![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
97 Cards in this Set
- Front
- Back
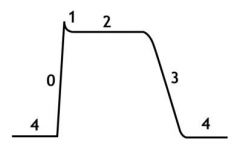
In the labeled regions of a cardiocyte action potential, which region corresponds to diastole?
|
4
|
|
In the labeled regions of a cardiocyte action potential, which region corresponds to rapid depolarization through opening of fast Na channels?
|
0
|
|
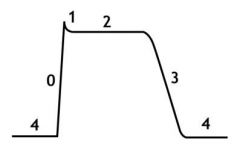
Describe the ionic movement during the plateau phase of the cardiac action potential.
|
(phase 2) - Ca moves in, K moves out
|
|
In stage 3 of the cardiac AP, what two things must occur to repolarize the cell?
|
Close Ca channels;
Influx of K |
|
|
What are the only two treatments for veterinary bradyarrhythmias? Which treatment is of the longest duration?
|
Pacemaker (long term)
Atropine (emergency only) |
|
|
What are the classes of arrhythmic drugs and what does each block?
|
I - Na blockers
II - Beta blockers III - K blockers IV - Ca blockers V - others |
|
|
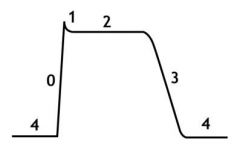
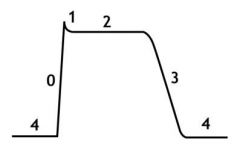
How do class I drugs affect the AP?
|
Decrease slope of phase 0 by blocking Na channels
|
|
|
What is the most commonly used Class I drug in vet med?
|
Lidocaine
|
|
|
Regarding group Ia and Ib drugs...
a) both groups are used for supraventricular and ventricular arrhythmias b) only Ia is used for supra and ventricular arrhythmias c) only Ib is used for supra and ventricular arrhythmias d) none of the above |
b) only Ia is used for supra and ventricular arrhythmias
explanation - Ia works for both but Ib is better for ventricular arrhythmias |
|
|
T or F:
Both groups Ia and Ib have a lengthening effect on the AP. |
False!
Ia lengthens the AP while Ib shortens the AP |
|
|
Which group I drug is mostly used in horses because it causes side effects in dogs and cats?
|
Quinidine
|
|
|
Which cardiac drug can cause color changes in dogs?
|
Procainamide
|
|
|
Why must procainamide be given slowly via IV?
|
Otherwise it causes cardiovascular collapse.
|
|
|
T or F:
Group Ia drugs are only safe for large animal cardiology. |
False!
Procainamide is OK in dogs but Quinidine is bad |
|
|
What are the two class Ib drugs discussed in class? Which can be used in cats?
|
Lidocaine (OK for cats but need 1/10 dose compared to dogs)
Mexiletine (NEVER USED in cats) |
|
|
T or F:
Lidocaine has no effect on atrial tissue. |
True!
|
|
|
In general, class I drugs depend on:
a) intracellular Na concentration b) extracellular Na conc. c) extracellular K conc d) intracellular K conc |
Even though they block Na channels they depend on EXTRACELLULAR K CONCENTRATION!!!
|
|
|
What effect does hyperkalemia have on the activity of class I cardiac drugs? How 'bout hypokalemia?
|
Hyper increases activity
Hypo decreases activity |
|
|
Why is mexiletine not used much in dogs?
|
Tough to find!!!
|
|
|
How can the selectivity of the Beta blockers be determined from the name of the drug?
|
If it starts with A-E then it is selective; all the rest are non-selective
|
|
|
Which drug class is used to slow the sinus rate of hyperthyroid cats?
|
Class II - Beta blockers!!!
|
|
|
T or F:
Class II drugs are the first line of treatment of tachycardia in patients with heart failure. |
False!
Beta blockers should NEVER be used in heart failure! |
|
|
Choose all correct answers:
Propanolol is contraindicated in patients with... a) heart failure b) respiratory disease c) hyperthyroid d) none of the above |
A and B; heart failure and respiratory disease;
POTENT negative inotrope and also has B2 activity |
|
|
What is remarkable about discontinuing the use of a class II drug?
|
Gradual withdrawal should be used; never sudden stop!
|
|
|
Which class II drug can be used in patients with airway diseases?
|
Atenolol
|
|
|
Which class II drug is an emergency drug? How is it administered?
|
Esmolol;
Administered via CRI |
|
|
What are general effects of class II drugs on the heart?
|
Decrease HR
Decrease contractility Decrease lucitropy Decrease conduction velocity Increase refractoriness (all anti-sympathetic functions) |
|
|
What enzyme is responsible for the extremely short half life of Esmolol?
