![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
118 Cards in this Set
- Front
- Back
|
The heart is enclosed in a sac called the ... |
pericardium |
|
|
The right side of the heart pumps blood to the ____, whereas the left side pumps blood to the _______.
|
The right side of the heart pumps blood to the lungs, whereas the left side pumps blood to the body. |
|
|
The top, smaller chambers are called _______ |
atria |
|
|
The lower, larger chambers are called _______ |
ventricles |
|
|
What is arteriosclerosis pathogenesis? |
|
|
|
What is the body's response to arteriosclerosis pathogenesis in order to repair the endothelium lining? |
|
|
|
What is arteriosclerosis?
|
When the plagues of arteriosclerosis pathogenesis deposits in various parts of the body |
|
|
What is peripheral vascular disease? |
a type of arteriosclerosis that results in plague formation in arms and legs
|
|
|
What is coronary heart disease (CHD) or coronary artery disease (CAD)? |
a type for arteriosclerosis that results in plague formation in the heart |
|
|
What is cerebrovascular disease? |
a type of arteriosclerosis that results in plague formation in the vessels of the brain |
|
|
Which lipoprotein is most associated with atherogenesis? |
LDL cholesterol (the "bad" cholesterol) so treatments typically involve lowering the LDL |
|
|
What condition poses the highest risk for an acute myocardiac infarction (AMI)?
|
coronary heart disease (or other forms of atherosclerotic disease, diabetes or multiple risk factors etc.) |
|
|
What are the major independent risk factors for acute myocardiac infarction (AMI)? |
|
|
|
What are other life-habit risk factors for AMI? |
|
|
|
How can the risk for AMI be reduced?
|
|
|
|
What drugs are used to treat patients who are at risk for AMI? |
|
|
|
What is the effect, adverse effect and monitoring levels of statins (HMG-CoA reductase inhibitors)? |
|
|
|
What is the effect, adverse effect and monitoring levels of bile acid sequestrants? |
|
|
|
What is the effect, adverse effect and monitoring levels of nicotinic acid (Niacin)? |
|
|
|
What is the effect, adverse effect and monitoring levels of fibric acids (gemfibrozil and fenofibrate)? |
|
|
|
The concentration of what 3 substances are all good indicators of cardiac risk in the future? |
|
|
|
What is lipoprotein (a)? |
|
|
|
What is hemocysteine? |
|
|
|
Deficiency of what can lead to hyperhomocysteinemia? |
B vitamins |
|
|
Ingestion of what can reduce homocysteine concentrations? |
folate, vitamins B6 and B12 help break down homocysteine concentrations |
|
|
What is homocysteine useful for? |
detect individuals at risk for unexplained premature CAD |
|
|
What is C-reactive protein (hsCRP)? |
|
|
|
Elevated baseline hsCRP are correlated with what? |
higher risk of future cardiovascular morbidity and mortality even in inviduals without hyperlipidemia |
|
|
How should a specimen for hsCRP be collected and analyzed? |
|
|
|
Whati s fibrinogen? |
|
|
|
What is D-dimer? |
|
|
|
What is myeloperoxidase? |
|
|
|
What happens first to the heart muscle when a heart attack occurs? |
|
|
|
What happens on day 4 to the heart muscle when a heart attack occurs? |
|
|
|
What happens between day 4 and 10 to the heart muscle when a heart attack occurs? |
Cardiac rupture most likely to occur as myocardium softens and fibrosis is poorly developed and unable to withstand the pressure of the ventricles as it works to pump the blood which results in the blood entering the pericardial sac causing cardiac tamponade.
|
|
|
What is cardiac tamponade? |
When the blood from the heart leaks and fills the space between the heart and the pericardial sac, there is less room for the heart to function. The pressure outside the heart prevents adequate filling of the chambers. Eventually, the heart will stop beating. |
|
|
What specimens are preferred to assess a patient's condition when they have a heart attack? |
4 serum preferred (heparinized plasma acceptable) specimens collected upon admission, a specimen 2-4 hours later, 6 hrs, 8 hrs, then 12 hrs later. |
|
|
What is creatine kinase? |
|
|
|
What are the 2 types of protein subunits of creatine kinase?
