![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
101 Cards in this Set
- Front
- Back
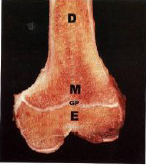
What is diagrammed on this distal femur?
|
D: diaphysis: corresponds to bone shaft
M: Metaphysis E: Epiphysis: distal to growth plate GP: growth plate (1) |
|

What is diagrammed on this proximal femur?
|
A: apophysis of the greater trochanter, associated with the smaller growth plate
GP: growth plate (2) M: metaphysis E: epiphysis D: diaphysis distal disease processes tend to occur in relatively specific regions of bone; |
|
|
Cortical bone - definition
|
= compact bone
|
|
|
Cancellous bone, definition
|
= spongey bone
includes trabeculae |
|
|
List bone cells and functions
|
osteoblasts - formation of new bone (osteoid)
osteoclasts - resportion of bone osteocytes - maintaining bone matrix |
|
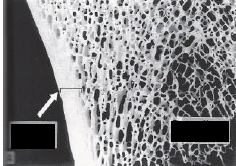
Label this diagram
|
Left - compact bone
Right - cancellous bone (spongy) |
|
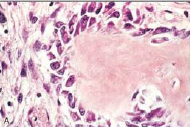
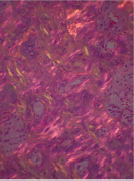
Which cells are these? What are their function?
|
Osteoblasts
Synthesize type I collagen, proteoglycans and glycoproteins for bone matrix Line up on the edges of bone resembling columnar epithelium The new bone they are laying down is called OSTEOID, which will then be calcified |
|
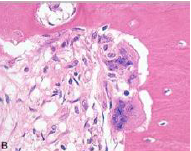
Which cells are these? What are their function?
|
Osteoclasts
Large, branched, motile, multinucleated cells Osteoclasts secret substances which digest collagen and dissolve calcium crystals |
|
|
What is lamellar bone?
|
Bone with collagen fivers that are arranged in highly ordered sheets or layers; pattern of arrangement is responsible for typical appearance in polarized light
|
|
|
What is woven bone?
|
Comes before lamellar bone
More haphazard pattern of collagen organization |
|

Which type of bone is this? (lamellar or woven?)
|
Lamellar!
Fully-formed, organized bone |
|
What kind of bone is this? (lamellar or woven?)
|
Woven!
New bone - disorganized |
|
What kind of bone is this? (lamellar or woven?)
|
Primary bone = WOVEN!
temporary, first formed either replaced by lamellar bone or resorbed to form marrow cavity found in growing skeletons under age 5 and in repair of fracture |
|
|
What are dysostoses?
|
Congenital malformations in bone - including aplasia of an appendage or supernumary bones
May be caused by genetic alterations that affect transcription factors (HOMEOBOX GENES) |
|

What kind of birth defect does Thalidomide cause? (see picture)
|
-phocomelia (among others0
-anomaly in which hands & feet are attached to shortened arms and legs |
|

What bone disease does this child most likely have? Describe.
|
Osteogenesis imperfecta (OI): group of disease associated with defects in extracellular structural proteins
-deficiency in synthesis of type I collagen! -muts affect genes that encode alpha 1 and 2 chains of collagen |
|
|
What are the different types of OI?
|
Type I: multiple fractures, normal lifespan; blue sclerae, hearing loss, misshapen teeth
Type II: fatal form; numerous fractures in utero & pulmonary hypoplasia due to chest compression b/c of multiple fractures; Also, types III, IV which were not covered extensively and are rarer |
|
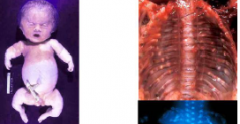
What type of OI is this?
|
Type 2 - fatal, fetal
The phenotype can be caused by mutation in either the COL1A1 gene on chromosome 17 or the COL1A2 gene on 7 As a result of faulty collagen I bone formation is markedly impaired The fetus suffers many fractures in utero The newborn has pulmonary hypoplasia as a result of chest compression Growth zones are normal but spicules in metaphysis are thin and cartilaginous |
|
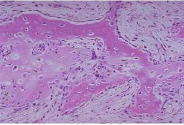
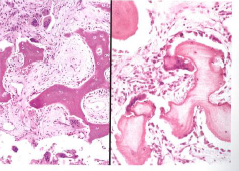
What type of OI do you see in the attached slide?
|
Type II, lethal
|
|

