![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
A false cardiac aneurysm (i.e., pseudoaneurysm) is lacking which of the following layers?
a. myocardium and endocardium b. epicardium c. endocardium d. myocardium, epicardium and endocardium e. myocardium |
E. myocardium
When the pericardium rather than myocardium composes the wall of the aneurysm, it is a false aneurysm or pseudoaneurysm. The usual cause is a rupture of the left ventricle into the pericardial space after myocardial infarction. Because of adhesions from previous pericarditis, the pericardium locally attaches to the epicardium which restrains the ventricular blood from extending into the remaining pericardial space and causing tamponade. Cardiac Requisites, 238 |
|
|
A fetal ultrasound shows parallel cardiac outflow tracts. Most likely diagnosis?
a. truncus arteriosus b. Tetralogy of Fallot c. Transposition of great vessels d. total anomalous pulmonary venous return e. normal |
C. Transposition of great vessels
Transposition of the great vessels can only be detected by seeing parallel cardiac outflow tracts. Truncus arteriosus dx is made with echo by demonstrating a large, single great vessel which overrides a large VSD. Tetralogy of Fallot shows a VSD beneath a large overriding aortic root, right ventricular hypertrophy, and often underdeveloped pulmonary artery (due to stenosis). Total anomalous pulmonary venous return has variable findings. Cardiac Requisites 87-91 Primer 130-132 |
|
|
A patient has big atria, enlarged hepatic veins and IVC. Anterior pericardial calcifications are seen on CT. Most likely diagnosis:
a. restrictive cardiomyopathy b. constrictive pericarditis c. Asbestoses d. Uremia |
B. constrictive pericarditis
The pericardium calcifies in 50% of cases of constrictive pericarditis. The pericardium does not calcify in restrictive cardiomyopathy. Constrictive pericarditis is a thickening of the pericardium that restricts diastolic filling of the heart. It can occur after any pericarditis but is frequently ascribed to viral or TB pericarditis, uremia with pericardial effusion, or cardiac surgery. Because of the restriction to right ventricular filling the right atrium, IVC, and hepatic veins are dilated. Hemodynamically, restrictive cardiomyopathy and constrictive pericarditis can appear similar. Asbestosis is lung parenchymal fibrosis with likely calcified pleural plaques. Cardiac Requisites 271-276, 288-290 |
|
|
Alcoholic cardiomyopathy is associated with which of the following?
a. left ventricle diastolic dysfunction b. left ventricle systolic dysfunction c. right ventricle diastolic dysfunction d. decreased right atrial filling |
B. left ventricle systolic dysfunction
Alcohol is one of many causes of dilated cardiomyopathy. In this, systolic function is depressed but diastolic function is nearly normal. Typically the left ventricle is enlarged with global hypokinesis whereas the right ventricle is less dilated and has a less severe contraction abnormality. Mild mitral and tricuspid regurgitation are common. Decreased EF with reduced stroke volume results from this and may have reduced cardiac output. Cardiac Requisites pg 288; Dähnert 5th p. 621 |
|
|
D-transposition of the great vessels is associated with--
a. AV concordance b. AV discordance c. LV connects to aorta d. RV connects to PA |
A. AV concordance
In D-TGA the atria and ventricles are in normal position—AV concordance. In L-TGA there is inversion of the ventricles—AV discordance. Primer, 128 D- transposition – AV concordance, ventriculoarterial discordance (RA RV aorta; LA LV PA); closed loop, requires shunt for viability [VSD in 50%] L- transposition – AV discordance, ventriculoarterial discordance (RA LV PA, LA RV aorta); “corrected” transposition, but 40% 1-yr survival (other defects); high incidence of dextrocardia Req 60-61; Dähnert 5th p. 652. |
|
|
For total anomalous pulmonary venous return, which is true?
a. the heart is enlarged. b. Kerley B lines c. d. e. |
B. Kerley B lines
This recall is incomplete; given that pulmonary edema is associated with some types of TAPVR (e.g., infradiaphragmatic), Kerley B lines is a correct choice. Further, note that both Cardiac TAPVR and infradiaphragmatic TAPVR are associated with a “notably normal” heart size. see Dähnert 5th p. 604. TAPVR = saturated blood from pulmonary veins returns to right side of heart (a closed circuit with no communication to left side of heart; this is incompatible with life without a R-L communication such as ASD). Incidence = 2% of CHD. Types: Type 1, Supradiaphragmatic (52%) – drainage into left brachiocephalic vein / azygous vein Type 2, cardiac (30%) – drainage into coronary sinus; “snowman” heart Type 3, subdiaphragmatic (12%) – drainage into IVC or other vein; unique appearance of pulmonary edema w/ normal sized heart Type 4, mixed – 6% (various sources, old notes, AFIP notes, Primer, Dähnert and Thoracic Requisites) |
|
|
In total anomalous pulmonary venous return, what forms the left/upper side of the “snowman”?
