![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
218 Cards in this Set
- Front
- Back
|
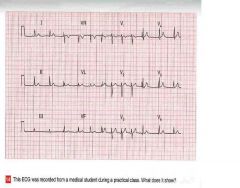
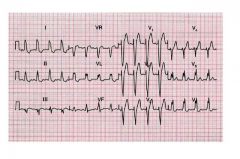
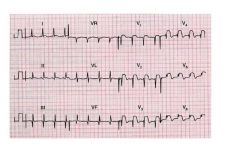
Clinical Interpretation:
there is a variation of the R to R interval, with the heart rate speeding up and slowing down (compare heart rate in V1, V2 and V3 with the heart rate in V4, V5, and V6) • Summary: Normal EKG with sinus arrhythmia (variation of heart rate related to respiration) |
ekg
|
|
|
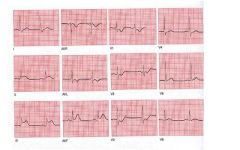
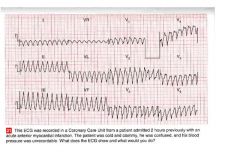
• The EKG shows:
– Narrow‐complex tachycardia, with rate of approximately 200 bpm – No P waves are visible – Normal axis – Normal QRS complexes, ST segment and T waves • Clinical interpretation: – Supraventricular tachycardia, and, since no P waves are visible, this is a junctional tachycardia • What to do – Junctional tachycardia is the most common form of paroxysmal tachycardia in young people – Try intravenous injection of adenosine – If unsuccessful: verapamil (5‐10 mg) in bolus IV – If unsuccessful: cardioversion |
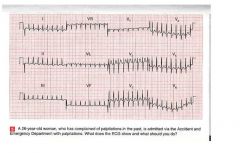
what does this ekg show you AND what should you?
|
|
|
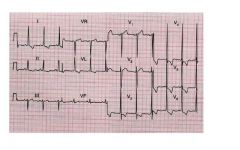
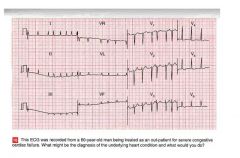
• Clinical Interpretation: tall R
waves in V1 and reduced R wave progression in the precordial leads. Right axis deviation with mean QRS vector of approximately +120 degrees • Summary: Right axis deviation with suspicion of right ventricular hypertrophy. Consider execution of echocardiogram |
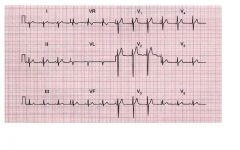
type ekg?
|
|
|
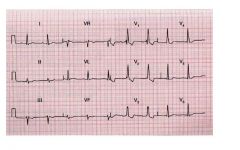
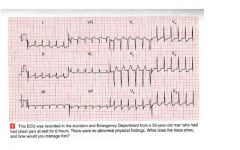
• Clinical Interpretation:
Vertical heart (mean QRS vector of approximately +90 degrees) • Summary: Normal EKG (vertical heart is a normal variant) |
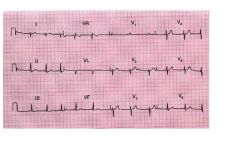
type ekg?
|
|
|
• Clinical
Interpretation: R‐R’ aspect in V5 and V6 • Summary: Left bundle branch block |
type ekg?
|
|
|
• Clinical
Interpretation: ST segment elevation in LII, LIII and AVF (inferior leads) • Summary: Acute inferior myocardial infarction |
type ekg?
|
|
|
• Clinical Interpretation:
Positivity of Socolow and Lewis indexes with ST segment depression in V5 and V6 • Summary: Left ventricular hypertrophy, with ventricular strain |
ekg?
|
|
|
• Clinical Interpretation:
PR interval >0.2 sec; RR’ aspect in V1 and V2; right axis deviation • Summary: 1st degree AV block; Right bundle branch block; right axis deviation |
ekg?
|
|
|
• Clinical Interpretation:
Deep Q waves in LII, LIII and AVF; ST segment elevation in V1 through V6 • Summary: Old inferior myocardial infarction; acute anterior myocardial infarction |
ekg?
|
|
|
• The EKG shows:
– Broad‐complex tachycardia, rate about 250 per min – Regular QRS complexes – QRS duration 200ms • Clinical Interpretation: – In the context of acute myocardial infarction a broad‐complex tachycardia should be considered to be ventricular • What to do – In case of severe hemodynamic impairment, immediate cardioversion • Summary – Ventricular tachycardia |
ekg?
|
|
|
• The EKG shows:
– Atrial fibrillation – Ventricular rate: 75‐200 bpm (need to calculate mean ventricular rate by means of a long LII o V1 strip) – Normal axis – Normal QRS complexes – Downsloping ST segment depression, in V5 and V6 • Clinical Interpretation: – The heart rate is no adequately controlled. ST depression, in absence of hypertrophy and ischemia, suggest that the patient is taking digossin • What to do – Check cardiac function by echocardiogram – Check serum levels of digossin and, if necessary, increase the dose. – Consider cardioversion to reestablish sinus rhythm, after adequate anticoagulant therapy |
ekg?
|
|
|
• The EKG shows:
– Sinus tachycardia – Horizontal heart – Normal QRS complexes – ST segment depression: horizontal in V3‐V4, ownsloping in LI, AVL, V5‐V6 • Clinical interpretation – Anterior and lateral ischemia, without evidence of infarction. Given the history, the diagnosis is unstable angina • What to do – Give aspirin, and intravenous heparin and nitrates – Also intravenous beta‐ blockade can help! |
ekg? what do you do?
|
|
|
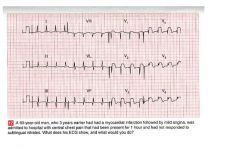
• The EKG shows:
– Sinus rhythm – Normal heart rate – Normal axis – ST elevation in inferiro leads – Tall R wave in V1‐V2, with ST depression and T wave inversion in V1‐V3 • Clinical interpretation – Acute inferior and posterior myocardial infarction • What to do – Immediate revascularization |

