![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
243 Cards in this Set
- Front
- Back
|
excitability is
|
ability of cell to respond to stimulus
|
|
|
Automaticity is
|
ability of cell to reach threshold potential and generate impulse without outside stimulus
|
|
|
pacemaker is
|
the SA node. sets the pace for the rest of the heart and transmits impulse throughout myocardium
|
|
|
the heart delivers blood to body by
|
contracting and relaxing myocardium
|
|
|
what is conductivity
|
ability of muscle to move impulse from cell to cell
|
|
|
what is contractility
|
shortening of muscle when stimulated
|
|
|
what neurtransmitters work within the sympathetic (adrenergic) nervous system
|
epinephrine and norepinephrine
|
|
|
What does epi- and norepinephrine do in the body?
|
raises the blood pressure
increases Heart Rate enhances force of myocardial contraction |
|
|
what is the NE for the cholenergic parasympathetic system?
|
acetylcholine
|
|
|
What does acetylcholine do
|
decreases heart rate
lowers bp reduces force of myocardial contraction |
|
|
what is the rate of the sinus node
|
60-100 bpm
|
|
|
what is the rate of the av node
|
40-60 bpm
|
|
|
what is the rate of the bundle of his
|
40-60 bpm
|
|
|
what is the rate of bundle branches
|
20-40
|
|
|
what is the rate of purkinjie fibers
|
15-40
|
|
|
during the resting state, are the following electrolytes higher or lower in side the cell.
K+, Ca+, Na+ |
Na+ is lower
K+ is higher Ca+ is lower |
|
|
what happens to K+, Ca+, Na+ during depolarization in reference to cells
|
during depolariztion, the heart is contracting due to Na+ and Ca+ moving inside the cell and K+ moving out.
|
|
|
what is action potential
|
depolarization
|
|
|
what is repolarization
|
returning to resting state
|
|
|
what is an electrocardiogram
|
ECG is a graphic display of conduction
It shows the magnitude and duration of the electrical activity of the heart |
|
|
monophasic action potential refers to
|
the depolarization and repolarization of the cardiac muscle cell
|
|
|
What happens during phase 0 of the monophasic action potential
|
Na+ enters the cell - Depolariztion!
|
|
|
What happens during phase 2 of the monophasic action potential
|
Ca+ enters the cell, initiation of contraction
|
|
|
When does the actual contraction start, with Na or Ca?
|
with Ca+
|
|
|
what happens during phase 3 of the monophasic action potential
|
K+ exits the cell - repolarization
|
|
|
What is the Chantest cardiac channel panel
|
this measures the currents of each of the channels of action potential with an ECG.
|
|
|
What do the electrodes do on the ECG , and then what does the machine do with them?
|
Electrocardiogram
• Electrodes sense activity & transmit to ECG machine • Machine transforms activity to waveforms that correspond with depolarization and repolarization |
|
|
In a 3 lead cardiac monitoring system what is the white lead polarity
|
negative
|
|
|
In a 3 lead cardiac monitoring system what is the red lead polarity
|
positive
|
|
|
In a 3 lead cardiac monitoring system what is the black lead polarity
|
Positive for lead I
negative for lead II it switches polarity depending on the lead chosen. |
|
|
In a lead II the complexes are downward or upright
|
upright, the impulses moves toward the positive
|
|
|
In a V1 or Lead MCL1 are the complexes upwards or downwards
|
downwards. impulses moves away from positive electrode
|
|
|
What are dysrhythmias
|
disorders of hearts conduction
disturbance of rate, rhythm or both identified by analyzing ECG |
|
|
in analyzing ecgs, the rhythm is named according to>>>
|
origin of impulse: sn, atria, AV node, ventricles
and mechanism of conduction: bradycardia, tachycardia, flutter, fibrillation, premature beats, escape beats, heart blocks |
|
|
what is the skin prep for electrode placement
|
have hair from electrode placement site
rub site briskly with alcohol pad rub site with 2x2 gauze place electrode, be sure that electrode has moist get. |
|
|
What does the V1 view
|
ventricular activity and differentiate between right and left bundle branch blocks
|
|
|
how can you view a VI
|
with a five lead system or the MCL1
|
|
|
How often should you change electrodes
|
q day
|
|
|
what are some trouble shooting tips for electrodes not reading correctly
|
make sure all elec pt care equip is grounded
make sure they are all intact make sure leads are connected tightly to electrodes batteries. pt may be moving |