|
muscle (M) brain (B) |
|
|
What are the 3 typical isoenzymes of creatine kinase? |
CK-BB (CK-1) CK-MB (CK-2) CK-MM (CK-3) |
|
|
What are the 2 atypical CK isoenzymes of creatine kinase? |
macro-type 1: CK-1 bound to IgG and CK-3 bound to IgA macro-type 2: CK-Mt from mitochondria |
|
|
CK activity is greatest in what? |
striated muscle, brain and heart |
|
|
The skeletal muscle has the highest concentration of which CK isoenzyme? |
CK-3 |
|
|
The brain has the highest concentration of which CK isoenzyme? |
CK-1 |
|
|
The left ventricle has the highest concentration of which CK isoenzyme? |
CK-3 and CK-2 |
|
|
The heart in general as the highest concentration of which CK isoenzyme? |
CK-2 |
|
|
What is Duchenne's?
|
a skeletal muscle disease where there is increased muscular dystrophy and it affects young boys with females being carriers |
|
|
What clinical symptoms are seen in Duchenne's? |
enzyme activity is highest in infancy and childhood (7-10 yrs of age) and shows a 3-6 fold increase of CK activity |
|
|
What diseases of skeletal muscle are CK levels increase in? |
Duchenne's viral myositis (inflammation of the heart) |
|
|
What conditions would NOT increase CK concentration in the plasma? |
|
|
|
An increase in serum CK-1 indicates what? |
head injury |
|
|
An increase in serum CK-2 indicates what? |
|
|
|
What conditions would cause an increase in CK-3 (but not CK-1)? |
|
|
|
CK may increase in the CSF in what conditions? |
|
|
|
CK increases six-fold in females during what? |
childbirth |
|
|
Gastrointestinal infarction would have an increase in which CK isoenzyme? |
CK-1 |
|
|
What conditions would increase CK-1? |
variety of cancers
|
|
|
What is the specimen requirements for CK? |
serum preferred because plasma containing heparin, EDTA, citrate, or fluoride may produce unpredictable reaction rates but it is still unstable in the serum and lost rapidly during storage |
|
|
CK is inactivated by what? |
bright sunlight |
|
|
Which CK isoenzyme is most unstable and least unstable? |
most unstable: CK-3 least unstable: CK-1 |
|
|
T/F: Hemolyzed specimens are ok for CK testing |
T (slight hemolysis is ok because RBCs contain no CK) |
|
|
Why is severely hemolyzed samples not acceptable for CK testing? |
RBCs contain ATP and G6P which are often substrates for reactions so it may affect the lag phase and side reactions in the assay |
|
|
CK concentration in the serum varies with what? |
|
|
|
How is total CK determined? |
|
|
|
For total CK determination, which reaction has a longer lag phase? |
forward (so the reverse reaction is preferred because it proceeds faster) |
|
|
T/F: Spectrophotometric methods are more sensitive than bioluminescent methods |
false |
|
|
Normal amount of _______ with trace amounts of __________ represents normal turnover of muscle, but _______ is NOT normally present! |
Normal amount of CK-3 with trace amounts of CK-2 represents normal turnover of muscle, but CK-1 is NOT normally present!
|
|
|
An increase of what is most often indicative of damage tot eh myocardium? |
CK-MB |
|
|
Total CK parallels with what, but remains elevated longer? |
CK-MB |
|
|
The immunoassay CK-MB measures what? |
|
|
|
CK-MB2 converts to CK-MB1 by what enzyme? |
lysine carboxypeptidase |
|
|
Normally, concentrations of _______ and _______ are about equal. However, after a heart attack, ______ rises faster than ______ . |
Normally, concentrations of CK-MB2 and CK-MB1 are about equal. However, after a heart attack, CK-MB2 rises faster than CK-MB1. (RATIO IS > 1) |
|
|
The CK-MB2:CK-MB1 ratio begins to rise at what time, peaks at what time and returns to baseline at what time? |
|
|
|
What substance is released when cells are damaged, increased in a wide range of diseases? |
lactate dehydrogenase (LD) |
|
|
LD concentrations are highest where? |
(all cells contain LD but in different concentrations of the isoenzymes) |
|
|
Describe the structure of LD |
It has 2 proteins, heart (H) and muscle (M) that result in 5 isoenzymes: LD1(HHHH): most anionic LD2 (HHHM) LD3 (HHMM) LD4 (HMMM) LD5 (MMMM): most cationic |
|
|
LD preferred specimens |
|
|
|
What inhibits LD in the assay? |
|
|
|
Alkaline pH favors what in the lactate dehydrogenase assay?