ekg?
|
|
|
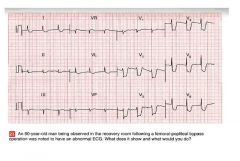
• The EKG shows:
– Sinus rhythm – Normal axis – Q waves in inferior leads – Marked ST elevation in Leads V1‐V6 • Clinical interpretation – Old inferior infarction, and acute anterior MI • What to do – Revascularize asap |
ekg?
|
|
|
• The EKG shows:
– Sinus Rhythm – Normal axis – Normal QRS complexes – Marked (about 8 mm) horizontal ST segment depression in leads V2‐V4, and downsloping ST segment depression in the lateral leads • Clinical interpretation – Severe antero‐lateral ischemia (unstable angina) • What to do – Aspirin, heparin, nitrates iv |
ekg? and what do you do?
|
|
|
1. major change: elevated pressure in LA and pul vasc.
2. complicated with RV hypertrophy/failure due to pul htn |
What hemodynamic change occurs here?
|
|
|
A fib, tx with cardiac glycosides (digoxin)dec av conduction and depress sa node
|
what ekg change is associated with this? How is it treated
|
|
|
1. dec vent compliance, interstial collagen
2. possible dec contractility chronically, myosin ATPase activity depressed 3. perfusion deficit, reduced coronary reserves (volume>capillary) 4. less efficient energy utilization sarcomere mass > mitochondrial mass |

What are the adverse consequenses of this?
|
|
|
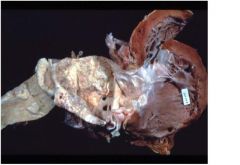
MS with dilated LA
1. with dilated LA, mural thrombi and emboli can develop 2. acute pulmonary congestion results in alveolar hemosiderin deposits 3. pulmonary venous htn may result in thickening of pulmonary vessels causing perminant inc in pul vasc resistance |
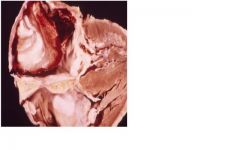
What secondary adaptive pathology and their sequelae can occur here?
|
|
|
1. diffuse fiberous thinkening leading to rigidity of both leaflets
2. commissural fusion **DX of rheumatic etiology 3. chordal fusion, thickening, shortening**DX of rheumatic etiology 4. calcification |
What are the primary pathologies here?
|
|
|
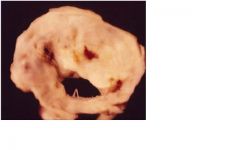
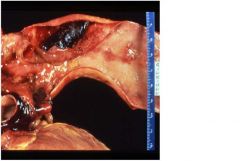
1. congenital bicuspid
2. • increased systolic pressure (pressure overload) • LV hypertrophy; concentric type, normal chamber volume • LV compliance decreases (becomes harder to fill) • preload must increase to maintain constant output • LA hypertrophy |

1. What is the pathology here?
2. Name one hemodynamic change that can occur here? |
|
|
1. as 2nd to chronic rheumatic heart disease
2. • increased systolic pressure (pressure overload) • LV hypertrophy; concentric type, normal chamber volume • LV compliance decreases (becomes harder to fill) • preload must increase to maintain constant output • LA hypertrophy |
1. What is the cause of this?
2. Name one hemodynamic change that occurs. |
|
|
pt > 70 yo, this is senile calcific aortic stenosis
clinical presentation: – Dyspnea – Syncope – Angina – Sudden death |
What patient population would this be seen in? and how would they present
|
|
|
• Pulsus parvus et tardus
(decreased volume & slow upstroke pulse) • Powerful, sustained apical systolic impulse S4 • Early ejection sound (click) that diminishes with age in congenital AS • Diamond shaped systolic murmur, peaking later in systole and lasting longer with severe AS. • Single S2 |
What cardiac findings occur with this lesion?
|
|
|
1. loud S1
2. opening snap during diastole 3. mid diastolic murmur 4. presystolic accentuation (PSA) due to atrial contraction which is absent with A Fib |
32 yo female pt presents with sob and hoarse voice starting 6 mo with past history of fever when younger. What cardiac findings will be seen with this pt?
|
|
|
1. surgery when pt sypmtomatic with transaortic gradient > 50 mm hg
2. balloon valvuloplasty pallitive for elderly pt |
What are 2 txmt options for this pt?
|
|
|
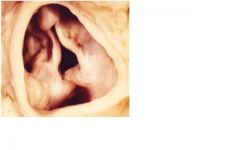
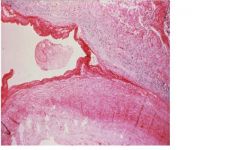
This is a floppy mitral valve.
floppy valve: myxoid egeneration causing thickened but floppy leaflets rheumatic: diffuse fibrous thickening of valve leaflets at the margins of closure causing leaflet retraction and poor closing. Chordal fusion/thickening is rare. |
What cardiac lesions can cause this?
|
|
|
This is mitral regurg due to acute bacterial endocarditis
• over time, eccentric LV hypertrophy • the regurgitant volume is pumped into a low pressure chamber (the LA) and therefore, cardiac work is not greatly increased • the chronic condition is well tolerated |

