![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
112 Cards in this Set
- Front
- Back
|
What two species may be protected from erisopilothrix with a vaccine? |
Turkeys and pigs
|
|
|
What is the survival rate for purpurra hemorrhagica?
|
>90%
|
|
|
Horse 3 weeks ago had strangles; now it has petechiae under the lips. What is your ddx?
|
Purpurra hemorrhagica
|
|
|
What are 3 main signs/groups of signs (only need one or 2 from each group) of equine PF?
|
scaling/crusting/exfoliation
Affects face, trunk, and coronary bands Urticaria or swelling of legs/ventral abdomen |
|
|
Rounded up epidermal cells (aka acanthlytic cells), crusty horse, subcorneal pustules= what disease?
|
Pemphigous folaceous
|
|
|
Ventral midline diffuse pattern of dermatitis in a horse: what is most likely dx?
|
culicoides
|
|
|
Ventral midline focal pattern of dermatitis in a horse: what is most likely dx?
|
horn fly/stable fly (hematobia calcitrans) or chorioptes in the literature.
|
|
|
If lice on a horse are running around, what are ddx?
|
BITING LICE: Damalinia equi
|
|
|
Name 2 biting lice on a horse
|
damalinia equi, werneckiella equi equi
|
|
|
Name a sucking louse on a horse
|
Haematopinus asini
|
|
|
What are the typical conditions where a horse gets lice? (Suspect lice if you see these conditions with pruritus).
|
Confined horses w/ poor sanitation.
|
|
|
Chiggers: what are they?
|
6-legged LARVAL FORM of mites.
|
|
|
What causes leg mange in horses? What breed is predisposed?
|
chorioptes- draft horse
|
|
|
Question about "munge" or perioral skin lesions in llamas-- what is it likely responsive to?
|
zinc
|
|
|
How do you treat equine sarcoidosis, and what is its other name?
|
Generalized Granulomatous Disease is treated with steroids
|
|
|
What are the top 3 ddx for widespread scaling in a horse?
|
sarcoidosis (rare)
dermatophilus (rainy) pemphigous folaceous (common) |
|
|
What causes generalized granulomatous disease in cattle but not horses?
|
"hairy vetch" plant-- vicia villosa
|
|
|
What is a common cause of aortic thromboembolism in cats?
|
Hypertrophic cardiomyopathy.
|
|

What disease caused this?
|
Epidermolysis Bullosa, EB
|
|
|
What disease in horses is caused by congenital deficiencies affecting stability of the dermal-epidermal junction? (Affects Belgians, Trait Bretons, Trait Comtois, Saddlebreds.)
|
Epidermolysis bullosa (EB)
|
|

What disease causes this appearance in a horse? This is a Belgian (sure...)
|
EB- epidermolysis bullosa
|
|

What disease caused this appearance? (It is a saddlebred horse.)
|
Epidermolysis Bullosa
|
|
|
Name a disease in horses that affects deep dermal collagen fibers and is usually noticed by 2 years of age? (Affects quarter horses, paints, appaloosas)
|
HERDA or hyperelastosis cutis
HERDA=hereditary equine regional dermal asthenia |
|
|
What disease causes lesions in horses primarily on the dorsum, sides of the neck and legs, and caused by easily torn/stretched skin with seromas, ulcers, or hematomas?
|
HERDA
|
|
|
Do HERDA lesions heal?
|
Yes, they usually heal okay often with scars.
|
|
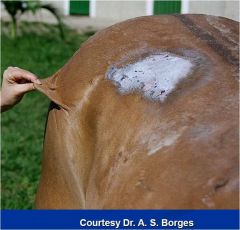
What disease causes this appearance?
|
HERDA, aka hyperelastosis cutis
|
|

Which disease causes this appearance in the horse?
|
HERDA aka hyperelastosis cutis
|
|
|
You get a referral case-- A Belgian horse-- initially diagnosed weeks ago as "pyoderma" ddx chorioptic mange. The case has progressed, and you see lower leg enlargement with firm swelling, thick skin folds, and large firm nodules. What is your primary ruleout?
|
Chronic Progressive Lymphedema
|
|
|
What 3 breeds of horse get chronic proressive lymphedema?
|
belgians, shires, and clydesdales
|
|

