![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
223 Cards in this Set
- Front
- Back
|
What is the inheritance of Neurofibromatosis type 1?
|
AD mutation in chromosome 17 neurofibromin tumor suppresor gene
|
|
|
What percentage of patients with NF 1 have new mutations?
|
50%
|
|
|
What is the mutaiton/abnormality in Neurofibromatosis type 2?
|
merlin chromosome 20
|
|
|
What is the second most common tumor in NF 1?
|
optic nerve glioma
|
|
|
What ocular feature is associated with NF 2?
|
subcapsular cataracts
|
|
What are the imaging features for vestibular schwannoma (NF 2)
|
hypo or iso intense on T1 with intense enhancement post contrast
|
|
|
What are the criteria for diagnosis of NF 2?
|
1 of following:
1. Bilateral vestibular schwannoma 2. 1st degree relative with NF2 and a) unilateral vest. schwann or b) any two of MSGNsubcapsular cataracts 3. Unilateral vestibular schwan and any two of MSGNC 4. multiple meningiomas and unilat vest schwannoma or any 2 of: SGNC |
|
|
What is the etiology/ inheritance of tuberous sclerosis?
|
AD hamartin or tuberin chromosome 9 or 16 (tuberin on 16 is also contiguous to gene for PCKD)
|
|
|
What is Vogt's triad assoc. with TS?
|
seizures
mr adenoma sebaceum (only present in 1/3) |
|
|
What percentage of patients with NF2 have posterior subcapsular cataracts?
|
85%
|
|
|
What percentage of patients with NF have NF1?
|
96%
|
|
|
What are some characteristics of patients with tuberous sclerosis?
|
1) cortical tubers
2) subependymal nodules SEGA (foramen of monroe) 3) skin findings; adenoma sebaceum, ungual fibromas, ash leaf spots, shagreen patches 4) renal disease -tumors 5) seizures in 95% 6) MR 7)propensity for intracranial aneurysms 8) heart- rhabdomyomas and dysrhythmias 9) Lungs- female-lymphangioleiomyomatosis recurrent spontaneous pneumothorax not involved: peripheral nerves, nerve roots, muscles |
|
|
What are the criteria for diagnosis of TS?
|
Definite:2 major & 1 minor
Probable: 1 major & 1 minor Possible: 1 major or 2 minor |
|
|
What are the major criteria for diagnosis of TS?
|
1) facial angiofibroma
b) ungual fibroma c) more than 3 hypomel macules 4) shagreen patches 5) cortical tuber 6) subependymal nodule 7) SEGA 8)retinal hamartomas 9) cardiac rhabdomyoma 10) lymphangioleiomyomatosis 11) renal angiomyolipoma |
|
|
What are the minor criteria for TS?
|
a) enamel pits multiple
b) hamartomatous rectal polyps c) bone csts d) cerebral white matter migration tracts? e) gingival fibromas f) nonrenal hemartomas g)retinal achromic patch h) confetti skin lesions i) multiple renal cysts |
|
|
What is the characteristic EEG finding associated with TS?
|
hypsarrhythmia
|
|
|
What are the criteria for diagnosis of NF 2?
|
1 of following:
1. Bilateral vestibular schwannoma 2. 1st degree relative with NF2 and a) unilateral vest. schwann or b) any two of MSGNsubcapsular cataracts 3. Unilateral vestibular schwan and any two of MSGNC 4. multiple meningiomas and unilat vest schwannoma or any 2 of: SGNC |
|
|
What is the etiology/ inheritance of tuberous sclerosis?
|
AD hamartin or tuberin chromosome 9 or 16 (tuberin on 16 is also contiguous to gene for PCKD)
|
|
|
What is Vogt's triad assoc. with TS?
|
seizures
mr adenoma sebaceum (only present in 1/3) |
|
|
What percentage of patients with NF2 have posterior subcapsular cataracts?
|
85%
|
|
|
What percentage of patients with NF have NF1?
|
96%
|
|
|
What are treatment options for patients with TS?
|
vigabatrin or ACTH
|
|
|
What EEG finding may be associated with TS?
|
hypsarrhythmia
|
|
|
What is Sturge-Weber syndrome?
|
port-wine stain nevus in distribution of CN V ophthalmic with ipsilateral leptomeningeal angiomatosis and seizures (95%)
|
|
|
What are some reasons that patients with Sturge-Weber should have yearly ophthalmologic examinations?
|
1) glaucoma if the port-wine stain involves the eyelids
2) choroid hemangioma 3) bupthalmos (enlarged eye) 4) hemianopsia (40%) b/c of location of lm angio |
|
|
What are the usual presentations of leptomeningeal angiomatosis besides seizures?
|
cerebral iscehmia due to a "steal phenomenon" and headaches
|
|

