatinine (renal function), glucose (DM), lipids (dyslipidemia), calcium (renal), urinalysis, EKG, CXR (cardiac abnormalities) |
|
|
Findings that indicate End organ damage in a pt with suspected/known HTN
|
o S4 gallop
o LV hypertrophy - enlarged, sustained, and laterally displaced apical impulse o Retinal: arteriolar light reflex, arteriovenous crossing defects, hemorrhages, and exudates, swollen optic nerve disc o Neurologic: CVA/TIA, hypertensive encephalopathy, mild cognitive impairment o Renal: atherosclerosis of large arteries of kidney, deposition of lipoproteinacious material in afferent artery walls, malignant arteriolar nephrosclerosis o Peripheral artery DZ: claudication |
|
|
Discuss the recommendations for follow-up based on initial blood pressure measurement
|
>Monthly until BP goal is reached (DM, chronic kidney disease goal: 130/80)
Then at 3-6 month intervals >Monitor serum K and Cr 1-2 times/ years for microalbuminemia |
|
|
Discuss the appropriate Dx studies obtained in the initial evaluation of a pt with suspected/known HTN
|
Clinic: Accurate BP measurement: pt seated with feet on floor with arm at heart level for 5 minutes. Cuff bladder should encircle 80% of arm.
>home measurements: pt keeps record at home, (white coat htN) >Ambulatory BP monitoring: helpful in drug resistant pts, monitor for 24 hours, pt keeps logs of activity (considered best prognostic vaule) |
|
|
Discuss the lifestyle modifications for management of HTN
|
Maintain a normal body weight
Consume a diet rich in fruits, veggies, and low-fat dairy Reduce sodium Engage in regular aerobic physical activity such as brisk walking (30 min day x 3-4 days/week) Moderate consumption of alcohol |
|
|
What are the main classes of hypertensive drugs?
|
a. Diuretics
b. B-Blockers c. Calcium Channel Blockers (CCB) d. ACE inhibitors e. Angiotensin Receptor Blocker (ARB) |
|
|
HTN Drugs:
Side Effects of Diuretics? |
i. N/V
ii. Hypokelemia iii. Hyponatremia iv. Hyperuricemia (pts with gout) v. Hypercalcemia vi. Orthostatic hypotension/light headedness vii. Acute hypovolemia viii. Ototoxicity (hearing affected, esp. when given with aminoglycoside abx) |
|
|
HTN Drugs:
Side effects of B-Blockers |
i. Drowsiness
ii. Bronchospasm iii. Bradycardia iv. Impaired exercise tolerance v. Insomnia vi. Worsening of claudication vii. Erectile dysfunction |
|
|
HTN Drugs:
Side effects of: Calcium Channel Blockers (CCB) |
ii. Anemia
iii. Excessive vasodilation (hypotension) iv. Aggravation of myocardial ischemia |
|
|
HTN Drugs:
Side effects of: ACE inhibitors |
i. Cough
ii. Hypotension iii. Angioedema iv. Hyperkalemia v. Worsening of renal function |
|
|
HTN Drugs:
Side effects of: Angiotensin Receptor Blocker (ARB) |
i. Hypotension
ii. Worsening of renal function iii. Hyperkalemia |
|
|
Discuss the BP goal in the following:
>→ Uncomplicated HTN > DM: >Chronic Kidney Failure |
→Uncomplicated HTN: 140/90
→DM: 130/80 →Chronic Kidney Failure: 130/80 |
|
|
What end organ systems does HTN affect?
|
>retinal vessels, the heart, the cerebral vessels, peripheral vessels and the kidney
|
|
|
Discuss the effects of HTN on
retinal vessels |
• (1) ↑ light reflex
• (2) AV nicking • (3) hemorrhages or cotton wool spots • (4) swollen optic nerve • Retinal detachment |
|
|
Discuss the effects of HTN on
the heart |
• CAD
• CHF • LV Hypertrophy (risk of arrhythmias and sudden death) |
|
|
Discuss the effects of HTN on
peripheral vessels |
• Peripheral Artery DZ
• Claudication |
|
|
Discuss the effects of HTN on
the kidneys |
• Atherosclerosis
• Deposition of lipoproteins in artery walls • Malignant arteriolar nephrosclerosis (AA) |
|
|
Discuss the effects of HTN on
the cerebral vessels |
• CVA
• TIA • HTN Encephalopathy • Mild cognitive impairment |
|
|
JNC 7's recommendations for treatment of HTN
part 2 |
5-MOST persons with HTN will require 2 drug tx’s to get to a BP of <140/90, and if diabetic <130/70.
6- if BP >20/10 mm Hg above goal then starting tx with 2 drugs should be considered, one of which should be a thiazide diuretic. 7- The most effective tx to control HTN is one in which the pt is motivated, compliant and has a positive experience with a clinician that they trust. Empathy builds trust/motivates. 8- authors of JNC recognize MD’s judgement as paramount |
|
|
Explain the TX of HTN based on risk factors as described by the JNC VII
part 1 |
1- in persons older than 50 years: systolic BP >140 is more a risk than Diastolic BP in terms of CVD risk factor.