What hemodynamic alteration and adaptation occurs here?
|
|
|
Thisis an acute bacterial endocarditis which causes MR.
In Chronic MR, PE findings include: 1. hyperdynamic lateral displaced apical impulse 2. parasternal lift 3. S1 often obscured by holosystolic blowing apical murmur that may radiate to axilla 4. loud S3 sound |
What physical exam features are seen with a chronic case?
|
|
|
this is a mitral valve prolapse which presents as midsystolic click and later systolic murmur
|
how does this present on physical exam?
|
|
|
rheumatic, endocarditis,
calcific/degenerative, bicuspid |

What are valvular causes of this?
|
|
|
dilated root in Marfan's syndrome
root pathologies include: ->idiopathic, syphilis, ankylosing spondylitis (inflammation), dissection, trauma also -abnormal collagen (marfan's synderome) -calcifiation (collagen vascular disease) |

What root pathologies cause this?
|
|
|
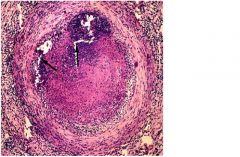
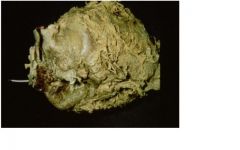
Polyarteritis Nodosa (PAN)
-transmural acute necrotizing inflamation of med sized vessles -can produce irregular aneurysmal dilation, nodularity and vascular obstruction and possible infact in kidney, heart, bowels and skin but NOT LUNG AND AORTA |
What clinical finding can be associated with this?
|
|
|
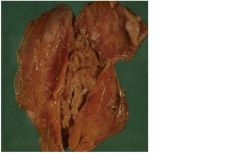
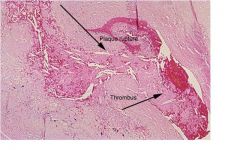
Polyarteritis Nodosa, bc transmural acute necrotizing inflamation of med sized vessels possibly causing vascular obstuction inc chance of infact from thrombi
|
what condition would lead to this?
|
|
|
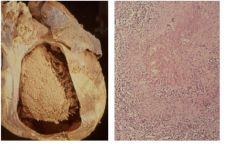
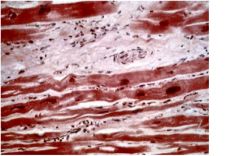
This is from a pt with PAN who suffered MI 24 - 48 hrs prior, notice pmn infiltrate, edema and cell structure loss
|
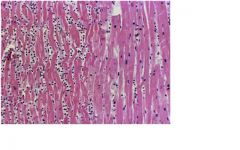
What is the cause of change in tissue on the left?
|
|
|
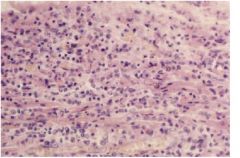
This is Wegener's Granulomatosis
1. necrotizing granulomas of the upper and/or lower respiratior tract 2. necrotizing or granulmatous vasculitis of small arteriies and veins, usually lungs 3. necrotizing glomerulonephritis, C-ANCA presents 95% of time txmt: respond to steroid |
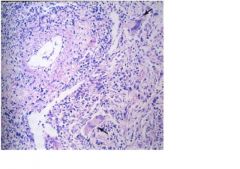
What triad is associated with this condition?
txmt? |
|
|
corticosteriod
|
Pt presents with pain when chewing, has blindness in eye on same side, muscle and joint pt. Labs show inc in erthrocyte sedimentation rate. How should this pt be tx?
|
|
|
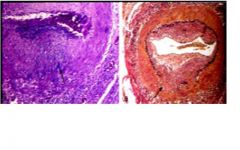
This is temporal arteritis or giant cell arteritis
->segmental acute and chronic, granulatomatous vascularitis involving often large areties of head particularly carotid artery branches |
what condition has this histological finding and what vessels are involved?
|
|
|
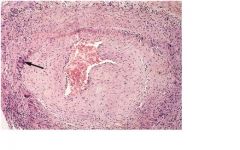
Takayasu's arteritis also known as pulseless disease
-granulatomatous large vessel vasculitis involving aortic arch vessels |
Pt comes in with complaint of cold and numb fingers. Physical finding show absence of upper extremity pulse. What vascular changes are associated with this pt condition?
|
|
|
child presents to ED with intenstly crying with high fever, parents have tried to give pt tylenol and advil to dec temp with no result. You notice that the pt also has red swollen palms and soles of his feet. The child's eyes are also irritated and red eyes. What immediate concern do you have for this pt?
|
MI due to thrombis. This child is suffering from Kawaski disease which is necrotizing mid sized vessel vasculitis involving coronary arteries
|
|
|
Throboangitis obliterans, also known as Buerger's disease, notice neutrophils and micro-abcesses
-foot claudication -Raynaud's synderome: paroxysmal digital color change, ulceration and gangreen |
What clinical findings present with this disease?
|
|
|
Throboangitis obliterans, also known as Buerger's disease
remitting, relapsing inflammation disorder that often leads to thrombosis of med sized vessels -Tibial and radial arteries |

