![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
What is Bone |
Consists of a mineralised collagen matrix which is very rigid and strong while still retaining some degree of flexibility |
|
|
Functions of bone |
Resistance to compression : inorganic content Resistance to tension - organic matrix Houses bone marrow Calcium homeostasis |
|
|
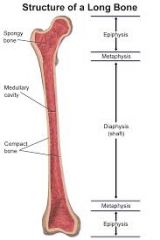
Long Bone - Anatomy |
|
|
|
Macroscopic organisation of Bone |
Cortical - 70% compact - mostly at diaphysis Trabecular - 30% cancellous, medullary bone, mostly at epiphysis |
|
|
Compact/ cortical bone |
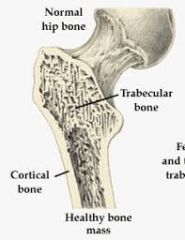
Provides most structural support Resists bending stresses, ,thicker at mid part bone |
|
|
Cortical bone - microscopic structure |
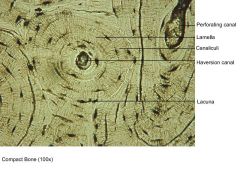
Osteons/ Haversian canals - bone cylinders - 8-15 concentric lamellae - axis parallel to long axis of bone - central cavity w/ blood vessels and nerve Volkmann's canals - carry blood vessels from periosteum to Havarian system |
|
|
Microscopic structure of cancellous/trabecular bone |
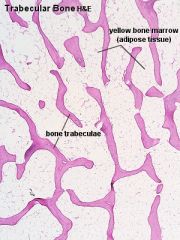
Found incide cortices Forms interconnecting network of plates/trabeculae Provides large SA for metabolic functions |
|
|
Function of cancellous/trabecular bone |
Provides strength w/o disadvantage of weight Organisation of trabecular plates is w/ purpose Arranged along lines of maximum mechanical stress, allows transmission of weight More metabolically active than cortical bone - larger surface area |
|
|
Composition of Bone |
Bone - 65% inorganic --> calcium hydroxypatite 35% organic (osteoid) --> type I collagen and non collagenous proteins |
|
|
Osteoid |
Unmineralised bone matrix Type I collagen (90%) Non collagenous proteins - osteocalcin - osteonectin - osteopontin - growth factors |
|
|
Bone Matrix - microscopic organisation |
Lamellar bone - Type I collagen fibres laid down in parallel sheets/lamellae, very stringn structurally Woven bone - collagen fibres randomally arranged produced when bone is being rapidly produced |
|
|
Name the four types of bone cells |
Osteoblasts - bone forming cells, secrete osteoid Osteocytes - a mature osteoblast surrounded by bone matrix Osteoclasts - function in resorption and degradation of existing bone Osteoprogenitor cells - osteoblast precursors |
|
|
What do osteoblasts derive from |
Osteoprogenitor cells Formation and proliferation of preosteoblast cells requires signalling through the Wnt-frizzled-Lrp5-B-catenin signalling pathway Osteoblast differentiation is controlled by transcription factors Runx2 and osterix w/o either of these no osteoblasts are formed |
|
|
Osteoblast function |
Produce and deposit osteoid Regulate osteoclast differentiation/ function - RANK ligand - RANK interaction |
|
|
Osteoblast Fate |
Life span 6 months - osteoid production - 10-15% entombed in bone - osteoctyes - others die by apoptosis or differentiate into bone lining cells |
|
|
What are the most common cell in bone |
Osteocytes Residue in lacunae in bone - connect to other osteocytes, osteoblasts and osteoclasts via long cytoplasmic processes |
|
|
Function of osteocyte |
Regulation of bone remodelling in response to local or systemic signals |
|
|
What does RANKL signalling do |
increases osteoclast formation |
|
|
Sclerostin signalling ? |
Inhibits osteoblast formation Production inhibited by PTH and mechanical loading PTH - rapid calcium release (osteocytic, osteolysis) |
|
|
What are osteoclasts |
Monocyte/macrophage derived multinucleate giant cells |
|
|
What regulates osteoclasts formmation |
Growth factors and RANK-RANKL interactions - M-CSF and TNF produced by stroma cells induces expression of RANK RANK-RANKL interactions induce precursor cell function and increase osteoclast activity |
|
|
What is osteoprotegerin |
Decoy receptor that binds RANKL and inhibits osteoclast formation |
|
|
How do osteoclasts resorb bone |
Production of acid to release calcium Proteases releassed to breakdown organic matrix |
|
|
Name two markers for bone formation |
Type I collagen fragments Tartrate-resistant acid phosphatase |
|
|
What is intramembranous ossification |
Osteoid laid down within loose fibroconnective tissue of a fibrous membrane Formation of skull, maxilla parts of clavicle, mandible Fracture repair Bone trabeculae formed directly from mesenchyme - woven bone, grow by appositional osteoid deposition, susbequentlly remodelled Subperiosteal bone growth |
|
|
What is endochondral ossification? |
Osteoid deposited on cartilage scaffolds - development of most of the skeleton - growth plates - fracture repair Programmed changes in chrondocyte - hypertrophy - matrix vesicles - type X collage - chondrocyte death |
|
|
Process of Intramembranous Ossification |
Mesenchymal stem cell proliferation --> formation of cluster/nodule --> differentiation into osteoblasts - formation of ossification centre --> production of osteoid (woven) --> mineralilsation of matrix --> osteoblasts embedded in matrix - osteocytes --> blood vessels become entrapped/ grow in --> bone remodelled into lamellar trabecular bone |