2- the risk of CVD doubles with each incremental increase of 20/10 mmHg above a baseline of 115/75 in pts over 40-70 y/o. 3- Defines the term “prehypertension” to be systolic Bp of 120-139 and diastolic BP to be 80-89, intervene with lifestyle modifications to prevent CVD. 4- thiazide type diuretics should be used for most patients w/ uncomplicated HTN or in conjugation with other classes of BP meds. Other classes should be considered for pts with “compelling indications” |
|
|
Discuss the most appropriate HTN drug choices for
Diabetes |
→ DM: all 6 (cautious with BB due to hyperglycemia unawareness)
best are ACEI's and ARB's. -thiazide diuretics increase blood glucose |
|
|
Discuss the most appropriate HTN drug choices for
CAD |
→ CAD: all (-) ARB and Aldosterone Antagonists
|
|
|
Discuss the most appropriate HTN drug choices for
Isolated Systolic Hypertension |
same as general care for HTN
(thiazides?) |
|
|
Discuss the most appropriate HTN drug choices for
CHF |
→ CHF: all (-) CCB
|
|
|
Discuss the most appropriate HTN drug choices for
Dyslipidemia |
→ Dyslipidemia: all 6, lifestyle
|
|
|
Discuss the most appropriate HTN drug choices for
African Americans |
→ AA not responsive to monotherapy: BB, ACEI, ARB
|
|
|
Discuss the most appropriate HTN drug choices for
Pregnancy |
→ Pregnancy: m-DOPA, BB, vasodilators
|
|
|
Discuss the most appropriate HTN drug choices for
Elderly |
→ Elderly: “go low, go slow” → same as general care for HTN
|
|
|
Discuss the most appropriate HTN drug choices for
CKD |
→ Chronic Kidney DZ: ACEI, ARB
|
|
|
Discuss the most appropriate HTN drug choices for:
Cerebrovascular disease |
→ Cerebrovascular DZ: ACEI + thiazides
|
|
|
Discuss the role of and proper techniques for self-monitoring including utilization of 24 hour monitoring
|
Self monitoring is a better predictor of future cardiovascular events than clinic follow-up. The patient must be instructed in the proper technique: adequate equipment (arm, not wrist or finger), seated with arm supported at heart level. Have the patient demonstrate proper technique using their own machine in your office and correlate their machine’s readings with yours to ensure accurate measurements.
If necessary, you can do 24 hr blood pressure recording. This can be helpful to see if there are particular times of the day when the patient’s blood pressure is higher than other times of the day (ie when at work or other times of stress). |
|
|
Discuss the causes of resistant HTN
|
>Resistant hypertension is defined as the failure to reduce blood pressure to the appropriate level after taking a three drug regimen (include thiazide diuretic).
Causes: → Improper measurements → Volume overload/pseudotolerance (excess salt intake, volume retention from renal DZ, inadequate diuretic therapy) → Drug-Induced (noncompliance, wrong dose, wrong combos, NSAIDs, drug use, HTN-causing Rx, steroids) → Associated conditions (obesity, excessive alcohol) → Identifiable causes |
|
|
Discuss the correct method for obtaining accurate blood pressure
|
Try to make sure the patient has not smoked or drank any caffeine 30 minutes prior to testing.
Make sure the room is quiet and comfortably warm Ask the patient to sit quietly for 5 minutes in a chair with feet on the floor and the arm supported at heart level. Make sure the arm is free of clothing, free from arteriovenous fistulas (for dialysis), scarring from brachial artery cutdowns, or signs of lymphedema Make sure the blood pressure cuff fits properly (not too large or small) Palpate the brachial artery to confirm the pulse is viable Position the arm so the brachial artery (in the anticubital crease) is at the heart level. If seated, rest the arm on a table above the patient’s waist; if standing, try to support the arm at midchest level. |
|
|
Define primary and secondary cardiomyopathy
|
PRIMARY – cannot be attributed to a specific cause
SECONDARY – due to specific cause; associated with DZ involving other organs as well as the heart |
|
|
Discuss the causes of secondary CM
|
General categories: ischemic, valvular, hypertensive, inflammatory, metabolic, inherited, toxic reactions, peripartum
Specific: lupus, pheochromocytomas |
|
|
inheritance pattern, genetic and clinical abnormalities associated with :
Dilated CM |
>Inheritance Pattern:Autosomal dominant/recessive, x-linked, mitochondrial
>Genetic Abnormalities: Specific genes coding for myosin, actin and dystophin (problem encoding contractile proteins) >Clinical Abnormalities: Abnormal energy production and contractile force generation. Associated phenotypes: skeletal muscle abnormalities, neurologic, and auditory. |
|
|
inheritance pattern, genetic and clinical abnormalities associated with:
Hypertrophic CM |
>Inheritance Pattern:Autosomal dominant (55%)
>Genetic Abnormalities: Mutation in one of four genes encoding proteins of cardiac sarcomere: Beta-MHC, cardiac troponin T, Myosin binding protein C, Alpha tropomyosin >Clinical Abnormalities:Mutation → Disarray in myofibers →myocyte hypertrophy→ clinical symptoms (Angina, Dyspnea, syncope and sudden cardiac death) Symptoms may not be present even if you have 1st degree relative with familial Hypertrophic CM. Echocardiogram every 12-24 months b/w ages 12 and 20 unless diagnosis established/ excluded by genetic testing. |
|
|
Dilated Cardiomyopathy
Etiology |
• Ischemic
• Valvular • Hypertensive • Familial • Idiopathic (Majority— 3X more prevalent in males and African Americans) • Inflammatory • Infectious includes: o Viral—picornovirus, Cox B, CMV, HIV, (Acute Viral Myocarditis is caused by Echovirus and Cox B) o Ricketsial—Lyme disease o Parasitic—Chaga’s Disease, Toxoplasmosis • Non infectious includes: • Collagen vascular disease (SLE, RA), peripartum • Toxic (alcohol, anthracyclins/ adrimycin, cocaine) • Metabolic (endocrine—thyroid, precromocytoma, DM, acromegaly), • Nutritional (thiamine, selenium, carnitine) • Neuromuscular (Duchene’s Muscular Dystrophy-x-linked) |
|
|
Hypertrophic Cardiomyopathy
Etiology |
• Often familial—most with autosomal dominant transmission (55%)