How does this patient develop the above findings?
|
|
|
Abdominal atherosclerotic aneuysm
->pt presents with left flank pain, hypotension, and pulsating mass in abdomin ->transmural wall damage is expected |
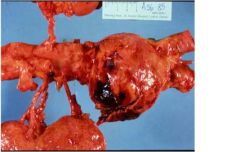
What 3 clinical findings would this pt present with?
What degree of wall damage is expected? |
|
|
Microscopic polyangiitis
-small vessel vasuclitis -see palpable pupura, glomerulonephritis p-ANCA antibodies 80% of time |
This pt presents with what key clinical and lab findings?
|
|
|
vasa vasorum of aorta resulting in dilatation/aneurysm of arota and aortic ring
-ischemic destruction of elsastic tissue and muscel of media which results in scaring "tree-bark" appearance ->sacular aneurysm ->develop aortic valve regurg, see wide pulse pressure, difference btwn systolic and diastolic pressure, manifested by hyperdynamic circulation - pulstatig uvula, bounding pulses |
What is the target of this disease which presents as a "tree bark" appreance?
|
|
|
Aortic dissection
1. tear of intima due to htn or underlying structural weakness in media, usually occur 10 cm of aortic valve -Cystic medial degeneration (CMD), associated with ct disorders, elastic tissue is fragmented 2. pt presents with loss of pulse on left and severe retrosternal chest pain NOT radiating down arm, x-ray shows double barrel aorta |
1. What pathologic change has occured here?
2. How does a pt in this condition present? |
|
|
aortic dissection seen in young pt with Marfan syndrome, fibrillin syn mutation, or Ehler-Danlos syndrome, collagen defect mutation
|
what disorders are associated with this histological presentation?
|
|
|
Aortic dissection
1. tear of intima due to htn or underlying structural weakness in media, usually occur 10 cm of aortic valve -Cystic medial degeneration (CMD), associated with ct disorders, elastic tissue is fragmented |
What pathogenisis is associated with this?
|
|
|
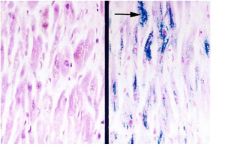
These ar contraction band necrosis, hyper eosinophilc transvers bands in myocytes reflect hypercontraction of myofibrils following exposure to oxygen and circulating plasma Ca, the effects of reperfussion
|
What is the cause of this pathology?
|
|
|
What is this?
-no necrosis -transient period of severe ischemia (ex: MI) -function returns over time (days) -flow/fxn mismatch |
myocardial stunning
|
|
|
WHat is this?
-no necrosis -chronic high grade stenosis (long standing) -fxn returns immediately upon reflow -flow/fxn matched |
myocardial hypernation, see with severe CAD due to atherlosclerosis, cell fxn return if relieve high grade stenosis
|
|
|
What is this?
-intermittent occlusion -good collateral fxn -low hr -low bp |
best case for MI
|
|
|
What is this?
-abrupts total occlustion -poor collateral fxn -high hr -high bp |
worst case for MI
|
|
|
timing of histologic damage in MI?
very early; wavy fiber change, edema, hemorrhage; beginning neutrophilic infiltrate |
4 to 12 hr after mi
|
|
|
timing of histologic damage in MI?
-heavey pmn inflitration |
24 to 72hr after mi
|
|
|
timing of histologic damage in MI?
-macrophage appear |
4 to 7 days after MI
|
|
|
timing of histologic damage in MI?
well-developed necrotic changes; prominent fibrovascular reaction in margins (early collagen deposition; pigment-laden macrophages) |
10 days after MI
|
|
|
pump failure
-low co despite high filling pressure -hypotension -hypoperfusion: periphearl vasoconstriction, oliguria, altered mental status |
What complication occured due to MI?
|
|
|
rv infaction
-occurs in 20% of inferior wall MI -sign of RV failure: inc JVP, hypotension |
MI complication?
|
|
|
Papillary muscle rupture
-inferior wall infarct can result in post medial papillary wall rupture -also can be due to anteriolateral muscle rupture due to anterolateral wall infaction |

MI complication?
|
|
|
ventricular aneurysm
-due to weakening of vent wall following large transmural infarct -closely related to post-infarct vent expansion or remodeling |
complicatin of MI?
|
|
|
What is this?
acute dilation and thinning of infact zone not explained by additional necrosis -associated with higher mortality and higher incidence of heart failure, aneurysms, and rupture -augments wall stress, impairs contractile fxn |
infarct expansion, complication of MI
|
|
|
What is this?
new necrosis in same anatomical zone of orgnial MI |
Infarct extension, complication of MI
|
|
|
rupture of free wall of infarcted ventricle occuring up to 5% of pt dying in hospital due to acute MI
-more common in htn pt -occur btween 3 to 5 days after MI -more common to occure in anterior or lateral lv Clinical sign: cardiac tamponade and sudden death -can involve septum and papillary muscles |

MI complication?
|
|
|
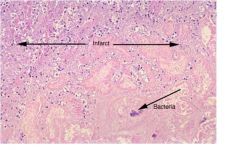
pericarditis
-very common with trasmural MI -result in pericardial frictional rub (leathery rub) -can be acute -> 2 to 4 days after MI -can be late, autoimmune response -> 2 to 10 wk after MI = Dressler's Synderome or post-MI synderome |

MI complication?
|
|
|
-fever
-chest pain -pericardial freictiona rub (leathery rub) -elevated ESR -elevated WBC -chest pain relieved when sit up or forward |

