![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
What type of ossification do bones of axial skeleton, appendicular skeleton and base of skull have? |
Endochondral Ossification |
|
|
What is Endochondral Ossification? |
Cartilaginous model of bone is first made by chondrocytes → osteoclast/osteoblast later replace with woven bone and then remodel to lamellar bone |
|
|
In adults, what type of bone occurs after fractures? In what disease we can see this? |
Woven Bone. In Paget disease of bone. |
|
|
What type of ossification is defective in Achondroplasia? |
Endochondral Ossification |
|
|
What type of ossification do bones of calvarium and facial bones have? |
Membranous ossification |
|
|
What is membranous ossification? |
Woven bone formed directly without cartilage → later remodeled to lamellar bone. |
|
|
What osteoblast do? How they do it? |
Builds bone by secreting collagen and catalyzing mineralization in alkaline environment via ALP. |
|
|
What osteoclast do? How they do it? |
Dissolve bone by secreting H+ and collagenases. |
|
|
What PTH do? How it works? From where it's secreted? |
Parathyroid Hotmone: At low, intermittent levels, exerts anabolic effects (building bone) on osteoblast and osteoclast (indirect). |
|
|
What happens to the bone if there is an ↑ in PTH? |
↑PTH = catabolic effects (osteitis fibrosa cystica) --Seen in 1° hyperparathyroidism |
|
|
What role do estrogen has in bone formation? |
Inhibits apoptosis in bone-forming osteoblast and induces apoptosis in bone-resorbing osteoclast. |
|
|
What happens to the bone in estrogen deficiency? What may cause estrogen deficiency? |
Excess cycles of remodeling, and bone resorption lead to osteoporosis. --Surgical removal of ovaries or menopause |
|
|
What mutation is seen in achondroplasia? |
Fibroblast growth factor receptor 3 (FGFR-3) |
|
|
Is achondroplasia is related with maternal or paternal advance age? |
Paternal advance age |
|
|
What fails in achondroplasia that manifiest in the affected individual? |
Failure of longitudinal bone growth (endochondral ossification) → short limbs |
|
|
Which ossification is not affected in achondroplasia? |
Membranous ossification Large head relative to limbs. |
|
|
If an heterozygote achondroplastic patient married another heterozygote individual and have children, what percentage might develop achondroplasia? |
Heterozygote Individual A= mutation a= wild type AA= 25% Homozygote mutation → Death in utero Aa= 50% Heterozygote mutation → Achondroplasia aa= Normal individual |
|
|
If an heterozygote achondroplastic patient married a non-achondroplastic individual and have children, what percentage might develop achondroplasia? |
Heterozygote indivual A= mutation a= wild type Aa= 50% heterozygote mutation → Achondroplasia aa= 50% normal individual |
|
|
Do achondroplastic patient have normal fertility and life expectancy? |
Yes, they do. Delivery must be in a C-section |
|
|
What percentage do mutation in achondroplasia occurs sporadically? |
Up to 85%. |
|
|
Bone disease 2° to drugs (eg, steroids, alcohol, anticonvulsant, anticoagulants, thyroid replacement therapy) |
Osteoporosis |
|
|
Bone disease due to ↑ bone resorption related to ↓ estrogen levels |
Osteoporosis |
|
|
What happens to the bone in osteoporosis? |
Trabecular (spongy) and cortical bone loss mass and interconnections despite normal bone mineralization and lab values (Ca2+ and PO4-) |
|
|
How is the lab values (Ca2+, PO4-, AP, PTH) in osteoporosis? |
All normal. |
|
|
What medical conditions are associated with osteoporosis? |
Hyperparathyroidism Hyperthyroidism Multiple Myeloma Malabsorption syndrome |
|
|
How can osteoporosis be diagnosed? |
DEXA scan: Dual-Energy X-ray Absorptiometry with a T-Score of ≤ 2.5 or by fragility fracture of hip or vertebra. |
|
|
What measure can be taken to prevent osteoporosis? |
Exercise (weight-bearing) Calcium and Vitamin D intake Avoid Smoking and Alcohol Watch out/Discontinous glucocorticoids, PPI, H2-blockers |
|
|
How can osteoporosis be treated? |
Biphosphonates (eg, alendronate) PTH analog (eg, teriparatide) SERMS (eg, raloxifene) RANKL Antibody (eg, denosumab) |
|
|
What is Colles fracture? In what disease it can be seen? |
Fracture distal radius. Osteoporosis |
|
|
What fractures can be seen in osteoporosis? |
Hip fracture / Femoral Neck Vertebra fracture Distal radius fracture (Colles) |
|
|
Acute back pain + loss of height + kyphosis |
Osteoporosis |
|
|
Pancytopenia + thickened, dense bone + Cranial Nerve palsie |
Osteopetrosis |
|
|
Bone disease with mutation in carbonic anhydrase II |
Osteopetrosis |
|
|
Bone disease due to failure of normal bone resorption (eg osteoclast failure) |
Osteopetrosis |
|
|
Bone disease where bone marrow space is filled with bone tissue → Pancytopenia and extramedullary hematopoiesis |
Osteopetrosis |
|
|
Bone-in-Bone ("stone" bone) appearance on X-ray |
Osteopetrosis |
|
|
What treat is definitively in osteopetrosis? |
Bone marrow trasnplant as osteoclast are derive from monocytes |
|
|
From which cell are osteoclast derived? |
Monocytes |
|
|
How are the lab values (Ca2+, PO4-, PTH, AP) in osteopetrosis? |
All normal but maybe ans slightly ↑AP |
|
|
Bone disease with defective mineralization of osteoid or cartilagenous growth plates |
Osteomalacia or Rickets |
|
|
Most common cause of Osteomalacia/Rickets |
Vitamin D deficiency |
|
|
X-rays shows osteopenia and "Looser zones" |
Osteomalacia/Rickets "Looser zones" → pseudofractures |
|
|
Bone disease with bowing of legs, bead-like costochondral junctions and soft skull |
Rickets Costocondral junctions → rachitic rosary Craniotabes → soft skull |
|
|
How are the lab values (Ca2+, PO4-, AP, PTH) in Osteomalacia/Rickets? |
↓ Vitamin D = ↓Ca2+ → ↑PTH → ↓PO4- ↑AP (hyperactivity of osteoblast - bone turnover) |
|
|
Bone disease where localized disorder of bone remodeling is caused by ↑osteoclastic activity follwed by ↑osteoblastic activity that forms poor-quality bone. |
Paget disease of bone |
|
|
Long bone chalk-stick fracture on X-ray |
Paget disease of bone |
|
|
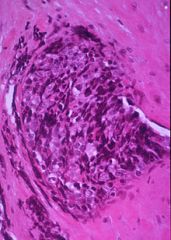
Bone disease with mosaic pattern of woven and lamellar bone (osteocytes with lacunar in chaotic juxtapositions) |
Paget diseas of bone |
|
|
How are the lab values (Ca2+, PO4-, PTH, AP) seen in Paget disease of bone? |
Serum Ca2+, PO4-, and PTH are normal. Only AP is increase! |
|
|
Mention the stages of Paget disease of bone. |
Lytic = osteoclast Mixed = osteoclast + osteoblast Sclerotic = Osteoblast Quiescent = minimalosteoclast/osteoblast activity |
|
|
With what neoplasia is Paget disease of bone might be associated? |
Osteosarcoma (osteogenic sarcoma) |
|
|
How does Paget disease of bone can cause heart failure? |
Sometimes ↑blood flow from ↑arteriovenous shunts may cause high-output heart failure |
|
|
A patient comes complaining that he lost his hearing gradually. He also mention that he can wear his hats anymore because the are getting smaller. What disease you might suspect? |
Paget disease of bone |
|
|
What artery is comprised in osteonecrosis? |
Medial circumflex femoral artery |
|
|
What is the common site affected in osteonecrosis? |
Femoral head. |
|
|
What may cause osteonecrosis? |
CAST Bent LEGS Corticosteroids Alcoholism Sickle cell Trauma "The Bends" (caisson/decompression disease) LEgg-Calvé-Perthes disease (idiopathic) Gaucher disease Slipped capital femoral epiphysis |
|
|
From what artery does medial circumflex femoral artery may be branched? |
Profunda femoris artery or occasionally from the femoral artery. |
|