• Mutations in one of four genes coding proteins of cardiac sarcomere account for majority of familial cases. o Beta-MHC o Cardiac Troponin T o Myosin binding protein C o Alpha-Tropomyosin • Remainder are spontaneous mutation |
|
|
Restrictive Cardiomyopathy
Etiology |
• Infiltration of myocardium by abnormal substance fibrosis or scarring of endocardium
• Restriction is caused by replacement of normal myocardial contractile elements by infiltrative interstitial deposits. • Amyloidosis o Primary—deposition of immunoglobulin light chains, multiple myeloma o Secondary—deposition of protein other than immunoglobulin (senile, familial, chronic inflammatory process) • Sarcoidoisis—restriction, conduction system disease (AV Block), ventricular arrhythmias and sudden cardiac death • Endomyocardial Fibrosis—endemic in parts Africa, India, South and Central America and Asia. Thickening of basal inferior wall. No known cause. |
|
|
Dilated Cardiomyopathy
Pathophys/ Clinical Presenatation |
>Pathophys:Neurohumoral — activates the adrenergic nervous system and the renin-angiotensin-aldosterone axis. Stimulates the release of vasopressin, natriuretic peptides, and endothelin
>CP: Dilation and impaired contraction of left ventricle. • Reduced systolic function with or without heart failure. • Characterized by myocyte damage. • Multiple etiologies with similar resultant pathophysiology. • Symptoms of right and left CHF develop gradually. • Symptoms do not include chest pain |
|
|
Hypertrophic Cardiomyopathy
Pathophys/ Clinical Presenatation |
Pathophys:Mutation →Disarray in myofibers → hypertrophy of myocytes → SX
If septum thickens, often affects mitral valve leading to dynamic LV outflow obstruction. >>CP: LV hypertrophy NOT due to pressure overload >Vigorous systolic function but impaired diastolic function (therefore pump is OK, but it is stiff during relaxing and can’t receive blood)—Elevated diastolic pressures Symptoms include: Syncope, Dyspnea, Angina, arrhythmia, LVOT obstruction, Sudden Cardiac Death (SCD) |
|
|
Restrictive Cardiomyopathy
Pathophys/ Clinical Presenatation |
Pathophys: Infilatration of myocardium by abnormal substance/fibrosis/scarring of endocardium
CP: Characterized by impaired ventricular filling due to an abnormally stiff ventricle. Normal systolic function early in DZ but eventual Diastolic Dysfunction. Right HF> Left HF Dyspnea Orthopnea/PND Peripheral Edema Ascites/Hepatomegaly Fatigue/decrease exercise tolerance >>Clinically mimics constrictive pericarditis |
|
|
Dilated Cardiomyopathy
Evaluation Ejection Fraction Treatment |
Evaluation:• Echocardiogram
• Endomyocardial Biopsy in monitoring of cardiac allograft rejection and anthracycline cardiotoxicity and possibly for detection and monitoring of myocarditis, diagnosis of secondary cardiomyopathies and differentiation between restrictive and constrictive heart disease. Ejection Fraction: REDUCED EF Treatment: normalize ejection fraction! • ACE Inhibitors (blocks conversion of Angiotensin I to Angiotensin II) • Angiotesin Receptor Blocker (blocks binding of Angiotensin II to AT-1 Receptors) • Spironolactone (Prevents effects of aldosterone) |
|
|
Hypertrophic Cardiomyopathy
Treatment |
>Treatment: Symptomatic Benefit
• Beta Blockers (decrease MVO2, Decrease gradient, arrhythmias) • Calcium channel Blockers • Anti-arrhythmics (amiodorone or disopyramide for afib, AICD for sudden death if there is a Hx of syncope) • Antibiotics prophylaxis for endocarditis No therapy has been shown to improve mortality (often have to transplant / surgery) • Myomyectomy (the gold standard)—removal of small portion of septum • Dual Camber pacing—little long term benefit • ETOH Septal Ablation—causes a control MI of septum |
|
|
Hypertrophic Cardiomyopathy
Evaluation Ejection Fraction |
>Evaluation: Physical Exam
• listen for swooshing (Holosystolic apical blowing murmur of mitral regurgitation) when squatting vs standing. • Bisferiens Pulse (spike and dome) • S4 Gallop • Crescendo/ Decrescendo systolic ejection murmur. squatting ↓intensity of murmur [↑ preload ↑ afterload] standing ↑ intensity of murmur >Ejection Fraction: HIGH EF |
|
|
Restrictive Cardiomyopathy
Evaluation Ejection Fraction Treatment |
Evaluation: Cardiac Catheterization showing prominent Y descent (rapid atrial emptying then abrupt cessation of blood flow due to non-compliant myocardium) and the “dip and plateau”/square root (rapid ventricular filling)
-CXR to check for fibrotic tissue >Ejection Fraction:NORMAL (until late stages) >Treatment: Treat underlying cause • r/o constriction which is treatable • for amyloid use melphalan, prednisone, colchicines • for endomycardial fibrosis use steroids, cytotoxic drungs, MVR (mitral valve replacement) • for hemochromatosis use chelation and phlebotomy • for sarcodoisis use steroid Diuretics (for congestive symptoms but decreasing LV/RV filling→decreased CO Digoxin Anti-arrhythmics for afib (amiodorone) Pacemaker for conduction system disease Anticoagulation for thrombus |
|
|
the limitations of genetic testing for dilated CM
|
Mutations HAVE been found in 20 + genes, but these mutations count for a minority of cases
(-) test doesn’t give much information Can test relatives of individuals identified with an IDC-causing mutation |
|
|
the limitations of genetic testing for hypertrophic CM
|
MOST genetic tests test for HCM; available for a subset of 24 known causative genes →phenotype correlations are unclear
Indicated in: • suspected/confirmed HCM • relatives of those with suspected/confirmed HCM Little prognostic value, OK for DX and family screening (-) result should be interpreted with caution, as the 8 MC genes explain less than 61% of HCM MOST ARE SPONTANEOUS MUTATIONS |
|
|
Describe the surveillance and screening available to PCPs for pts with CM
|
CXR -- ↑ cardiac silhouette
vascular redistribution interstitial edema, pleural effusions EKG --CAN BE NORMAL tachycardia, A/V enlargement LBBB, RBBB, Q waves Blood Tests -- ANA, RF, Fe2+ TFT’s, ferritin ECHO -- LV size wall thickness, function, valve DZ, pressures Cardiac Cath --hemodynamics LVEF, angiography Endomyocardial Bx-- |
|
|
Describe the risk factors associated with peripheral vascular disease.