a. pulmonary artery b. pulmonary vein c. right sided aorta d. vertical vein |
D. vertical vein
(TAPVC), a congenital anomaly in which none of the pulmonary veins are connected to the left atrium but instead all drain by various routes into the right atrium. A 'snowman' sign or figure of 8 configuration is seen in the supracardiac type but rarely before 4 months of age. The snowman configuration is due to widening of the superior mediastinum and cardiac silhouette. A right to left shunt is necessary for survival. In type I TAPVR (supracardiac, 55% of all types) the pulmonary veins drain cephalad into a left SVC (aka left vertical vein), into left brachiocephalic vein, then into the SVC. The superior mediastinum is enlarged secondary to dilation of the right vena cava, innominate vein and ascending vertical vein. The vertical vein is to the left-upper aspect of the mediastinum. amershamhealth.com Primer, 130-132 AFIP 2002-2003 Notes, pg 938-939 |
|
|
Ischemia associated with anomalous origin of left coronary artery is associated with which of the following?
a. decreased oxygen content from an anomalous vessel b. steal c. spasm / intermittent flow d. small caliber of the vessel e. abnormal distribution of the LCA |
B. steal
Bland-White-Garland syndrome: anomalous origin of the left coronary artery arising from the pulmonary artery (ALCAPA) is a rare but serious congenital anomaly. Initially, myocardial ischemia is transient, occurring during periods of increased myocardial demands, such as when the infant is feeding and crying. Further increases in myocardial oxygen consumption lead to infarction of the anterolateral left ventricular free wall and/or papillary muscle dysfunction (terminating in CHF). Mechanism: with postnatal fall in pulmonary arterial pressure, perfusion of LCA drops (ischemic left coronary bed) as flow is preferentially directed towards the lower-resistance pulmonary vascular bed (steal); there may be collateral flow from RCA with flow reversal in LCA: - adequate collateral circulation = lifesaving - inadequate collateral circulation = myocardial infarction - large collateral circulation = L-to-R shunt with volume overload of heart. Dähnert 5th p. 603; Emedicine.com * This makes sense from a physiology standpoint, as the mean pressure in the aorta is 70-90 mm Hg, but that in the PA is 15-20 mm Hg—a huge difference in perfusion pressure. [Update—7/01/03: Primer 3rd p. 145 lists “venous blood” as the mechanism. This is incorrect, as the pressure differential will allow little (if any) venous blood to enter the coronary circulation.]. |
|
|
What artery supplies the A-V node?
a. branch of the proximal RCA b. branch of the distal RCA c. conus branch of the RCA d. branch on the LCA e. brach of the left circumflex |
B. branch of the distal RCA
Arterioventricular nodal artery supplied by a distal branch from the RCA 90% of the time. The Conus artery is the first branch of the RCA. The SA node is supplied by a proximal RCA branch 40-55% of the time. Primer, 111 |
|
|
Old man with symptoms of aortic dissection (back pain). Blood pressure of 130/80. What do you do?
a. Angiography b. Non-contrast enhanced CT c. MR d. US |
A. angiography
If concerned with aortic dissection angiography is utilized to establish a dx, visualize the proximal and distal extent of a dissection, and identify serious complications. Contast-enhanced CT could also be useful, especially CT angiography. MR could be useful but is not a first line method to evaluate for dissection. Echocardiography can not image the aortic arch completely. Cardiac Requisites 391-393 ** This may be a “spin” on the AAA question from this same year; however, as stated [dissection], contrast is absolutely essential for visualizing the false-lumen. ** |
|
|
What causes the interventricular septum to rotate clockwise on the MRI transverse view?
a. aortic stenosis b. pulmonary arterial hypertension c. d. |
B. pulmonary arterial hypertension
Increase in right ventricular afterload (caused by pulmonary arterial htn) results in hypertrophic myocardium which results in right ventricular htn. The normal convexity of the interventricular septum towards the right ventricular cavity is straightened or even reversed so that the septum bows toward the LV cavity. Cardiac Requisites, pg 112 (picture on 117, image 3-15). |
|
|
What is the most common cardiac manifestation of Systemic Lupus Erythematous?
a. coronary artery disease b. myocarditis c. valvular pathology d. pericarditis |
D. pericarditis
Incidence of pericarditis in SLE has been reported1,2 from 50-70%. Nonbacterial thrombotic endocarditis (Libman-Sacks endocarditis) has vegetations that are considerably smaller than those in bacterial endocarditis and frequently occur beneath the cusps. Mean incidence reported3 as 43%. The ACR syllabus2 calls these lesions the “most characteristic” of SLE in the heart. 1Harrison’s 14th p. 1344; 2ACR 4th Chest Syllabus p. 242; 3Doherty: Am. Heart J. 1985 Dec;110(6) p. 1257. Cardiac Requisites, 286. |
|
|
Which is true of coronary artery bypass?