What type of OI do you see in the attached slide?
|
Type II, lethal
|
|
|
Describe achondroplasia.
|
- caused by defects in signal transduction mechanisms
- AD trait, 80% de novo muts - point mut in FGFR3 --> constitutive inactivation and inhibition of chondrocyte proliferation - homozygotes --> fetal or neonatal death due to pulmonary hypoplasia |
|
|
Describe thanatophoric dwarfism (dysplasia)
|
- caused by defects in signal transduction mechanisms
-pt mut in FGFR3, which is different than achondroplasia - lethal condition - Heterozygotes have limb shortening, frontal bossing of the skull, and a small thorax |
|

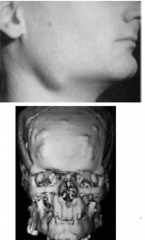
What disease does this child have? (note telephone receiver arms)
|
Thanatophoric dysplasia
Note: growth zone is disorganized and retarded in histo |
|
|
Describe OSTEOPETROSIS
|
- AKA Marble bone disease or Albers-Schoenberg disease
- associated with a defect in ion channels - responsible mutations (e.g.CA2 gene encoding carbonic anhydrase II) interfere with acidification of the osteoclast resorption pit - several other genes have also been implicated in the development of this disorder -disease results in deficient osteoclast activity with dense bones seen on x-ray. -medulla is filled with primary spongiosa -deposited bone is not remodeled, and the bone that is present is brittle and subject to fracture -variant with cloverleaf skull |
|
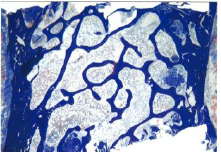
What disease does this slide depict?
|
OsteoPETROSIS
|
|
|
Describe osteoporosis
|
-common, characterized by dec bone mass and progressive discontinuity of bone architecture --> structural failures and increased likelihood of fracture
- both primary and secondary causes osteoporosis - T-score assesses bone mineral density; peak during young adulthood, influenced by heredity, physical activity, muscle strength, nutrition and hormonal status - once max skeletal mass achieved, deficit accrues with each bone resorption and bone formation cycle - number of sequelae of menopause and aging --> further bone loss and development of osteopor. |
|
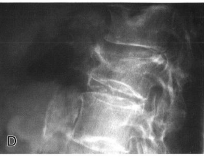
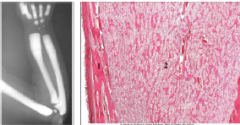
Radiological findings in osteoporosis - spine
|
Spine x-ray: shows diminished mineralization of verterbral bodies w/ anterior compression fracture of middle vertebral body
Vertebral body on right is shortened by compression fractures |
|
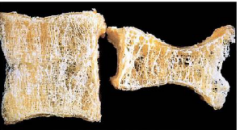
What disease is at work here? Which is normal and which is diseased?
|
Osteoporotic vertebral body (right) shortened
by compression fractures, compared with a normal vertebral body. Note that the osteoporotic vertebra has a characteristic loss of horizontal trabeculae and thickened vertical trabeculae |
|
|
What are primary and secondary causes of osteoporosis?
|
Primary
Postmenopausal Senile Idiopathic Secondary Endocrine disorders Neoplasia Gastrointestinal Drugs Others |
|
|
What is a T-score in osteoporosis?
|
Difference between a patient’s bone mineral density (BMD) and BMD at same site in health young adults matched for gender and ethnicity
T> -1.0 (Normal) T< -2.5 (Osteoporosis) T score between normal and osteoporosis = Osteopenia |
|
Is this normal or abnormal?
|
Normal iliac crest
|
|