|
|
on the ekg paper, what is measured along the horizontal axis
|
time
|
|
|
what is measured along the vertical axis
|
voltage
|
|
|
the large square measures ___ seconds
|
0.2 seconds
|
|
|
each small square measures ___ secondds
|
0.04 seconds
|
|
|
each small square measures __ volts
|
1mm
|
|
|
the pr interval measures from where to where
|
from the begining of the P to the begining of the R
|
|
|
the pr segment measures from where to where
|
end of P to begining of R
|
|
|
the qrs segment measures from where to where
|
begining of q to end of s
|
|
|
the st segment measures from where to where
|
end of s to begining of t
|
|
|
the tp interval measures from where to where
|
end of T to begining of P
|
|
|
the QT interval measures from begining of Q to
|
end of T
|
|
|
15 large blocks on the ekg equals how many seconds
|
3 seconds
|
|
|
6 second strip has how many large blocks
|
30
|
|
|
voltage of 1mV =
|
1 mm
|
|
|
one small block vertical voltage =
|
1mm
|
|
|
one large block vertical voltage =
|
5mm
|
|
|
in 5 large blocks or 1 second, how many mm per second is there
|
5
|
|
|
easy count for heart rate can be done by counting ____ waves in a 6 second strip and x ____
|
R waves x 10
|
|
|
using the 1500 method, the 1500 small squares represents 1 minute, you can count the small square between identical points on 2 consecutive P or R waves then divide .......
|
1500 by that number
|
|
|
1500 method
You can count the number of big squares between 2 consecutive R waves, then divide..... |
300 by that number
|
|
|
What does the QRS complex indicate
|
ventricular depolarization, or contraction of the ventricles
|
|
|
what does the p wave indicate
|
atrial depolarization or contraction of the atrium
|
|
|
what is normal duration of P waves
|
less than 3 small squares or .11 or less and less than 3mm in amplitude
|
|
|
what is the normal length of QRS waves
|
not longer than 0.10 in duration or 5 mm in amplitude in lead II
|
|
|
what does the T wave indicate
|
ventricular repolariztion
|
|
|
how should the T wave look
|
rounded and asymmetrical, not more than 5MM in ampliture
|
|
|
what is the normal PR interval
|
0.12 to 0.20 seconds
|
|
|
what does the PR interval indicate
|
AV conduction time
|
|
|
What does the QT interval indicate
|
repolarization time
|
|
|
what is the general rule of length for the QT interval
|
duration is less than half the preceding RR interval
|
|
|
what are the first 3 steps for interpretation of the EKG strip
|
1. Scan strip: look for all components: P-QRS-T
2. Determine rates ATRIAL = Count P waves VENTRICULAR = Count R waves 3. Determine A-V rhythms Check R-wave to R-wave for Regularity or Irregularity |
|
|
after you have rate and rhythms, what do you evaluate and measure
|
4. Evaluate P waves before every QRS complex. Are they uniform? Regular? Do they march out?
5. Measure PR interval: 0.20 seconds or less. Uniform? Regular? March out? 6. Measure QRS complex: between 0.06 – 0.12. Uniform? Regular? March out? 7. Evaluate T wave Uniform? 8. Measure QT interval - Normal 0.36- 0.44 |
|
|
What are the components of NSR
|
regular interval between each QRS complex (R-R interval)
PR interval of 0.12 - 0.20 seconds All components and rate with in normal limits (WNL) Normal EKG with P, QRS and T waves present |
|
|
What does sinus arrhythmia mean
|
minor regular variations in hr and pulse pressure associated with respiration
|
|
|
What are the components of Sinus Bradycardia
|
~ A sinus rhythm (originates in the SA node)
~ Slower than 60 beats per minute (BPM). ~ May occur with vagal (parasympathetic) stimulation, such as in trained athletes or in patients with the carotid sinus syndrome ~ May also occur as a result of pharmacological beta-blockade. No treatment necessary unless patient symptomatic |
|
|
What is Tx for Bradycardia?
|
none, unless pt is symptomatic
Then O2. Persistent cadiorespiratory compromise - CPR is poor perfusion and >60 bpm Then epinephrine . repeat 3-5 minutes. If increased vagal tone or primary AV block - atropine consider H & Ts |
|
|
what are Hs in Hs & Ts
|
hypovolemia
hypoxia hydrogen ion hypo/hyperkalemia hypoglycemia hypotermia |
|
|
What are the Ts in Hs & Ts
|
Toxin
Tamponade, cardiac Tension pneumothorax Thrombosis Trauma (hypovolemia or ICP) |
|
|
What are the components for sinus tachycardia
|
• Sinus rhythm with a heart rate greater than 100 BPM.