|
Blood esterase inactivates it
|
|
|
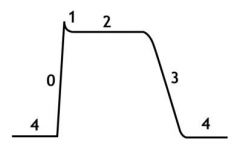
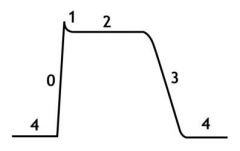
What effect do class III drugs have on the cardiac AP?
|
Lengthen plateau phase (phase 2)
Lengthen AP time and refractory period Prolong repolarization |
|
|
Which class III drugs have activities indicative of other classes?
|
Amiodarone also has class I, II, and IV
Sotalol also has class II |
|
|
Which drug is reserved for refractory arrhythmias?
|
Amiodarone
|
|
|
T or F:
Class III drugs are used for supraventricular and ventricular fibrillation? |
True!
|
|
|
Which method of amiodarone administration allows it to be used as an emergency drug?
a) CRI b) IV bolus c) Oral d) none of the above |
d) none of the above;
Amiodarone has a LOW onset of actions and a low oral bioavailability, thus it is a bad emergency drug! |
|
|
Why might amiodarone not be used in hyperthyroid cats?
|
it alters thyroid function
|
|
|
What is a prime indication for sotalol use (specific breed even)?
|
Acute Right Ventricular Cardiomyopathy in Boxers
|
|
|
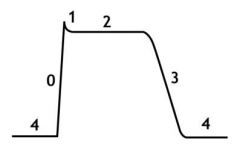
What effect does Sotalol have on phase 0 in the cardiac AP?
|
NO EFFECT
|
|
|
What effect do class IV drugs have on the cardiac AP?
|
Shorten phase 2
|
|
|
Which of the following has the least effect on contractility?
a) class Ia b) class Ib c) class II d) class III e) class IV |
e) class IV;
these drugs are mild negative inotropes |
|
|
What are the three main groups of the class IV drugs? Give an example of each.
|
Phenylalkylamines (Verpamil)
Benzothiazepine (Diltiazem) Dihydropyridines (Amlodipine) |
|
|
Which of the following has vasodilation as one of its actions?
a) class Ia b) class Ib c) class II d) class III e) class IV |
Class IV
|
|
|
Which class of type IV drugs has the most cardiac effects? Which has the least?
|
Phenylalkylamines (Verapamil) have the most cardiac effect;
Dihydropyridines (Amlodipines) ONLY have a vascular effect |
|
|
What is a specific indication for the type IV drugs?
|
Nodal reentry tachycardia
|
|
|
Which type IV drug is for emergency use? Which for chronic?
|
Verapamil (emergency)
Diltiazem (chronic) |
|
|
Which drugs are considered emergency cardiac drugs?
|
Atropine
Verapamil Lidocaine Esmolol Pimobendan Nitrates |
|
|
What is THE example of class V drugs discussed in class?
|
Digoxin
|
|
|
Which of the following is Digoxin indicated for?
a) Ventricular fibrillation b) Atrial fibrillation c) Bradycardia |
A-fib! The ONLY thing it is indicated for!
|
|
|
What is the most important priority in the treatment of heart failure?
|
Maintain arterial pressure
|
|
|
What three parameters does acute cardiac compensation maintain?
|
CO
BP Venous pressure |
|
|
What are the signs of chronic cardiac compensation and what are the causes of each?
|
Pale MM and increased CRT (increased vasoconstriction)
Edema/effusions (increased volume) Tachycardia (incrsd sympathetic) Fatigue (decreased CO) |
|
|
What types of drugs are used to treat the tachycardia experienced in heart failure?
|
Inotropes
|
|
|
What is used to treat the edema and effusion experienced in heart failure?
|
Diuretics and diet
|
|
|
What is the most important factor in heart disease progression?
|
Renin/Angiotensin/Aldosterone system
|
|
|
Why is furosemide not used in long-term heart disease therapy?
|
It activates the renin/angiotensin/aldosterone system!
|
|
|
What are the two 2nd diuretic classes in use for heart failure therapy?
|
Thiazides (loop diuretic)
Mineralocorticoid receptor agonists |
|
|
T or F:
Mineralocorticoid receptor agonists are the only diuretics that slow the progression of heart disease. |
True!
They block aldosterone!!! |
|
|
Why can't spirinolactone be used in cats?
|
Causes severe skin reaction!
|
|
|
When should diuretics be used?
|
when the patient is wet!!! ie: when there is a reason to use them (fluids and effusions are present)
|
|
|
What should always be used in conjunction with diuretics?
|
ACE inhibitors!
|
|
|
What are the venodilators used in veterinary medicine? Which is also an arteriodilator?
|
Nitroglycerin
Isosorbide Nitroprusside (general vasodilator) |
|
|
T or F:
Tolerance develops with prolonged use of all of the nitrate drugs. |
False!