What condition is depicted?
|
Chronic progressive lymphedema
|
|
|
Name 4 coagulase positive staph species that can cause large animal dermatological problems
|
Staph pseudintermedius
S aureus S hyicus S delphini |
|
|
Name 2 drugs that can encourage growth of MRSA in large animals
|
ceftiofur
Aminoglycosides |
|

What condition is seen here? (Pathogen/condition)
|
Staph aureus vasculitis
|
|
|
Name an equine skin pathogen that causers deeper infections rather than superficial lesions. How do you treat it?
|
Corynebacterium pseudotuberculosis
Treat with pain meds (phenylbutazone) and a hot pack. |
|
|
What is the most common bacterial skin disease in horses?
|
Dermatophilus congolensis
|
|
|
Is d congolensis gram-positive or gram-negative?
|
gram positive actinomycete
|
|
|
Name four bacteria with a filamentous phase in their life cycle; which two cause pyogranulomatous inflammation with fistulous tracts?
|
Actinomyces*, nocardia*, dermatophilus, streptobacillus
|
|
|
Where is actinomyces found normally?
|
Oral mucous membranes and tooth surfaces, urogenital mucous membranes.
|
|
|
What causes lumpy jaw? How is it treated?
|
actinomyces bovis, and rarely actinomyces israelii. Tx with oral iodine compounds (oral or IV) or penicillins with aminoglycosides.
|
|
|
What causes "poll evil"?
|
Actinomyces (along with other bacteria)
|
|
|
How is feline and canine actinomyces treated?
|
surgical treatment-- drainage/lavage/excision/removal of foreign bodies, plus abx long-term (ampicillin.)
|
|
|
Name two antibiotic classes not useful in canine or feline actinomycosis
|
aminoglycosides and fluoroquinolones
|
|
|
What causes strawberry footrot and how is it treated?
|
Dermatophilus congolensis. Usually self-limited, extreme cases tx with penicllins G, tetracycline, or chloramphenicol.
|
|

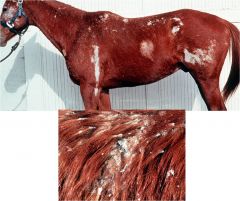
What condition is shown here? In addition to presence of the pathogen, what two conditions are ncessary for this condition to develop?
|
Dermatophilosis; moisture and skin damage
|
|
|
Name a zoonotic horse skin pathogen that causes nodules, ulcers, and lymphatic cording.
|
sprothrix schenckii
|
|

What condition is seen here? How do you treat it?
|
Sporotichosis- organic iodides.
|
|
|
You treat sporotrichosis with the typical RX; what signs might you see as a side-effect of the drug, and how should you respond?
|
iodinism causes scaling, alopecia, serous ocular/nasal discharge, salivation, coughing, and other problems.
D/C 1 week, resume at 3/4 dosage. |
|

This horse from the vet school at Ross in the caribbean was self-mutilating; what is this and how do you treat it?
|
Pythium insidiosum, tx surgical debulking, therapeutic vaccine
|
|
|
List four equine dermatophytes. What is the best diagnostic method?
|
Trichophyton equinum, trichophyton mentagrophytes, trichophyton verrucosum, microsporum equinum.
FUNGAL CULTURE-- wood's lamp only rarely positive |
|
|
What dermatophytes do cattle and goats get?
|
T mentagrophytes and verrucosum
|
|

What condition is depicted?
|
Dermatophytosis (caused in cow by Trichophyton mentagrophytes or t verrucosum)
**Note: the image has been repeatedly updated, however it still seems to sometimes show the same image as the HERDA case. If this image was answered as HERDA elsewhere, HERDA is correct and dermatophilus should be an image of a dun or grey horse (I think, I hate horses and stupid horse colors) with white spots all over. |
|
|
You see a pig with a history of lethargy and anorexia and scaling and now is covered in dark red macules and pustules, as well as coronary band erosions. What is the disease, and what organism causes it?
|
Staphylococcus hyicus-- greasy pig disease (aka exudative epidermitis of swine)
|
|

What causes the lesions seen here? How is it treated?
|
purpurra hemorrhagica. 90% survival rate; tx with steroids and procaine penicillin.
|
|
|
How do you treat chorioptes?
|
Topical lime sulfur. (Can use fipronil/ aka Frontline spray if O wants to pay for it.)
|
|

