![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
189 Cards in this Set
- Front
- Back
|
Where are the D1 receptors located?
|
cerebral cortex, basal ganglia
|
|
|
Where are D2 receptors located?
|
striatum (caudate and putamen)
|
|
|
Where are D3 & D4 receptors located?
|
limbic system
|
|
|
Where are D5 receptors located?
|
hypothalamus and hippocampus
|
|
|
What is the difference between schizophreniform disorder and schizophrenia?
|
Schizophreniform symptoms that impact functioning last at least 1 month but less than 6 months. Schizophrenia symptoms impact functioning last more than 6 months (2 out of 5 positive/negative symptoms only need to last 1 month)
|
|
|
What is the prognosis for schizophreniform disorder?
|
33% will recover within 6 months
|
|
|
What is the best studied SSRI in pregnancy?
|
Fluoxetine
|
|
|
Which SSRIs have the best profile in regard to sexual side effects?
|
fluoxetine and fluvoxamine
|
|
|
Which SSRI has the longest half life?
|
fluoxetine
|
|
|
What is considered the most potent SSRI?
|
paroxetine
|
|
|
What are the clinical characteristics of serotonin syndrome?
|
altered mental status
agitation tremor hypotension fever ataxia diarrhea hyperreflexia myoclonus |
|
|
What is the MOA of buproprion?
|
DNRI
|
|
|
What dose of Buproprion can lead to seizures?
|
more than 450 mg per day
|
|
|
What arethe MOA of duloxetine?
|
SNRI
|
|
|
What is the MOA of Mirtazpine?
|
enhances release of NE, inhitibits 5HT2 and 5HT3 receptors, alpha 2 adrenergic agaonist
|
|
|
What is the MOA of Nefazodone?
|
5HT2 antagonist/reuptake inhibitor
|
|
|
What is the MOA of trazodone?
|
5HT2 receptor antagonist/weak inhibtor of 5HT reuptake
|
|
|
What are the SE of clozapine?
|
sedation, wieght gain, orthostatic hypotension, hypersalivation, eosinophilia, hypertriglyceridemia, hyperglycemia, agrnaulocytosis, seizures
|
|
|
What is MOA of lithium?
|
inhibits inositol-1-phosphatase decreases cellular responses to neurotransmitters
|
|
|
What are 3 MOA of VPA?
|
1) Na channel blocker
2) T-type calcium channel blocker 3) GABA transaminase |
|
|
What is the MOA for GABApentin?
|
increase GABA synthesis
reduce levels of glutamate |
|
|
What is the MOA of Topiramate? (3)
|
na channel blocker
carbonic anhydrase inhibitor weakly enhances post-synaptic GABA (adjunct for bipolar disorder) |
|
|
What illegal drugs do not lead to withdrawal symptoms?
|
cannabis, hallucinogens, inhalants, or phencyclidine
|
|
|
What SSRIs have short half lives leading to concern for serotonin discontinuation syndrome?
|
paroxetine and fluvoxamine
|
|
|
Which subtype of schizophrenia has the best prognosis?
|
paranoid subtype
|
|
|
What is Fregoli syndrome?
|
id a familiar person in various other people without physical resemblance, believe they are pscyhchologically identacal
|
|
|
What clang?
|
thoughts proceed from one to another by sound of words, such as rhyming
|
|
|
What is the difference between schizoaffective disorder and schizophrenia?
|
schizoaffective disorder prominent mood symptoms with psychosis and at least 2 weeks of psychosis without mood symptoms
|
|
|
What is the prognosis for brief psychotic disorder?
|
50-80% completely recover
|
|
|
What is the differential for medical & neurologic causes of psychotic disorder due to a general medical condition?
|
Vascular: stroke left hemisphere
Infection: CJD, HIV, syphillis, TB Trauma: Autoimmune: Lupus Metabolic: Thyrotoxicosis, hypothyroidism, Diabetes, B12 deficiency, Pellagra Iatrogenic: Neoplastic: Cancer, Pareneoplastic Neurodegen: Dementia, Wilson's Disease, Huntington's disease, Temporal Lobe Epilepsy, MS, Parkinson's disease |
|
|
What is the rate of recurrence of postpartum depression?