how does this pt present acutely?
|
|
|
Pt presents with past hx of cancer comes in bc fatigue, dyspnea, dizziness, sycope. Upon measuring bp, pt bp drops 12 mm Hg during inspiration. What is the cardiac conditon seen in this pt?
|
cardiac tamponade with paradoxical pulse
|
|
|
Pt with past exposure to radiation come in to see you because if fatigue and increase swelling in pt abdomin and legs. You notice that the pt distention of neck veins with inspiration and a loud early S3 sound. What cardiac disease does this pt present with?
|
chronic constrictive pericarditis seen in post malignancy with radiation
Kussmal' signs = distension of neck veins with inspiration Pericardial knock = loud early S3 sounds |
|
|
What organism is associated with acute endocarditis?
|
staph aureus - infection with high virulence organisms
-may infect normal valves -destruction due to hyaluronidase production |
|
|
What organism is associated with subacute endocarditis?
|
infection with low virulence organisms ex: strep viridans
-damage occurs to damaged or abnormal valves |
|
|
What organism common with prosthetic valve infective endocarditis?
|
staph epidermidis
|
|
|
what do these 3 relate to?
1. rupture of leaflet, chordae tendinae, or papillary muscles 2. ring abcess, extension of infection to surrounding tissue 3. embolization or septic infact |
complications of acute endocarditis
|
|
|
What type of prostetic cardiac valve could develop complications of mechcanical deterioation
|
bioprostetic cardiac valve from animals
|
|
|
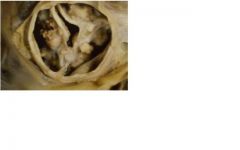
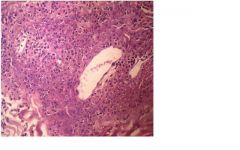
leaflet perforation, due to acute endocarditis
|

complication for infective endocarditis
|
|
|
abcess
-ring abcess-> extension of infection to surrounding tissue |

complication of infective endocarditis
|
|
|
pericarditis
|

complication of bacterial endocarditis?
|
|
|
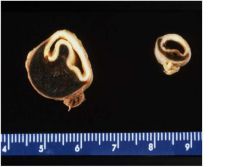
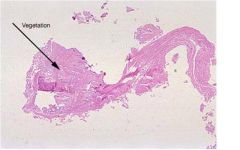
1. Non-bacterial thromboitc endocarditis (NBTE)
2. malignancies, paticularly adenocarcinomas 3. deposition of small masses of fibrin, platelets and other blood components on leaflets but no micro-organisms and no valvular damaged needed/required |

1. disease state?
2. common etiology? 3. definition? |
|
|
gross exam:
-groups of small nodules along the line of valve closure (recall RF) -aortic valve more commonly involved Microscopically: -nodules composed of fibrin and platelet -underlying valve normal (no fibrosis or necrosis) |

What is the pathology of this disease?
|
|
|
What prosthetic cardic valve can have the complication of hemolysis?
|
mechnical or man-made cardiac valves
|
|
|
bioprosthetic valve with paravalvular leak
|

what type of valve and valve complication can be seen here?
|
|
|
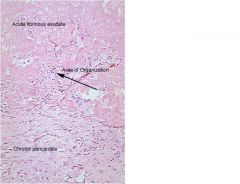
suppurative pericarditis
-pericardial space invaded by infective organism, organization is usually outcome not resolution |

What are causes of this type of pericarditis?
|
|
|
fibrinous / serofibrinous
-most frequent, due to acute mi, dressler, uremia, radiation, RF, SLE, trauma, post surgical |

type of pericarditis?
|
|
|
post surgical (adhesive) pericarditis
-type of chronic pericarditis due to surgery, TB, suppurative pericarditis and irradiation |
type of pericarditis?
|
|
|
constrictive pericarditis
-type of chronic pericarditis -hemodynamically resembles restrictive cardiomyopathy -due to chronic inflammation and fibrosis/thickening which results in decreased ventricular compliance |
type of pericarditis?
|
|
|
TB pericarditis
-chronic pericarditis, specifically, adhesive mediastinopericarditis |
type of pericarditis?
|
|
|
type of pericardial effusion?
caused by congestive heart failure, hypoalbunemia of any cause |
serous
|
|
|
type of pericardial effusion?
blunt chest trauma, malignancy |
serosanguinous
|
|
|
type of pericardial effusion?
mediastinal lymphatic obstruction |
chylous mediastinal lymphatic obstruction
|
|
|
etiology of primary myocarditis
|
viral: picorna virus, esp coxsackie A and B, others: ECHO, influenza, CMV, HIV
|
|
|
type of cardiomyopathy?
characterized by progressive cardiac hypertrophy, dilation and systolic dysfxn |
dilated cardiomyopathy
|
|
|
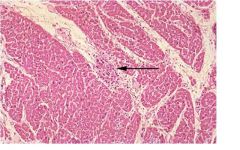
myocarditis - mononuclear inflitrate with necrosis
actue, fulminating infection - lymphocytic infiltrates, myofiber degeneration in patchy, focal fashion |
cardiac disease?
|
|
|
dialated cardiomyopathy - non specifica microscopic features including mixture of myocyte hypertrophy, interstitial fibrosis, and myocyte atrophy
|
cardiac disease?
|
|
|
hypertrophic cardiomyopathy - mutation in gene coding for heavy chain of B-myosin on chr 14
-leading cause of sudden death in young athletes |

genetic mutation seen in 50% of familial cases for this disease
|
|
|
what cardiac disease is assocaited with adriamycin and has a globoid outline?
|
dialated cardiomyopathy
|
|
|
category of myocarditis:
chagas disease, toxoplasmosis, trichinosis |
parasite
|
|
|
category of myocarditis:
lyme disease (borrelia), diptheria (endotoxin) |
bacterial
|
|
|
category of myocarditis:
allograft rejection, SLE, drug hypersensitivity, and sarcodosis |
Immune
|
|
|
category of myocarditis:
sarcoidosis, giant cell myocarditis |
unknown
|
|
|
all of the following cause what cardic disease?
adriamycin (dose related > 500 mg/m2) cyclophosphaminde lithium tricyclics chloroquine |
drug-induced cardiomyopathy
|
|
|
this is restrictive cardiomyopathy caused by hemochromoatosis
other causes include: amyliodosis, radiation injury, glycogen storage disease (pompe's disease) |

