![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
97 Cards in this Set
- Front
- Back
|
List four (4) indications for electroencephalographic monitoring during anesthesia.
|
› (1) carotid endarterectomy (perfusion jeopardized during cross-clamping of the carotid artery)
› (2) cardiopulmonary bypass procedures › (3) cerebrovascular surgery, for example, temporary clipping during aneurysm surgery or vascular bypass procedures › (4) when burst suppression is desirable for cerebral protection. |
|
|
List two (2) indications for electroencephalographic monitoring in the intensive care unit.
|
• In the intensive care unit, EEG monitoring is indicated (1) for barbiturate coma for patients with traumatic brain injury, and (2) when subclinical seizures are suspected.
|
|
|
Electroencephalogram (EEG) waves are categorized as alpha, beta, delta, and theta, based upon frequency and amplitude. Give the frequency range (in Hz) of each of these EEG waveforms and the brain region(s) from which each is recorded.
|
• Delta waves are the lowest frequency (0-4 Hz), greatest amplitude waves in the electroencephalogram (EEG).
• Theta waves range from 4 to 7 Hz and exhibit a slightly lower amplitude than delta waves. • Alpha waves are typically recorded over the posterior aspect of the head during awake, alert, but relaxed activities. Alpha waves have an intermediate amplitude--less than delta and theta, but greater than beta waves--and a frequency range of 8-12 Hz. • Finally, beta waves are the highest frequency (> 12 Hz), lowest amplitude waveforms and are recorded predominantly over the frontal areas of the head, but can be seen from all brain regions. |
|
|
Briefly describe the typical brain activities associated with each electroencephalogram(EEG) waveform. Reminder: the waveforms are delta, theta, alpha, and beta.
|
• Delta waves (0-4 Hz) are seen in the sleeping adult, but are considered abnormal in the awake adult. Delta waves are also seen in encephalopathy, deep coma, and deep anesthesia.
• Theta waves (4-7 Hz) are seen in sleep and in deep anesthesia. • Prominent alpha wave activity is characteristic of awake, alert, but relaxed activities. An "eyes closed" resting alpha pattern is the baseline awake pattern used when anesthetic effects on the EEG are described. • Beta waves (> 12 Hz) are characteristic of aroused, attentive, active thinking. |
|
|
What happens to the electroencephalography (EEG) waveforms as anesthetic depth increases?
|
• Increasing depth of anesthesia from the awake state is characterized by increased amplitude and synchrony in the EEG waveforms.
|
|
|
As anesthetic depth increases, periods of electrical silence occupy greater proportions of the electroencephalogram (EEG). Give a synonym for "electric silence" in the EEG.
|
• A period of electrical silence in an EEG is called an isoelectric EEG pattern.
|
|
|
What MAC correlates with an isoelectric EEG pattern?
|
• An isoelectric pattern dominates the EEG in the range of 1.5 to 2.0 MAC.
|
|
|
During certain surgical procedures, maximal suppression of cerebral metabolic rate is desirable to protect the brain during an ischemic insult. Under such circumstances, the anesthetic agent can be titrated against the EEG until the desired effect is achieved. Typically, instead of an isoelectric EEG, the goal is a state called burst suppression. Characterize "burst suppression on the electroencephalogram (EEG).
|
• Electroencephalogram (EEG) burst suppression is characterized by periods of isoelectric EEG punctuated by "bursts" of EEG activity. The "burst" is high-frequency activity and the "suppression" is 0.5- to several-second periods of isoelectric activity.
|
|
|
The electroencephalogram (EEG) is occasionally used during cerebrovascular surgery to confirm adequate cerebral oxygenation. Identify four conditions or agents that can produce EEG changes mimicking cerebral ischemia.
|
• The electroencephalogram (EEG) changes that accompany cerebral ischemia can be mimicked by
› (1) hypothermia › (2) electrolyte disturbances › (3) marked hypocapnia › (4) anesthetic agents |
|
|
Which intravenous anesthetic agents have minimal effect on evoked potentials and are thus compatible with effective monitoring of evoked potentials?
|
• Barbiturates, propofol, and fentanyl or remifentanil have less of an effect on cortical evoked potentials and are thus compatible with effective monitoring of somatosensory evoked potentials (SSEP) and brainstem auditory evoked potentials (BAEP).
|
|
|
213 Brainstem auditory evoked potentials (BAEP) are generally very resistant to alteration by anything other than structural pathology in the brainstem. What operating room environmental variable will decrease latency and prolong interpeak intervals in BAEPs?
|
• Mild hypothermia has been associated with decreased latency and prolonged interpeak intervals during brainstem auditory evoked potentials (BAEP).
|
|
|
214 What agents will not alter bispectral index (BIS) monitoring?
|
• Since the bispectral index (BIS) is based upon the hypnotic action of agents, the BIS is not affected by opioids or analgesics.