Which disease is this?
|
Osteoporosis
|
|
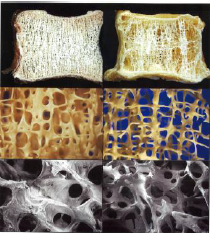
Which side is normal and which side has osteoporosis?
|
R - osteoporosis
L - normal |
|
|
Describe Paget disease
|
aka osteitis deformans
- common, starts in mid age - osteoclast dysfunction - single bone or entire skeleton - frontal bossing + bowing of legs - affected area is enlarged and sclerotic with irregular thickening of both cortical and cancellous bone -easy fracture, and there is an increased incidence of benign and malignant bone tumors, including osteogenic sarcomas. |
|
|
What are the 3 phases of Paget's disease?
|
3 phases;
1) early (osteolytic phase) - paratrabecular fibrosis, osteocastic activity, NO OSTEOBLAST action 2) mixed phase: Osteoclastic-osteoblastic with latter predominant 3) osteosclerosis (burnt out): thickened bone w/ mosaic pattern and prominent cement lines; hypervascular, and inc blood flow acts like ateriovenous shunt --> high output cardiac failure |
|
|
Where does Paget's occur? (which bones?)
|
Mono- or poly-ostotic
• Pelvis (70%), femur (55%), lumbar spine (53%), skull (42%), tibia (32%) |
|

What disease do these people have?
|
Paget's
|
|

What disease is shown in this radionuclide scan?
|
Pagets - hot spots of bone remodeling
|
|