• Causes: fever, sympathetic stimulation (from a variety of causes, including medications) and cardiac toxicity • The pulse pressure may be lower due to a lower stroke volume and decreased time for diastolic run-off. |
|
|
what are the components of atrial flutter
|
• Atria are stimulated to contract at a rapid rate (typically 200-350 BPM).
• In atrial flutter the depolarization wavefront travels in a circular fashion around and around the atrium. • This is not a sinus rhythm. • Atrial flutter is associated with aging as well as hypoxia, electrolyte and membrane disturbances, increased atrial pressures, mitral or tricuspid valve disease, hyperthyroidism, and hypercalcemia. |
|
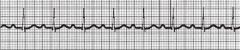
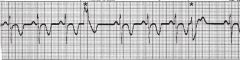
name the ekg
|
1st degree block
|
|

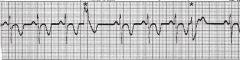
name the ekg
|
artifact
|
|

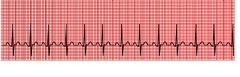
name the ekg
|
astole
|
|

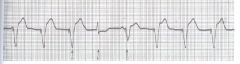
name the ekg
|
A Fib
|
|
name the ekg
|
AV nodal reentry tachycardia
|
|
name the ekg
|
ECG on demand pacing
|
|
name the ekg
|
Fixed Pacing
|
|

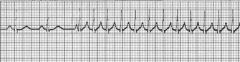
name the ekg
|
Mobitz 1 wenchkebach
|
|

name the ekg
|
Mobits II
|
|
name the ekg
|
Mulifocal PVC quadrigeminy
|
|

name the ekg
|
PAC
|
|

name the ekg
|
PVC
|
|

name the ekg
|
sinus bradycardia
|
|
name the ekg
|
sinus Tachycardia
|
|

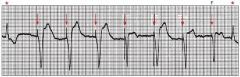
name the ekg
|
3rd degree block
|
|

name the ekg
|
ventricular Fibrillation
|
|
name the ekg
|
ventricular pacemaker
|
|

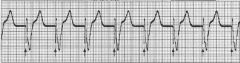
name the ekg
|
V - Tachycardia
|
|

name the ekg
|
wolff parkinson white
|
|
|
what is the Tx of atrial Flutter
|
if unstable
Cariovert if stable Adenosine IV amiodarone |
|
|
describe atrial fibrillations regular or irregular contractions
|
There is no concerted depolarization
or contraction of the atria. Also, due to the chaotic nature of atrial depolarization's, there is irregular penetration of the AV node, resulting in irregular ventricular contractions. |
|
|
Tx of AFib
|
If acute onset (within 48 hrs)
Adenosive IV Amiodarone |
|
|
what are the Tx goals of Atrial Fibrillation
|
to Decrease atrial irritation
decrease rate of ventricular response |
|
|
if your pt has chronic A-Fib, what is the medication treatment
|
Anticoagulation so they don't throw a clot. Warfarin sodium (coumadin)
Digoxin and Diltiazem (cardizem) |
|
|
What are the conditions to use Cardivorsion?
|
unconscious or appropriately sedated, IV access, Oxygen turned off,
monophasic machine 50-100 joules synchronized - shock during ventricular depolarizaiton so we don't get it on the T wave. |
|
|
is a consent needed for cardioversion
|
yes, if conscious
elective procedure |
|
|
Why would you want to do cardioversion
|
so pt doesn't go into V fib and need defibrillation.
|
|
|
What is the criteria for Junctional Rhythm
|
• Occurs when the AV node becomes the pacemaker of the heart
• P wave may be absent • PR interval: is less than 0.12 seconds • Regular rhythm • QRS: usually normal |
|
|
When does AV nodal reentry tachycardia occur.
|
when an impulse is conducted to an area in the AV node that causes the impulse to be rerouted back into the same area over and over again at a very fast rate.