|
Nonmodifiable: age, gender (males), race (AA), family history
Modifiable: smoking, HTN, hi cholesterol, DM, sedentary lifestyle/obesity, stress Peripheral vascular disease = aorto-iliac arteries & below |
|
|
Chronic lower limb ischemia
|
>Etiology: 1.Atherosclerosis
2.Connective tissue disease 3.Infection 4.Trauma >Pathogensis: claudication → rest pain → tissue loss >CP:-Pulses: diminished or absent, +/- abdominal bruits -skin: shiny, thin, hairless -nails: thickened and discolored -delayed/absent cap refill -dependent rubor -ABI <1 >Mgmt: -control risk factors: smoking cessation, diabetes control, ASA, lipid control --aerobic exercise --cilostazol – improves Sx, but not circulation |
|
|
Acute arterial occlusions
|
>Etiology: Like MI…Occlusion from embolus or thrombus; signs/symptoms rapid and severe; need rapid intervention to prevent muscle/nerve death
>Pathogensis: Embolic sources: aortic aneurysm; atrial fibrillation; L ventricular thrombus (following MI) >CP: 6 P's! Pain, Pallor, Pulselessness, Paresthesia, Poikilothermia (assumes temp of the room), Paralysis (late) >Mgmt: Anticoagulation with Heparin IV hydration; thrombectomy/embolectomy; revascularization procedure |
|
|
Mesenteric ischemia
|
>Etiology: Chronic: atherosclerosis risk factors
Acute: Atherosclerosis + thrombosis, embolism (A-fib), low flo state. >Pathogensis: thrombus that embolizes into superior/inferior mesenteric or celiac; must be 2 of 3 >CP: Abdominal pain after meals (intestinal angina); food fear with weight loss; may have epigastric bruit due to stenosis >Mgmt: Diagnostics: US, CTA, angio MGMT: revascularize→ endartectomy (surgical removal of plaque from an artery), angioplasty/ stent, bypass Manage medical risk factors |
|
|
Renal artery stenosis
|
>Etiology: Atherosclerosis/ fibromuscular dysplasia (congenital connective tissue DZ)
>Pathogensis: Natural Hx: -appx 40% will progress -70% of these will have worsening kidney function -accounts for appx 24% of CKD on dialysis >CP:Suspect when: -acute onset of severe HTN in patients under 35 or over 55 -acute worsening of pt w/ previously well controlled BP -out of control BP despite multiple drug regimen -Hx of significant atherosclerosis >Mgmt: Dx: US, CTA/angiography, MRA, renal vein assay (Bx), captopril stim test (in pts with bad renal function) MGMT: risk factor management; angioplasty/stent indicated for discrete lesion; endartectomy or bypass possible; may need nephrectomy if kidney nonfunctional Stenting preferred over PTA in atherosclerotic disease |
|
|
Intracranial aneurysms
|
>Etiology: Most aneurysms are located On the anterior part of the circle of Willis, esp. on the anterior or posterior communicating arteries
>Pathogensis: Focal dilation of artery becomes >2.5 cm diam of adjacent normal artery. >CP: May cause a focal neurologic deficit by compressing adjacent structures, headache, neck stiffness. →most are asymptomatic until they rupture causing a subarachnoid hemorrhage >Mgmt:Angiography, CT scan to dx. → Ca++ channel blockers reduce or reverse vasospasm, and nimodipine reduces ischemic deficits from arterial spasm without any SE. --SA hemorrhage has its own protocol for tx. |
|
|
Abdominal aortic aneurysms
|
>Etiology: -atherosclerosis (90%) -inherited connective tissue (marfans) -acquired conntv tisue/inflammatory -infection (fungal)
>Pathogensis: Focal dilation of artery becomes >2.5 cm diam of adjacent normal artery. Incr size assoc w/ incr. rupture. -all major arteries can become affected. >CP:Nonruptured: most asymptomatic, pulsatile mass on abd. Exam, incidental finding on KUB & CT -LE embolic phenom -family hx Ruptured: acute back pain, pulsatile tender abd. Mass, shock, mortality >80% Dx: Ultrasound (best screening/follow) -CTA or CT (CTA for surgical planning) >Mgmt:-traditional surgical resection w/ graft (AAA >5 cm) -Endovascular aneurysm repair, -complications: renal failure, ischemia or bowel, spinal cord, or LE. EVAR- NOT recommended (proximal neck angulation) |
|
|
Popliteal artery aneurysms
|
>Etiology: Often bilateral, associated with AAA’s. See also the etiologies of AAA’s.