a. ostial markers are not needed if the native vessels are completely occluded. b. in repairing VSD's, the patches are on the low pressure RV side. c. The Jantene or switch procedure involves switching the venous inflow to the atria. d. |
B. in repairing VSD’s, the patches are on the low pressure RV side
40% of VSD require surgery for repair. They can be repaired using suture or placement of a patch. Either way, the RV is the one opened. Ventricular Septal Defect: Effects, Assessment & Treatment on askjeeves.com.; Dähnert 5th p. 656. Jantene procedure is a repair for D-TGA. In it the ascending aorta and pulmonary arteries are divided above the sinus of Vasalva and the coronary arteries excised from the aorta. The coronary arteries are replanted in the new aortic root, which is connected to the left ventricle. The pulmonary artery bifurcation is brought anterior and anastomosed to the right ventricular sinuses. Cardiac Requisites, 324 |
|
|
Which is true regarding left atrial myxomas?
a. Most commonly arises from mitral valve b. Mimics ASD c. Mimics mitral stenosis d. Mimics aortic stenosis |
C. mimics mitral stenosis
Primary tumors of the heart are rare, but the most common is the myxoma (25% of heart tumors), typically arising in the left atrium from the interatrial septum. 75% occur in the left atrium, remainder in the RA, very few occur in the ventricles. They occur more commonly in women. Interference with function by the tumor mimics symptoms and signs of valvular dysfunction due to rheumatic disease. Thus, left atrial myxomas may cause pulmonary congestion and signs of mitral stenosis (eg, the typical murmur, an opening snap, an accentuated first heart sound). Murmurs of mitral insufficiency may also result from chronic damage to the valve leaflets or to the tumor's interference with proper closure. Cardiac Requisites 280, Merck Manual, Benign Cardiac Tumors (via askjeeves.com) |
|
|
Which MRI sequence best evaluates blood flow when imaging the heart?
a. gradient echo b. spin echo c. Phase contrast d. |
A. Gradient echo
Flow-related enhancement occurs in both spin-echo and gradient reversal sequences; however, it is more prominent on gradient-reversal sequences. Cardiac Requisites 103 |
|
|
Which of the following increases the ejection fraction?
a. aortic insufficiency b. idiopathic hypertropic cardiomyopathy c. d. |
B. idiopathic hypertropic cardiomyopathy
Hypertrophic cardiomyopathy tends to be associated with a hyperdynamic heart with ejection fractions above 60-65%. Ejection fraction is often not reduced in aortic insufficiency, but is not elevated. Headdocs.com, Hypertrophic Cardiomyopathy |
|
|
Which of the following is associated with anterior motion of the anterior leaflet of the mitral valve?
a. Mitral valve prolapse b. Papillary muscle dysfunction c. Hypertrophic cardiomyopathy d. mitral valve stenosis |
C. Hypertrophic cariomyopathy
Hypertrophic cardiomyopathy often leads to Systolic Anterior Motion (SAM) of the anterior leaflet of the mitral valve. This is movement of the anterior leaflet of the mitral valve into the outflow region in systole, causing an increasing stenosis. This abnormal motion of the mitral valve increases throughout systole and frequently causes the valve to touch the ventricular septum, creating an occlusion of the outflow from the left ventricle. SAM is variable. Cardiac Imaging Requisites, pg 291; Dähnert 5th p. 622. |
|
|
Which of the following is false regarding cardiac transplants?
a. rejection rate is the same for orthotopic and heterotopic transplants b. angina is uncommon c. the heart rate after transplant is slower than the native heart rate d. |
C. the heart rate after transplant is slower than the native heart rate
When the heart is removed from the body, the nervous system is disconnected and cannot be re-attached. The heart continues to beat adequately, but without an external nervous supply. The denervated heart beats faster at rest, but its rate does not rise as quickly with exercise. In addition, patients usually do not experience angina.. Orthotopic heart transplant: This is the procedure of choice for most patients, with the donor heart replacing the recipient's, and taking the correct position in the thorax. It is the most reliable and effective type of cardiac transplant, and accounts for almost 99% of such procedures. Heterotopic heart transplant: This procedure is also known as "piggy-back" heart transplantaion, as it leaves the recipient's heart intact to work in series with the donor heart. Rare--accounts for only 1% of procedures. Originally it was used when there was a moderately elevated pulmonary vascular resistance, and also in urgent cases when the donor heart is under-sized. Askjeeves.com and Heart1.com, multiple articles |
|
|
Which of the following is most commonly associated with aortic stenosis?
a. Angina b. Aortic nipple c. Enlarged left ventricle d. Dilatation of aorta |
C. Enlarged left ventricle
LVH is commonly associated with aortic stenosis. Poststenotic dilatation of the aorta is only present in valvular AS. Aortic valve calcification occurs in all types of AS after age 40 if severe. Types of AS: Subvalvular, Valvular (most common, bicuspid aortic valve most common congenital anomaly causing), Supravalvular. Cardiac Requisites, 149-162 Primer 123 |
|
|
Which of the following is true regarding calcification of the mitral annulus?
a. more common in men b. associated with aortic stenosis c. d. |
B. associated with aortic stenosis
Mitral annulus calcifications are more common in the elderly and in women. It usually has little clinical significance although in extreme cases can cause mitral regurg and stenosis or grow posteriorly into the ventricular wall causing heart block. Aortic stenosis and htn have a higher incidence of mitral annulus calcification. Mitral annular calcification differs from mitral valve calcification, which is often caused by rheumatic valvular dz. Cardiac Requisites, 17 |
|
|
Which of the following most commonly metastasizes to the heart?