• Nitrous oxide alone will have no effect on BIS. • Ketamine has minimal effect on BIS, and may slightly increase BIS transiently. |
|
|
215 In addition to barbiturates and propofol, what three (3) other anesthetic agents are compatible with somatosensory evoked potential (SSEP) monitoring?
|
• Ketamine, etomidate, and opiates do not appear to alter the latency or amplitude of somatosensory evoked potential (SSEP) monitoring.
|
|
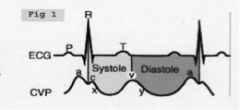
Think about a central venous pressure (CVP) waveform: you know what the a, c and v waves represent. What do the x-descent and y-descent indicate?
|
• On the central venous pressure (CVP) waveform, the x-descent occurs during ventricular systole and represents atrial relaxation with downward displacement of the tricuspid valve. The y-descent occurs during diastole and represent early ventricular filling through the open tricuspid valve.
|
|
|
Give three (3) contraindications to use of a pulmonary artery catheter.
|
• Relative contraindications to pulmonary artery catheterization are
› (1) complete left bundle branch block › (2) Wolff-Parkinson-White syndrome, and › (3) Ebstein's malformation. |
|
|
Where could a central venous or pulmonary artery catheter be inserted in the patient with superior vena cava syndrome?
|
• The edema due to superior vena cava syndrome often times necessitates venous access through the lower extremity. A central venous or pulmonary artery catheter can be inserted through the femoral vein in such cases.
|
|
|
What three (3) valuable cardiovascular parameters are obtained from an arterial line?
|
• Invasive arterial blood pressure monitoring provides information regarding
› (1) left ventricular volume › (2) left ventricular function › (3) systemic vascular resistance. |
|
|
What condition or situations result in an abnormal arterial waveform with a false elevation of systolic pressure?
|
• A decreased arterial compliance or a decreased transducer system frequency (ringing or overshoot) produce distortion of the arterial waveform. This particular distortion produces extra waveforms and results in overestimation of systolic blood pressure.
|
|
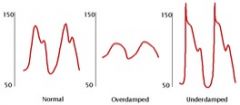
What factors may cause damping of the arterial pressure transducer system? What effect does system damping have on arterial blood pressure readings?
|
• Damping refers to how quickly a system comes to rest after being set in motion.
• The presence of air bubbles in the tubing, thrombus formation in the catheter, or inadvertent kinking of the catheter may overly damp the system. • Losses of the dicrotic notch and fine details in the waveform indicate an overly damped system. • Overdamping results in an underestimation of systolic blood pressure and an overestimation of diastolic pressure; MAP remains fairly accurate. |
|
|
Your patient requires arterial cannulation: list 6 arterial cannulation sites, in order of preference.
|
• Multiple arteries can be used for direct measurement of blood pressure; the top 6 sites for arterial cannulation are:
› (1) radial artery › (2) ulnar artery › (3) brachial artery › (4) axillary artery › (5) femoral artery, and › (6) dorsalis pedis artery. (Note: Morgan, et al. place axillary #6 in their list.) • RUB FDA (according to M&M) |
|
|
For each of the 6 arteries listed in the previous question, list a clinical point of relevance or interest.
|
• (1) Radial artery: the most commonly selected site for arterial cannulation non-tapered catheters are preferred for cannulation of the radial artery.
• (2) Ulnar artery: more difficult to cannulate owing to its deeper and more tortuous course; the ulnar artery is the primary arterial supply of hand blood flow. • (3) Brachial artery: large and easily identifiable in the antecubital fossa; insertion site is medial to biceps tendon; can accommodate an 18 gauge needle; median nerve damage is possible. • (4) Axillary artery: the insertion site is at the junction of the pectoral and deltoid muscles-special kits are now available; nerve damage can result from hematoma or traumatic cannulation. • (5) Femoral artery: provides easy access in low flow state; the femoral artery is prone to pseudo aneurysm and formation of atheroma, and there is potential for retroperitoneal hemorrhage. • (6) Dorsalis pedis artery: being the farthest distance from the aorta, arterial waveforms are most distorted, leading to higher systolic pressure estimates |
|
|
Identify and describe phase I of the C02 waveform.
|
• Phase I of the C02 waveform reflects late inspiration, during which carbon dioxide levels should be near zero.
|
|
|
Identify and describe phase II of the C02 waveform.
|
• Phase II represents the emptying of connecting airways and the beginning of the emptying of alveoli.
• As exhalation continues, gas from alveoli in regions with relatively short conducting airways appears and mixes with dead space gas from regions with relatively long conducting airways, resulting in an increasing C02 level. • Phase II reflects a mixture of anatomic and alveolar dead-space. |
|
|
Identify and describe phase III of the C02 waveform
|
• Phase III is the alveolar plateau.
• Because of uneven emptying of alveoli, the slope continues to rise gently. Point D shows the best approximation of alveolar C02 (end of expiration, beginning of inspiration, end-tidal C02). |
|
|
Identify and describe phase IV of the C02 waveform.
|
• As the patient inhales, CO2-free gas enters the patient's airway, and the CO2 level abruptly falls to zero. Phase IV is inspiration.
|
|
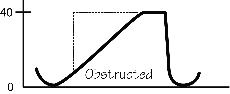
Interpret the a (alpha) angle of the C02 waveform.
|
• The angle between Phases II and III is called the a (takeoff, elevation) angle. Normally, it is between 100 and 110 degrees.