|
30-50%
|
|
|
What is the incidence of post-partum depression?
|
1:500 to 1:1000 births
|
|
|
How many patients have chronic depression?
|
20% OF mdd PATIENTS
|
|
|
What percentage of patients commit suicide with MDD?
|
10-15%
|
|
|
What are the criteria for dysthymic disorder?
|
ACHE2S (at loeast 2 of following)
appetite concentration hopelessness energy esteem 2 years sleep |
|
|
What are the critieria for bipolar 1 disorder?
|
manic episode for at least 1 week
>4 of the following Distractibility Insomnia Grandiosity Flight of ideas Activities increased pressured Speech Thoughtlessness |
|
|
What is the difference between bipolar ii disorder and bipolar 1 disorder?
|
bipolar 2 has at least 1 MDD and 1 hypomanic without any previous manicc episodes
|
|
|
What is the difference between cyclothymic d/o and bipolar ii d/o?
|
@ least 2 years hypomania and depressive sx but do not meet MDD
|
|
|
What are the physical symptoms associated with panic attacks?
|
at least 4 of following
Palpitations, paresthesias, pounding heart Anxiety Nausea Increased perspiration, increased dread/doom, Chest pain, choking, chills, lack of control Sweating, shortness of breath, shaking/trembling |
|
|
What is cynophobia?
|
fear of dogs
|
|
|
What are the criteria for abuse?
|
failure at social obligations due to drug use, legal problems, use in hazardous situations, social problems
|
|
|
What is the differential diagnosis for delirium or encephalopathy?
|
Vascular- vasculitis, CNS angiitis, left hemispheric stroke,, brainstem infarct, venous infarct (straight sinus/vein of galen), hypertensive encephalopathy, SAH
Infxn: bacterial: mening fungal viral encephalitis: SSPE, WNV, SLE prion disease Trauma: EDH, SDH Toxins: mercury, lead, arsenic Autoimmune: SLE, APLA, WG, Churg-Strauss, Neuro-Behcet's Metabolic: Acid/Base: Hypoxia Electrolytes: Hypona, Hyperna, Uremic Encephalopathy, Hypoglycemia/Hyperglycemia Endocrine: Cushings, Hypo or hyperthyroid AIP Nutrtitional: B12 deficiency, Wernicke's Inflammatory/Iatrogenic: Sarcoid Drugs of abuse: PCP, Cocaine, Amphetamines Neoplastic: Neoplastic, Paraneoplastic, Carcinomatous mening degen: Epilepsy |
|
|
What is the data for donepezil and amnestic MCI?
|
less likely to convert to AD in 1st 12 months, rate of conversion is 15% per year, the effect is gone after 3 years
|
|
|
What is the current AAN recommendation regarding APOE typing for patients with AD?
|
It should not be used currently for diagnosis or management because some carriers will never develop AD (used in studies currently)
|
|
|
What is the difference between Capgras syndrome and Fregoli's syndrome?
|
Capgras syndrome is when a family member is thought to be an impostor, Fregoli syndrome is when an unfamiliar person is id'ed as a family member
|
|
|
What is the relationship between extrapyramidal symptoms and AD?
|
the extrapyramidal symptoms may present in late AD
|
|
|
What is something to consider in patients on cholinesterase inhibitors prior to general anesthesia?
|
These medications should be discontinued
|
|
|
What are the major side effects of donepezil? (4)
|
nausea vomiting diarrhea vivid dreams (watch out for bradycardia)
|
|
|
When should a patient take donepezil?
|
in morning on early stomach
|
|
|
What is the dosing for Aricept?
|
5 mg daily for 1 month then 10 mg daily thereafter
|
|
|
What is the dosing for Galantamine?
|
4 mg twice daily for 1 month, 8 mg twice daily then 12 mg twice daily (if tolerated)
|
|
|
What is the dosing for rivastigmine?