What are the intracranial findings associated with this patients?
|

Sturge weber
leptomeningeal angiomatosis sz, h/a, ischemia, dev delay, hemiparesis, hemianopsia (40%) |
|
What are the characteristic imaging findings associated with SW-syndrome?
|
calcifications on CT
occipital lobe predilection and more uncommonly involvement of frontal lobe with atrophy |
|
|
What is Osler-Webber-Rendu disease?
|
autosomal dominant with multiple telangiectasias mucocutaneous (epistaxis, GI bleeding) and neurologic symptoms arise from AVM or aneurysms
|
|
|
What are some features that should prompt consideration of HHT?
|
multiple cerebral malformation, spinal avm, aneurysm, cavernous angiomas ischemic stroke can bedue to pulmonary AV fistula (should have antibiotics for dental or surgical procedures to prevent brain abcess
|
|
|
What is Osler-Webber-Rendu disease?
|
autosomal dominant with multiple telangiectasias mucocutaneous (epistaxis, GI bleeding) and neurologic symptoms arise from AVM or aneurysms
|
|
|
What are some features that should prompt consideration of HHT?
|
multiple cerebral malformation, spinal avm, aneurysm, cavernous angiomas ischemic stroke can bedue to pulmonary AV fistula (should have antibiotics for dental or surgical procedures to prevent brain abcess
|
|
This finding of mucocutaneous telangiectasia in a patient could lead to consideration of what diagnosis?
|

hereditary hemorrhagic telangiectasia or osler-weber-rendu disease
|
|
|
What is incontinentia pigmentosa?
|
X linked dominant disorder characterized by skin, hair, teeth, eye and neurologic findings
|
|
|
What are some of the skin findings associated with incontinentia pigmentosa?
|
marble-like rash that follows specific stages 1-bullous 2- verrucous 3-hyperpigmented 4-atrophic/hypopigmented
|
|
|
What are the teeth findings associated with incontinentia pigmentosa
|
conical teeth
|
|
|
What are the eye findings associated with IP?
|
neovascularization, vitreal hemorrhage, retinal detachment, (35%)
|
|
|
What are the neurologic findings associated with IP?
|
less than 25% have manifestations including MR or seizures (<13%)
|
|

These teeth findings could prompt consideration of what neurocutaneous syndrome?
|

incontinentia pigmentosa
|
|

Besides these characteristic skin findings, these patients can have involvement of neurologic, ocular, hair and teeth as well.
|

incontinentia pigmentosa bullous stage
|
|
|
What is von-hippel lindau disease?
|
AD chromosome 3 disorder characterized by retinal/neurologic/spinal cord hemangioblastomas, renal tumors, pancreatic tumors, pheochromoctyoma
(tumor suppressor gene) |
|
|
What monitoring should be done for patients with Von Hippel Lindau disease?
|
yearly optho exams
blood pressure plasma catecholamines and after age 10 abdominal CT screening |
|
|
What percentage of VHL patients have new mutations?
|
20%
|
|
|
What is cerebrotendinous xanthomatosis?
|
AR disorder characterized by xanthomas, demyelination, chornic diarrhea, bilateral cataracts, neuropathy
|
|
|
What findings would be seen in patients with Cerebrotendinous xanthomatosis in metabolic screening?
|
increased plama and bile cholestanol level
increased urinary bile alcohol glucoronides with decreased biliary concentration of chenodeoxycholic acid, normal lipoprotein profile |
|
|
What is the abnormality in cerebrotendinous xanthomatosis?
|
mitochondrial sterol 27-hjydroxylase deficiency eading to impaired hepatic conversion of cholesterol to cholic and chenodeoxycholic acids
|
|
|
What neurologic symptoms may lead to consideration of Ehlers Danlos?
|
spontaneous rupture or dissection of arteries, carotid-cavernous fistulas, intracranial aneurysms
|
|
|
What is the abnormality in pseudoxanthoma elasticum?
|
ATP binding casette membraneAR disorder
Eye Skin CV Cerebrovascular disease |
|