What bone caused the tibia, here, to be bowed and the affected area is enlarged and sclerotic?
|
Paget's
|
|
What disease is this? What phase of the disease?
|
EARLY Paget's disease
|
|
What disease is this? What phase of the disease?
|
LATE (osteosclerotic) Paget's disease
|
|
|
Genetics of Paget's disease.
|
15% have + family history
Mutations of SQSTM1 gene that encodes p62 Mutations in 50% patients with familial and 5-10% patients with sporadic disease p62 plays a key role in function of osteoclasts Other genes involved in osteoclast function may also be involved |
|
|
Describe rickets/osteomalacia.
|
- most commonly caused by deficiency of Ca and vitmin D
- palisading pattern of cartilage at growth plate is lost - bowing of legs due to formation of poorly mineralized bone - excess unmineralized bone - osteoid |
|
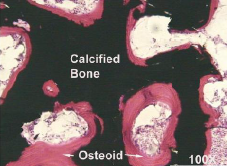
What disease is this?
|
Rickets/osteomalacia
A characteristic feature of osteomalacia is an excess of unmineralized bone (osteoid) which appears pink in this image, while calcified bone appears black |
|
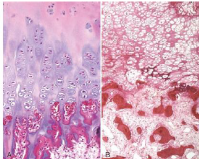
What disease is this?
|
Rickets/osteomalacia
In rickets (right), the palisading pattern of cartilage at the growth plate is lost, as compared to normal (panel A) |
|
|
Describe hyperparathyroidism.
|
- increased OSTEOCLASTIC activity (cortical > cancellous)
- dissecting osteitis - tunneling of cancellous bone by fibrous tissue with increased osteoclasts - loss of bone --> microfractures w/ ingrowth of macrophages and fibrous tissue - large numbers of giant cells w/ hemorrhage and hemosiderin pigment --> brown tumor |
|
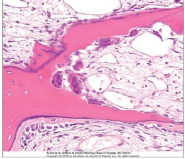
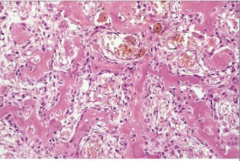
What disease causes this finding?
|
Hyperparathyroidism - note osteoclasts dissecting a trabeculum; osteoblastic activity is also increased
- cortices will be thin and dissections --> railroad track pattern on x-ray |
|
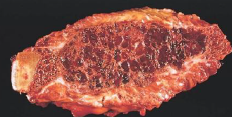
What is this?
|
Brown tumor (from a rib)
Hyperparathyroidism Undergoes cystic degeneration |
|
|
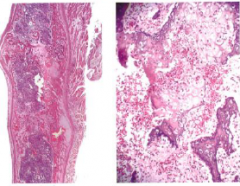
Describe fracture healing.
|
- healing (formation of callus) occurs quickly and after some months it may be impossible to distinguish an old fracture from normal bone
- if ends of bone fail to attach properly --> synovial cells may line non-united surfaces --> pseudosarthrosis - @ about 10 days after fracture (left), there is a highly cellular stroma w/ foci of early osteoid matrix formation; by 14 days (right), there is cartilage matrix formation together with bone and fibrous tissue - increased woven bone are then formed --> mature lamellar bone |
|
|
Steps of fracture healing
|
Hematoma --> Organization --> Soft tissue callus (pro-callus) --> SUBPERIOSTEAL woven bone (produced by activated osteoprogenitor cells) --> Cartilage formation (from activated mesenchymal cells) --> ENDOCHONDRAL OSSIFICATION (bony
callus) --> Remodeling of bone |
|
What is depicted in this picture?
|
Fracture site healing 1-2 weeks
|
|
What kind of bone is this? (lamellar vs woven?)
|
Woven! aka primary bone
- temporary, first formed - either replaced by lamellar bone or resorbed to form marrow cavity |
|
What is shown here?
|
Non-union fracture site pseudoarthorsis
- inadequate immobilization --> delayed union or non-union - pseudoarthrosis (central portion of callus undergoes cystic degeneration and can become lined by synovium-like cells) |
|
|
What is avascular necrosis? (osteonecrosis)
|
- development of ischemic necrosis of bone
- spares cortical bone, but when subchondral bone is involved --> collapse of boney structures --> osteoarthritis - mostly after fractures or due to steroids - other causes- primary vascular disease, caisson disease, sickle cell disease & Gaucher disease |
|
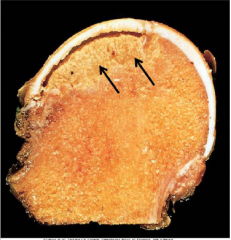
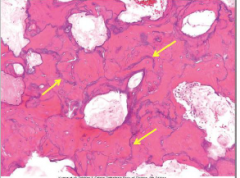
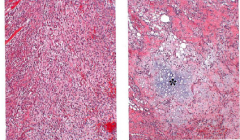
What is shown in this image?
|
Avascular necrosis of the femoral head
Note subchondral wedge of necrotic yellow tissue (arrows) |
|
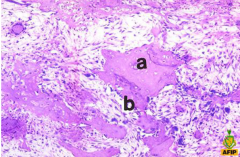
What is shown in this image?
|
Avascular necrosis
Creeping substitution is simultaneous removal of necrotic bone (a) and replacement w/ newly formed, woven bone (b) More basophilic woven bone is termed juxtaposed bone |
|
|
What is osteomyelitis
|
- inflammatory bone disease
- mostly infection - S. Aureus (Salmonella in SSD) - reach bone by hematogenous routes, local extension, direct implant - bacteria can extend to overlying periosteum w/ formation of subperiosteal abscess and draining sinus - bone in center undergoes necrosis (loss of nuclei) = sequestrum; - extension from epiphysis to adjacent joint --> suppurative arthritis; w/i bone acute phase then reparative phase w/ formation of fibrous tissue and new bone - reactive bone = involucrum - new bone around fragments of dead bone - squamous cell carcinoma may develop adjacent to sinus if long case |
|
|
What is the sequestrum of osteomyelitis?
|