How would you treat this llama?
|
Zinc!
|
|
What is this and how do you treat it?
|
Equine sarcoidosis, tx with pred.
|
|
|
You see a 6 year old Jack Russel Terrier with corneal edema. What is your primary differential?
|
lens luxation
|
|
|
You see a cocker spaniel with corneal edema. What is your primary differential?
|
Glaucoma.
|
|
|
You see a german shepherd with corneal edema. What is your primary differential?
|
pannus (chronic superficial keratitis)
|
|
|
What are normal values for intraocular pressure and schrimer tear test?
|
<25, >15
|
|
|
In what order would you do the following: dilate the eye, perform a schirmer tear test, perform tonometry, neuro exam, opthalmoscopy, fluroescein
|
1. Schirmer. 2. fluorescein 3. Tonometry. 4. Dilation 5. Opthalmoscopy
|
|
|
KCS: who is predisposed?
Tx-- medical, plus what to do if medical tx fails |
brachycephalic breeds |
|
|
Dog has IOP of 31. What are your treatment options? (List 7 treatments and one major contraindication.)
|
Glaucoma- rx underlying cause.
Can give mannitol in an emergency. Beta-blockers Carbonic anhydrase inhibitors (methazolamide systemic, dorzolamide topical) Prostaglandin analogues (latanoprost) Miotics (pilocarpine) Anterior chamber valve implantation DO NOT GIVE ATROPINE. |
|
|
Name 4 dog breeds predisposed to glaucoma
|
Basset hound, cocker spaniel, beagle, samoyed.
|
|
|
Name 5 causes of canine cataracts
|
inherited, DM, trauma, uveitis, senile
|
|

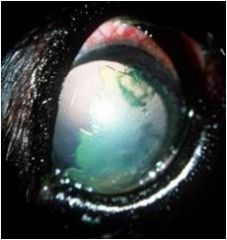
What condition is pictured? What classic sign is present?
|
Chronic superficial keratitis, starts ventrolaterally and extends across.
|
|
|
WIth KCS, how long does melanosis take to resolve?
|
It is permanent.
|
|
|
A cocker spaniel comes to you with blepharospasm, mydriasis, and absent PLR in the left eye; no abnormal history and no abnormalities on PE and hx.. What after treating the current problem, what is an important action to take?
|
Primary glaucoma-- treat the other eye pre-emptively to delay onset.
|
|
|
A dog comes to you with acute vision loss. What is your primary diagnosis? What is one definitive test? How do you tx?
|
SARDS-- severe acute retinal degeneration. Should see flatline ERG. No treatment.
|
|
|
A dog comes to you with gradual vision loss. What is your primary diagnosis? What are some supportive findings? How do you tx?
|
PRA-- progressive retinal atrophy. See retinal vasculature attenuation, tapetal hyperreflectivity, optic disk atrophy. No tx.
|
|
What condition is pictured here? In what dog might you find this (2 features of signalment.) What is the treatment?
|
This is an indolent ulcer, aka boxer ulcer. See in boxers or any older dog. Tx: blunt debridement, grid keratotomy, superficial keratectomy. Antibiotics, NSAIDs, atropine won't help.
|
|
|
A cat has keratoconjunctivitis. What is your primary ruleout? What are 3 ddx? How do you treat.
|
FHV-1. DDx: calicivirus, chlamydophila, mycoplasma. Tx: oxytetracyclin (Terramycin (r)) topical, doxy or azithromycin systemic, or antiherpetics.
|
|
|
Name 4 antiherpetic medications.
|
trifluridine, idoxuridine, cidofovir, and lysine (competitively inhibits arginine.)
|
|
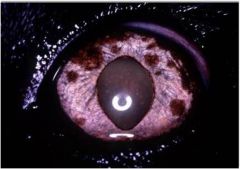
You see this; how do you respond?
|
Systemic workup includes lymph node aspirates, AUS, and chest rads. |
|
|
Cat has acute vision loss, unilateral mydriasis. What is your first diagnostic step?
|
Possibility of retinal detachment: get systemic BP first!
(SARDS is in DOGS) |
|
|
What can cause retinal detachment in a cat? (6 categories or diseases)
|
Systemic hypertension-- secondary to renal disease or hyperthyroidism.
Toxoplasmosis Trauma Fungal infection FIP Neoplasia |
|
|
How do you treat feline acute blindness (assuming the most common cause) and what is the prognosis?
|
Most common cause: hypertension, usually secondary to renal disease/hyperthyroidism. Treat the primary disease and put on BP meds, and they'll regain vision in a week quite frequently.
|
|
|
Cattle eye problem: name a disease more prevalent in summer than winter, in calves than cows, and in bos taurus than bos indicus.
|
infectious bovine keratoconjunctivitis
|
|
|
what is the major pathogen leading to IBK, as well as secondary pathogens? How is it transmitted?
|
Major pathogen is moraxella bovis. Secondary pathogens include infectious bovine rhinitis virus, mycoplasma. Transmitted by handlers, flies, infected animals. WILL SPREAD THROUGH HERD! |
|
|
A cow has pinkeye; it started in the left eye, and spread to the right. The C/S were first noted in June. Now the cow has decreased milk production and slow weight gain. What is your treatment?
|
This is infectious bovine keratitis. Treat with any antibiotic-- usually penicillin, ampicillin, or oxytetracycline. Also HERD MANAGMENT: segregation and tx of carriers plus fly control.
|
|
|
What's the most common horse eye problem?
|
ERU-- equine recurrent uveitis
|
|
|
A client shows you a horse with bilateral cataracts, bupthalmos, and degeneration of the corpora nigra. On examination, you note chorioretinal scarring. History reveals that the horse was septic in Feb, but it's July now. How do you treat?
|
This is equine recurrent uveitis; treat with topical anti-inflammatories, atropine, oral NSAIDS, or cyclosporine implant.
|
|
|
What are some signs that an equine eye problem is in the active stage?
|
ANy sign of active inflammation-- edema, blepharospasm, conjunctival hyperemia, corneal vascularization, aqueous flare, epiphora, miosis. |
|