|
|
|
what is the criteria for AV nodal reentry tachycardia
|
• P wave; is difficult to discern
• Regular, rapid rate, sudden onset and termination • Atrial rate usually 150-250 and the ventricular rate is usually 75-250 |
|
|
when there is a disease of the AV junction or the His-Purkinje system, the result is an impaired conduction from the atria to the ventricles. This results in _____ _________ Blocks
|
Atrioventricular conduction blocks
|
|
|
name the heart blocks
|
First Degree heart block
2nd degree heart block,Mobitz type 1 (W) 2nd degree heart block,Mobitz type II |
|
|
What are the components of the First Degree heart block
|
First Degree Heart block.
Delayed conduction through the AV junction resulting in a PR interval of !! greater than 0.20 seconds !! All other components of EKG WNL |
|
|
What are the components of the Second Degree heart block
|
Not all impulses are conducted through the AV junction then the condition.
There are 2 P waves for every QRS complex. This is termed a 2:1 block. The PR interval is less than 0.20 seconds. In second degree block the PR interval may be normal, prolonged, or may progressively increase until a QRS is missed (Wenckebach rhythm). |
|
|
What are the components of the Second Degree mobitz I heart block
|
• Rate variable
• P wave normal morphology with constant P-P interval • QRS normal • Conduction: the P-R interval is progressively longer until one P wave is blocked; the cycle begins again following the blocked P wave. • Rhythm irregular |
|
|
Where does the 2nd degree AV block occur
|
in the AV node above the bundle of His
|
|
|
What may cause it?
|
acute Inferior MI or
Digitalis Toxicity |
|
|
What is the Tx for wenckebach
|
not indicated as rhythm usually produces no symptoms
|
|
|
What are the components of the Second Degree mobitz II heart block
|
the pp is regular, but the rr is irregular
|
|
|
where does the mobitz II block usually occur
|
below the bundle of His and may progress into a higher degree block
|
|
|
when can a mobitz ii occur
|
after an acute anterior MI due to damage in the bifurcation or the bundle branches
|
|
|
which is more serious, the type 1 or type 2 block
|
Type ii block
|
|
|
What is the treatment for Type II block
|
artificial pacing
|
|
|
What is a 3rd degree block
|
no impulses are conducted through the AV junction
|
|
|
What are the components of the Third degree heart block
|
• Rate atrial rate is usually normal;
ventricular rate is usually less than 70/bpm. The atrial rate is always faster than the ventricular rate. • P wave normal with constant P-P intervals, !! but not "married" to the QRS complexes. !! |
|
|
what does the QRS look like in a 3rd degree block
|
normal or widened
|
|
|
what is the rhythm in a 3rd degree block
|
irregular
|
|
|
what may cause a 3rd degree block
|
digitalis toxicity
acute infection |
|
|
what is a complete heart block
|
3rd degree heart block
no av conduction!! |
|
|
what happens in a complete heart block
|
MI
degeneration of the conductive tissues |
|
|
Tx for 3rd degree block
|
external pacing and Atropine for aute symptomatic episodes
permanent pacing for chronic complete heart block |
|
|
What is the key feature of an AV conduction block - 1st degree
|
prolonged PR interval over .20
|
|
|
What is the key feature of an AV conduction block - 2nd degree
|
not all impulses conducted through the AV junction
|
|
|
What is the key feature of an AV conduction block - 3rd degree
|
no impulses conducted through AV junction, dissociated atrial and ventricular rhythms
|
|
|
what is ectopic
|
Ectopic - 'in abnormal place or position' from the Greek 'ektopos' which means "out of place".