• It is decreased with obstructive lung disease, as the dead space volume takes longer to be exhaled. The slope of Phase III depends on the lung's ventilation-perfusion status. • Airway obstruction and PEEP cause an increased slope and a larger a angle. |
|
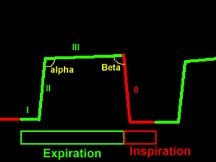
Interpret the b (beta) angle of the C02 waveform.
|
• The angle between the end of Phase III and the descending limb of the capnogram is called the b angle.
• Normally, it is approximately 90 degrees. • The angle will be increased with rebreathing. Another possible cause of an increased b angle is a prolonged response time compared with the respiratory cycle time, particularly in children. |
|
|
What two hemoglobin alterations will yield falsely high pulse oximeter readings?
|
• Carboxyhemoglobin (carbon monoxide poisoning) will cause falsely high pulse oximeter readings. Carboxyhemoglobin and oxyhemoglobin absorb light at 660 nm identically, thus the falsely high reading.
• Methemoglobin has the same absorption coefficient at both red and infrared wavelengths; the resulting 1:1 ratio corresponds to a saturation reading of 85% --the pulse oximeter is essentially "locked at 85% by the presence of methemoglobin. Thus, if Sa02 is actually less than 85%, the reading will be falsely high. |
|
|
What is the best monitor to detect a disconnection?
|
• According to Stoelting and Miller, capnography and spirometry have the highest value in detecting disconnection. The next best monitors for detecting disconnection are pulse oximetry and the stethoscope.
|
|
|
List seven characteristics of nondepolarizing neuromuscular blockade.
|
• Seven characteristics of nondepolarizing NM blockade are:
› (1) Decreased twitch height, › (2) fade during tetany, › (3) fade during train-of-four (T1:T4 ratio >0.7), › (4) post-tetanic potentiation, › (5) absence of fasciculations, › (6) antagonism of block by acetylcholinesterase inhibitors, and › (7) augmentation of block by other nondepolarizing agents. |
|
|
Describe the basic operation of a forced air warmer.
|
• A forced-air warmer (such as the Bair Hugger", Arizant Healthcare) entrains ambient air through a microbial filter. The air is warmed using an thermostat-controlled electric heater, and then blown through a hose that is connected to an inflatable patient cover. Forced-air warmers are also known as convection warming devices and warm air blowers.
|
|
|
List two standard for forced-air warming devices.
|
• The U.S. standards for forced-air warming devices (2002) are
› (1) the maximum contact surface temperature shall not exceed 48°C, and › (2) the average contact surface temperature shall not exceed 46°C during normal conditions |
|
|
State advantages afforded by forced-air warmers.
|
• Forced-air warming is safe, simple effective, and inexpensive. There are a variety of available covers, both disposable and reusable, as well as pediatric styles.
• Forced-air warming provides more calories-to-cost than other warming modalities. • Fiberoptic laryngoscopes can be warmed before use with a forced-air device. • The forced-air warmer can be used to warm the operating table before the patient is transferred to the table. • It can also be used for cooling. • Finally, forced-air warmers have been used to relieve claustrophobia. |
|
|
List some disadvantages of forced-air warmers.
|
• Electric power requirements of forced-air warmers make them unsuitable for field use.
• They are cumbersome to transfer or set up in a CT scanner. • The forced-air warmer must occasionally be removed from the patient to expose covered areas. • Finally, many systems do not permit the concurrent use of multiple blankets (i.e., upper and lower body) without using two separate forced-air units. |
|
|
Define perioperative blood salvage.
|
• Perioperative blood salvage refers to the recovery of shed blood from the surgical field or wound drains and re-administration to the patient. In most instances, the process involves "washing" of the salvaged material with return of only the RBC component of blood.
|
|
|
List seven situations in which intraoperative blood salvage (IBS) may be employed.
|
• Seven situations in which intraoperative blood salvage (IBS) is commonly employed are:
› (1) cardiovascular surgical procedures, › (2) aortic reconstruction, › (3) spinal instrumentation, › (4) joint arthroplasty, › (5) liver transplantation, › (6) resection of arterio-venous malformations, and › (7) occasionally in the management of trauma patient. |
|
|
Briefly describe the operation of contemporary "cell saver" (blood salvage) devices. What is the hematocrit range of the salvaged blood aliquots returned to the patient? How efficient is the modern cell saver?
|
• Contemporary "cell saver" devices anticoagulate the salvaged blood as it leaves the surgical field, separate the RBCs from other liquid and cellular elements by centrifugation, and then wash the salvaged RBCs extensively with saline. The RBCs are typically returned to the patient suspended in saline in aliquots of 125 or 225 mL with a hematocrit of 45 to 65%. Approximately 50% of RBCs are salvaged, therefore anticipate administration of allogenic blood.