What is the cause of this disease?
|
|
|
this is restrictive cardiomyopathy caused by hemochromoatosis
other causes include: amyliodosis, radiation injury, glycogen storage disease (pompe's disease) |

What is the cause of this disease?
|
|
|
What cardiac disease has the following as primary causes:
1. endomyocardial fibrosis (primary form)children, young adults in Africa • starts in apex and moves toward valves 2. Loeffler endomyocarditis (eosinophilia) 3.endocardial fibroelastosis- children usually with congenital defect/aortic valve |
restrictive cardiomyopathy
|
|
|
restrictive cardiomyopathy, specifically due to hemochromotosis using Perl's iron stain
|
type of cardiac disease?
|
|
|
congenital cardiac disease?
1.due to rubella 2. pink on top and blue on bottom 3. hear machinery murmur 4. close giving indomethacin |
patent ductus arteriosus
|
|
|
cardiac disease that presents histologically with ashoff bodies
|
myocarditis due to rheumatic fever
|
|
|
most common cause of congenital heart disease in children charcterized by defect in interventicular septum
-possibley developing eisenmenger syndrome leading to pul htn and cynosis from r to l shunt |
VSD - ventricular septal defect
|
|
|
congenital defect seen in downs syndrome and fetal alcohol syndrome
|
ASD
|
|
|
associated with:
1. VSD 2. pulmonary stenosis 3. RVH 4. overriding aorta |
tetralogy of fallot
|
|
|
most common cyanotic congenital heart disease
|
tetralogy of fallot
|
|
|
type of coarctation seen in children and associated with tuner's synderome
|
preductal coarctation of aorta
|
|
|
disease?
1. see disparity btwn upper and lower extermites pulse 2. associated with notching of ribs 3. inc risk of intracranial anerysm rupture |
postductal coarcation of aorta
|
|
|
What disease is associated with cynotic spells and pt squattto improve symptoms?
|
Tetrology of Fallot, pt squatt to inc total systemic vascular resistance so to inc arterial pressure
|
|
|
What disease is associated with the following sx:
-splinter hemmorhages in nail bed -glomerulonephritis -roth spots -jainway lesons -osler node |
infective endocarditis which causes mitral regurg
|
|
|
what is oxygen supply due to?
|
coronary perfusion pressure and coronary vascular resistance
|
|
|
what disease are children with vsd likely to develop?
|
pul htn due to eisenmenger synderome which causes the left to right shunt to change to right to left causing pul htn to develop and cynosis
|
|
|
coronary blood flow is based on?
|
myocardial consumption of O2
|
|
|
type of angina?
coronary artery vasospasm at rest with stress test showing ST elevation = transmural ischemia |
prinzmetal angina
|
|
|
What coronary artery thrombosis is associated with mural thrombus?
|
LAD
|
|
|
triad for cardiac tamponade
|
1. sob with hypotension
2. elevated jvp 3. muffled heart sound |
|
|
-pericarditis (fibrinous pericarditis)
-arthritis of large joints, subcutaneous nodules, erythema marginatum, myocarditis, pulmonary involvement (pleuritis; uncommon) |
What was the likely cause of the friction rub when your patient was 12 years old? What other clinical manifestations may have been present?
|
|
|
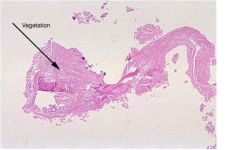
-tests: echo, blood cultures
-slide shows acute bacterial endocarditis; therapy is IV antibiotics to treat impending sepsis (heart valves are avascular and therefore difficult to eradicate the offending organism) |
When your patient’s sister presented, what laboratory tests would be the most helpful in establishing the correct diagnosis? Based upon your diagnosis what therapy is indicated and why?
|
|
|
-tests: echo, blood cultures
-slide shows acute bacterial endocarditis; therapy is IV antibiotics to treat impending sepsis (heart valves are avascular and therefore difficult to eradicate the offending organism) |
When your patient’s sister presented, what laboratory tests would be the most helpful in establishing the correct diagnosis? Based upon your diagnosis what therapy is indicated and why?
|
|
|
-a.) sepsis secondary to acute bacterial endocarditis
-b.) acute mitral regurgitation secondary to ruptured papillary muscle and/or chordae tendineae -arrhythmia -c.) sepsis (flushed skin, hypotension) |
What complications of acute endocarditis might have accounted for the patient’s demise? What pathologic findings would be associated with these complications? Which was most likely in our patient and why?
|
|
|
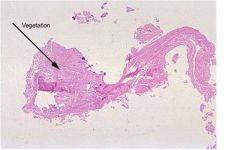
coagulation necrosis and liquefactive necrosis (septic infarction)
|
Describe in detail the histologic findings in the slides. What kinds of necrosis are present?
|
|
|
What are potential complication of a new mitral valve?
|
-at increased risk for endocarditis/paravalvular leaks (prosthetic valve)
-at risk for thrombosis (prosthetic valve) -at risk for arrhythmias (atrial hypertrophy) -other complications of prosthetic valves (i.e. mechanical deterioration, hemolysis) |
|
|
-pericarditis (fibrinous pericarditis)