Which neurocutaneous disease is this verrucous abnormality found in?
|

Incontinentia pigmenti
|
|

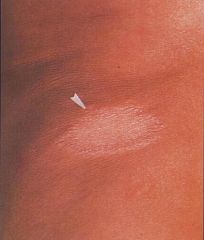
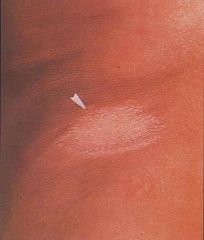
what disease is this characteristic skin finding associated with?
|

pseudoxanthoma elasticum
|
|
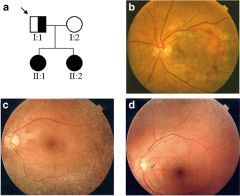
What disease is this peau d'orange appearance of retina associated with?
|
pseudoxantoma elasticum
|
|
|
What are the clinical findings assoc with pseudoxanthoma elasticum?
|
skin: plucked chicken, neck
eye: peau d'orange retina, hemorrhages CV: early atherosclerosis, sudden death, claudication, renovascular disease, MVP/MVS neuro: occlusion, atherosclerosis intracranial and aneurysms |
|
|
What is the abnormality in Menke's syndrome?
|
X linked recessive, associated with abnormality in copper metabolism with low copper and low ceruloplasmin
|
|
|
What are hte clinical findings associated with menke's syndrome?
|
thalamic degen, brain atrophy
seizures, delayed devlopment pili torti twisted hair blindness subdural hematoma most die before 2 |
|

This finding can be caused by low copper and this syndrome
|

Menke's kinky hair disease
|
|
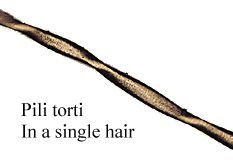
Menke's disease may have this abnormality of hair
|
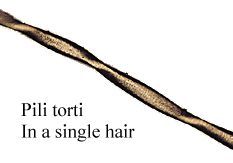
pili torti
|
|

What are the manifestations associated with epidermal nevi syndrome?
|

nervous-mr, ssz
ocular cv renal skeletal malignancy |
|
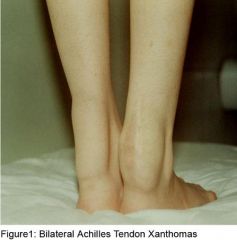
This finding associated with axonal neuropathy, progressive neurologic deterioration could consider what syndrome?
|
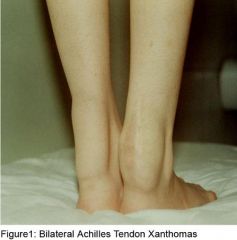
cerebrotendinous xanthomatosis
|
|

This disease is caused by what abnormality?
|

AR disease gene product usually nucleotide excision repair in DNA damaged by UV radiation
|
|
|
What are the manifeswtations of xeroderma pigmentosa?
|
Skin: freckling, blistering, snburn, basal cell carcinoma (less common melanoma/sq cell carcinoma)
eyes: corneal keratitis, cancer, ocular melanom, telagniectasia Neuro: MR, ataxia, spasticity, abnormal ocular motility, senosirneural deafness, sz, axonal neuropathy malignancy: cause of death in 33% of patients by age10-14 50% have Ca |
|
|
What is hypomelanosis of Ito? Incontinentiia pigmenti achromians
|
2rd most common neurocutaneous disorder
|
|
|
What neurology sx are assoc with hypomelanosis of ITo?
|
sz, mr, autism, abnl head growth, mr
|
|

What percentage of patients with giant melanocytic nevi may develop neurocutaneous melanosis?
|

2.5%
|
|
|
What clinical features are associated with neurocutaneous melanosis?
|
the melanin can deposit in the pia and arachnoid leading to hydrocephalus, seizures, cranial nerve abnl, papilledema, myelopathy, cauda equina syndrome, ICH, SAH
|
|
|
What is the inheritance of neurocutaneous melanosis?
|
completely sporadic due to failure of neural crest cells to differentiate to melanocytes
|
|

What disease is associated with these findings in a bathing trunk distribution?
|