Name four treatments, including one specific drug.
|
Radiation, surgery, cryotherapy, cisplatin (chemo). |
|
|
How is IOP affected by acute inflammation?
|
DECREASES; may possibly increase with chronicity.
|
|
|
How do you treat an uncomplicated ulcer?
|
Topical antibiotic
Atropine NO STEROIDS |
|
|
What is ptosis?
|
drooping eyelid
|
|
|
What is miosis?
|
CONSTRICTED pupil-- smaller word, smaller pupil
|
|
|
What is mydriasis?
|
Dilated pupil
|
|
|
How do you determine preganglionic vs postganglionic horner's?
|
Because of the principle of denervation supersensitivity, a Horner’s syndrome produced by a lesion interrupting the postganglionic fibres should dilate the pupil when phenylephrine 1% is placed in the conjunctival sac. The pupil of a patient with central (first order) Horner’s syndrome should not dilate, while a pre-ganglionic (second order) pupil may dilate minimally1; a normal pupil may, at best, dilate minimally.
|
|
|
An owner has a lab and a pekingese that ran into each other in a head-on collision. They are both in your office right now with proptosis, and every single prognostic indicator is identical between the two: vision present, PLR and dazzle response intact, non-mydriatic, no hyphema. You give lubrication and pain relief and replace both eyes. What do you tell the owner regarding prognosis?
|
The signs that are seen are all positive prognostic indicators. However, signalment also plays a role. Both of them have a good chance of regaining vision, but the Pekingese has the best prognosis-- Easy Out, Easy In (brachycephalics do better generally.)
|
|
|
Describe the surgical process to repair proptosis, and list 4 kinds of drugs you should give.
|
General anesthesia
2. Place simple interrupted sutures (lid margin) 3. Tighten sutures while applying gentle pressure with scalpel handle Atropine Antibiotics (topical and systemic) oral anti-inflammatories Analgesics |
|
|
What are 3 anticipated complications after proptosis repair?
|
re-proptosis, KCS, strabismus
|
|
|
You are presented with a 2 year old female spayed cocker spaniel dog with a history of acute blepharospasm and a “red eye.”
Which medication is initially contraindicated? Carprofen Dorzolamide Latanoprost Tropicamide |
Tropicamide is a mydriatic (anticholinergic). A cocker spaniel with acute eye problems=GLAUCOMA, don't dilate a glaucomic eye! (That thing with the changing the angle and acute problems...)
|
|
|
Which of the following is the incorrect order to complete an ophthalmic examination?
a) Corneal cytology, tonometry, fluorescein stain b)STT, tonometry, pupil dilation, fluorescein stain c) Pupil dilation, STT, fluorescein stain, tonometry d) Indirect ophthalmoscopy, STT, fluorescein stain, tonometry |
c-- STT needs to be done early on.
|
|
|
A 3 year old male castrated German Shepherd dog presents for evaluation of dorsolateral corneal vascularization and melanosis. You diagnose Chronic Superficial Keratitis (pannus). Which of the following is not part of your treatment plan?
Topical latanoprost Topical cyclosporine ophthalmic ointment Topical glucocorticoid ophthalmic solution Reducing time spent outdoors during summer months |
Latanoprost is not indicated. (Latanoprost reduces IOP by increasing aqueous outflow.)