-arthritis of large joints, subcutaneous nodules, erythema marginatum, myocarditis, pulmonary involvement (pleuritis; uncommon) |
What was the likely cause of the friction rub when your patient was 12 years old? What other clinical manifestations may have been present?
|
|
|
What complications of MI’s at this stage (5 days) might have accounted for the patient’s demise? What pathologic findings would be associated with these complications?
|
cardiogenic shock- >40% of LV infarcted and pulmonary edema
acute mitral regurgitation- ruptured papillary muscle and pulmonary edema ruptured MI- pericardial sac filled with blood (tamponade) arrhythmia- no changes or +/- pulmonary edema |
|
|
The tissue section was taken from the posterior wall of the left ventricle. In which coronary artery would you expect to find a thrombus? What if the section were from the lateral or anterior ventricular wall?
|
LAD---anterior LV and anterior 2/3 of the interventricular septum
LCA---lateral wall of the LV (posterior wall in 10-20% of patients) RCA---posterior wall of the LV and posterior 1/3 of the interventricular septum |
|
|
reductions greater than 75% can cause critical stenosis resulting in ischemia on (manifest as angina pectoris)
|
In examining the heart at autopsy, you find atherosclerotic plaques in the left anterior descending and left circumflex coronary artery. The luminal diameter of the LAD is reduced by 90%. How is this finding significant?
|
|
|
drug of choice to treat stage 1 htn (145 - 159 / 90 - 99)
|
1st - hctz, chlorothalidone
2nd - ACEI, ARB, BB, CCB or combo |
|
|
drug class?
inhibit active exchange of Cl-Na in distal convoluted tubule |
thiazides
|
|
|
drug class?
inhibit reabsorption of Na in dital convoluted and collecting tubule |
potasium sparing diuretics
-triamterne -amiloride |
|
|
drug class?
inhibit exchange of Cl-Na-K in the thick segment of acending loop of henle |
Loop diuretics
-furosemide -torsemide |
|
|
drug of choice to treat stage 2 htn (> 160 / > 100)
|
2 drug combo, usually hctz and ACEI or ARB or BB or CCB
|
|
|
major ae: hypokalemia, hypotension, DM, gout
->dec morbidity and mortality |
hctz
|
|
|
compelling indication for dieurtics
|
hf, high cad risk, dm, recurrent stoke prevention
|
|
|
drug group used to tx chf and htn
ae: acute renal failure (imp) and hypokalemia and hypomag |
loop diuretics
|
|
|
ae: ototoxicity
|
loop diuretics
|
|
|
drug used when creatine clearance low
|
dont use hctz
use loop diuretics |
|
|
drug group added to hctz and loop diuretics to tx hypokalemia
|
K sparing diuretics - triamterene, amiloride
|
|
|
what effect does salt sub like Mrs Dash have on drug txmt of htn
|
can cause hyperkalemia if pt on hctz or loop diuretic and K sparing diuretic
|
|
|
drug group which acts to inc hr, dec cardiac contractility, dec cond vel and ince refractory period of av node
|
bb
|
|
|
ae: bradycardia, bronchospasm, mask hypoglycemia in dm
|
bb
|
|
|
drug group?
contraindication: asthma caution: pt with bradycardia due to lv failure |
bb
|
|
|
ae: othostatic hypotension, syncope, hypotension
|
a-blockers: terazosin, prazosin, doxazosin
|
|
|
used to be used for bph
|
a-blockers: terazosin, prazosin, doxazosin
|
|
|
cardiac effects of ACEI
|
dec preload, dec afterload, inc co, inc sv, dec cardiac and venous remodeling
|
|
|
drug class?
ae: hyperkalemia, acute renal failure, cough (accum of bradykinin) and angioedema |
ACEI: lisinopril, captropril, ramipril
|
|
|
compelling indication:
hf, post mi, cad high risk, dm, dec repeat stock |
ACEI: lisinopril, captropril, ramipril
|
|
|
caution use in bilateral renal artery stenosis
|
ACEI: lisinopril, captropril, ramipril
ARB: valsartan, losartan, candesartan, irbesartan |
|
|
used when pt develops cough due to ACEI
|
ARB: valsartan, losartan, candesartan, irbesartan
|
|
|
moa: blockade of aldosterone receptor
|
aldoserone antagonist: spironolactone, eplerenone
|
|
|
drug class with compelling indication for post mi and hf
|
aldoserone antagonist: spironolactone, eplerenone
|
|
|
moa: act on rate-limiting step in renin-angiotensin-aldosterone system
|
renin inhibitor: aliskiren
|
|
|
moa: block L-type calcium channel in cardiac cells and smooth muscle cells
|
ccb: dihydropyridines=> amlodipine and nifedipine
non-dihydropyridines=> diltiazem and verapamil |
|
|
ccb which only vasodilate
|
dihydropyridines=> amlodipine and nifedipine
|
|
|
ccb which vasodilate and dec hr
|
non-dihydropyridines=> diltiazem and verapamil
|
|
|
what drug class has these compelling indication:
dm and cad high risk |
ccb
|
|
|
What ccb have ae: bradycardia?
|
non-dihydropyridines=> diltiazem and verapamil
|
|
|
ae: peripheral edema and reflex tachycardia
|
dihydropyridines=> amlodipine and nifedipine
|
|
|
used to tx supraventricular tachycardia
|
non-dihydropyridines=> diltiazem and verapamil
|
|
|
vasodilator with ae of constipation
|
non-dihydropyridines> verapamil
|
|
|
cheep vasodilator which must be tapered off otherwise will cause htn crisis