See image - dead bone in the middle of healing osteomyelitis
The bone in the center of the inflammation undergoes necrosis (characterized by loss of nuclei), forming a sequestrum |
|
|
What is the involucrum of osteomyelitis?
|
Within the bone, the acute phase is followed by a reparative phase with the formation of fibrous tissue and new bone. The reactive bone is called an involucrum.
|
|
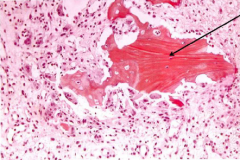
What disease is this?
|
Osteomyelitis - ACUTE
Arrow = necrotic bone |
|
What disease is this?
|
Osteomyelitis - SUBACUTE and CHRONIC
Arrow = necrotic bone |
|
What disease is this?
|
Osteomyelitis - CHRONIC, HEALING
Viable bone overlying necrotic bone Arrows = visible bone |
|

What disease is this? What is it a comlication of?
|

Squamous cell carcinoma as a result of chronic osteomyelitis
|
|
|
What are the major bone forming tumors?
|
Osteomas, osteoid osteomas/osteoblastomas, osteosarcomas
|
|
|
Describe osteomas
|
-Composed of admixtures of lamellar and woven bone
-often solitary , aside from those in Gardener syndrome (AD, intestinal adenomas, osteomas, desmoid tumors, lipomas) |
|
|
Describe osteoid osteomas
|
- < 2cm
- 10-20yrs peak - cortex of proximal femur and tibia and circumscribed lesions - central part of lesion (nidus) is radiolucent, but may becme calcified, while surrounding bone is sclerotic - pain relieved by aspirin |
|
What disease is this?
|
Osteoma
|
|
What disease is this?
|
Osteoid osteoma
|
|
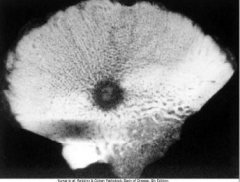
What disease is this?
|
Osteoid osteoma on x-ray
Intracortical osteoid osteoma Dark lesion is the tumor (nidus) Center of lesion - mineralization Reactive bone formation surrounds the lesion |
|
|
Describe osteoblastomas
|
>2cm
Same mortphology as osteoid osteomas Vertebral column |
|
|
Describe osteosarcomas
|
- malignant tumors
- bimodal age distribution - metaphysis of long bones, particularly around knee joint - muts in RB gene in > 70% of sporadic cases - patients w/ hereditary retinoblastoma >1000x inc risk - muts in p53 also found in those with sporadic tumors & those w/ Li Fraumenia syndrome - gray white tumors with areas of necrosis, hemorrhage and cyst formation - pleomorphic cells w/ numerous mitosis - must make mineralized or non-mineralized osteoid - some make cartilage (chondroblastic osteogenic sarcoma) - met to lung, other bones - limb sparing surgery + chem --> 90% survival |
|
What is this?
|
Osteoblastoma
Benign tumor with similar histology to osteoid osteoma but tumor > 2cm More likely to involve spine |
|
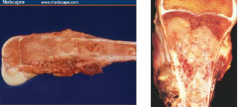
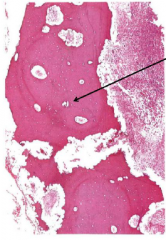
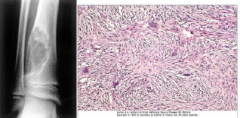
What disease is this?
|
Osteosarcoma
Grossly: gritty, gray-white, areas of hemorrhage, sometimes cystic degeneration Can destroy cortex and extend into soft tissue |
|
What disease is this?
|
Osteosarcoma
Malignant bone forming tumor Bimodal age distribution -Biggest peak in patients under 20 -Smaller peak in older patients most of whom have a pre-existing condition such as Paget, bone infarct, history of radiation or chronic osteomyelitis Most commonly arise in metaphysis of long bones-one half at the knee Osteosarcoma-Genetics Frequent mutation of 2 genes—RB and p53 Patients with germline mutations of RB have 1000 fold increase in incidence of osteosarcoma Patients with germline mutation of p53 (Li-Fraumeni syndrome) also susceptible For the dog lovers, high incidence on large dogs. This together with the fact that most lesions are associated with growth plates may suggest that normal proliferation of osteoblasts may lead to mutations in some individuals |
|
|
Osteosarcoma - prognosis and treatment
|
- mets occur; most to lung but also to other bone, brain
- chemo + limb sparing surgery; 5-yr survival 80-90% (up from 10-20%) |
|
|
What are the cartilage forming tumors?
|
Osteochondromas, chondromas, chorndrosarcomas
|
|
|
Describe osteochondromas
|
- common, peak at 10-30 yrs
- develop from metaphysis of long tubular bones - most solitary, some with hereditary exostosis have multiple - cap of lesion is composed of hyaline cartilage while inner portion of head and stalk is newly formed bone |
|
|
What are chondromas?
|
- composed of mature hyaline cartilage
- when develop in medullary regions of bone - enchondromas - lesions developing from surfaces of bone = juxtacortical chondromas - Ollier syndrome = multiple, on 1 side of body - Maffucci syndrome = multiple, soft tissue angiomas |
|
|
Describe chondrosarcomas
|
- sholuder, pelvis, proximal femur, ribs
- 40-60yrs old - medullary cavities - glistening appearance on cut section - atypical chondrocytes w/ variable amounts of surrounding cartilaginous matrix - well differentiated = good prognosis; poorly differentiated = < favorable prognosis, hi likely of mets |
|