Fabry's disease
|
|
|
What is the mode of inheritance of Fabry's disesae?
|
X linked recessive lyusosomal stroage disease deficiency of alpha-galactosidase A
|
|
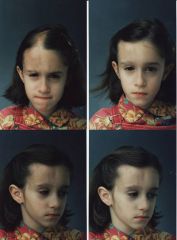
What is parry romberg syndrome?
|
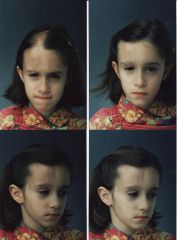
progressive hemifacial atrophy in distribution of CN V
|
|
|
What is ataxia telangiectasia?
|
autosomal recessive, slowly progressive ataxia, telangiectasia, variable immunodeficiency and ionizing radiation sensitivity
|
|
|
What is abnormal in ataxia telagniectasia?
|
AR mutation of ATM AT mutant gene on chromosome 11
|
|
|
What are the clinical features of Marchiafavi Bignami disease?
|
dementia
dysarthria weakness seizures incontinence |
|
|
What is the risk of conversion to MS after demyelinating event in 10 years with a) no MRI lesions b) 1 lesion c) 2 lesions?
|
a) 15%
b) 50% c) 90% |
|
|
What is the target of NMO antibodies?
|
aquaporin 4
|
|
|
What is the rate of monophasic versus recurrent disease in NMO?
|
monophasic 33%
recurrent 67% |
|
|
Which type of NMO has better prognosis?
|
monophasic NMO
|
|
|
What are the features of systemic lupus erythematosus?
|
malar rash/photosensitivity
uveitis oral ulcers arthritis nephropathy pleuritis pericarditis/Libmann Sacks endocarditis uveitis anemia/thrombocytopenia/leukopenia neurologc |
|
|
What percentage of SLE patients dev neuropsych manifestations?
|
50%
|
|
|
What are some of the neuromuscular manifestations of SLE?
|
neuropathy distal symmetric
mononeuritis multiplex radiculopathy/polyradiculopath myelopathy cranial neuropathy (optic, trigemnial) |
|
|
What rheumatologic disease may present with movement disorders such as parkinsonism, ataxia or chorea?
|
Lupus, Antiphospholipid syndrome
|
|
|
What connective tissue diseases may cause a distal symmetric axonal polyneuropathy (sensory) or sensorimotor?
|
1) SLE
2) RA 3) Sjogren's 4) Wegener's 5) Churg Strauss 6) Neuro-Behcet's 7) PAN (asymmetric polyneuropathy) 8) buerger's disease (Scleroderma, Takayasu's, Temporal arteritis does not) |
|
|
What connective tissue d/o should be considered in differential for cranial neuropathies?
|
a) SLE
b) Sjogren's c) wegener's granulomatosis d) churg strauss e) PAN f) Neuro-behcet's g) temporal arteritis (ocular) h) scleroderma |
|
|
What connective tissue d/o should be considered in differential for myopathy?
|
a) SLE
b)Temporal arteritis (50% have PMR) c) RA- treatment related (penicillamine) d) Behcet's e) Wegener's f) PAN g) mixed connective tissue disease |
|
|
What are the clinical findings assoc with Takaysu's arteritis?
|
large vessel arteriopathy (no neuromuscular)
|
|
|
What CNS findings are assoc. with RA?
|
very rare, but could have myelopathy due to atlantoaxial subluxation
|
|
|
What CNS findings are associated with scleroderma?
|
rare
|
|
|
What features are asssociated with Wegener's granulomatosis?
|
upper & lower airway lesions (granuloma)
glomerulonephritis ear |
|
|
What CNS findings are assoc with WG?
|
encephalopathy
cranial neuropathies (cav sinus, pituitary) ICH headache aseptic meningitis uncommon vasculitis |
|
|
What type of vessels are affected with WG?
|
small vessels
|
|
|
What are the features assoc with Churg-Strauss?
|
upper respiratory, skin, heart
|
|
|
What are the CNS findings associated with Churg-Strauss?
|
necrotizing vasculitis with predilection for hemorrhage
|
|
|
What ethnicities have a high incidence of neuro-Behcet's disease?
|
"silk road"
highest in turkey Japan, Korea, Middle East, Mediterrenean |
|
|
What CNS findings are associated with Behcet's?
|
venous thrombosis
aspetic mening headache myelopathy brainstem/cranial nerve peripheral nerves, myopathy CNS arterial(dissection, stenosis, aneurysm) |
|
|
What percentage of patients with neurosarcoidosis have muscle involvement?
|
50%
|
|
|
What CNS findings are associated with neurosarcoid?
|
cranial neuropathies (facial most common)
meningoencephalitis aseptic meningitis intracranial parenchymal disease spinal cord parenchymal disease symmetric distal polyneuropathy/polyradiculonuropathy myopathy |
|
|
What groups of patients should have added coverage for Listeria monocytogenes?
|
elderly
immunocompromised alcoholics or pregnancy infants |
|
|