|
twice daily 1.5 mg twice daily then escalate monthly by 3 mg up to 6 mg twice daily if tolerated
|
|
|
What is the difference between galantamine, rivastigmine and donepezil?
|
they all have the same side effect profile but frequency increases in this order
donepezil < galantamine < rivastigmine |
|
|
What are the side effects of memantine with dementia?
|
confusion, headaches, dizziness
|
|
|
When should memantine be used for treatment?
|
in patients with moderate to severe dementia
|
|
|
What is the dosing for memantine?
|
5 mg once daily then increase by 5 mg every week upto 10 mg twice daily
|
|
|
What is initial therapy for apathy?
|
acetylcholinesterase inhibitors should be considered first
|
|
|
What is the effect of memantine on behavior?
|
some improvement in irritability and agitation
|
|
|
What percentage of patients with FTD have sporadic disease?
|
only 20% inherited
|
|
|
What is tau?
|
microtubule binding protein
|
|
|
What chromosome is linked to FTD-MND?
|
Chromosome 9
ubiquitin immunoreactive, tau negative inclusion bodies in motor neurons |
|
|
What is Sneddon's syndrome? (6)
|
1. small vessel strokes
2. extensive white matter disease 3. livedo reticularis 4. antiphospholipid antibodies 5. seizures 6. miscarriages recurrent |
|
|
What are the features of Lindenberg-Spatz disease or Buerger's disease?
|
rare cause of vascular dementia determined by biopsy showing "thromboangiitis obliterans" without media wall thickening/eo deposits (CADASIL) or inflammation/amyloid/granulomatous depositis (amyloidosis, granulomatous disease, vasculitis) and obliteration/occlusion of the vessels (unlike Binswanger's which has thickening of layers without obliteration/occlusion)
|
|
|
What is the difference between Buerger's disease and Lindenberg-Spatz?
|
Buerger's does not occur in women, non-smoker, non-hypertensive
|
|
|
What variants are associated with Creutzfeldt Jakob disease? (4)
|
1. Heidenhain variant (rapidly progressive cortical blindness-occipital lobes)
2. amyotrophic variant- prominent early LMN signs 3. Brownell-Oppenheimer variant- early prominent progressive ataxia 4. Stern-Garcia- x-pyr variant |
|
|
What is the etiology of fatal familial insomnia?
|
mutation of PRNP D178N in addition to MET residue at codon 129, affects mediodorsal thalamic nuclei little spongiform change
|
|
|
what are the clinical features of fatal familial insomnia?
|
intractable insomnia
subacute onset, rapidly progressive dysautonomia (hypertension, tachycardia, hyperhidrosis) ataxia, myoclonus, pyr signs, x-pyr features, tremor |
|
|
what percentage of patients with Whipple's disease have the pathognomonic oculomasticatory myorhythmia?
|
20% of patients
|
|
|
What are the characteristic affected structures in Marchiafava-Gibnami Disease?
|
central corpus callosum, optic chiasm, cbl peduncles, pons, commisure and deep white matter
|
|
|
What heavy metal has been associated with "dialysis dementia"?
|
aluminum
|
|
|
What is the usual age of onset and ethnicity in patients with adult polyglucosan body disease?
|
5th and 7th decades
Ashkenazi Jewish patients |
|
|
What are the usual clinical features of adult polyglucosan body disease?
|
peripheral neuropathy, dementia, neurogenic bladder, UMN signs
|
|
|
What is seen in pathology for adult polyglucosan body disease?
|
accumulation of cytoplasmic PAS + polyglucosan bodies in CNS & PNS
|
|
|
What are some caveats to watch out for interpreation of nerve biopsy with polyglucosan bodies?
|
nonspecific and can bee seen in normal subjects, axonal neuropathies and ALS patients (must combine with clinical features)
|
|
|
What is the etiology of transient global amnesia?
|
5 in 100000 in Minnesota
24% will have recurrent episodes, none at greater risk for subsequent strokes |
|
|
What is the risk of recurrence (another child with autism) after 1 child with autism?