• Occurs from an abnormal site (called an ectopic focus) before the expected time of the next contraction. • Ectopic beats (also called extra systoles or premature contractions) may originate in the atria, the AV junction or the ventricles. |
|
|
what are causes of ectopics
|
local
ischemia, drugs (caffeine is a good example), calcified plaques and physical contact (such as contact of the heart with catheters or surgical instruments) |
|
|
what does PVC stand for
|
Premature Ventricular Contraction
|
|
|
What are the components of a PVC
|
• QRS earlier than expected (premature) i.e. shorter RR interval than
normal • QRS wider than normal • QRS voltage higher than normal • inverted T wave • obscured P wave • next RR interval longer than normal |
|
|
common characteristics of most PVCs
|
• Wide and bizarre QRS, often with a high voltage and inverted T wave
• Reduced or no left ventricular ejection • Fully compensatory pause |
|
|
BIGEMINY is every
|
every other beat
|
|
|
TRIGEMINY is every
|
every third beat
|
|
|
UNIFOCAL they all are
|
all uniform
|
|
|
MULTIFOCAL they all look
|
look different
|
|
|
Tx for PVC
|
If multifocal or with ischemia - notify MD
|
|
|
Multifocal PVC medicine Tx is
|
Amiodarone Bolus 150 mg over 10 minutes. May repeat in 10 to 15 minutes. flow with IV drip of 1 mg/minute.
May need oral antiarrythmic |
|
|
What are the components of the idioventricular rhythm
|
• Ventricular rate: 20-40
• Regular • QRS: Bizarre, abnormal shape, duration is 0.12.seconds or more |
|
|
What are the components of the ventricular tachycardia rhythm
|
• Rate usually between 100 to 220/bpm, but can
be as rapid as 250/bpm • P wave obscured if present and are unrelated to the QRS complexes. • QRS wide and bizarre morphology • Conduction as with PVCs • Rhythm three or more ventricular beats in a row; may be regular or irregular. |
|
|
When does V-Tach occur
|
almost always in diseased hearts
|
|
|
what are some causes of V-tach
|
CAD
Acute MI Digitalis Toxicity CHF Ventricular aneurysms |
|
|
Tx for Ventricular Tachycardia
|
• Electrical countershock is the intervention
of choice if the patient is symptomatic and rapidly deteriorating. • Some pharmacological interventions include amiodarone and lidocaine • May insert Automatic Internal Cardiac Defibrillator (AICD) |
|
|
components of Ventricular Fibrillation
|
• Rate unattainable
• P wave may be present, but obscured by ventricular waves • QRS not apparent • Conduction chaotic electrical activity • Rhythm chaotic electrical activity |
|
|
Tx for Ventricular Fibrillation
|
• Defibrillation (Start with 120-200 joules)
• CPR • Epinephrine 1 mg • Vasopressin 40 units • May insertion of AICD |
|
|
With cardioversion, the current delivery is unsynchronized or synhronized with pts ECG
|
synchronized
|
|
|
With defibrillation, the current delivery is unsynchronized or synhronized with pts ECG
|
unsynchronized.
|
|
|
What is the pounds of pressure for the paddles with defibrillation
|
20-25 lbs of pressure
|
|
|
during cardioversion or defibrillation
DO NOT>>>>> |
shock a pt who is awake
forget to synchronize when cardioverting forget the conduction gel forget to clear the bed take orders from two doctors at the same time |
|
|
After cardioversion or defibrillation make sure to....
|
– Monitor the patient carefully
– Keep the patient well-oxygenated – Check the patient’s labs – Get a 12-lead EKG for documentation – Assess the patient’s skin |
|
|
when does asystole occur
|
• Asystole occurs most commonly following the
termination of atrial, AV junctional or ventricular tachycardias. This pause is usually insignificant. • In the presence of acute MI and CAD, asystole may continue—Cardiac Arrest |
|
|
Tx for Asystole
|
CPR
Artifical Pacing Epinephrine Atropine |
|
|
What is a pacemaker
|
an electronic device that provides electrical stimuli to the heart muscle
|
|
|
What are two types of pacemakers
|
Permanent
Temporary |
|
|
What is the NASPE-BPEG code
|
....for pacemaker function
(North American Society of Pacing and Electrophysiology) |
|
|
What are complications of Pacemaker use?
|
• Infection
• Bleeding or hematoma formation • Dislocation of the lead • Skeletal muscle or phrenic nerve stimulation • Cardiac tamponade • Pacemaker malfunction |
|
|
What is a implantable Cardioverter Defibrillator (ICD)
|
A device that detects and terminates life threatening episodes of tachycardia or fibrillation
and Antitachycardia pacing |
|
|
What is Catheter Ablation Therapy
|
• Destroys specific cells that are the cause or
central conduction route of a tachydysrhythmia. • Performed after a electrophysiologic study. |
|
|
What rhythms are the usual indicators for Catheter Ablation therapy
|
• Usual indications:
– AVNRT – Recurrent atrial dysrhythmia • AF – VT |
|
|
What is Wolff-Parkinson-White rhythm look like
|
• Short PR interval, slurred initial upstroke of the QRS
comples (delta wave) and prolonged QRS duration |
|
|
is the SA Node the pump?