|
|
|
What are the contraindications to intraoperative blood salvage?
|
• Contraindications to intraoperative blood salvage are the presence of infection, malignant cells, urine, bowel contents, or amniotic fluid in the operative field.
|
|
|
Identify expected complications of intraoperative blood salvage.
|
• The potential complications of intraoperative blood salvage (IBS) are a function of the reinfusion of materials that might remain after the washing process. Such materials that escape from the washing process include fat, microaggregates such as platelets and leukocytes, air, red cell stroma, free hemoglobin, heparin, bacteria, and debris from the surgical field. Most of these are in fact removed quite efficiently by contemporary cell salvage equipment. Bacteria are the exception and contamination of cell saver return with skin organisms is relatively common.
|
|
|
What coagulopathy is expected after intraoperative blood salvage? How would you manage this coagulopathy?
|
• Dilutional coagulopathy is to be expected after intraoperative blood salvage because the washing process removes essentially all clotting factors and most platelets. Management is the same as for a dilutional coagulopathy occurring with administration of homologous or preoperative autologous donation (PAD) blood.
|
|
|
Briefly describe the basic operation of a heat and moisture exchanger (HME).
|
• A heat and moisture exchanger (HME) conserves some exhaled water and heat and returns them to the patient in the inspired gas.
• Many HMEs also perform bacterial/viral filtration to prevent inhalation of small particles. • The HME is also known as a condenser humidifier, Swedish nose (!), artificial nose, nose humidifier, passive humidifier, regenerative humidifier, moisture exchanger, and vapor condenser. |
|
|
What are the indications for heat and moisture exchanger (HME) use?
|
• An heat and moisture exchanger (HME) can be used to increase inspired heat and humidity during both short- and long-term ventilation. HMEs are indicated if the patient is hypothermic and for use in the neonatal circuit HMEs may be especially useful in transporting the intubated patients.
|
|
|
List two contraindications to heat and moisture exchanger (HME) use.
|
• Heat and moisture exchangers are contraindicated in
› (1) patients with thick and copious, or bloody secretions, and › (2) patients with a leak that prevents exhaled gas from passing through the HME (e.g., bronchopleural fistula, or leaking tracheal tube cuff). |
|
|
List 5 adult patients who are inappropriate candidates for ambulatory (outpatient) surgery.
|
• The following 5 adult patients are inappropriate candidates for ambulatory (outpatient) surgery:
› (1) patients expected to have major blood loss or undergoing major surgery; › (2) ASA III and IV patients who require complex or extended monitoring or postoperative treatment; › (3) morbidly obese patients with significant respiratory disease, including sleep apnea; › (4) patients with a need for complex pain management; and, › (5) patients with significant fever, wheezing, nasal congestion, cough, or other symptoms of a recent upper respiratory infection. |
|
|
List 6 other adult patients who are inappropriate candidates for ambulatory (outpatient) surgery.
|
• The following 6 additional patients are not appropriate candidates for ambulatory (outpatient) surgery:
› (1) patients susceptible to malignant hyperthermia; › (2) patients with uncontrolled seizure activity; › (3) patients with acute substance abuse; › (4) patients with active infection; › (5) uncooperative or unreliable patients; and, › (6) patients who have no responsible adult at home during convalescence |
|
|
Which two crystalloid solutions contain potassium (K')?
|
• The two crystalloid solutions that contain potassium (K') are isotonic lactated Ringers (LR) and hypertonic D5LR.
|
|
|
Banked blood may go through many changes before it is infused into the patient. What factors are absent in banked blood?
|
• Blanked blood is devoid of platelets, factors V and VIII, and 2,3-DPG.
|
|
|
What blood product "should be ABO compatible, but is not strictly mandatory?
|
• Platelets bear both ABO and HLA (human leukocyte antigen) and therefore ABO compatibility is ideal because incompatibility shortens the lifespan of the platelet.
• However, platelet ABO compatibility is not required. |
|
|
Describe the current treatment of dilutional coagulopathy.
|
• Dilutional coagulopathy usually becomes a problem during massive transfusions.
• Both platelets and coagulation factors are markedly decreased and must be replaced. • They should be administered after laboratory documentation of the deficiency. • It is no longer accepted practice to give fresh frozen plasma (FFP) routinely after 5 units of packed red blood cell (PRBC), and it is not proper to give platelets after 10 units of PRBC. • At present, dilutional coagulopathies appear to be rare, even with the transfusion of one blood volume. |
|
|
If an acute hemolytic reaction is suspected, the blood bank should be notified. Blood and urine samples should be sent to the laboratory for examination. What two immediate tests will be performed on the specimens?