a. Melanoma b. Breast c. Lymphoma d. Bronchogenic CA e. colon |
D. Bronchogenic CA
Metastatic tumors to the heart and pericardium are 20 to 40 times more frequent than primary heart tumors. Melanoma, leukemia, and malignant lymphoma are the tumors that more frequently metastasize to the heart. Because of their adjacent location, lung and breast tumors frequently go to the pericardium during the terminal stage of the dz. In order of decreasing frequency: lung, breast, melanoma, lymphoma/leukemia. Cardiac Requisites, pg 278-279 and Metastatic Tumor of the Heart, from www.rbrs.com |
|
|
Which of the following requires a PDA for life?
a. D-transposition of the great vessels b. Hypoplastic left ventricle c. AP window d. Tetralogy of Fallot e. Truncus, Type II |
B. Hypoplastic left ventricle
Hypoplastic left heart is a spectrum of cardiac anomalies characterized by underdevelopment of the LA, LV, MV, aortic valve, and aorta. Survival requires a large ASD and PDA with R-L and L-R shunting. Complete Transposition of the Great Arteries (D-TGA) is when there are two independent circulations, from body to body via the RV and from lung to Lung via the LV. It is incompatible with life unless there are associated anomalies that permit mixing of the two circulations (eg, ASD, VSD, PDA). Aorticopulmonary window have plain film findings identical to PDA; PDA associated 10-15%. Tetralogy of Falot and Truncus have a VSD. Primer of Diagnostic Imaging, 3rd Edition pg 125-129, 138 |
|
|
A child who has had a bone marrow transplant has a 3 cm upper lobe nodule. Most likely diagnosis:
a. CMV b. Invasive Aspergillus c. TB d. lymphoma e. mycoplasma |
B. Invasive Aspergillus
Given the Hx of bone marrow transplant (BMT), the child is presumably immunocompromised. Invasive Aspergillosis is then a concern, and findings include single / multiple ill-defined peripheral opacities 1-3cm in size (possibly with a halo of ground glass on CT). Time course is 2-3 weeks (neutropenic phase)—high mortality (70-90%) Dähnert 5th p. 458, 462. CMV pneumonia would certainly be a possibility, given the Hx, however it is characterized by multiple small nodules. Time course is 1st 100 days post transplantation. Late phase pulmonary complications include BOOP, chronic GVHD, and infections (in patients > 100 days post BMT). Mycoplasma favors the lower lobes and is typically not nodular. Radiology Review Manual, 1999. p.385 |
|
|
A dilated aortic knob is associated with
a. aortic valve stenosis b. left ventricular dilatation c. d. e. |
A. aortic valve stenosis
Poststenotic dilatation of ascending aorta (in 90% of acquired, in 70% of congenital AS). It is thought that the jet of blood leaving the stenotic valve causes the aortic dilatation. Dähnert 5th p. 613 |
|

A female has leg pain, glucose of 20, fatigue and a well-defined chest mass. Most likely diagnosis:
a. bronchogenic carcinoma b. lymphoma c. localized fibrous tumor of pleura d. Large cell lung CA e. Pulmonary blastoma |
Localized fibrous tumor of the pleura (LFTP) is a benign mesothelioma (no association with asbestos exposure). It is largely resectable, even when the size is large, and has a favorable prognosis. Episodic hypoglycemia is seen in 4%; hypertrophic pulmonary osteoarthropathy [pain / swelling of limbs, especially tibia / fibula] in 20-35%. Other Sx include dyspnea and cough. Dähnert 5th p. 504, 104
Bronchogenic CA is more common than LFTP, and causes 88% of cases of hypertrophic pulmonary osteoarthropathy. However, it typically does not cause hypoglycemia (other paraneoplastic syndromes, e.g. SIADH, however), and the well-defined chest mass favors a benign tumor. www.emedicine.com |
|
|
An elderly lady with shortness of breath and cough has bronchiectasis in the right middle lobe and lingula. Most likely cause:
a. drug adverse effect b. cancer c. pulmonary fibrosis d. mycobacterium avium-intracellulare (MAC) e. pulmonary embolism f. missed diagnosis of cystic fibrosis |
D. mycobacterium avium-intracellulare (MAC)
This is the “Lady Windermere Syndrome”, caused by atypical mycobacteria. It is thought that suppression of the cough reflex in a “lady” leads to aspiration of secretions, which favors the growth of MAC. See Harrison's 14th ed., 1998, p. 1022 MAC lung disease occurring in older women who are usually nonsmokers without evidence of COPD is noncavitary and is associated with bronchiectasis. The findings are those of cylindrical bronchiectasis associated with multiple small but focal lung nodules usually measuring approximately 5 mm in diameter. Any lobe may be involved, but the lingual and middle lobe have the highest prevalence. Thor. Req. p. 122. Obviously, MAC also affects immunocompromised (HIV) patients and males who are heavy smokers, but the presentation is somewhat different (e.g., cavitary lesions). The other answers do not selectively affect the RML / lingual. CF patients rarely live past their early 40’s. |