|
no it is electrical pacemaker for the heart
|
|
|
The sympathetic system does 3 things that reflects the Fight or flight response, what are they
|
increase HR and BP, and enhances the force of myocardial contraction.
|
|
|
during resting state, the K+ is higher where?
|
inside the cell
|
|
|
Repolarizing is R______
|
Repolarizing is Resting
|
|
|
Depolarization is the _ wave
|
QRS
|
|
|
Repolarization is the _ wave
|
T
|
|
|
Red lead is ____ polarity, so the Black lead is ____ for lead I
|
positive, positive
|
|
|
The white lead is ____ polarity, and the black lead is ____ for lead II
|
negative, negatiave
|
|
|
The triangle of lead has positive or negative at the L arm?
|
Negative White lead
|
|
|
The triangle of the leads has the ___ lead at the R arm
|
black + or -
|
|
|
The triangle of leads has the ____ lead at the LL
|
+ lead, - lead is White
|
|
|
leads V1- V6 look at the ____ part of the heart, mainly the ___ ventricle
|
anterior, left
|
|
|
Lead II looks at the ___ part of the heart
|
inferior
|
|
|
legs and arms look at more ____ or ____ parts of the heart
|
inferior or posterior
|
|
|
V1 lead is the best lead to differentiate between ___ and ____
|
right and left bundle branch blocks
|
|
|
What may cause a ekg that mimics ventricular Tachycardia
|
artifacts from parkinsons or brushing teeth
|
|
|
to figure the heart rate, use the 1500 method, count the number of ____ and divide______
|
the number of large blocks between R R and divide into 300
|
|
|
QT interval follows the rule of time:
|
duration is less than half the preceding RR interval
|
|
|
What is a normal QT interval
|
.36 to .44
|
|
|
Treatment for symptomatic Bradycardia - what are the meds?
|
Atropine IV
1st doese o.5 mg repeat in 3-5 minutes max dose 3 mg Dopamine - iv infusion 2-10mcg/kg or Epinephrine 2-10 mcg/per minute |
|
|
Is bradycardia treated?
|
no, unless they are symptomatic - then atropine, then dopamine or epinephrine
|
|
|
What meds make produce sinus bradycardia?
|
Beta blockers
|
|
|
what can cause sinus tachycardia
|
fever, medications (such as those that slow A fib down), cardiac toxicity
|
|
|
is atrial flutter regular or irregular
|
regular
|
|
|
What is the conductions you can have with Atrial flutter
|
4:1, 3:1, 2:1
|
|
|
what may cause Atrial flutter
|
aging, hypoxia
electrolyte and membrane disturbances increased atrial pressures, hyperthyroidism, hypercalcemia, mitral or tricuspid valve disease |
|
|
if pt has atrial flutter and is unstable, how do you treat?
|
Meds: Adenosine IV
Amiodarone |
|
|
if pt has atrial flutter and is stable, how do you treat?
|
Cardivert
|
|
|
key features of atrial flutter
|
saw tooth shaped flutter waves in the ecg atrial rate
typically 200-350 whole number ration of flutter waves to QRS complexes. |
|
|
1st thing - when you look at a strip, and it is irregular - then think....
|
A fib
|
|
|
Treatment of A Fib
|
Same as unstable A tach;
Adenosine IV Amiodarone (within 48hrs) |
|
|
why are you treating A Fib
|
because they are making clots!
|
|
|
Chronic AFib needs to be on what type of meds
|
anticoagulants: warfarin or high dose lovenox., Digoxin a positive inotropic to increase contractility.
|
|
|
Why do you put pts on meds for Chronic A Fib?
|
They have lost their atrial kick - no contraction, loss of 30% of their ejection rate.
|
|
|
3 things go together with Cardioversion
|
Sedation
O2 off Syunchronized |
|
|
When the AV node becomes the pacemaker of the heart, what type of rhythm is there?
|
Junctional Rhythm
40-60 bpm |
|
|
junctional rhythm - where is the P wave
|
absent or inverted and under .12
|
|
|
is junctional rhythm regular
|
yes
|
|
|
what are irregular rhythms?