|
"Soap bubble" appearance. Giant cell tumor. |
|

|
Bony exocitosis with cartilaginous (chondroid) cap. Osteochondroma. |
|

|
Codman triangle (from elevation of periostium) Osteosarcoma (osteogenic sarcoma) |
|

|
Codman traingle (from elevation of periostium) Osteosarcoma (osteogenic sarcoma) |
|

|
Sunburst pattern Osteosarcoma (osteogenic sarcoma) |
|

|
"Onion skinning" appearance Ewing sarcoma |
|
|
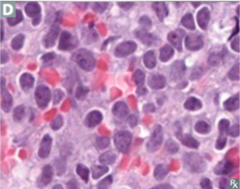
Anaplastic small blue cell malignant tumor. Ewing Sarcoma |
|
|
Anaplastic small blue cell malignant tumor. Ewing sarcoma |
|
|
Ewing sarcoma is associated with what translocation? |
t11;22 causing fusion protein EWS-FLI 1 |
|
|
Bone Tumor Age Association: A male less than 25 years old → ? Pt between 20 - 40 years old → ? A boy less than 15 years old → ? Bimodal distribution (10-20; >65 years old) → ? |
Males < 25 y/o → Osteochondroma Pt 20 - 40 y/o → Giant cell tumor Boy < 15 y/o → Ewing sarcoma Bimodal distribution → Osteosarcoma |
|
|
What are the predisposing factor of osteosarcoma? |
Paget disease of bone Bone infarcts Radiation Familial retinoblastoma Li-Fraumeni syndrome |
|
|
Most common benign bone tumor |
Osteochondroma |
|
|
Most common malignant bone tumor in children |
Osteosarcoma |
|
|
Common localization of bone tumor: 1.Metaphysis of long bone (often aroung the knee) 2. Diaphysis of long bone, pelvis, scapula, ribs 3.Epiphyseal end of long bones (often arounf the knee) |
1.Osteosarcoma 2.Ewing sarcoma 3.Giant cell tumor |
|
|
What tumor may metastasized to the bone? |
Prostate, Renal cell cancer, Testes, Thyroid, Lungs, Breast |
|
|
What type of lesion can do metastasic bone tumor? What tumor can cause it? What is the common presentation? |
Lytic = destroy bone --Breast, Lung Blastic = abnormal formation --Prostate Presentation: Bone pain, epidural spinal crod compression, hypercalcemia |