|
5%
|
|
|
What is developmental dyslexia?
|
diagnosis delayed until 3 rd grade, unexpected difficulty reading despite normal intelligence
|
|
|
What is the definition of MR?
|
below-average intelligence, 2 SD below mean IQ <70
|
|
|
What is the risk of recurrence (another child with autism) after 1 child with autism?
|
5%
|
|
|
What is developmental dyslexia?
|
diagnosis delayed until 3 rd grade, unexpected difficulty reading despite normal intelligence
|
|
|
What is mild MR?
|
55-70
|
|
|
What is moderate MR?
|
40-55
|
|
|
What is the definition of MR?
|
below-average intelligence, 2 SD below mean IQ <70
|
|
|
What is mild MR?
|
55-70
|
|
|
What is moderate MR?
|
40-55
|
|
|
What is severe MR?
|
25-40
|
|
|
What is profound MR?
|
<25
|
|
|
When do patients with Trisomy 21 usually develop AD?
|
late 30s early 40s
|
|
|
What is the etiology of Down's patients developing AD?
|
amyloid precursor protein is on chromosome 21
|
|
|
What are Brushfield's spots?
|
small white spots in the iris
|
|
|
What is associated with trisomy 18?
|
rocker bottom feet, dev dissbility, global psychomotor retardation, cardiac malformations, hearing loss, cleft lip
|
|
|
What is the etiology of cri du chat syndrome?
|
chrosome 5 deletion
"meowing" cry round face, microcephaly, hypertelorism, low set ears, micrognathia |
|
|
What is Fragile X syndrome?
|
mutation in the FMR1 gene caused by trinucleotide repeat expansion >200 with MR in all males and half of females
|
|
|
What is FXTAS?
|
permutation caused by 50-200 triplet repeats associated with normal intelligence, ataxia and tremor
|
|
|
What is Rett's syndrome?
|
X linked dominant d/o, MECP gene mutation
1. hypotonia/truncal ataxia 2. nl dev. until 7-18 mos. then regression 3. stereotypy of hand movement 4. loss of speech/communication 5. seizures 6. sudden death/prolonged QT interval 7. microcephaly/deterioration in growth 8. hyperventilation/apnea |
|
|
What is Williams syndrome?
|
1. difficult visuospatial skills
2. supravalvular ao stenosis 3. short stature 4. infantile hypercalcemia 5. elfin like facies, micrognathia |
|
|
What is Prader Willi syndrome?
|
imprinting, deletion of paternal 15q11-q13 chromosomal region
1. small hands & feet 2. hypopigmentation 3. short stature 4. hypogonadotrophic hypogonadism 5. hyperphagia, morbid obesity 6. mild to moderate MR |
|
|
What is Angelman syndrome?
|
maternal deletion of 15q11-q13
1. severe MR 2. ataxia, hyperactive, hypotonic "happy puppet" 3. happy disposition 4. absence of inteliggible spech 5. seizures prior to age 2 |
|
|
What is the breathing pattern in a comatose patienht with a cortical lesion?
|
cheyne-stokes
|
|
|
What is the breathing pattern in a patient with diencephalon lesions?
|
cheyne stokes
|
|
|
What is the breathing pattern in a patient with a midbrain lesion?
|
tachypnea/hyperventilation
|
|
|
What is the breathing pattern in a patient with pontine lesion?
|
apneustic or cluster
|
|
|
What is the breathing pattern in a patient with lesion caudal to the pons?
|
ataxic
|
|
|
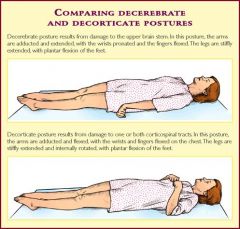
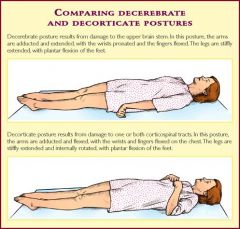
Differentiate between decorticate and decerebrate posturing?