While Nitroglycerine and isosorbide induce tolerance, Nitroprusside does not!! |
|
|
What are the most important diet nutrients to monitor in cardiac failure maintenance?
|
Na and Cl mostly
Also Protein |
|
|
When is diet maintenance indicated in cardiac failure? Why is this?
|
Only indicated when patient is WET!! This is because Na restriction activates renin/angiotensin system and causes disease progression
|
|
|
What is the mechanism of action for dobutamine and dopamine?
|
Increase Ca conc via cAMP which increases contractility
|
|
|
What drugs are used for acute inotropic support to increase CO? Which is best to use under anesthesia?
|
Dobutamine (best for anesthesia)
dopamine |
|
|
Which is more arrhythmogenic, dobutamine or dopamine? Which of these two also has a pressor effect?
|
Dopamine does both
|
|
|
T or F:
Digitalis only increases mortality at high concentrations. |
True! It does not increase mortality at low concentrations.
|
|
|
Which positive inotrope also inhibits NF-kB?
|
Pimobendan
|
|
|
What is the mechanism of action of Pimobendan?
|
Increases affinity between troponin C and Ca; this increases contractility;
Also inhibits phosphodiesterase III, causing vasodilation |
|
|
What is the only inotrope that increases survival time in dogs with heart failure?
|
Pimobendan
|
|
|
T or F:
Pimobendan should always be used with an ACE inhibitor. |
True!
|
|
|
Which three hormones are the major culprits in the progression of heart disease?
|
Angiotensin II
NE Aldosterone |
|
|
What are TGF B1 and NFK-B activated by?
|
Angiotensin II
|
|
|
What drug should you pretty much take with your morning vitamin?
|
An ACE inhibitor, apparently! Any of the 'prils...Enalapril or Benzapril
|
|
|
What are three classes of drugs that, used in conjunction, can theoretically manage heart failure?
|
ACE inhibitors (the 'prils)
Beta blockers (the 'olols) Aldosterone blockers (spirinolactone) |
|
|
T or F:
Due to the lipophilic cornea, the pharmacodynamics of the eye are much different than the rest of the body. |
False!
PD are the same in the eye as everywhere else! |
|
|
What are the three main factors influencing drug penetration into ocular tissue?
|
Concentration
Viscosity Lipid solubility |
|
|
What can be added to increase a drug viscosity? What does this do?
|
PVA or Methylcellulose;
increased viscosity lengthens residence contact time of the drug |
|
|
What factor or substance serves to remove the majority of topical ocular drugs?
|
Tears!
Go cry, emo kid... |
|
|
What can cause reflex tearing? (crying type tearing, not ripping type tearing)
|
pH out of whack
|
|
|
What are some factors affecting the penetration of topically applied opthalmic pharmacologics?
|
Corneal epithelium (water impermeable)
Corneal stroma (water soluble) Conjunctiva and sclera (may be more easily penetrated) |
|
|
How much drug is lost when application is performed dropwise?
|
~40% per drop...
One drop is 50uL and the cul-de-sac only holds 30uL |
|
|
When will fluorescein penetrate the eye? Why does this happen?
|
Penetration occurs when there is ulceration;
Fluorescein is water soluble and if the outer lipid soluble layer is ulcerated, then fluorescein can penetrate! |
|
|
Approximately how much drug reaches the aqueous humor via dropwise administration?
|
10%
|
|
|
What "artificial mucus" can be added to a drug to increase residency time?
|
Polyvinylpyrrolidone
|
|
|
What is the max contact time for eyedrops?
For ointments? |
drops - 5-10min
ointment - 20min |
|
|
When should ointments be applied intraocularly?
|
NEVA!
|
|
|
What is the preferred method for treating diseases in the ocular posterior segment?
|
Systemic administration
|
|
|
What are indications for ocular anesthetics?
|
Minor surgery
Manipulation of eye structures |
|
|
Why shouldn't ocular anesthetics be used as a treatment?
|
blocks healing
|
|
|
What are the delivery mechanisms for ocular anesthetics?
|
Topical
Injectable |
|
|
What is the ONE federally approved ocular antifungal?
|
Natamycin
|
|
|
What is the most potent ocular steroid?
|
Dexamethasone
|
|
|
What are side effects of topical non-steroidals administered to the eye?
|
Stinging and burning!
|
|
|
When are ocular steroids contraindicated?
|
Corneal ulceration (reduces healing);
Or, any time there is no inflammation |
|
|
What is the major goal of anti-glaucoma drugs?
|
Decrease intraocular pressure
|
|
|
Which anti-glaucoma class is contraindicated in cats?
|
Cholinesterase inhibitors
|
|
|
What is a side effect of atropine in horses?
|
Colic! Happens when atropine gets systemic!
|