|
|
An elderly man has facial and upper extremity swelling with a widened mediastinum on chest x-ray. Most likely diagnosis:
a. teratoma b. bronchogenic ca c. mediastinitis d. lymphoma |
B. Bronchogenic Carcinoma
The clinical description points to SVC syndrome. Mediastinal widening is seen in 64%, head & neck edema in 70%. Greater than 50% of all cases of SVC syndrome are caused by bronchogenic carcinoma. Lymphoma is the next most common cause, however, there is no mention of lymphadenopathy. see Dähnert 5th p. 648 The most common benign causes (only 10% to 20% collectively) of SVC syndrome are granulomatous mediastinitis and post-iatrogenic manipulation (long-dwelling lines, etc.). Between TB and Histoplasmosis, Histoplasmosis more classically results in mediastinal fibrosis and also results in more fulminant lymphadenopathy than TB. Histo is also not an opportunistic infection, and would therefore reasonably be seen more frequently. (Radiology Review Manual, p. 538.) |
|
|
Best way to measure COPD emphysema:
a. FVC b. FEV1 c. FEV1/FVC d. VC e. RV |
B. FEV1
A simple staging system based on FEV1 has been proposed for COPD (American Thoracic Society) - Stage I is an FEV1 50% or more of the predicted value. The patients generally have mild exercise limitation because of COPD and are at low risk of serious exacerbations. - Stage II is an FEV1less than 50% but greater than 35% of the predicted value. Stage III is an FEV135% or less of the predicted value. The exercise capacity of patients with - Stage III COPD is severely limited. These patients tend to have frequent exacerbations and consume the greatest expenditure of health care dollars for care among persons with COPD. MKSAP (medicine disc) Chronic air-flow obstruction (decrease FEV, DL, increased TLC, RV). The air-flow obstruction can be measured with pulmonary function tests by a diminution of the forced expeiratory volume in one second (FEV) or the ratio of the FEV to the forced vital capacity (FVC). Thoracic Requisites (289-90), Primer 48; B&H p. 451 |
|
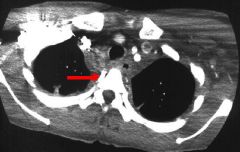
Diagram of axial CT slice through superior mediastinum above aortic arch. Tubular structure labeled on right/anterior aspect of vertebral body. What is it?
a. azygous vein b. hemiazygous vein c. aberrant subclavian d. paraspinal vessel e. superior right intercostal vein |
E. Superior right intercostal vein
The right superior intercostal vein lies along the spine superior to and draining into the arch of the azygos vein. It is above the arch of the aorta. Netter, old notes; http://www.uhrad.com/ctarc/ct116.htm The azygos vein arches under the right mainstem bronchus into the SVC. This is about the level of the inferior part of the aortic arch. * Be aware that there is a variant of this question that shows a CT cut at the level of the heart and great vessels; in this case (below intercostals), the correct answer would be azygous vein. |
|
|
For which of the following is CT densitometry most useful?
a. PCP b. asbestosis c. silicosis d. lipoid pneumonia e. alveolar proteinosis |
D. Lipoid Pneumonia
Lipoid pneumonia may show a mass of low-attenuation approaching that of subcutaneous fat (-150 to 50 HU). When seen, this is very specific. Acute Exogenous lipoid pneumonia – “fire-eater pneumonia” - ingestion of liquid paraffin or petroleum [poisoning in children or accidental ingestion by “fire eaters”] Chronic Exogenous lipoid pneumonia: - aspiration or inhalation of fatlike material (vegetable oil, cod liver oil, mineral oil) - in elderly, debilitated, those with neuromuscular disease - predilection for RML and lower lobes Endogenous phospholipoidosis induced by amiodarone is an important cause of pulmonary toxicity. Thoracic Radiology the Requisites page 274-5; Dähnert 5th p. 400, 499 |
|
|
In patient with COPD, what is the most common cause of heart failure?
a. Pulmonary hypertension (Cor pulmonale) b. atherosclerotic heart disease c. d. e. |
B. Atherosclerotic heart disease
Cardiac disease in patients with chronic pulmonary disease is usually caused by coronary artery disease, especially in older patients with a history of smoking. Coronary artery disease leads to CHF (LHF) superimposed on the chronic lung disease. Right heart failure is much less common than left heart failure (LHF) and is most commonly caused by LHF. Other causes include increased pulmonary arterial pressure – pulmonary stenosis, tricuspid regurgitation, right ventricular infarction, and volume overload from septal defect. Conclusion: The most common cause of heart failure in a patient with chronic lung disease is atherosclerotic disease (of coronary arteries). Freundlich 2nd p. 354 |
|
|
IV drug abuser with fever, chest pain, and multiple focal areas in lungs bilaterally. Which is most likely?