>Pathogensis: >Acute occlusion can result in severe distal ischemia. Distal embolization can also result in severe distal ischemia. >CP: Symptoms are due to thrombosis, embolization, pressure from an expanding aneurysm, or (rarely) rupture. >There may be an arterial mass in the popliteal fossa or the groin. can cause symptoms (e.g., signs of venous obstruction, weakness, sensory defects) when they compress the popliteal vein or tibial nerve >Mgmt:Get a vascular surgeon, because immediate operation is required when severe distal ischemia has occurred secondary either to acute thrombosis or to distal embolization |
|
|
Aortic dissection
|
>Etiology: NOT due to atherosclerosis; Marfan syndrome; HTN; pregnancy; age
>Pathogensis: blood gets in between layers of the aorta (in between intima & adventitia) false lumen occludes true lumen >CP:Severe intrascapular pain; hypertensive; deficits in blocked organ systems >Mgmt:Type A: emergent ascending aorta replacement - Type B: BP control, surgery if end organ ischemia Long term risk of aneurysm |
|
|
diagnostic studies used in the evaluation of peripheral vascular disease:
Doppler ultrasound |
- 1st line diagnostic!
o Safe, non-invasive method to measure flow velocities o Can see velocity, disturbances → NARROWING |
|
|
diagnostic studies used in the evaluation of peripheral vascular disease:
• CTA |
o Spiral CT scan
o IV contrast only o Images compiled into a 3D picture o Quality dependent upon technician, machine and radiologist o Less risk, cost, time than angiography |
|
|
diagnostic studies used in the evaluation of peripheral vascular disease:
• MRA |
o Variable sensitivity
o Open MR not available for arterial protocol o Metal interference o ? safer for CKD (chronic kidney disease) – non-iodine dye o Gold standard for aortic dissection |
|
|
diagnostic studies used in the evaluation of peripheral vascular disease:
• Angiography |
still gold standard
o Invasive study with injection of contrast media • Hyperosmolar and nephrotoxic • For patients with contrast allergy- Benadryl, prednisone • For patients with renal insufficiency – hydration, bicarbonate • Day surgery- puncture of femoral artery |
|
|
Discuss the etiology, clinical presentation, diagnostic evaluation, management, and complications associated with **varicose veins**.
|
• Etiology: oRisk factors- female gender, family history, prolonged standing/ weight lifting, pregnancy, overweight/ obesity
oPost-phlebitic Syndrome- venous clot that does not resolve OR scarring of venous valves following thrombophlebitis •CP: oTelangiectasias → active ulceration oAching pain, stinging or heaviness oEdema Dx Studies: oVenous ultrasound- define anatomy, determine presence of chronic or acute thrombus oMRI/MRV oVenogram- Gold Standard- puncture of vein o+/- ABI- not going to have an abnormal ABI because of venous problem but good to know for surgical or tx precautions -Mgmt: oMedical Therapy- support hose, weight loss, leg exercises, elevation, Unna boot prn, skin grafting oIf superficial, Surgery for refractory symptoms and cosmesis- ultrasound or venogram FIRST, then sclerotherapy vs. stab avulsions vs. vein stripping vs. endoscopic laser/ radiofrequency ablation. |
|
|
Describe the pathogenesis, clinical presentation, and treatment of chronic venous insufficiency and post-phlebitic syndrome
|
• Pathogenesis: Chronic venous insufficiency can present as Post-phlebitic syndrome, which is a venous valvular dysfunction due to an unresolved clot or scarring following thrombophlebitis.
• Clinical presentation: telangiectasias, active ulceration; aching pain, stinging or heaviness; Edema • Diagnostic studies: o Venous ultrasound- to define anatomy; determine presence of chronic acute thrombus o MRI/MRV o Venogram- similar to an angiogram; involves puncturing the vein o +/- ABI- need to check this before any intervention because of healing/blood flow issues • Management: support hose, weight loss, leg exercises; elevation; Unna boot prn; skin grafting. |
|
|
Define heart failure
|
Complex clinical syndrome with abnormality of LV function and neurohormonal regulation accompanied by effort intolerance, fluid retention and reduced longevity.
|
|
|
Define preload & factors that influence it.
|
Pressure exerted in the LV before the ventricle contracts.