|
decorticalte, flexor elbow and flexor wrist, feet pointed downard
decerebrate posturing extended elbows, wrists flexed out and toes plantar-flexed |
|
|
Differentiate between decorticate and decerebrate posturing?
|
decorticalte, flexor elbow and flexor wrist, feet pointed downard
decerebrate posturing extended elbows, wrists flexed out and toes plantar-flexed |
|
|
|
|
|
What are the position of the eyes in cortical lesions?
|
can have a dilated eye or be normal
|
|
|
What is the position of eyes in diencephalon lesions?
|
small reactive
|
|
|
What are the eyes characterized by in midbrain lesions?
|
midposition fixed
|
|
|
What are eyes characterized by in pontine lesions?
|
pinpoint pupils
|
|
|
What are eyes characterized by in lesions caudal to pons?
|
large and dilated, unreactive
|
|
|
Will oculocephalic maneuvers overcome gaze preference caused by frontal eye field lesions?
|
yes (will not be overcome if pontine lesions look away from stroke)
|
|
|
What is the etiology of periodic alternating gaze?
|
bilateral cerebral hemisphere dysfunction
|
|
|
What is the etiology of ocular bobbing?
|
localize to pons
|
|
|
What are 2 most consistent predictors of outcome for ICH?
|
volume more than 60 Ml and GCS less than 8
|
|
|
What is Terson's syndrome?
|
vitreal hemorrhage and SAH
|
|
|
what is the sensitivity of CT scan within 24 hours after bleed?
|
92%
|
|
|
What is the sensitivity of CT scan within 1 week after bleed?
|
50%
|
|
|
What is definition of giant aneurysm?
|
>25 ,, om doa,eter
|
|
|
What percentage of patients with SAH develop hydrocephalus?
|
20-25%
|
|
|
What is the usual timing of vasospasm?
|
day 4- 14
|
|
|
What are EKG findings associated with SAH?
|
U waves, arrhythmia, myocardial stunning
|
|
|
What percentage of patients have multiple aneurysms?
|
20-30%
|
|
|
What 5 etiologies may predispose to aneurysms?
|
1. Neurofibromatosis
2. Pseudoxanthoma elasticum 3. Marfan's 4. ehler's Danlos 5. coarctation of aorta |
|
|
What percentage of aneurysms are mycotic?
|
3% of all IC aneurysms
|
|
|
What is the definition of a fusiform aneurysm?
|
Dilation of an artery more than 1.5 times normal size without a definable neck
|
|
|
What is the 20/30/40 rule for impending neuromuscular failure?
|
VC <20 ml/kg, MIP <-30 , MEP M40 could be indications for intubation
|
|
|
What is the regimen for patients with cord compression secondary to trauma and presenting within 3 hours of symptoms?
|
30 mg/kg bolus then 5.4 mg/kg/hour for 24 hours
|
|
|
What is the dose of steroids to give patients with cord compression secondary to truama presenting 3-8 hours of symptoms?
|
30 mg/kg bolus then 5.4 mg/kg/hr X 48 hours
|
|
|
What is the grading system for periventricular-intraventricular hemorrhage of neonates?
|
Grade I: caudate head, subependymal layer
Grade II: extension into lateral ventricle, without ventriculomegaly Grade III: extension in LV, with ventriculomegaly Grade IV: extension into parenchyma |
|
|
What is the prognosis if examination shows complete loss of myotomes/dermatomes below the level 24 hours after presentaiton?
|
recovery is unlikely
|
|
|
What are the 4 segments of the ICA?
|
cervical (branch into ICA-ECA at C3-4); petrous (caroticotympanic); cavernous (meningohypophyseal); supraclinoid
|
|
|
What are the branches of the ICA?
|
ophthalmic artery
anterior choroidal artery pcomm aca mca |
|
|
What percentage of people have a complete circle of willis?
|
less than 35%
|
|
|
Where does the vertebral artery enter the vertebral bodies?