|
lactate (pH 9.5) |
|
|
Neutral pH favors what in the lactate dehydrogenase assay? |
pyruvate (pH 7.4) |
|
|
Total levels of limited value in what conditions? |
multiple organs are diseased |
|
|
LD begins to rise at what hours, peaks at and returns to baseline? |
|
|
|
Which LD isoenzyme predominates in heart muscle and RBCs?
|
LD1 (LD2 is high in these tissues too) |
|
|
Which LD isoenzyme predominates in the liver and skeletal muscle? |
LD5 |
|
|
Which LD isoenzyme predominates in varying degrees in all tissues? |
LD2, LD3, and LD$ |
|
|
Which LD isoenzyme predominates in platelets? |
LD3 and LD4 |
|
|
LD isoenzymes can aid in identifying what? |
tissue source of elevated total LD |
|
|
What substance is present in all fluids (plasma, CSF and saliva) except urine (unless there's a kidney lesion)? |
AST |
|
|
What substance is increased in hepatitis and liver disease associated with necrosis? |
AST |
|
|
What is the concentration of AST after AMI? |
|
|
|
Describe a typical AMI enzyme graph timeline |
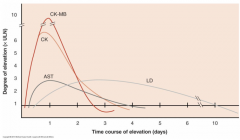
|
|
|
Myoglobin is found in what muscles? |
cytosol of striated muscle: skeletal and cardiac |
|
|
What protein is the first to rise after a heart attack? |
myoglobin (peaks within 6-9 hrs) |
|
|
Myoglobin specimen |
serial samples: on admission, 2-4 hrs later, 6-9 hrs later, and 12-24 hrs later |
|
|
AMI is suspected if myoglobin concentration is.... |
doubled in 1-2 hours |
|
|
What interferes with myoglobin assays? |
hemolysis, bilirubin, lipemia |
|
|
What methodologies are used to measure myoglobin? |
|
|
|
What are troponins? |
|
|
|
What are the 3 subunits of troponin? |
C, I and T |
|
|
Which troponin subunit is the calcium binding component? |
C |
|
|
Which troponin subunit is the inhibitory component? |
I |
|
|
Which troponin subunit that is the tropomyosin binding component? |
T |
|
|
Troponins are released into circulation upon what? |
injury |
|
|
What methodology is used to measure troponin? |
ELISA assays |
|
|
Which troponin is highly specific for cardiac muscle injury? |
cTnI (cardiac troponin I) |
|
|
What is used for diagnosing AMI in patients with conmitant skeletal muscle trauma/disease or monitor graft vs. host disease in heart transplant patients? |
cTnI |
|
|
What is used for risk assessment with acute myocardial ischemia? |
cTnT |
|
|
Following myocardial damage, troponin I in plasma is often found complexed with what? What is the importance of this? |
Troponin I if complexed with troponin C, undergo structural changes that affect the binding of monoclonal antibodies that are used in the assays for detection
|
|
|
Describe the timeline of AMI markers |
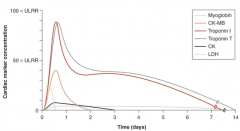
|
|
|
What are some thrombolytic agents? What is used for? |
Streptokinase and urokinase are used to dissolved blood clots and restore blood flow to minimize ischemic injury and cell death but must be administered within 4 hours of onset of symptoms (if given in the 1st hr, there's a 50% reduction in mortality) |
|
|
If reperfusion with thrombolytic agents are successful, what changes are seen? |
|
|
|
What is congestive heart failure? |
failure of the heart to pump sufficiently
|
|
|
If the left side of the heart fails, what happens? |
pressure builds upt owards the lungs and causes pulmonary edema (difficulty breathing) |
|
|
If the right side of the heart fails, what happens? |
pressure builds up towards the body, and causes abdominal, leg and ankle adema |
|
|
What is the marker for congestive heart failure? |
B-type natriuretic peptide (BNP) |
|
|
The cardiac ventricles secret what cardiac neurohormone? |
BNP |
|
|
What does BNP do? |
stimulates urinary excretion of sodium and increase urine flow without affecting GFR, blood pressure, or renal flow |
|
|
Concentrations of BNP increases in what conditions? |
|