What 3 antibiotics could cover suspected pseudomonas mening?
|
cefepime
ceftazidime meropenem |
|
|
What groups of patients should have added coverage for Listeria monocytogenes?
|
elderly
immunocompromised alcoholics or pregnancy infants |
|
|
What percentage of blood cultures are positive in bacterial meningitis ?
|
50%
|
|
|
What is recommended regarding treatment with steroids and bacterial meningitis?
|
For adults patients should receive Dexamethasone 10 mg IV every 6 hours for 4 days
|
|
|
What 3 antibiotics could cover suspected pseudomonas mening?
|
cefepime
ceftazidime meropenem |
|
|
What groups of patients should have added coverage for Listeria monocytogenes?
|
elderly
immunocompromised alcoholics or pregnancy infants |
|
|
What type of prophylaxis should people in contact with meningococcal meningitis receive?
|
chemoprophylaxis with rifampin
|
|
|
What percentage of blood cultures are positive in bacterial meningitis ?
|
50%
|
|
|
What 3 antibiotics could cover suspected pseudomonas mening?
|
cefepime
ceftazidime meropenem |
|
|
What is recommended regarding treatment with steroids and bacterial meningitis?
|
For adults patients should receive Dexamethasone 10 mg IV every 6 hours for 4 days
|
|
|
What type of prophylaxis should people in contact with meningococcal meningitis receive?
|
chemoprophylaxis with rifampin
|
|
|
What percentage of blood cultures are positive in bacterial meningitis ?
|
50%
|
|
|
What is recommended regarding treatment with steroids and bacterial meningitis?
|
For adults patients should receive Dexamethasone 10 mg IV every 6 hours for 4 days
|
|
|
What type of prophylaxis should people in contact with meningococcal meningitis receive?
|
chemoprophylaxis with rifampin
|
|
|
What are the main mechanisms that bacterial abcess can from intracranially?
|
hematogenous spread
direct contiguous spread seeding due to trauma |
|
|
What are the main mechanisms that bacterial abcess can from intracranially?
|
hematogenous spread
direct contiguous spread seeding due to trauma |
|
|
What are the most comon pathogens for abcess?
|
streptococci and anaerobes
|
|
|
What are the most comon pathogens for abcess?
|
streptococci and anaerobes
|
|
|
What are the main mechanisms that bacterial abcess can from intracranially?
|
hematogenous spread
direct contiguous spread seeding due to trauma |
|
|
What are the usual pathogens of epidural abcess?
|
staphylococcus aureas, aerobes, anerobes and gram negative organisms
|
|
|
What are the usual pathogens of epidural abcess?
|
staphylococcus aureas, aerobes, anerobes and gram negative organisms
|
|
|
What are the most comon pathogens for abcess?
|
streptococci and anaerobes
|
|
|
What are hte usual pathogens for subudral empyema?
|
aerobic, microaerophilic and anaerobic streptococci
|
|
|
What are hte usual pathogens for subudral empyema?
|
aerobic, microaerophilic and anaerobic streptococci
|
|
|
What are the usual pathogens of epidural abcess?
|
staphylococcus aureas, aerobes, anerobes and gram negative organisms
|
|
|
What are hte usual pathogens for spinal epidural abcess?
|
staphylococcus aureus, gram negative rods and streptococci
|
|
|
What are hte usual pathogens for spinal epidural abcess?
|
staphylococcus aureus, gram negative rods and streptococci
|
|
|
What are hte usual pathogens for subudral empyema?
|
aerobic, microaerophilic and anaerobic streptococci
|
|
|
What are hte usual pathogens for spinal epidural abcess?
|
staphylococcus aureus, gram negative rods and streptococci
|
|
|
What is the most common location for spinal epidural abcess?
|
thoracic spine
|
|
|
What type of pateitns are suspecptible to neisseria meningitidis?
|
complement deficiency
|
|
|
What regions are prone to lyme disease?
|
northeast, midwest and northwest us
|
|
|
What are the characteristic features of the 3 phases of lyme disease?
|
1st stage: target like rash with migrating red ring (erythema migrans)
2nd stage: h/a, stiff neck, aseptic meningiits radiul, CN, PN, Plexopathy 3rd stage: neuropsych, mild encpehalopathy |
|
|
What is the treatment for neuroborreliosis?
|
ceftriaxone intravenous
|
|
|
What is the time frame for the 2 stages of lyme disease?
|
1st stage: 3-32 days
2nd stage: several weeks after rash 3rd stage: many months after second stage |
|

