![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
8 Cards in this Set
- Front
- Back
|
Describe the process of intramembranous ossification
|

-is the process by which most of the flat bones are formed
1. Mesenchymal cells, in the presence of a vascular zone, condense into primary ossification centers, differentiate into osteoblasts & begin secreting osteoid 2. As calcification occurs, osteoblasts become trapped in their own matrix & become osteocytes. These centers of developing bone are called trabeculae (fused spicules) 3. Fusion of the bony trabeculae produces spongy bone as blood vessels invade the area and other undifferentiated mesenchymal cells give rise to bone marrow 4. The periosteum & endosteum develop from portions of the mesenchymal layer that do not undergo ossification 5. Mitotic activity of the mesenchymal cells gives rise to osteoprogenitor cells, which undergo cell division and form more osteoprogenitor cells or differentiate into osteoblasts within the inner layer of the developing periosteum |
|
|
Describe the process of endochondral ossification
|

ENDOCHONDRAL OSSIFICATION
-is the process by which long bones are formed -it begins in a segment of hyaline cartilage that serves as a small model for the bone -the 2 stages of endochondral bone formation involve the development of primary & secondary centers of ossification PRIMARY CENTER OF OSSIFICATION -the primary center of ossification develops at the midriff of the diaphysis of the hyaline cartilage model by the following sequence of events: 1) Vascularization of the perichondrium at this site causes the transformation of chondrogenic cells to osteoprogenito cells, which differentiate into osteoblasts. This region of the perichondrium is now called the periosteum 2) Osteoblasts elaborate matrix deep to the periosteum, and via intramembranous bone formation, form the subperiosteal bone collar 3) Chondrocytes within the core of the cartilaginous model undergo hypertrophy and degenerate, and their lacunae become confluent, forming large cavities (eventual marrow spaces) 4) Osteoclasts create perforation in the bone collar that permit the periosteal bud (blood vessels, osteoprogenitor cells, and mesencymal cells) to enter the newly formed spaces in the cartilaginous model. The cartilage that constitutes the walls of these spaces becomes calcified 5) Newly developed osteoblasts elaborate bone matrix that becomes calcified on the surface of the calcified cartilage model, forming a calcified cartilage-calcified bone complex. In histological sections, the calcified cartilage stains basophilic, whereas the calcified bone stains acidophilic 6) The superiosteal bone collar becomes thicker and elongates toward the epiphysis 7) Osteoclasts begin to resorb the calcified cartilage-calcified bone complex, thus enlarging the primitive marrow cavity 8) Repetition of this sequence of events results in bone formation spreading toward the epiphysis SECONDARY CENTERS OF OSSIFICATION -develop at the epiphyses in a sequence of events similar to that described for the primary center, except a bone collar is not formed 1) Development of these centers begins when osteoprogenitor cells invade the epiphysis and differentiate into osteoblasts, which elaborate bone matrix to replace the disintegrating cartilage. When the epiphyses are filled with bone tissue, cartilage remains in 2 areas, the articular surfaces & the epiphyseal plates 2) Articular cartilage persists and does not contribute to bone formation 3) Epiphyseal plates continue to grow by adding new cartilage at the epiphyseal end while it is being replaced with bone at the diaphyseal end (lengthening the bone) |
|
|
What are the zones of the epiphyseal plate?
|
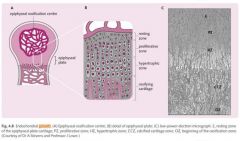
ZONES OF THE EPIPHYSEAL PLATES:
✦Zone of Reserve Cartilage: is at the epiphyseal side of the plate. It possesses small, randomly arranged inactive chondrocytes ✦Zone of Proliferation (of chondrocytes): is a region of rapid mitotic divisions giving rise to rows of isogenous groups ✦Zone of Cell Hypertrophy & Maturation: is the region where the chondrocytes are greatly enlarged ✦Zone of Calcification: is the region where hypertrophied chondrocytes die and the cartilage becomes calcified ✦Zone of Ossification is the area where newly formed osteoblasts elaborate bone matrix on the calcified cartilage, forming a calcified cartilage-calcified bone complex which is resorbed & replaced by bone |
|
|
Describe the regulation of endochondral ossification
|
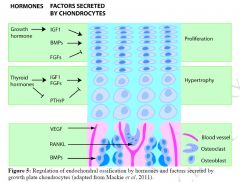
PROLIFERATION:
STIMULATED BY: Growth hormone which acts through insulin-like growth factor-1 (IGF-1) secreted by the liver & secreted locally by chondrocytes AND by locally produced bone morphogenic proteins (BMPs) INHIBITED BY: Fibroblast growth factor (FGF) CARTILAGE MATRIX SECRETION STIMULATED BY: IGF-1 & BMPs HYPERTROPHY: STIMULATED BY: Thyroid hormones, acting through release by chondrocytes of IGFs and FGFs, and through inhibition of release by chondrocytes of parathyroid hormone-related peptide (PTHrP, which acts through the same receptor as PTH to suppress chondrocyte hypertrophy) |
|
|
What regulates the behavior of invading cells?
|
-regulated by secreted factors by chondrocytes:
*vascular endothelial growth factor (VEFG) stimulates angiogenesis and invasion of blood vessels into cartilage *BMP stimulates osteoblast differentiation from bone marrow stromal cells *receptor activator of NF-κB ligand (RANKL, found on osteoblasts) stimulates osteoclast differentiation |
|
|
How do we model bone?
|
-shaping of bone during growth or in response to changing mechanical loads
-occurs because of formation by osteoblastic activity and resorption by osteoclastic activity |
|
|
Describe the process of bone remodeling
|
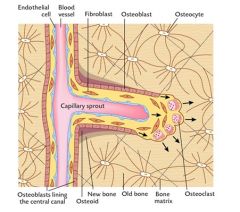
-osteoclasts resorb bone & create new Haversian canal in the old bone, while osteoblasts divide and line the new canal
-the osteoblasts form osteoid and new bone that adjusts the diameter of the canal -all the Haversian canals contain blood vessels & nerves |
|
|
Describe the regulation of bone cell behavior during modeling, remodeling, repair and pathology
|
OSTEOBLASTIC activity stimulated by:
-sex steroid hormones (estrogen, testosterone), BMPs, other growth factors -mechanical load -inflammatory cytokines & prostaglandins OSTEOCLASTIC activity stimulated by: -PTH (calcitonin homeostasis, especially during pregnancy & lactation) -mechanical unloading (rest periods following training – horses) -inflammatory cytokines & prostaglandins -most of these effected mediated by osteoblasts – hormones & cytokines stimulate RANKL expression in osteoblasts |