|
|
Primary centre of ossification |
Genetically predetermined sites and times of ossification in diaphyses of cartilage bone in utero - perichondrium transforms to perichondrium - formation of bony collar - chondrocyte hypertrophy - matrix calcification - osteoprogeinitor and blood vessel ingrowth |
|
|
Secondary Centre of Ossification |
Ossification in epiphysis at or after birth Similar process to that of primary centre formation Line of cartilage btwn primary and secondary centres = epiphyseal plate |
|
|
Epiphyseal Growth Plate |
Site of continued endochondral ossification during growth Longitudinal growth |
|
|
Cessation of Bone growth |
Growth stops when epiphyseal growth plates close Varies at different sites Genetically determined Under control of pituitary gland |
|
|
What is achondroplasia? |
Mutation in fibroblast growth factor receptor 3 (FGFR3) Decreased chondrocyte proliferation and hypertrophy |
|
|
What is gigantism |
Excess growth hormone production before puberty |
|
|
What maintains a healthy skeleton? |
Bone remodelling Removal of small bone increments and which are replaced by the same amount of bone Maintains mechanical integrity of skeleton - removal of microdamaged bone - reinforcement of bone in areas subject to increased stress Calcium homeostasis |
|
|
Bone remodelling Cycle |
Activation --> Resorption --> Reversal --> Formation/ Mineralisation |
|
|
What regulates bone remodelling? |
Mechanical Loads Systemic Hormones - PTH - Vit D - Endocrine Hormones Locally produced cytokines |
|
|
Activation of bone remodelling cycle |
Bone lining cells - become rounded, expose bone, secrete collagenase Osteoclasts recruited - differentiate from mononucleate precursors, RANK ligand - RANK interactions Control - microfractures - RANKL and sclerostin secretion by osteocytes Mechanical stresses |
|
|
What regulates Osteoclast Formation and Activity |
Activated following binding to RANKL, expressed stromal cells osteocytes and osteoblasts Osteoprotergerin blocks RANK-RANKL interactions |
|
|
Bone Remodelling Cycle - Resorption |
Osteoclasts adhere to bone via integrins Form ruffled border, secrete acid and proteases Produce biomarkers, tartrate resistant acid phosphate 5B also bsp, ctx, pyd osteoclasts die by apoptosis replaced by mononuclear cells |
|
|
Reversal of bone remodelling cycle |
Osteoblasts differentiate from bone marrow stromal cells Roles of osteoclasts - release of bone matrix derived factors - EphrinB2-EphB4 increased OB differentiation S1P - increased OB migration and survival |
|
|
Bone Remodelling Cycle - Formation |
osteoblasts lay down osteoid
osteocyte formation - scerostin - inhibitory factor for bone formation |
|
|
Bone Mineralisation |
75% occurs over several days Ca/PO4 ratio of hydroxyapatite changes w/ time |
|
|
Systemic regulation of bone mineralisation |
Regulation of Ca2+ and phosphate levels - FGF23 . osteocytes and osteoblasts . increases Pi secretion . Decreases PTH and Vit d levels - PTH - Vit D |
|
|
When is Peak Bone Mass achieved |
Young adulthood Determined by: - genetic factors - physical activity - muscle strength - diet = calcium intake during adolescence - hormonal state |
|
|
What is osteoporosis? |
Progressive bone disease characterised by a decrease in bone mass and density which can lead to an incnreased risk of fracture |
|
|
Osteoporotic bone |
Cortical - thinner Trabecular - struts thinner and less connected Normally mineralised Mechanically weak |
|
|
Osteoporotic Features |
Radius - colles fracture Neck of femur Vertebrae - crush, wedge |
|
|
Pathology of Paget's Disease of Bone |
Abonormal bone remodelling - lytic, mixed and sclerotic Clinical features - weak deformed bones nerve compression Radiology - lytic and sclerotic changes X-ray changes Exaggerated bone remodellling - lytic, mixed and sclerotic phases |
|
|
Osteopetrosis |
Marble bone disease and Albers-Schonberg disease Hard dense bone decrease in number and activity of osteoclasts Number of causes - carbonic anhydrase II deficiency, CSF-1 signalling abnormalities, chloride channel mutations |
|
|
Primary hyperparathyroidism |
Parathyroid adenoma results in increased PTH production |
|
|
Secondary hyperparathyroidism |
Chronic renal disease low serum calcium phosphate induce parathyroid hyperplasa |
|
|
Bone changes of hyperparathyroidism |
Increased bone turnover - increased osteoclastic, osteoblastic activity, peritrabecular fibrosis Serum calcium increased - phosphate decreased - Alk Phos increased |
|
|
Vitamin D metabolism |
Source of Vit d2 = skin, requires sunlight,, dietary intake Hydroxylation |
|
|
Causes of vitamin D deficiency |
Lack of sunlight Dietart Gastro-intestinal disease - malabsorption LIver disease Kidney disease |
|
|
Vitamin D deficiency - Bone Effects |
Osteomalacia - decreased mineralisation of bone Rickets - decreased Ca2+/ Vit/D in childhood soft bones that deform and fracture easily serum calcium decreased |

