![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
Epiphysis, metaphysis and diaphysis. What are these? |
Epiphyses = the ends of a typical long bone. Diaphysis = shaft of long bone. Metaphyses = the region at each end between the diaphysis and epiphysis. |
|
|
Are bones solid? |
NO. They have a structure of outer cortical (compact) bone, and inner cancellous (spongy) bone, with a medullary cavity in the diaphysis. |
|
|
What is found in the medullary cavity? |
Bone marrow |
|
|
There are two types of marrow. What are they and what are the differences? |
Red marrow = haematopoeietic Yellow marrow = adipose - the body's 'last resort' store of triglycerides to be used as energy in the last stages of starvation |
|
|
The ___________ is the outer fibrous covering of the bone |
The periosteum is the outer fibrous covering of the bone |
|
|
The __________ is the inner lining of the bone |
The endosteum is the inner lining of the bone |
|
|
Bones are very vascular. How do blood vessels enter? |
Via holes called nutrient foramina |
|
|
What is the difference between fatigue and monotonic failure? |
Fatigue = small repeated stress over time Monotonic failure = a single catastrophic trauma |
|
|
Bones have several functions, depending on location. Apart from supporting the body and resisting compression/torsion/shear/tension forces, what are other functions of bones in the body? |
-Filtering air (nasal turbinates) -Transmitting vibrations (malleus, incus, stapes) -Protective space for soft organs (skull, ribs) -Fatigue life and monotonic strength -Attachment for ligaments/tendons -Sites of articulation - to allow motion |
|
|
BONE MODELLING |
In response to stress - bone deposition and/or resorption - results in an overall change in the shape of the bone |
|
|
BONE REMODELLING |
Normal physiological turnover of bone matrix - resorption and deposition of bone with no overall shape change. Repairs fatigue damage. |
|
|
What type is collagen is found in bone? (BONUS QS: Where else is this type found?) |
Type I collagen (35%) Provides tensile strength (Also found in fibrocartilage) |
|
|
The bone matrix is a composite of FOUR things. What are they? |
(1) Type I collagen (35%, tensile) (2) Hydroxyapatite mineral (60%, compressive) (3) Water (4%) (4) Proteoglycans (1%) |
|
|
What is osteoid? |
Osteoblasts obviously can't secrete hard, mineralised bone. So they secrete osteoid - all the composition of bone, but without the mineral part (more watery, instead). This is then mineralised to become bone matrix. |
|
|
Osteoblasts become osteocytes. TRUE or FALSE? |
TRUE. Osteoblasts (derived from MSCs) secrete osteoid on to bone surface. Bury themselves in osteoid. Then become osteocytes, sitting inside a lacuna. |
|
|
What is the function of osteocytes? |
Mature cell of bone. Maintains local bone mineralisation. (Some research points to them having a function in sensing mechanical load, but this is controversial.) |
|
|
What is the function of osteoclasts? |
Resorb bone. Derived from haematopoeitic tissue - similar to a macrophage. Large multinucleated cells, with a ruffled border (increase surface area for resorption). Secretes HCl to dissolve mineral, and proteases to break down collagen. |
|
|
CHOOSE THE CORRECT WORD: There is a high/low level of communication between the different bone cells (osteoblasts/cytes/clasts). |
There is a HIGH level of communication between the different bone cells. |
|
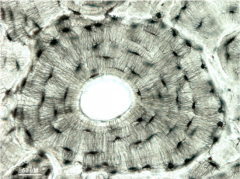
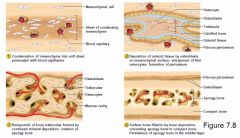
This is an osteon, the fundamental functional unit of bone. Describe its structure. |
Osteocytes (black dots) - cell bodies in lacunae - contact each other via long processes called canaliculi (many thin lines radiating out from central Haversian canal, which contains blood vessel). The concentric layers of compact bone are called lamellae. |
|
|
Do osteoclasts bind to and resorb unmineralised or mineralised bone? |
Mineralised bone only. |
|
|
There is crosstalk between osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells). What are the main signalling factors? |
Osteoblasts secrete M-CSF and express surface RANKL, which bind to a receptors on osteoclast progenitors. This stimulates them to become active osteoclasts. |
|
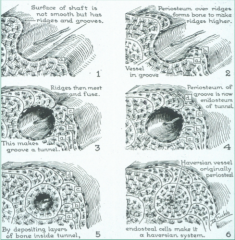
What is a primary osteon? |
They increase the diameter of diaphysis... ...by subperiosteal bone deposition... ...which leaves periosteal blood vessels buried inside the osteonal tunnels (Haversian canals). |
|
|
What is a secondary osteon? |
During bone remodelling... ...osteoclasts burrow through bone, resorbing it... ...followed by osteoblasts laying down new bone... ...creating a new osteon (Haversian structure of concentric lamellae). |
|
|
How can you distinguish a secondary osteon from a primary osteon? |
Secondary osteon will have a ruffled border, where the osteoclastic resorption took place before the new bone was laid down. |
|
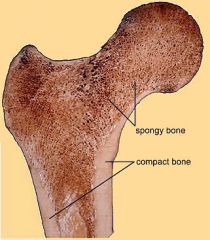
What are the two main arrangements of bone tissue? |
Spongy/trabecular/cancellous bone Compact bone (notes: BOTH are made of osteons!) |
|
|
Osteoblasts align to mechanical forces. What does this mean for the collagen they secrete? |
Collagen is secreted in line with the strain field. This results in a regional variation in collagen orientation - transverse in compression, longitudinal in tension. |
|
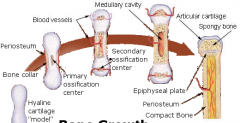
What is endochondral ossification? |
One of two key methods of fetal bone tissue growth. Starts with a cartilage template, and bone is formed at two ossification centres (primary = diaphysis; secondary = epiphyses). |
|
What is intramembranous ossification? |
Growth of bone without a cartilage template. Bone forms directly within mesenchyme. E.g. the flat bones of the skull. |
|
|
One of the endocrine functions of bone is calcium regulation. Which two opposing hormones act on bone to regulate calcium release into blood? |
PTH (parathyroid hormone), when blood Ca is low: stimulates osteoblasts to express RANKL, which stimulates osteoclasts - INCREASES bone resorption - RELEASES Ca into blood. Calcitonin (from thyroid gland), when blood Ca is high - inhibits osteoclasts - STOPS THE RELEASE of Ca into blood. |
|
|
How is vitamin D involved in calcium regulation? |
Active vitamin D is released by kidney in response to PTH (low blood Ca). It enhances Ca absorption in the gut until blood Ca levels are normalised, signalling PTH hormone release to slow down. Not enough vitamin D = PTH pulling MORE Ca from bone into blood. |