What is this rash characteristic of?
|

Early stage of lyme disease
erythema chronicum migrans |
|
|
What are the 3 stages of syphillis characterized by?
|
1st stage: painless chancre
2nd stage: syphilitic meningitis: h/a,n/v,meningismus, sz, cranial neuropathies (generalized infxn, rash, etc.) 3rd stage: a) Tabes dorsalis b) meningovascular syphilis c) argyll robertson pupil (brainstem damage) d) parenchymatous neurosyphilis |
|
|
Wat is the treatment for neurosyphilis?
|
Aqueous crystalline penicillin G 4 million units IV every 4 hours for 2 weeks (10-14 days)
|
|
|
What is the most common site of Pott's disesae?
|
vertebral tuberculosis infection most commonly involves low thoracic and thoracolumbar region
|
|
|
What are some neurologic manifestations of TB?
|
TB meningitis (subacute, fever, h/a, n/v, meningismus, basilar mening with CN- can lead to hydrocephalus or infarcts)
Tuberculoma Miliary TB Spinal TB with radiculomyelitis |
|
|
What is the most likely route of TB infection?
|
aerosol
|
|
|
What is the most likely route of leprosy infection?
|
aerosol or cutaneous
|
|
|
What egion is endemic to leprosy?
|
southeastasia
|
|
In patients with good host immunity they can contract this limited form of leprosy.
|
tuberculoid leprosy
|
|

With poor host immunity, orgnanisms deposit throughout body particularly with predilection for cooler region (pinna of ear, zygomatic arch, upper & lower limb extensor surfaces
|