|
• Immediate tests on the post transfusion specimen will include
› (1) a visual check for hemoglobinemia and › (2) a direct antiglobulin (Coombs) test. • The direct antiglobulin test examines recipient RBCs for the presence of surface immunoglobulins and complement. If positive, an acute hemolytic reaction may have occurred and additional testing is indicated to ascertain the cause, including repeat ABO/Rh type, antibody screen, cross matching, and other tests as indicated. The blood bank will determine whether the unit of blood had been correctly released to the patient. |
|
|
The Jackson table and Wilson frame are examples of what type of equipment?
|
• The Jackson table and Wilson frame are examples of orthopedic frames. Orthopedic frames--also called bolsters, or spinal surgery frames--are used to free the chest and abdomen during surgery in the prone position.
|
|
|
What advantages do an orthopedic frame, such as the Jackson table or Wilson frame afford?
|
• Orthopedic frames (spinal surgery frames, or bolsters) minimize abdominal compression by the operating room table and maintain normal pulmonary compliance. By minimizing abdominal compression, the inferior vena cava is not impaired thus also optimizing venous return.
|
|
|
Venous air embolism is the most feared consequence of posterior fossa craniotomies in the head-up position. What three other complications are possible consequences of posterior fossa craniotomies in the head-up position?
|
• Pneumocephalus, quadriplegia, and peripheral nerve injuries are possible complications of posterior fossa craniotomies in the head-up position.
|
|
|
Describe the cause of a (tension) pneumocephalus.
|
• Pneumocephalus occurs because air enters the cranium while the patient is in a head-up position (with respect to gravity) at a time when the volume of the intracranial contents has been reduced as a result of some combination of hypocapnia, good venous drainage, osmotic diuresis, and CSF loss from the operative field. When the cranium is closed, and the patient is returned to the near-supine position, CSF, venous blood volume,and extracellular fluid return or reaccumulate, and the air pocket becomes an unyielding mass lesion (because of the very slow diffusion of nitrogen).
|
|
|
How does pneumocephalus manifest?
|
• Clinically, tension pneumocephalus usually presents as a delayed emergence from general anesthesia following craniotomy. A severe headache may also ensue.
|
|
|
Describe the "beach chair" position.
|
• The "beach chair" position--a variation of the sitting--is used increasingly for shoulder surgeries, including arthroscopic procedures.
› The torso is elevated at 45 degrees in the beach chair position, compared to 90 degrees in the sitting position. › The patient's head, neck, and hips must be secured to prevent additional lateral movement. The head and neck must remain firmly supported by the operating table and secured in a neutral position; excessive rotation or flexion of the head away from the operative side results in stretch injury to the brachial plexus. Care also must be taken to avoid pressure on the eyes and ears. › All airway connections should be tightened and possibly reinforced with tape because after surgical draping, access to the patient's face and airway is limited. › The knees are usually slightly flexed for balance and to reduce stretching of the sciatic nerve, and the feet and ankles are supported and padded. |
|
|
The "beach chair" and sitting positions may cause excessive cervical flexion. What adverse consequences may result from excessive cervical flexion in the sitting or "beach chair" position?
|
• Excessive cervical flexion in the sitting and "beach chair" positions (or any position for that matter) can impede arterial and venous blood flow, causing hypoperfusion or venous congestion of the brain. Excessive cervical flexion can obstruct the endotracheal tube and place significant pressure on the tongue, leading to macroglossia.
|
|
|
To reduce the risk associated with excessive cervical flexion in the "beach chair" position, how many fingerbreadths should be maintained between the chin (mandible) and sternum?
|
• Maintaining at least 2 fingerbreadths of space between the chin (mandible) and sternum is recommended for normal sized adults.
|
|
|
Consider the patient in the lateral decubitus position with no axillary roll and a pulse oximeter on the dependent hand. What is the most likely cause for an apparently low S,02 from the pulse oximeter?
|
• The axillary neurovascular bundle is compressed, compromising blood flow to the extremity. A small support placed just caudad of the downside axilla can be used to lift the thorax enough to relieve pressure on the axillary neurovascular bundle and prevent disturbed blood flow to the arm and hand.
• This chest support (inappropriately called an axillary roll by some) should support only the chest wall and it should be periodically observed to ensure that it does not impinge on the neurovascular structures of the axilla. |
|
|
In the lateral position, injuries to what nerves are most likely? Why?
|
• The common peroneal (fibular) nerve is the most commonly injured nerve of the lower extremity when the patient is in the lateral position. The injury results from compression of the common peroneal (fibular) nerve between the OR table and the head of the fibula. To prevent common peroneal nerve injury in the lateral position, padding extending from the knee to the heel should be placed along the lateral aspect of the dependent leg.
• Injury to brachial plexus because of improper padding of the chest and head is possible. |
|
|
Describe the use and operation of the fracture table.
|
• The orthopedic fracture table consists of a body section to support the head and thorax, a sacral plate for the pelvis with a perineal post, and adjustable footplates. The most important features of the table are the ability to maintain traction on a lower extremity and to obtain surgical and fluoroscopic access. Because the patients requiring this table are often in pain, anesthesia is usually induced before the patient is moved to the table. The supine patient who is placed on a fracture table for repair of a fractured femur usually has the pelvis retained in place by a vertical pole at the perineum, with the foot of the injured extremity fixed to a mobile rest. A worm gear on the rest lengthens the distance between the foot and the pelvis so that the bone fragments can be distracted and realigned.
|
|
|
The patient is positioned on a fracture table; what nerve injuries are possible?
|
• Unless the pole is well padded, severe pressure can be exerted on the pelvis, and damage can occur to the genitalia and the pudendal nerves.