|
A Fib
mobitz I, Wenchebach 3rd Degree Block V Tach may be irregular or regular V Fib |
|
|
1st degree block, the PR interval is greater than ____ block
|
1 large block > .20
|
|
|
If a second degree block has 2 P waves for every QRS, then it is termed?
|
a 2:1 block
|
|
|
The block occurs above the bundle of His in what blocks?
|
Block 2, type 1 is above, Block 2, Type 2 is below
|
|
|
Where does the block occur in Block 1
|
it is a delayed conduction through the AV junction
|
|
|
in a 3rd degree block, where does the block occur?
|
complete block of atrial impulses at the AV junction, common bundle or bilateral bundle branches.
|
|
|
Is the 2nd degree, type 1 block treated?
|
Not treated, may be due to acute inferior MI or digitalis toxicity
|
|
|
is 1st degree, type 2 block treated?
|
yes, serious.
Usually artificial pacing. |
|
|
what is a key feature of a 3rd degree block
|
the p waves and qrs waves are not married to each other. The QRS are wide
|
|
|
what is the rate of a complete heart block
|
under 70 bpm.
|
|
|
what is the rhythm of a complete heart block
|
irregular
|
|
|
is the PR Interval consistent in a 3rd degree block
|
not consistent, the P waves are not married to the QRS
|
|
|
what causes a 3rd degree block
|
MI
degeneration of the conductive tisssue |
|
|
Tx for 3rd degree block
|
external pacing
Atropine for actue symptomatic episodes permanent pacing (pacemaker) |
|
|
what is sundbergs poem
|
*if R is Far from P, then you have a first Degree...
*Long, longer, longer - Wenchebach *if some Ps dont' go through, then you have a Mobitz II *If R & P don't agree then you have a 3rd degree. |
|
|
what are Ectopics
|
premature contractions, extra systoles
|
|
|
can a pt feel a PAC
|
no
|
|
|
can a pt feel a pvc
|
yes
|
|
|
Why is the next R to R interval longer than normal after a PVC
|
because it has a full compensatory pause after PVCs
|
|
|
What is the ventricular ejection with a PVC
|
it is reduced or no left ventricular ejection
|
|
|
How do you count the PVCs, with 3 regular beats and one PVC it is
|
Quadrigeminy
|
|
|
How do you count the PVCs, with 1 regular beats and one PVC it is
|
Bigeminy
|
|
|
How do you treat PVCs
|
Amiodarone
|
|
|
What is the Tx for AV Nodal Reentry Tachycardia
|
Adenosine
|
|
|
Tx for V Tach
|
electrical shock
meds: amiodarone, lidocaine and new is adenosine if not irregular and side complexes. |
|
|
2nd degree type 2 Tx
|
artifical pacing
|
|
|
3rd degree tx
|
external pacing
Atropine Permanent pacing for chronic |
|
|
PVC tx if more than occasional
|
Amiodarone
|
|
|
Tx for V fib
|
Defibrillation (120-200 joules)
CPR Epinephrine 1mg Vasopressin 40mg may insert AICD |
|
|
Cardioversion joules, if narrow then ___
if wide QRD then ______ |
narrow QRS is 50-100 joules
wide QRS is 120-200 joules |
|
|
Tx for Asystole
|
same as V fib but no D Fib!
CPR (using CAB) Epinephrine Vasopressin if it goes on do CPR |
|
|
What is the fusion on a pacemaker
|
fusion is the patient and pacemaker beats together.
|
|
|
PVC tx if more than occasional
|
Amiodarone
|
|
|
Tx for V fib
|
Defibrillation (120-200 joules)
CPR Epinephrine 1mg Vasopressin 40mg may insert AICD |
|
|
Cardioversion joules, if narrow then ___
if wide QRD then ______ |
narrow QRS is 50-100 joules
wide QRS is 120-200 joules |
|
|
Tx for Asystole
|
same as V fib but no D Fib!
CPR (using CAB) Epinephrine Vasopressin if it goes on do CPR |
|
|
What is the fusion on a pacemaker
|
fusion is the patient and pacemaker beats together.
|
|
|
what is AVNRT
|
AV Nodal Reentry Phenomanon
|
|
|
what is catheter ablation therapy used for
|
AVNRT
Recurrent atrial dysrhythmia such as AF VT |