lepromatous leprosy
|
|
|
What is the treatment for leprosy?
|
dapsone, rifampin or clofazimine
|
|
|
What are the clinical manifestations of rocky mountain spotted fever?
|
rash maculopapular-> petechial -> ecchymotic
wrists/ankles -> palms/soles |
|
|
What neurologic manifestations can present with RMSP?
|
aseptic meningitis
retinal vasculitis CNS micro infarcts |
|
|
What is the most common cause of aseptic meningitis?
|
enterovirus fecal-oral spread
|
|
|
What is the most common cause of meningoencephalitis?
|
arbovirus California Lacross Encephalitis
|
|
|
What age group is most commonly affected in La Crosse encephalitis?
|
85% in children < 12 years
|
|
|
What is the prognosis for La Crossa encephalitis?
|
self- limited usually mild disease course
|
|
|
What is the distinguishing feature of this disease?
|
seizures are common, status in 25% of patients
|
|
|
What are the multisystemic features of Whipple's disease?
|
arthralgias
weight loss GI symptoms diarrhea neurologic (later in disease course or can precede) |
|
|
What are the neurologic features of Whipple's disease?
|
supranuclear ophthalmoplegia
myelopathy ataxia cerebellar oculomasticatory myorhythmia or oculoskeletal abnormalities dementia, altered mentation, seizures |
|
|
What are some possible neurologic sequelae of La Crosse Encephalitis?
|
seizures, behavioral/memory disturbance, cranial nerve palsies in 10-15%
|
|
|
What is the most common cause of benign recurrent aseptic meningitis?
|
HSV 2 (Mollaret's)
|
|
|
What other systemic manifestations may occur in HSV meningitis?
|
previous, concurrent or post genital signs of infection
|
|
|
What are the neurologic manifestations of VZV infection?
|
cerebellar ataxia
brainstem encephalitis radiculitis radiculomyelitis myelopathy angiopathy arteritis brain infarction |
|
|
What are the characteristic clinical findings in cryptococcus meningitis?
|
basilar meningitis
cranial neuropathies focal findings/seizures/dementia/personality changes elevated ICP |
|
|
What is the treatment for crypto meningitis?
|
2 wks IV amphotericin
8-10 wks maintenance fluoconazole |
|
|
What are the clinical findings of CMV neurologic?
|
polyradiculitis
myelitis aseptic meningitis |
|
|
What ophthalmologic finding may be associated with CNS TB?
|
choroidal tubercles (small frx) or papilledema
|
|
|
What percentage of patients with CNS TB will have positive AFB?
|
10-30% of cases
|
|
|
What is the sens/spec of PCR for TB?
|
sens- 54-100%
spec 94-100 |
|
|
What is the sens/specificity of nucleic acid amplification of CSF for TB?
|
highly sens/spec and available in 24 hours
|
|
|
What is the most common etiology of viral encephalitis?
|
HSV 1
|
|
|
What findings are associated with HSV 1 encephalitis?
|
PLEDS
inferior fronto-temporal hemorrhagic predilection elevated RBC on CSF (not sensitive) CPS, aphasia, personality change |
|
|
What is mortality for untreated patients with HSV1?
|
70%
|
|
|
What 3 viruses may affect the anterior horn cell leading to symptoms of LMN disease?
|
Poliomyelitis
West Nile Virus Japanese encpehalitis virus (Flavivirus) |
|
|
What is the most common cause of arbovirus encephalitis worldwide?
|
Japanese encephalitis virus (Flavivirus)
|
|
|
How is Japanese encephalitis virus transmitted?
|
bite of culex mosquito (infected birds/pigs) then hematogenous to CNS
|
|
|
What are the neurologic manifestations associated with japanese encphalitis?
|
X-pyramidal signs-chorea, athetosis, rigidity
Anterior horn cells/Spinal Cord Brianstem involvement-rhombencephalitis, CN palsies Cerebellar involvement |
|
|
What is the age range of people infected with Japanese encpehalitis virus?
|
usually children
|
|
|
Where & when is St. Louis encephalitis virus most common to occur?
|
south/west/midwest US
late summer/autumn months |
|
|
How is SLE transmitted?
|
culex mosquito bite
|
|
|
What is the mortality for Japanese encphalitis virus?
|
30%
|
|
|
What is the prognosis for Japanese encephalitis virus?
|
50% have severe neuro sequelae
|
|
|
What are neurologic manifestations of SLE?
|
1) Labial/lingual/hand tremors
2) aseptic meningitis 3) encephalitis/psychotic features |
|
|
What is the mortality rate for SLEV?
|
20%
|
|
|
What is a prominent and distinguishing feature of WNV in 94% of patients?
|
tremor (94%), myoclonus (40%) and parkinsonism (75%)
|
|
|
What are methods of diagnosis for WNV?
|
anti-WNV IGM Elisa
CSF PCR (low sens/spec) |
|
|
What can be found on imaging for WNV?
|
meningeal/thalamus/basal ganglia
|
|
|
What is the most severe arbovirla encpehalits?
|
easter equine encpahlitis
|
|
|
What are the clinical manifestations?
|
abrupt onset fever, convulsions, altered mentation and then coma
|
|
|
What are the clinical manifestations of westen equine encphalitis virus?
|
asymptomatic infections
|
|
|
What are some complications of ophthalmic zoster?
|
aseptic meningitis or grnulomatous arteritis
|
|
|
What is Ramsay Hunt syndrome?
|
painful facial weakness and VIII with vesicular eruption in EAC or posterior pharynx
|
|
|
Who should be treated with antiviral agents for Zoster?
|
all elderly patients as they are at higher risk for dev. meningoenphalitis and also anyone with ophtlamic zoster
|
|
|
What are some manifestations of CMV in CNS?
|
1) meningitis
2) CMV encphalitis 3) myeloradiculitis 4) Ventriculitis 5) Ependymitis 6) Cauda Equina 7) polyradiculopathy 8) Congenital CMv-sensorineuralhearing loss, seizures, microcephaly (TORCH) |
|
|
What percentage of asymptomatic adults are positive for CMV?
|
80%
|
|
|
What type of nuclear inclusions are present in CMV?
|
Cowdry type A intranuclear inclusions