• Complete loss of penile sensation has been reported after use of the fracture table. • The correct position for the pole is against the pelvis between the genitalia and the uninjured limb. Other possible nerve injuries on the fracture table include brachial plexus damage (due to extended arm or arm placed directly across the chest) or lower extremity compartment syndrome. |
|
|
What is compartment syndrome? What features characterize compartment syndrome?
|
• Compartment syndrome is a potentially life-threatening position-related complication that causes damage to neural and vascular structures from swelling of tissues within a muscular compartment, especially those of the leg.
• If perfusion to an extremity is inadequate, a compartment syndrome may develop. • Compartment syndrome is characterized by ischemia, hypoxic edema, elevated tissue pressure within fascial compartments, and extensive rhabdomyolysis. |
|
|
How can compartment syndrome in the leg be precipitated?
|
• Compartment syndrome can be precipitated by intraoperative hypotension in conjunction with leg elevation that causes low-flow states.
• Pneumatic compression boots and fluid extravasation into tissues have been linked to compartment syndromes. • Vascular obstruction of major leg vessels by intrapelvic retractors, by excessive flexion of knees or hips, or by undue popliteal pressure from a knee crutch may cause compartment syndrome. • External compression of the elevated extremity by straps or leg wrappings that are too tight, by the inadvertent pressure of the arm of a surgical assistant, or by the weight of the extremity against a poorly supportive leg holder may also precipitate compartment syndrome. |
|
|
What is the definitive treatment for compartment syndrome? What sequelae will ensue if compartment syndrome is not treated?
|
• The definitive treatment for compartment syndrome is fasciotomy.
• If untreated, compartment syndrome will progress to tissue necrosis with myoglobinuria and acute renal failure (crush syndrome). Amputation and even death may occur. |
|
|
State five (5) risk factor for difficult mask ventilation, from greatest risk to least.
|
• Five risk factors for difficult mask ventilation, from greatest to least risk are:
› (1) presence of a beard, › (2) body mass index >26 kg/m2, › (3) lack of teeth (edentulous), › (4) age > 55 years, and › (5) history of snoring. |
|
|
What is the pressure limit for positive pressure face mask ventilation?
|
• Positive-pressure ventilation via a face mask should normally be limited to 20 cm H2O to avoid stomach inflation.
|
|
|
List the guidelines to be followed in order to use a laryngeal mask airway (LMA) during a laparoscopic procedure.
|
• The following guidelines are recommended for use of the laryngeal mask airway (LMA) during laparoscopy:
› (1) the clinician should be an experienced LMA user; › (2) careful patient selection is required (e.g., fasted, not obese); › (3) use correct size LMA; › (4) tell the surgeon you are using an LMA; › (5) use a total IV anesthetic technique or volatile agent; › (6) adhere to the "15" rule: <15 degrees tilt, <I5 cm H20 intra-abdominal pressure, <15 minutes duration; › (7) avoid inadequate anesthesia during surgery; and › (8) avoid disturbing the patient during emergence. |
|
|
You decide a laryngeal mask airway (LMA) is appropriate for the airway management of the 9-kg patient, but a 1.5 LMA is not available; will you use a size 1 or a size 2 LMA?
|
• LMA size selection is critical to its successful use, and to the avoidance of minor as well as more significant complications. The manufacturer recommends that the clinician choose the largest size that will fit comfortably in the oral cavity, and then inflate to the minimum pressure that allows ventilation to 20 cm H20 without an air leak. Accordingly, a size 2 LMA classic is appropriate for the 9-kg patient (Morgan, et al. 6.5-20 kg + size 2
|
|
|
What is the Murphy eye on a tracheal tube? What is the purpose of the Murphy eye?
|
• A Murphy eye is a hole through the tracheal tube wall opposite to the bevel. The purpose of the Murphy eye is to provide an alternate pathway for gas flow if the bevel becomes occluded.
|
|
|
What is the name for tracheal tubes that lack a Murphy eye?
|
• Tracheal tubes that lack a Murphy eye are called Magill-type tubes. An advantage of the Magill-type tube is that the cuff can be placed closer to the tip of the tube.
|
|
|
What does the ASTM require of tracheal tubes?
|
• The ASTM requires that a radio-opaque marker is placed at the patient end of the tube or along the entire length of the tube to determine the position of the tube after intubation.
|
|
|
How will the PaC02 change during the first minute of low-flow apneic ventilation (apneic insufflation)? During each minute after the first minute?
|
• During low-flow apneic ventilation (apneic insufflation), the PaC02 rises approximately 6 mmHg during the first minute, and approximately 3-4 mmHg each minute thereafter.