|
c6 transverse processes
|
|
|
Where does basilar artery begin & end?
|
joining of vertebrals at pontomedullary junction then ascends to the interpeduncular fossa
|
|
|
What does AICA supply?
|
lateral pons
|
|
|
What does SCA supply?
|
part of midbrain and cerebellum
|
|
|
What supplies the head of caudate?
|
recurrent art Huebner & anterior choroidal (anteromedial portion)
|
|
|
What supplies the lateral GP?
|
lateral lenticulostriate arteries
anterior choroidal |
|
|
What supplies the medial gp?
|
anterior choroidal artery
pcom |
|
|
What supplies the ALIC?
|
lateral and medial lenticulostriates
|
|
|
What supplies the genu?
|
lenticulostriate
|
|
|
What supplies the PLIC?
|
lateral lenticulostriates and anterior choroidal artery
|
|
|
What supplies the anterior thalamus?
|
PCOM anterior thalamoperforating branches
|
|
|
What supplies the medial thalamus?
|
posterior thalamoperforating branches from PCS + basilar + posterior choroidal artery
|
|
|
What supplies lateral thalamus?
|
thalamogeniculate from P2 segment
|
|
|
What supplies the medial medulla?
|
anterior spinal artery
|
|
|
What supplies the posterior spinal artery?
|
posterior 1/3 of spinal cord, including dorsal columns
|
|
|
What is the watershed area of spinal cord?
|
T4-T6 fewer radicular arteries, cervical, intercostal and lumbar arteries contributing to spinal cord
|
|
|
What is the artery of Adamkiewicz?
|
large anterior radicular artery @ level T12, L1 or L2
|
|
|
What is Osler-Weber-Rendu disease?
|
telangiectasia in multiple locations including liver, lung, skin, brain
AD condition |
|
|
How does Osler-Weber-Rendu disease lead to neurologic manifestations?
|
pulmonary fistulae leading to cerebral ischemia
|
|
|
When does the risk of stroke persist until after acute MI?
|
1 week highes up to 6 months
|
|
|
What is the significance of left atrial spontaneous echo contrast?
|
local blood stasis unclear significance, Maorecommends further eval with Holter or telemetry
|
|
|
What is the difference between marantic endocarditis and Libman-Sacks endocarditis?
|
They are both under umbrella of nonbacterial thrombotic endocarditis, but marantic endocarditis is generally considered related to malignancy
|
|
|
What are usual etiologies of non-bacterial thrombotic endocarditis?
|
1) HIV
2) SLE 3) Antiphospholipid antibody syndrome 4) malignancy |
|
|
What is the data for PFO and stroke association?
|
unclear at this point but generally these factors make PFO + stroke more worrisome: a) dvt b) right to left shunt c) atrial septal aneurysm d) cortical stroke
|
|
|
Even after device closure and surgery for PFO closure what is the risk for recurrent stroke?
|
3 to 4% per year
|
|
|
What is the prevalence of cardioembolic stroke among all strokes?
|
20-25%
|
|
|
What is the prevalence of extracranial large artery disease among all strokes?
|
15-20% of strokes are secondary to large vessel disease
|
|
|
What are the data for symptomatic ICA stenosis from 70-99%?
|
NASCET trial 2 year rate of ipsilateral stroke 26% medically treated 9% surgically treated group
|
|
|
What are the data for symptomatic ICA stenosis 50-69%?
|
5 year risk of fatal/nonfatal ipsi stroke was 22% medical and 15.7% surgical group
(poor op prognostic: women, diabetes, contralateral disease, left sided disease, retinal disease, TIA rather than stroke previously) |
|
|
Which patients are considered high risk for CEA?
|
age older than 80
cardiac disease pulmonary disease restenosis after CEA contralateral disease previous neck surgery/radiation |
|
|
What is seen on pathology in Takayasu's arteritis?
|
granulomatous arteritis affecting large vessels
|
|
|
What are the clinical symptoms in patients with Takayasu's arteritis?