[can’t measure clinically, so we use pulmonary capillary wedge pressure] Volume depletion: ↓ preload Volume expansion: ↑ preload |
|
|
Define afterload & factors that influence it
|
The load against which the LV contracts
Can measure with systemic vascular resistance Sepsis, oral vasodilators/antihypertensives ↓ afterload HTN ↑ afterload |
|
|
Define cardiac contractility & factors that influence it.
|
Measure of intrinsic cardiac function – how well the heart contracts for any given HR, preload and afterload
NO TOOLS TO MEASURE, so measure of systolic function used instead Measure of systolic pressure = EJECTION FRACTION Myocardial damage (MI, long HTN) ↓ contractility Ionotropic Agents (Dbx, Milrinone) ↑ contractility |
|
|
Compare/contrast the definition, etiology, and management of systolic and diastolic dysfunction:
>SYSTOLIC DYSFUNCTION |
>Definition: decreased ability of ventricle to eject blood
>EF: decreased >Etiology: CAD, HTN, idiopathic, endocrine, valvular, toxins, arrhythmia, SLE, genetic, viral >Mgmt: ACEI + BB + Diuretic |
|
|
Compare/contrast the definition, etiology, and management of systolic and diastolic dysfunction
>DIASTOLIC DYSFUNCTION |
>Definition: decreased ability of ventricle to accept blood
>EF: normal >Etiology: filling problem >Mgmt: avoid tachycardia, treat ischemia, control BP |
|
|
Discuss the natural history of chronic heart failure
|
LV Systolic Dysfunction → ∆ size, geometry and function of heart after injury → ventricular wall thinning → reshaping of LV (increase volume in DCM, increased mass in hypertrophy, Cowboys instead of Mavericks) → accumulation of collagen in cardiac interstitium → progressive systolic and diastolic dysfunction
|
|
|
RIGHT Heart Failure
|
>Etiology: RV failure
>Pathophysiology: due to incr pressure in systemic veins >CP :edema, anorexia, weight gain/loss and SX below most important PE finding: JVP cachexia, rales, effusions, RV/LV lifts, S3, MR/TR (valves pulled apart due to dilation) , ascites, hepatomegaly, cool edematous limbs, low sodium >Dx Studies: CXR: increased cardiac silhouette, pulmonary edema B-type Natriuretic Peptide: secreted from LV in response to myocyte stretch; can DX HF |
|
|
LEFT Heart Failure
|
>Etiology: LV failure valvular abnormality (mitral stenosis)
>Pathophysiology: increased pressure in pulmonary veins leads to pulmonary congestion/edema >CP : breathlessness, DOE, orthopnea, PND, fatigue, mental status, TIA/CVA, syncope >Dx Studies: CXR: increased cardiac silhouette, pulmonary edema >B-type Natriuretic Peptide: secreted from LV in response to myocyte stretch; can DX HF |
|
|
Describe typical radiographic findings of a pt with HF
|
Increased heart size and PVR/pulmonary edema
|
|
|
Identify pharmacologic agents for treating HF and their mechanism of action
|
>ACE Inhibitor: inhibit angiotension-converting enzyme which blocks the downstream effects of angiotensin II (potent vasoconstrictor)
>Beta-Blocker: inhibits the beta-1 receptor which decreases contractility, HR; improves LVEF, prevents DZ regression, improves survival >Aldosterone Antagonist: reduces mortality, blocks aldosterone which causes sodium retention >>Digoxin: for residual SX, but doesn’t improve survival Isosorbide >Dinitrate/Hydralazine: improves survival in AA with class 3-4 SX |
|
|
Describe the general management principles, including non-pharm management, for pts with chronic HF
|
Reduce mortality → Control Volume → Treat Residual SX
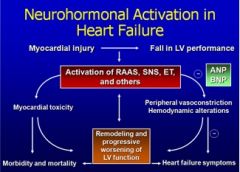
Pt Education: salt restriction, flexible diuretic regimen, exercise program >>ANP/BNP – trying to reduce sodium in the body; trying to vasodilate; can measure in patients Once a pt beings activation of the RAAS, SNS, leads to myocardial toxicity, then remodeling, worsening of LV function, then increased activation – spiral downward |
|
|
ANP/BNP – trying to reduce sodium in the body; trying to vasodilate; can measure in patients
Once a pt beings activation of the RAAS, SNS, leads to myocardial toxicity, then remodeling, worsening of LV function, then increased activation – spiral downward |
|
|
Identify precipitating causes which may lead to the decompensation of chronic heart failure
|
Noncompliance (diet, medication)
-HTN -Arrhythmias -Iatrogenic (wrong med started, right med stopped) -Infection -MI/Active Ischemia -Endocrine/anemia -Pulmonary Edema |
|
|
Identify the indicators for hospitalization for pts with chronic heart failure
|
Deterioration of SX (decompensated); not responsive to oral meds
-Concern for ischemia/MI in ischemic CM -Altered lab results -Syncope -Thromboembolic event -Arrhythmia: VT/VF, new atrial fibrillation |
|
|
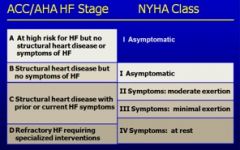
Compare the NYHA and ACC/AHA classification of HF
|
|
|
|
Acute Pericarditis
|
>Etiology: outpt MC: viral or idiopathic // MC viral: coxsackie A and B //bacterial (less common, severe)
TB /Lupus >>inpt: TUMOR -trauma, uremia, MI, meds, other infections, rheumatoid. >CP:•pleuritic chest pain that radiates to back, scapula •LESS pain when leaning forward, inspiration •SOB, tachycardia •As, Vs, Vd component – friction rubbb •PR depression, diffuse ST elevation •Normal CXR •ECHO may show effusion >Dx Studies: EKG, ECHO,EKG • ST elevation (epicardial inflammation) •ST concave upward (peaky) •PR segment depression •T-wave inversion ALL LEADS OF THE EKG! >Mgmt:ASA/ NSAIDS Steroids – ONLY for refracty SX |