• By extension, during apnea--from any cause--PaCO2 will rise by 6 mmHg during the first minute, and 3-4 mm-Hg each minute thereafter. |
|
|
What is Klippel-Feil syndrome? What other problems are associated with Klippel- Feil syndrome?
|
• Klippel-Feil syndrome is a musculoskeletal disorder characterized by a short neck owing to a reduced number of cervical vertebrae, or fusion of several vertebrae
• Movement of the neck is severely limited. Spinal stenosis and kyphoscoliosis are associated with Klippel-Feil and mandibular malformations and/or micrognathia may be present. • Taken together, the patient with Klippel-Feil presents as a difficult airway. |
|
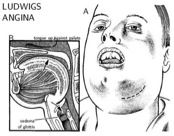
What is Ludwig's angina? What are the signs and symptoms of Ludwig's angina?
|
• Ludwig's angina is an overwhelming generalized septic cellulitis of the submandibular region.
• Ludwig's angina generally occurs after dental extraction; early signs and symptoms include chills, fever, drooling of post saliva, inability to open the mouth, and difficulty in speaking, as well as edema of the tongue, neck, and submandibular region. • The cause is often hemolytic streptococci, but may be a mixture of aerobic and anaerobic organisms. |
|
|
Describe airway management for the patient with Ludwig's angina.
|
• Airway management in the patient with Ludwig's angina may be extremely difficult.
• Preliminary tracheostomy using local anesthesia in the awake patient is the safest course. |
|
|
List contraindications for cricothyrotomy.
|
• Cricothyroidotomy, cricothyrotomy, coniotomy, and minitracheostomy are synonyms for establishing an air passage through the cricothyroid membrane. Although cricothyrotomy is the procedure of choice in an emergency situation, it may also apply to an elective situation when there is limited access to the trachea (e.g., severe cervical kyphoscoliosis).
• Cricothyrotomy is contraindicated in neonates and children younger than 6 years of age, and in patients with laryngeal fractures. |
|
|
A cricothyrotomy with a 14-gauge catheter has been done on the patient. What driving pressure is needed to generate sufficient gas flow for transtracheal jet ventilation?
|
• A 12- or 14-gauge catheter requires a driving pressure of 50psi to generate sufficient gas flow for transtracheal jet ventilation.
|
|
|
What two amide local anesthetics and one ester local anesthetic are most often used for infiltration anesthesia?
|
• The two amide local anesthetics most often used for infiltration anesthesia are lidocaine (0.5% to 1.0%) and bupivacaine (0.125% and 0.25%). The most commonly used ester local anesthetic for infiltration anesthesia is procaine (0.5% to 1.0%).
|
|
|
State the advantage of EMLA cream and the typical dosing.
|
• EMLA cream is able to diffuse through the keratinized layer of intact skin to block neuronal transmission from dermal sensory receptors. EMLA cream is thus used for topical anesthesia of skin.
• The recommended dose of EMLA for minor dermal procedures is 2.5 g applied over a 20- to 25- cm2 skin surface for at least 60 minutes before the procedure. • For painful procedures, 2 g of EMLA cream per 10-cm2 of skin is applied and left in place for at least 2 hours. • EMLA cream is useful for pain associated with venipuncture and arterial cannulation, skin graft harvesting, arteriovenous shunt procedures, and lumbar puncture. |
|
|
Since EMLA cream contains prilocaine, methemoglobinemia may be a concern, even though the prilocaine is topically administered. What population of patients may be susceptible to methemoglobinemia following EMLA cream and why?
|
• Methemoglobinemia may occur in children age < 3-12 months, reflecting immature reductase pathways.
• Red blood cells contain Methemoglobin reductase that normally reduces ferric (Fe3+) iron to ferrous (Fe2+", normal") iron. Concurrent administration of EMLA cream with other oxidizing agents (sulfonamides, acetaminophen, benzocaine, phenytoin, nitroglycerin, nitroprusside) may overload the immature reductases in the child < 3-12 months of age. |
|
|
List 4 contraindications for EMLA cream.
|
• EMLA cream is not recommended for:
› (1) use on mucous membranes, › (2) use on skin wounds, › (3) use on patients being treated with the antidysrhythmic agent mexiletine, and › (4) use in patients with known history of allergy to amide local anesthetics. |
|
|
The mechanism(s) of differential block of sensory and motor nerve fibers by local anesthetics is a controversial topic, at best. State the clinical progression of fiber block and list 6 mechanisms that contribute to the differential block produced by local anesthetics.
|
• The clinical progression of differential nerve block by local anesthetics, from first blocked to last blocked, is autonomic fibers, sensory fibers and motor fibers.