|
elevated ESR
fatigue, weight loss pulseless extremities extremity claudication stroke young, female patients |
|
|
What is the treatment for Takayasu's arteritis?
|
immunosuppressants and endovascular surgery are options
|
|
|
What is the pathology for giant cell arteritis?
|
inflammation in media, intimal thickening, fragement IEL, T cell lymphocytes
|
|
|
When should the biopsy be performed in Temporal arteritis?
|
as soon as possible but 2 weeks of steroids should not affect treatment
|
|
|
What conditions may lead to dissection in a patient?
|
a) fibromuscular dysplasia
b) Ehlers-Danlos syndrome type IV c) Marfan's syndrome d) polycystic kidney diseasee) pseudoxanthoma elasticum e) osteogenesis imperfecta |
|
|
What is the etiology of osteogenesis imperfecta?
|
AD condition characterized by abnormality in collagen I
|
|
|
What is Ehler's Danlos type Iv?
|
abnormality in collagen- III
|
|
|
What is the etiology of pseudoxanthoma elasticum?
|
AR disease characterized by mutation in ABCC6 gene, MRP 6 protein
|
|
|
what are the clinical features associated with pseudoxanthoma elasticum?
|
raised yellowish bumps on skin
retina looks like an orange skin retinal hemorrhage early atherosclerosis can lead to dissection b |
|
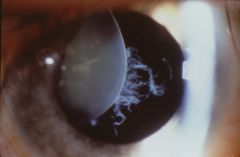
Which connective tissue disorder could this finding be associated with?
|
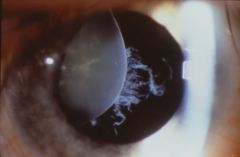
Marfan's syndrome
|
|
|
What are the features of Marfan's syndrome?
|
ectopia lentis
long fingers/limbs arachnodactyly pectus deformity predisposed to aneurysm formation |
|
|
What is the etiology of pseudoxanthoma elasticum?
|
AR disease of connective tissue progressive dsytrophic minerlization of elastic fibers
|
|
|
What is Cogan's syndrome?
|
interstitial keratitis/scleritis/uveitis
vestibuloauditory dysfunciton systemic symptoms in 10% |
|
|
What is Eale's disease?
|
visual loss monocular/binocular, retinal vasculitis, recurrent vitreos hemorrhage and CNS vasculitis
|
|
|
What is Susac's syndrome?
|
microangiopathy affecting arterioles in brain (corpus collosum), retina and cochlea
1) sensorineural hearing loss 2) retinal angiopathy visual field loss 3) encephalopathy, behavioral, affective dysfunction |
|
|
What is Sneddon's syndrome?
|
non-inflammatory vasculopathy of medium sized arteries with intimal hyperplasia
|
|

What non-inflammatory vasculopathy could have this skin finding as well as an association with anti-phospholipid syndrome?
|

Sneddon's syndrome
|
|
|
What is the etiology of Kohlmeier-Degos disease?
|
fibrous intimal proliferation accompanied by thrombosis leading to vasculopathy of skin, cerebral circulation and other organs
|
|
|
What are the symptoms associated with Kohlmeier-Degos disease (or malignant atrophic papulosis)?
|
raised papules whith white center (skin infarcts)
GI manifestations: ulcers, bowel dismotility, dilation ischemic stroke/tia |
|
|
What CNS structures are most sensitivie to anoxia?
|
purkinje cells, dentate nucleus, globus pallidus, hippocampus CA1 pyramidal cells, cortical layers III and V
|
|
|
What are the 6 layers of the cerebral cortex?
|
I: Molecular layer
II: external granular layer III: ext pyramidal layer IV: internal granular layer V: int pyramidal layer VI:mulforme layer |
|
|
What is the usual etioloogy of transcortical motor aphasia?
|
arterial border zones b/t bilateral ACAs and MCAs
|
|
|
What is the etiology of transcortical sensory aphasia?
|
arterial borderzones between bilateral MCAs and PCAs
|
|
|
What is Sommer's sector of hippocampus?
|
CA 1
|