a. TB b. Staph. c. Endocarditis d. |
C. Endocarditis
IV drug abusers get endocarditis of the tricuspid valve (right-sided endocarditis), which causes multiple septic pulmonary emboli. Mortality rate is only 3%-9%, lower than left-sided [aortic valve] endocarditis. Dähnert 5th p. 616 Septic emboli are trapped in the pulmonary circulation. Consequently, patients typically present with cough and pleuritic chest pain. Chest radiographs typically show multiple round pulmonary infiltrates that may cavitate. Systemic complications are uncommon unless the mitral valve or the aortic valve has become secondarily involved. MKSAP (medicine disk) |
|
|
Most common lung infection in HIV:
a. Aspergilllus b. Cryptococcus c. PCP d. TB e. bacterial pneumonia |
C. PCP
Opportunistic infection accounts for the majority of pulmonary disease in HIV: - PCP (60-80%): bilateral interstitial disease (ground-glass opacities), 25% fatal; CD4 count usually < 200; frequently associated with pneumatoceles - Fungal Disease e.g., Cryptococcus or Aspergillus (2-15%) - Mycobacterial 20% - Bacterial (staph, strep, H. Flue, nocardia) 5-30% Dähnert 5th p. 452 |
|
|
On an axial CT image which takeoff to the RLL do you see at the same level as the bronchus to the RML?
a. Superior b. Medial Basal c. Lateral Basal d. Anterior Basal e. Posterior Basal |
A. Superior
At the level of the right middle lobe bronchus many structures are seen. The superior segment of the right lower lobe, the right middle lobe lateral and medial branches, the right and left superior veins and the left lower lobe. See Figure in Dähnert 5th p. 444 or Freundlich 2nd Fig. 3-20. The remainder of the answers are segments of the right lower lobe. The medial basal, posterior basal, and lateral basal arise clearly at the level of the lower lobe bronchi. |
|
|
Patient has right upper lobe mass with ipsilateral paratracheal node mets. Proper staging includes:
a. NX b. N0 c. N1 d. N2 e. M1 |
D. N2
Paratracheal is mediastinal – ipsilateral is N2 (see below) Primary Tumor: TX – malignant cells in secretions, T0 – No tumor, T1S – ca in situ, T1 – 3 cm or less without invasion, T2 - 3cm or more or local invasion, associated atelectasis, or pneumonitis, T3 – direct extension to chest wall, T4 – invasion of mediastinum Nodal Involvement: N0 – no mets to nodes, N1 – Mets to peribronchial or ipsihilar nodes, N2 – Mets to ipsilateral mediastinal and carinal, N3 – Mets to contralateral mediastinal or hilar nodes Distant Metastasis: M0 – no distant mets, M1 – distant mets present Stage I = T1 or T2, N0, M0; Stage II = T1 or T2, N1, M0; Stage IIIA = T3, N2, M0. (all potentially resectable) Stage IIIB (T4, any N, M0 or any T, N3, M0) or stage IV (any T, any N, M1) disease are usually unresectable. Dähnert 5th p. 469; Armstrong 2nd p. 285. |
|
|
Pleural effusion is not commonly seen with
a. lymphangiectic carcinomatosis b. lymphoma c. lupus d. usual interstitial penumonitis (UIP) e. |
D. usual interstitial pneumonitis (UIP)
UIP is the same as idiopathic pulmonary fibrosis and cryptogenic fibrosing alveolitis. It is the commonest form of idiopathic interstitial pneumonia (90%). Idiopathic (50%), familial (25%), associated with collagen vascular disease (20-30%). Clinical: progressive dyspnea, dry cough, fatigue over 1-3 yrs; clubbing of the fingers (83%); poor prognosis—45% 5-year mortality. Radiologically: bilateral diffuse linear / small irregular reticulations - honeycombing (74%), reticulonodular pattern - pleural effusion in only 4-6% HRCT: simultaneous early & late fibrosis (Hallmark finding); subpleural honeycombing Dähnert 5th p. 496. Lymphangiectic carcinomatosis (effusion “common”); lymphoma (effusion in 10-28%, in 2/3 chylothorax); SLE (15-74%)—most common collagenosis to give pleural effusion. Dähnert 5th p. 438-439; Freundlich p. 569 |
|
|
Which of the following avidly enhances in mediastinum?
a. Paraganglioma b. lymphoma c. thymoma d. |
A. Paraganglioma
Paragangliomas are tumors of the paraganglionic cells and in the chest are chemodectomas or functioning paragangliomas. Chemodectomas are aortic body tumors and are seen as masses of the aortopulmonary window. Functioning paragangliomas occur rarely in the chest and mostly in the posterior mediastinum. These masses are usually extremely vascular and enhance brightly at enhanced CT. At MRI they may show high signal intensity on T2 wieghted images. www.galter.northwestern.edu “Exhuberant enhancement”—Dähnert 5th p. 529 Masses that are known to possibly strongly enhance at CT are: goiters, vascular tumors (hemangiomas), parathyroid masses, castelman disease, medullary cancer of the thyroid, thymic carcinoid, and metastasis of sarcomas and melanomas. |
|
|
Which of the following does not run with or contain lymphatics?