|
|
Chronic Constrictive Pericarditis
|
>Etiology: “thickened, calcified pericardium leading to restriction of ventricular filling” //acute pericarditis//TB/previous sgx,
collagen vascular DZ, idiopathic >CP: •Dyspnea •Venous cngest •Ascites, edema >Dx Studies: •CXR – calcification in pericardial sac •CT/MRI – thickening of pericardium •ECHO – wall motion abnormalities •R Heart Cath >Mgmt:-pericardial resection -low Na diet -diuretics -treat underlying cause |
|
|
Cardiac Tamponade
BAD effusion causes tamponade |
>Etiology: pericardial effusion that causes intrapericardial pressure >>increase in atrial pressure (thinner wall) → decrease in venous return → decrease in CO
>CP: •Pulsus paradoxus •Beck’s Triad: JVD, muffled heart sounds, hypotension (because of decrease in CO) •Oftentimes tachycardiac >Dx Studies: •EKG oElectrical alternans (∆ in QRS shape from beat to beat) •ECHO oEffusion oA,V collapse •CXR o“water bottle configuration >Mgmt: DRAINAGE (catheter) surgical window rarely required |
|
|
Understand the cause and clinical significance of pulsus paradoxus
|
An exaggerated drop in SBP with inspiration (> 10 mmHg)
It results from an accentuated decrease of the blood pressure, which leads to the radial pulse not being palpable |
|
|
Discuss the differential diagnosis of pericardial effusion
|
MC: Infection, TB
Inflammation: collagen vascular disease Hypothyroidism Uremia Malignancy Blood: myocardial injury/rupture CHF, volume overload |
|
|
Endocarditis
inflammation/infection of endothelium of heart |
>Etiology:in children: •Congenital
in adults: •MVP •Bicuspid aortic valve •Prosthetic valves •IV drug abuse >Pathophys:1 start with abnormal vascular endothelium then >platelet, fibrin deposition then> thrombus formation then> adherence, colonization by bacteria then> vegetation → healing with fibrosis, embolization, abscess formation, leaflet destruction >Risk Factors: •MVP – no MR murmur •MVP – murmur •VSD – V septal defect •congenital aortic stenosis •prosthetic valve >CP:•fever •new or changing murmur •Osler nodes •Janeway lesions •Splinter hemorrhages •Roth spots •Emboli >Mgmt:Abx >uncommon: surgery PROSTHETIC VALVE IE: TEE |
|
|
Discuss the diagnosis of endocarditis using the Duke criteria
Major Factors |
MAJOR
• (+) blood cultures • Persistently positive cultures • Evidence of endocardial involvement o Vegetation on ECHO o Abscess o Prosthetic valve dehiscence o New valve regurgitation |
|
|
Discuss the diagnosis of endocarditis using the Duke criteria
|
MINOR
• Predisposing heart condition • Fever > 38 degrees • Vascular phenomenon • Immunologic phenomenon: GNF, Oslers, Roth spots, Janeway • Microbiologic evidence not meeting major • ECHO finding not meeting major criteria |
|
|
conditions and procedures for which antibiotic prophylaxis is indicated for the prevention of bacterial endocarditis
|
PATIENTS:
• Prosthetic heart valves • Prior Hx of IE • Cyanotic congenital heart DZ • Repaired congenital heart defects with prosthetic material • Cardiac valvulopathy in transplanted heart PROCEDURES: • Dental: perf of mucosa, gingival movement • Respiratory: invasive procedures (goes directly to heart) • Skin/soft tissue/mucosa: surgery on infected tissue |
|
|
bacterial organisms responsible for Endocarditis
|
VIRIDANS STREP:
• MC cause • Course is slow or sub-acute; we commonly refer to this as SBE, or sub-acute endocarditis. STAPH/B-HEMOLYTIC STREP: • 2nd MC cause • Much more acute, FULMINANT • MC with IVDU • MC with prosthetic valve surgery |
|
|
Most common valve affected in IV Drug users?
|
mitral valve
|
|
|
course of bacterial endocarditis with viridans strep & HACEK organisms?
|
For viridans strep species & HACEK organisms, the course is slow or sub-acute; we commonly refer to this as SBE, or sub-acute endocarditis. The disease caused by staph & B-hemolytic strep is much more acute.
(Hacek = Hemophilus Actinobacillus, Cardiobacterium, Eikenella, Kingella) |
|
|
Discuss the risk factors associated with dyslipidemias.
|
Lipids have a central role in atherogenesis.
Which then leads to CHD (especially high LDLs, which make up most of the total cholesterol level). |
|
|
Familial Hypercholesterolemia typical clinical presentation, lipid levels and prognosis.
|
-FamilialHypercholesterolemia: high total cholesterol levels with LDL elevations
>CP> a defect in LDL receptors so they don’t bring LDLs to the liver, the liver then produces more LDL, tendinous xanthomas- firm subcutaneous nodules, tendons and ligaments-Achilles/hands/knees/elbows, can make a clinical diagnosis with this finding >>-homozygotes (one in a million) have 8 times normal LDL levels and present with atherosclerotic disease in childhood, may need liver transplants -heterozygotes (one in 500) LDLs of 200-400 (2 times normal), may develop CHD in 30s or 40s |
|
|
Familial Hyperchylomicronemia:
|
Familial Hyperchylomicronemia: abnormality in lipoprotein lipase, the enzyme that enables peripheral tissue to take up triglycerides from chylomicrons and VLDLs, hypertriglyceridemia with current pancreatitis and hepatosplenomegaly
|
|
|
List the secondary causes of dyslipidemias.