|
clonidine
|
|
|
vasodilator dosed 3 or 4 times a day and causes rash and SLE-like rxn
|
hydralazine
|
|
|
inhibit platelet aggregation, prevent acute coronary syndrome
|
asa and clopidogrel
|
|
|
reduce O2 demand on heart, prevent sx of cardiac ischemia
|
bb, ccb
|
|
|
drug classes which reduce plaque formation, stabilzed plaque, dec long term risk :
-reduce cv risk |
ACEI, ARB, eplerenone
|
|
|
gold standard tx for cad and dm
|
asa
|
|
|
tx for stable angina
|
bb (1st), ccb, nitro
|
|
|
tx for unstable angina
|
iv nitro, asa, bbl, anticoag
revascularize |
|
|
how long in advance does asa or clopidogrel need to be stoped before surgery
|
5 - 7 days
|
|
|
drug which dec hr, dec contractility, dec O2 demand, dec ischemia
|
bb
|
|
|
added on to bb in tx of stable angina
|
ccb
|
|
|
order of drug add on for tx of angina
|
bb 1st, ccb 2nd, nitrates 3rd
|
|
|
long acting nitrate
|
isosorbid mononitrate
|
|
|
moa: alters the trans-cellular late Na current, alter Na-dependent Ca channel during myocardial ischemia
reserved for refractory pt prolongs QT interval |
ranolazine
|
|
|
ae: rhadomyolysis and lft elevation
|
statins
|
|
|
drug classes that dec mortality
|
hctz, bb, asa, acei, arb, spirolactone
|
|
|
drug classes that can cause acute renal failure
|
k-sparing, ACEI, aldosterone antagoinst
|
|
|
drug classes that cause hyperkalemia
|
K-sparking dieurtics, ACEI, renin inhibitor
|
|
|
how to tx htn crisis due to clonidine
|
intially tx with clonidine then taper pt off
|
|
|
T or F
You can change pt stage in HF but not class. |
F, class based on sx, stage based on progression of disease state, sx (class) can be improved but disease state can not be reversed
|
|
|
AE: hypokalemia, angioedema, dry cough, renal insuffiency, hypotension
|
ACEI: lisinopril, captopril, enalapril, ramipril
|
|
|
what lab monitered when tx pt with ACEI
|
serum Cr
|
|
|
what pt characteristic will lend them to develop acute renal failure with ACEI?
|
dont use with pt in low volume state seen in pt with pul cong and pitting edema, also hf and bilateral renal stenosis leading to dec GFR
|
|
|
what is the lab value to moniter with dierutics in chf
|
fluids, i/o, electrolytes, weight
|
|
|
moa: antagonized aldosterone effect of facilitating myocardial fibrosis
|
spirolactone
|
|
|
ae of diuretic = gyneomastia
what drug to switch to? |
spirolactone
eplerenone |
|
|
ae: bradycardia, av block, arrythymia, confusion, visual disturbances, hyperkalemia in acute OD, n/v, diarrhea, narrow theraputic window
|
digoxin
|
|
|
moa: block Na-K ATPase
|
digoxine
|
|
|
early sign of digoxin toxicity
|
cns and gi toxicity
|
|
|
T or F
Digoxin can be pushed to treat a fib |
F
|
|
|
cause venous vasodilation
|
nitrates
|
|
|
cause arterial vasodilation
|
hydralazine
|
|
|
ae: cyanide and thiocynate toxity
|
nitroprusside
|
|
|
T or F
htn pt and chf pt can take same doses of bb |
F, with chf must start bb very lowest does and very gradually inc dose
|
|
|
moa: synthetic analog of brain natiuretic peptide
|
nesiritide
|
|
|
B agonist used in pt with acute decompensatd heart failure - stage III or IV, last resort
|
dobutamine
|
|
|
inhibit breakdown of cAMP
AE:hypotension, arrythmia, tachycardia |
milrinone
|
|
|
used by IV for txmt in htn crisis
|
nitroprusside
|
|
|
ae of nesiritide
|
hypotension
|
|
|
asymtomatic chf pt with lv dysfxn, ef< 40%
txmt? |
ACEI, ARBS
|
|
|
symptomatic chf pt, nyha II
txmt? |
dieurtics and bb
|
|
|
symptomatic chf pt, nyha III
txmt? |
inc diuretics, maybe add spirolactone or digoxin
|
|
|
symptomatic chf pt, nyha IV
txmt? |
inotropes, vasodilator, specialzed therapy, transplant
|
|
|
vasodilators
|
hydralazine, nitrates
|
|
|
pressors
|
dopamine,ne, epi
|
|
|
dose of dopamine?
renal, cerebral and mesenteric vessel dilation |
low dose
|
|
|
dose of dopamine?
mainly see B1 simulating effects, inc contractility and HR |
med dose
|
|
|
dose of dopamine?
overwelming effect on A1 stimulation, inc SVR, inc afterload, inc bp |
high dose
|
|
|
pressor indication
|
systolic bp < 90 mm Hg
-w/o hypovolemia -frequently in spetic or cardiogenic shock |
|
|
precaution with pressors
|
inc hr = arrhythmogenesis
inc O2 demand on heart monitore for signs and sx of mycardial ischemia |
|
|
tx hf and afib
|
amiodarone and dofetilide
|
|
|
ekg changes seen couple hours after MI
|
st elevation and inverted t wave
|
|
|
what changes in ekg are seen couple days after mi
|
normal st segment and normal t wave
|
|
|
when does the following histological change occur after MI?
continuing coagulation necrosis; pyknosis of nuclei, shrunken eosinophilic cytoplasm, neutrophilic infiltrate well developed |
18-24 hours
|
|
|
when does the following histological change occur after MI?
scarring complete |
> 4 weeks
|
|
|
when does the following histological change occur after MI?
beginning disintegration of dead myofibers and resorption of sarcoplasm; onset of marginal fibrovascular response (fibroblasts, macrophages) |
3 - 7 days
|