|
|
|
How should one diagnose CMV neurologic complications?
|
CMV PCR 95% sens/00% specific
|
|
|
What is the treatment for CMV?
|
ganciclovir/foscarnet
|
|
|
What are the neurologic manifestations of EBV?
|
1) myelopathy
2) assoc. CNS lymphoma 3) aseptic meningitis 4) CN palsy/ Optic neuritis 5) GBS |
|
|
How should one diagnose neuro EMB?
|
EBV antib against VCA
CSF EBV IgM VCA, EBNA antibodies IgG (present thoughout remore infection) Heterophil antiB/Monospot (high false negative rate) |
|
|
What are the clinical manifestations of HHV-6?
|
exanthem
*recurrent febrile seizures immunocomp consider meningoencephalitis |
|
|
What are the clinical manifestations of HHV-7?
|
similar to HHV-6
|
|
|
What are the neuro manifestations of Rabies?
|
1) furious Rabies
hydrophobia, aerophobia, hypersalivation, personality change, lethargy, coma, *dysautonomia (priapism,spontaneous ejactuliation, anisocoria) 2) Classic Rabies ascending weakness axonal polyradiucloneuropathy with myoedema 3) non-classic rabies non-specific meningoencephalitis picture |
|
|
What are some infections that may mimic GBS?
|
1) HIV - acute seroconversion
2) EBV 3) Paralytic Rabies |
|
|
Where are Rabies inclusion bodies found?
|
purkinje cells and hippocampus
|
|
|
What is the characteristic rash distribution in measles?
|
head down then disappears the same way; maculopapular
|
|
|
What are some of the neuro manifestations of Measles?
|
1) X-pyramidal symptoms-choreoathetosis, rigidity, dystonia
2) personality change 3) EEG with slower spike and wave occuring every 4 to 15 seconds |
|
|
What are some manifestations of HIV infection?
|
1) GBS- early, acute
2) HIV Dementia- late apathy, bradyphrenia, mental slowing, akinetic mutism 3) vacuolar myelopathy (most common myelopathy) 4) HIV transverse myelitis (rare) 5) aseptic meningitis (early, acute) 6) HIV myopathy (rare) 7) HIV neuropathy (axonal polyneuropathy sm, painful) 8) Med-induced myopathy/neuropathy 9) CN palsy 10) Monnoneuritis multiplex 11) HIV associated lumbosacral plexopathy 12) Motor neuron-like disease 13) CMV polyradic |
|
|
What is the characteristic triad associated with PML?
|
1) Mentation-Dementia-personality
2) Visual field cuts 3) weakness |
|
|
What percentage of asymptomatic people are positive forJC virus?
|
70%
|
|
|
Who gets PML in the HIV positive population?
|
patieints with AIDS CD4 < 200
|
|
|
Who in the HIV population gets Toxo?
|
CD4 <100 latent infection reactivation
|
|
|
What are some manifestations of HIV infection?
|
1) GBS- early, acute
2) HIV Dementia- late apathy, bradyphrenia, mental slowing, akinetic mutism 3) vacuolar myelopathy (most common myelopathy) 4) HIV transverse myelitis (rare) 5) aseptic meningitis (early, acute) 6) HIV myopathy (rare) 7) HIV neuropathy (axonal polyneuropathy sm, painful) 8) Med-induced myopathy/neuropathy 9) CN palsy 10) Monnoneuritis multiplex 11) HIV associated lumbosacral plexopathy 12) Motor neuron-like disease 13) CMV polyradic |
|
|
What is the characteristic triad associated with PML?
|
1) Mentation-Dementia-personality
2) Visual field cuts 3) weakness |
|
|
What percentage of asymptomatic people are positive forJC virus?
|
70%
|
|
|
Who gets PML in the HIV positive population?
|
patieints with AIDS CD4 < 200
|
|
|
Who in the HIV population gets Toxo?
|
CD4 <100 latent infection reactivation
|
|
|
What are some manifestations of HIV infection?
|
1) GBS- early, acute
2) HIV Dementia- late apathy, bradyphrenia, mental slowing, akinetic mutism 3) vacuolar myelopathy (most common myelopathy) 4) HIV transverse myelitis (rare) 5) aseptic meningitis (early, acute) 6) HIV myopathy (rare) 7) HIV neuropathy (axonal polyneuropathy sm, painful) 8) Med-induced myopathy/neuropathy 9) CN palsy 10) Monnoneuritis multiplex 11) HIV associated lumbosacral plexopathy 12) Motor neuron-like disease 13) CMV polyradic |
|
|
What is the characteristic triad associated with PML?
|
1) Mentation-Dementia-personality
2) Visual field cuts 3) weakness |
|
|
What percentage of asymptomatic people are positive forJC virus?
|
70%
|
|
|
Who gets PML in the HIV positive population?
|
patieints with AIDS CD4 < 200
|
|
|
Who in the HIV population gets Toxo?
|
CD4 <100 latent infection reactivation
|
|
|
What are some manifestations of HIV infection?
|
1) GBS- early, acute
2) HIV Dementia- late apathy, bradyphrenia, mental slowing, akinetic mutism 3) vacuolar myelopathy (most common myelopathy) 4) HIV transverse myelitis (rare) 5) aseptic meningitis (early, acute) 6) HIV myopathy (rare) 7) HIV neuropathy (axonal polyneuropathy sm, painful) 8) Med-induced myopathy/neuropathy 9) CN palsy 10) Monnoneuritis multiplex 11) HIV associated lumbosacral plexopathy 12) Motor neuron-like disease 13) CMV polyradic |
|
|
What is the characteristic triad associated with PML?
|
1) Mentation-Dementia-personality
2) Visual field cuts 3) weakness |
|
|
What percentage of asymptomatic people are positive forJC virus?
|
70%
|
|
|
Who gets PML in the HIV positive population?
|
patieints with AIDS CD4 < 200
|
|
|
Who in the HIV population gets Toxo?
|
CD4 <100 latent infection reactivation
|
|
|
What percentage of adult population seropositive for toxo?
|
1/3
|
|
|
What isprimary route of transmission of toxo?
|
cat oocysts or feces
|
|
|
How should one establish the diagnosis of toxo?
|
acute mass lesoin, subacute encphalitis
|
|
|
What is the most frequent cause of meningitis in AIDS patients?
|
cryptococcus
|
|
|
What are the neuro manifestations of crypto infection?
|
1) Basilar meningitis
2) CN palsy 3) Increased ICP 4) seizures and focal signs |