|
chronic kidney disease
-nephrotic syndrome -*DM/Insulin resistance* -*Hypothyroidism* *Hyperthroidism* -Hepatobiliary disease -Alcoholism -smoking, Diet -Obstructive liver disease, cirrhosis -malignancy -Cushing Disease Drugs: **thiazide diuretics, B-blockers** estrogens, anabolic steroids, glucocorticoids, antiretroviral tx, cyclosporine |
|
|
Recognize the clinical presentations of lipoprotein disorders in the :
vascular, GI, ophthalmic, derm systems |
1)vascular system- atherogenesis → Coronary Heart Disease
2) GI system- pancreatitis, atherogenesis lead to pain with eating→acute pain in abdomen 3) ophthalmic system – corneal arcus (FH), xanthelasmas, lipemia retinalis- cream-colored blood vessels in fundus (above 2,000 mg/dL of triglycerides) 4) dermatologic system – tendinous xanthomas (Familial Hypercholesterolemia) |
|
|
laboratory evaluation of dyslipidemias:
Total Cholesterol |
a part of complete lipid panel, <200 desirable, >240 high
|
|
|
laboratory evaluation of dyslipidemias:
LDL |
must be fasting, calculated not measured, total cholesterol–
HDL–(TG/5), if TG>400 calculated LDL is not accurate so measure directly i)> 20% 10-year risk on Framingham (CHD/equivalent) LDL Goals for: <100 mg/dL (high risk) (<70 very high risk) =10-20% 10 yr risk on Framingham <130 (moderate risk) <100 (moderately high risk) <10% 10-year risk <160 mg/dL (lower risk) |
|
|
laboratory evaluation of dyslipidemias:
HDL |
- a part of complete lipid panel, <40 low, >60 high (protective)
|
|
|
laboratory evaluation of dyslipidemias:
Triglycerides |
must be fasting
(also, LDL is calculated and because of this having an incredibly high TG level [>400] then you can't calculate LDL) |
|
|
how and when labs are done on lipids
|
Complete lipid profile after overnight fast- total cholesterol, HDL, TG;
Screening of all adults aged 20 years or older for high blood cholesterol |
|
|
6. Discuss the importance of fractionation of LDL and HDL and measurement of LP(a), homocysteine, and C-reactive protein in the evaluation and management of dyslipidemias.
|
LP(a), homocysteine, CRP- predict future CHD events
Those with total cholesterol > 200 mg/dL should be reevaluated with a fasting LDL and HDL cholesterol measure. |
|
|
Discuss the life-style modifications which improve blood lipid disorders
|
-Exercise (TG decreased 5-15%, HDL increased 3-5%)
-Weight loss- BMI < 25 kg/m^2 TG dec 7%, LDL dec 6%, total cholesterol dec 10%, inc HDL 8% -Smoking cessation (HDL increased by 5%) -Diet- avoid trans fats saturated fat <7% total calories Dietary cholesterol <200 mg/day Total fat 25-35% total calories Carbohydrates 50-60% total calories Dietary fibers 20-30 g/day lowers LDLs 8-10% |
|
|
Discuss the alternative supplements widely used to improve blood lipid levels
|
-Niacin- reduces VLDL production w/ secondary reduction in LDL and increase in HDL, reduce TG by half, and lower lipoprotein (a) and increase homocysteine levels
-Fish Oil- omega 3 fatty acids- decrease TG -Red Rice Yeast -Plant sterol esters- cholesterol lowering |
|
|
NCEP guidelines for management of lipid disorders
Step 1 |
1. *LDL-C is first goal of tx*
– CHD/equivalent: <100 mg/dL or <70mg/dl (highest risk) – 10-20% 10-yr risk: <130 mg/dL (<100mg/dl) – <10% 10-yr risk: <160 mg/dL Steps: CHD/equivalent? Yes LDL goal is <100 (<70), No (go to number of risk factors-smoker, HTN, HDL <40, FH of premature CHD, female 55 and over, male 45 and over) Risk Factors 0-1 LDL <160 Risk Factors 2 or more calculate Framingham Score - <10% LDL goal <130 - 10-20% LDL <130 (<100) - >20% LDL <100 |
|
|
NCEP guidelines for management of lipid disorders
|
2.**Non HDL is second goal of therapy** (if TG >200)
NHDL=TC-HDL NHDL goal= LDL goal+30 mg/dL Initiate therapy if NHDL above goal- low carb diet, weight loss, improved glycemia, exercise, decreased EtOH, intensify LDL lowering, add fibrate, add niacin, fish oil |
|
|
NCEP guidelines for management of lipid disorders
|
3. Consider treating HDL-C after above goals are met
If HDL below 40, then weight loss, smoking cessation, exercise, low carbs, EtOH, add fibrate and niacin |
|
|
Discuss the prognosis for the long term effects of dyslipidemias
|
Atherogenesis > CHD, high triglycerides risk for pancreatitis/metabolic syndrome, stroke
|
|
|
Discuss the indications for referral/consultation for patients with dyslipidemias
|
When you should suspect somebody has Familial Hypercholesterolemia/Refer: an LDL >190 mg/dL in an adult, >160 in a child, family hx of premature coronary artery disease, tendinous xanthomas or other physical findings.
Extremely high Triglycerides. Extremely low HDL (also striking family hx of early atherosclerosis) |
|
|
NCEP ATP III Guidelines for lipid management
when to initiate drug therapy? |
basically the higher Framingham risk/general CHD risk you are, the earlier it is appropriate to initiate drug therapy.
Statin + Cholesterol absorption inhibitor (Zetia) is best. Bile acid resins decrease LDLs by 15-30%, Diet, plant stanols/sterols, and weight loss reduces LDLs as well |