What do these pictures depict?
|
Osteochondroma
From L --> R 1) X-ray of osteochondroma arising from posterior aspect of tibia 2) CT scan - fibula to left, tibia to right and tumor in middle attached to tibia; note continuity of tumor with tibia 3) A sessile osteochondroma w/ cap of hyaline cartilage showing enchondrial ossification 4) Catilage cap - disorganized growth plate |
|
What is this?
|
Chondroma
an enchondroma showing a nodule of hyaline cartilage surrounded by a thin layer of reactive bone. In the syndromes there may be sufficient atypia in the cells to raise the question of chondrosarcoma |
|

What is this?
|
Enchondroma
Tumors of hyaline cartilage Arise in enchondral bones -Enchondromas arise in medulla -Suberiostal or juextacorical chondromas arise on surface of bone Ollier syndrome -Multiple enchondromas Maffuci syndrome -Enchondromatosis associated with soft tissue hemangiomas |
|
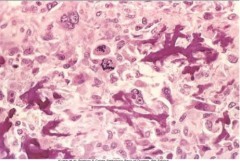
What do these images depict?
|
Conventional chondrosarcoma
Left: intramedullary tumor growing thru cortex to form soft tissue mass Right: anaplastic chondrocytes |
|
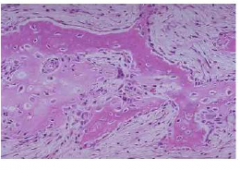
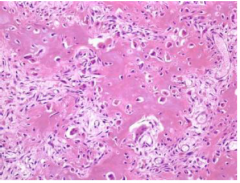
What does this depict?
|
A fibrous cortical defect
Storiform pattern of benign spindle cells and occassional osteoclast-type giant cells |
|
|
What are fibrous tumors?
|
- include fibrous cortical defects/non-ossifying fibroma, fibrosarcoma, fibrous dysplasia
|
|
|
Describe fibrous cortical defects
|
- 50% of children > 2
- most in metaphysis of long bones, multiple, <.5 cm - swirling arrays of fibroblasts (storiform arrangement) together w/ scattered osteoclast-like giant cells - larger (>3-5cm) = non-ossifying fibromas |
|
|
Describe fibrosarcoma
|
- malignant tumor derived from fibroblasts
- after middle age - either de novo (in metaphysis) or from pre-existing bone condition (Paget) - large tumors, often extend into surrounding soft tissues - lo grade tumors often w/ lots of collagen, while high grade have little collagen - hi grade --> met to lungs |
|
|
Describe fibrous dysplasia.
|
- benign tumor-like condition
- 3 forms: 1) monostotic (70%) - single bone 2) polyostotic (27%) - multiple bones, NO endocrine dysfunction; 3) polyostotic + cafe au lait pigmentation + endocrineopathies (3%) - radiologically: raidionlucenciences w/ cortical thinning and ground glass appearance - grossly, medullary cavities replaced w/ dense white tissue - microscopically, curvilinear trabeculae of woven bone + fibrous stroma |
|