a. Bronchial artery b. bronchial vein c. alveolar wall d. pulmonary artery e. interlobular septa |
C. Alveolar wall
Pulmonary lymphatics are seen in all of the following locations except alveolar walls. There are two lymphatic plexuses that drain the lung: superficial and deep. The superficial lymphatic plexus lies deep to the viceral pleura and lymph vessels from it drain into the bronchopulmonary lymph nodes in the hilum. The deep plexus is located in the submucosa of the bronchi and in the peribronchial connective tissue. There are no lymph vessels in the walls of the alveoli. Lymph vessels from the deep plexus drain into the pulmonary lymph nodes, located along the large branches of the bronchi. Lymph vessesls from these nodes follow the bronchi and pulmonary vessels to the hilum, where they drain into the bronchopulmonary lymph nodes. Clinically Oriented Anatomy by Moore, Keith |
|
|
Which of the following has similar histology as UIP (usual interstitial pneumonia)?
a. LAM b. Histiocytosis X c. Sarcoid d. lymphoma e. Lupus |
E. Systemic Lupus Erythmatosus
Multisystem disorder, Surgical biopsy nonspecific, indistinguishable from UIP/IPF. (www.ssharma.com/residents). One histology website that said lupus. Polymyositis/dermatomyositis was also listed as indistinguishable. “Usual interstitial pneumonia (UIP) is a distinct histological lesion that is observed in idiopathic pulmonary fibrosis (IPF),[1,2] but can also be observed in various etiologies (e.g., collagen vascular diseases…)” http://www.medscape.com/viewarticle/410887 |
|
|
Which of the following is characteristic of smoking related emphysema?
a. Basilar predominance b. Centrilobular distribution c. Panlobular distribution d. |
B. Centrilobular Distribution
There are four major types of emphysema defined anatomically. These are: 1. Centrilobular or centriacinar; 2. panlobular or panacinar; 3. paraseptal (distal acinar) emphysema; and 4. paracicatricial (irregular). Centrilobular emphysema affects the predominately the respiratory bronchioles in the central portion of the secondary pulmonary lobule. It usually identified in the upper-lung zones, and it is associated with cigarette smoking (causes up to 50%). Panlobular involves all the components of the acinus an therefore involves the entire lobule. It is classically associated with alpha-1 protease inhibitor (alpha-1-antitrypsin) deficiency (cause in 10-15%), although it may be seen without protease deficiency in smokers and eldely. Paraseptal involves the distal part of the secondary lobule (alveolar dusts and sacs). It can be an isolated phenomenon in young adults, and is associated with spontaneous pneumothorax. (Thoracic Requisites 288, Dähnert 5th p. 485) |
|
|
Which of the following is false regarding pulmonary embolism?
a. infarcts not very common with PE b. distal emboli are more likely to cause infarcts c. rare from upper extremity d. the clinical triad of cough, chest pain, and hemoptysis is present in a majority of patients with angiographically proven emboli |
D. the clinical triad of cough, chest pain, and hemoptysis is present in a majority of patients with angiographically proven emboli * Common Repeater *
PTE Sx: cough (53%), pleuritic chest pain (88%), hemoptysis (30%). So obviously, patients who have all three of these symptoms will be < 30% [14% if these are independent variables]. Other Sx—dyspnea (84%), apprehension (59%), ↑ RR (92%). Infarcts occur in 10-60%; source is DVT of lower extremity / pelvis in > 90%; distal emboli produce infarcts mainly due to the lack of collateral flow Dähnert 5th p. 516 |
|
|
Which of the following is false regarding subcarinal lymph nodes?
a. Can easily be differentiated from bronchogenic cyst on CT b. Involvement does not preclude surgical resection of primary lung cancer c. Easily accessible by mediastinoscopy d. Can posteriorly displace the left mainstem bronchus |
** This question was recalled 3 different ways in 3 recall sets from 2002. Therefore, the following discussion is meant as a guide **
Brohchogenic cysts typically arise in the mediastinum (80-90%), and in the vicinity of the carina (52%). If it is a thin-walled cyst of water density (0-10 HU), then CT is diagnostic. However, 40-50% are of higher density, making differentiation from a node or soft tissue mass difficult / impossible. Biopsy may then be necessary. Dähnert 5th p. 470; Primer 3rd p. 80. Anterior subcarinal nodes can be easily reached via mediastinoscopy (B&H p. 394); but, the other subcarinal nodes cannot. http://www.moffitt.usf.edu/pubs/ccj/v8n4/pdf/311.pdf Involvement of subcarinal nodes would be N2 (= Stage IIIA), which could be resectable (depending on T and M). Dähnert 5th p. 469 Subcarinal nodes extend inferior to the margins of the main bronchi, but may be present anterior and posterior to the carina; it is therefore plausible they could posteriorly displace the left mainstem bronchus. Freundlich 2nd 142. |
|
|
Which of the following is false regarding traumatic rupture of a bronchus?