• At least 6 factors contribute to differential nerve block by local anesthetics: › (1) the anatomic and geometric arrangement of the individual fibers in a nerve bundle; › (2) the size (diameter) of the individual nerve fibers; › (3) the inherent impulse activity (firing rate, frequency) of the individual nerve fibers; › (4) the variability in longitudinal spread of agent along the nerve fibers; › (5) the effects on ion channels other than the sodium channel, and › (6) the choice of local anesthetic. • Sensory nerve fibers fire more often than motor fiber and this may explain to a large extent why sensory fibers are blocked before motor nerve fibers (Nagelhout). |
|
|
Caudal anesthesia is a form of epidural anesthesia in which the injection is made at the sacral hiatus, as you know. What landmarks are palpated to locate the sacral hiatus?
|
• The sacral hiatus usually lies 5 cm above the tip of the coccyx and directly beneath the uppermost limit of the natal cleft. The two sacral cornua lie on either side of the sacral hiatus and cephalad to the coccyx, and provide useful landmarks when performing an epidural from a caudal approach. Direct palpation of the depression between the sacral cornua is the best method to locate the sacral hiatus.
|
|
|
How did the sacral hiatus and sacral cornua arise developmentally?
|
• The sacral hiatus results from failure of fusion of the laminae of the 5th sacral segment. The spinous process is also lacking posteriorly. The sacral cornua lie on each side of the sacral hiatus (lateral to the hiatus) and represent articular crests of the residual laminae.
|
|
|
What two nerves are derived from the posterior cord of the brachial plexus?
|
• The posterior cord of the brachial plexus gives rise to the axillary and radial nerves.
|
|
|
What two nerves are derived from the lateral cord of the brachial plexus?
|
• The lateral cord of the brachial plexus gives rise to the musculocutaneous and median nerves.
|
|
|
What two nerves are derived from the medial cord of the brachial plexus?
|
• The medial cord of the brachial plexus gives rise to the median and ulnar nerves.
|
|
|
Describe the landmarks and relative needle location in order to perform a median nerve block at the wrist.
|
• In order to perform a median nerve block at the wrist, a 22-gauge needle is directed just medial to the ulnar artery pulse, or, if the ulnar pulse is not palpable, just medial to the flexor carpi radialis. A total volume of 3 to 5 mL of anesthetic is injected to block the median nerve.
|
|
|
Which segment of the brachial plexus is targeted in the interscalene approach to a brachial plexus block? (Hint: branches, roots, cords, trunks, divisions ...)
|
• The interscalene approach to a brachial plexus block targets the trunks of the brachial plexus.
• After the roots emerge from cervical and thoracic vertebrae (C5-TI), the trunks are sandwiched between the anterior and middle scalene muscles. Two sheathes of fibrous tissue enclose the trunks between the scalene muscles, forming the space into which local anesthetics can be injected to produce brachial plexus block. • Mnemonic: Robert Taylor Drinks Cold Beer (Roots, Trunks, Division, Cords, Branches, in order from vertebral origins to upper extremity terminations). |
|
|
Your patient requires hand surgery. Which upper extremity block would not be appropriate?
|
• The interscalene block is suitable for shoulder and arm surgery, but not for hand surgery.
• A supraclavicular, infraclavicular, axillary, or Bier block may be used for hand surgery. |
|
|
What nerve branches can be blocked in a popliteal fossa block?
|
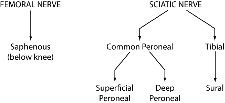
• The sciatic nerve can be localized in the upper area of the popliteal fossa. The goal is to block the sciatic nerve can be blocked before it branches into the tibial and peroneal nerves.
|
|
|
Which two nerves are anesthetized in a popliteal block?
|
• At the upper margin of the popliteal fossa, the sciatic nerve divides into the tibial and common peroneal nerves. The posterior and lateral approaches to the popliteal fossa block these two branches of the sciatic nerve.
|
|
|
List the indications for a popliteal fossa block.
|
• A popliteal fossa block is used for foot and ankle surgery, short saphenous vein stripping, and in the pediatric population. The popliteal block provides improved calf tourniquet tolerance and an immobile foot, compared to an ankle block.
|
|
|
List four (4) surgical and three (3) nonsurgical indications for intercostal nerve block.
|
• Surgical intercostal block indications include upper abdominal and thoracic superficial procedures, such as
› (1) insertion of thoracotomy and gastrostomy tubes, › (2) minor breast surgery, › (3) extracorporeal lithotripsy, and › (4) cardiac pacemaker insertion. • Three nonsurgical indications for intercostal nerve block are to provide relief from: › (1) fractured rib pain, › (2) pleuritic pain, and › (3) herpes zoster ("shingles") pain. |
|
|
What is the occurrence rate of headaches following unintentional dural puncture with an 18-gauge epidural needle while attempting an epidural anesthetic in the pregnant patient?
|
• When a 17- or 18-gauge epidural needle results in unintentional dural puncture in the obstetric patient, the subsequent incidence of postdural puncture headache is as great as 70% to 80%.
|
|
|
You perform a successful epidural blood patch according to standard policy. How long should the patient rest and in which position before ambulating?
|
• Following a successful epidural blood patch, the patient should rest in the supine position for 30-60 minutes (up to 2 hours, according to Yao).
|