What does this x-ray depict?
|
Fibrous dysplasia
x-rays are from 2 different patients with involvement of the femur (left) and humerus (right) |
|
|
What is depicted here?
|
Fibrous dysplasia
Microscopically, there are curvilinear tabeculae of woven bone surrounded by a fibrous stroma. |
|

What disease is this?
|
Fibrous dysplasia
|
|
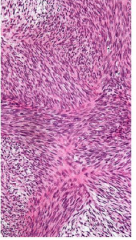
What disease is this?
|
Fibrosarcoma
• Mostly in middle-aged and elderly • Usually arise denovo but, just as in osteosarcoma, some develop in prior lesions such as bone infarcts, previously radiated tissue or Paget disease. • Can also arise in previously benign tumors. |
|
What disease is this?
|
Fibrosarcoma - thigh mass in middle-aged male
• Mostly in middle-aged and elderly • Usually arise denovo but, just as in osteosarcoma, some develop in prior lesions such as bone infarcts, previously radiated tissue or Paget disease. • Can also arise in previously benign tumors. |
|
|
Describe Ewing sarcoma
|
aka primitive neuroectodermal tumor
pediatric 6-10% of primary bone tumors • 2nd most common bone sarcoma of children • Diaphysis of long tubular bones and pelvis • Pain, fever, increased sedimentation rate • 11;22 (q 24: q 12) Translocation EWS (22) and FLI1 (11) |
|
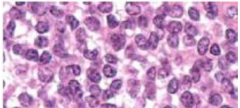
What tumor is this?
|
Ewing sarcoma
|
|

What tumor is this
|
Ewing sarcoma
|
|
|
Describe giant cell tumors.
|
- arise in epiphysis of long bones and have peack incidence between 20-40yrs
locally aggressive and rarely met to lungs aka osteoclastoma "benign" tumor of midlife large red-brown tumors |
|
|
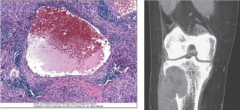
What tumor is this?
|
MRI of GIANT CELL TUOR
tumor replaces femoral condyle and extends to subchondral bone plate sheets of multinucleate giant cells and mononuclear stromal cells locally aggressive and rarely met to lungs |
|
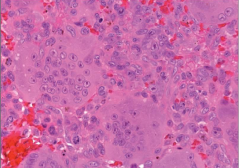
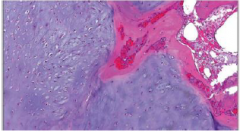
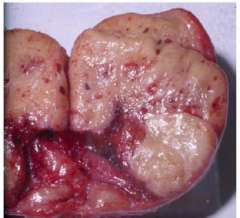
What tumor is this?
|
Giant cell tumor
aka osteoclastoma "benign" tumor of midlife large red-brown tumors |
|
|
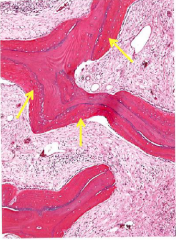
Describe aneurysmal bone cysts
|
- rapidly developing but benign tumors that have peak incidence in first 20 yrs
- radiologically, look slike large lytic lesion - multiloculated blood-filled cystic spaces - walls are composed of fibroblasts, multinuc osteoclast like cells, woven bone |
|
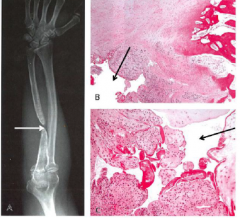
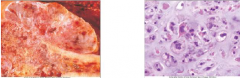
What is this?
|
Aneurysmal bone cyst
Blood-filled central space Wall contains proliferating fibroblasts, osteoclast-like giant cells and reactive woven bone Right: ABC of tibia |