? a. distal more involved than proximal b. pneumomediastinum R/L pneumothorax c. prompt / easy re-expansion with chest tube d. commonly see pneumomediastinum and pneumothorax |
A. distal more involved than proximal
The above statement is False (a correct choice)-- ”The fractures usually involve the proximal main bronchi (80%) or distal trachea (15%) within 2 cm of the tracheal carina; the peripheral bronchi are involved in 5% of cases.” B&H p. 444. C. prompt / easy re-expansion with a chest tube The above statement is also False (a correct choice). If anything, a bronchial fracture will show inadequate reexpansion of lung despite adequate placement of one or more chest tubes (due to the large size of the air leak). Basically, the chest tubes can’t keep up. Dähnert 5th p. 488. Pneumothorax is seen in 70%, Fx of 1st 3 ribs (53-91%). Pneumomediastinum may be the only finding, particularly with injury to the left main stem bronchus, which has a longer mediastinal course. The fallen lung sign occurs with complete disruption of the main stem bronchus. The lung falls inferiorly and laterally to the base of the hemithorax in contrast to a pneumothroax from a partial bronchial tear, where the lung collapses medially and centrally. Thoracic Requisites 179 ** Clearly this recall is not entirely accurate, as both choices A and C are viable answers. ** |
|
|
Which of the following is most likely to cause an exudative pleural effusion?
a. cirrhosis b. congestive heart failure c. neoplasm d. nephrotic syndrome e. Uremia |
C. Neoplasm
Exudative effusion = high-protein pleural fluid - Malignancy (e.g., pleural mets.): 60% - Uremic pleuritis: 20% - Infection: Empyema, TB, pneumonia - other: SLE, Wegeners (50%), trauma, Meigs, pancreatitis, etc. Transudative effusion = low-protein [1.5-2.5 g/dL] pleural fluid - CHF (increased hydrostatic pressure) - cirrhosis (low osmotic pressure) - nephrotic syndrome (low osmotic pressure) - hypothyroid, constrictive pericarditis, overhydration Dähnert 5th p. 438. |
|
|
Which of the following is most likely to cause round atelectasis?
a. resolving pleural effusion b. resolving pneumonia c. d. |
A. Resolving pleural effusion
A type of focal atelectasis is rounded atelectasis. This type of atelectasis (which is often an incidental finding on chest radiograph) is a peripheral rounded type of atelectasis that is always associated with pleural thickening or less commonly, pleural effusion. It appears as a sharply defined mass abutting the pleura and ranging in size from 2 to 7 cm in diameter usually located posteriorly in the lower lobes. Air bronchograms or focal collections of air (“psuedocavitation”) may be present within the atelectasis. The most distinctive finding is that vessels and bronchi located more centrally than the peripheral area of atelectasis are crowded together in a “whorled” pattern coursing like a “comet tail” toward the hilum. On CT the finding is that of a rounded peripheral lung mass associated with pleural thickening. The comet-tail appearance is more easily visualized. Rounded atelectasis can be associated with any cause of pleural thickening but particularly with asbestos-related disease. Thoracic Radiology Requisites p. 45; Freundlich 2nd p. 105 |
|
|
Which of the following is not typical chest finding of Rheumatoid arthritis?
a. honeycombing b. pleural effusion c. lower lobe interstitial disease d. nodules e. hilar adenopathy |
E. Hilar adenopathy
There are five pleuropulmonary abnormalities associated with rheumatoid disease: 1. pleurisy with or without effusion 2. diffuse interstitial pneumonitis or fibrosis (lower lobe predominance) 3. pumonary (necrobiotic) nodules, often cavitate 4. Caplan’s syndrome (pneumoconiotic nodules) 5. Pulmonary hypertension secondary to vasculitis Thoracic Requisites 252; Dähnert 5th p. 434. Felson gives a good summary but says hilar adenopathy is sometimes seen: The interstitial fibrosis seen with rheumatoid arthritis has no specific histologic or roentgen features. Honey combing is frequent. Pleural effusion or hilar adenopathy may be present. Occasionally the diffuse pulmonary process may be preceded by basilar alveolar infiltrates. |
|
|
Which of the following is true regarding lateral chest x-rays?
a. the anterior wall of the bronchus intermedius is usually seen b. the confluence of the pulmonary venous system is lower than both the right and left upper lobe bronchi c. the right upper lobe bronchus is more often seen than the left upper bronchus d. left PA is inferior to the left mainstem bronchus |
B. Confluence of the pulmonary venous system is lower than both the right and left upper lobe bronchi.
This is a true statement (therefore the answer); Netter 194 shows the relationship clearly. If you’re less visual, you can read about it in Fraser & Pare Synopsis 2nd p. 35-39. Other choices are False-- The posterior (not anterior) wall of the bronchus intermedius is usually seen in 95% of individuals—this is the intermediate stem line. F&P 2nd p. 33; Primer 3rd p. 3 The left (not right) upper lobe bronchus is more commonly seen. LUL bronchus seen in 75%, RUL in only 50%. because-- ”The orifice of the RUL bronchus is seldom as well circumscribed as that of the left… [because] the latter is completely surrounded by vessels (left PA above, interlobar artery behind, pulmonary vein in front). Fraser & Pare synopsis 2nd p. 33. The left mainstem bronchus enters the lung below (not above) the left pulmonary artery (hyparterial). Felson p. 187. |