|
|
|
Glaucoma is a leading cause of blindness in dogs. Underlying mechanisms include:
A) Anterior lens luxation, uveitis, keratoconjunctivitis sicca B) Posterior lens luxation, trauma, indolent (Boxer) ulcers, herpesvirus C) Cataracts, anterior lens luxation, trauma, retinal detachment D) Proptosis, anterior lens luxation, ehrlichiosis, trauma |
C)... I guess. But I kinda suspect that these are associated, not underlying mechanisms necessarily.
|
|
|
Herpesvirus is the leading infectious agent causing conjunctivitis in cats. Which of the following statements is true of this pathogen?
A) Infection is life-long and treatment involves topical antibiotics, topical antivirals and topical prednisolone acetate (1%) ophthalmic solution B) Infection is short-lived and rarely causes ongoing disease. Treatment consists of oral antivirals C) Infection is short-lived and rarely causes ongoing disease. Treatment consists of oral and topical antivirals D) Infection is life-long and recrudescence can be stimulated by stress. Lysine is one therapeutic agent. |
D)
|
|
|
A 4 year old Quarter Horse mare is presented for a pre-purchase examination. On ophthalmic examination you detect cataracts, blunted corpora nigra, chorioretinal scarring and hobs striae. You advise the prospective owner:
A) That the horse likely suffers from herpesvirus keratitis B) That the horse will likely become blind eventually C) That the horse likely has Equine Recurrent Uveitis (ERU), but this is a common condition in horses and rarely causes ongoing problems D) That the horse should not be used for breeding |
B)- the horse is likely to become blind.
|
|
|
Which of the following is the incorrect order to complete an ophthalmic examination?
a) Corneal cytology, tonometry, fluorescein stain b)(STT, tonometry, pupil dilation, fluorescein stain c) Pupil dilation, STT, fluorescein stain, tonometry d) Indirect ophthalmoscopy, STT, fluorescein stain, tonometry |
c-- STT needs to be done early on.
|
|
|
A 3 year old male castrated German Shepherd dog presents for evaluation of dorsolateral corneal vascularization and melanosis. You diagnose Chronic Superficial Keratitis (pannus). Which of the following is not part of your treatment plan?
Topical latanoprost Topical cyclosporine ophthalmic ointment Topical glucocorticoid ophthalmic solution Reducing time spent outdoors during summer months |
Latanoprost is not indicated. (Latanoprost reduces IOP by increasing aqueous outflow.)
|
|
|
Glaucoma is a leading cause of blindness in dogs. Underlying mechanisms include:
A) Anterior lens luxation, uveitis, keratoconjunctivitis sicca B) Posterior lens luxation, trauma, indolent (Boxer) ulcers, herpesvirus C) Cataracts, anterior lens luxation, trauma, retinal detachment D) Proptosis, anterior lens luxation, ehrlichiosis, trauma |
C)... I guess. But I kinda suspect that these are associated, not underlying mechanisms necessarily.
|
|
|
Herpesvirus is the leading infectious agent causing conjunctivitis in cats. Which of the following statements is true of this pathogen?
A) Infection is life-long and treatment involves topical antibiotics, topical antivirals and topical prednisolone acetate (1%) ophthalmic solution B) Infection is short-lived and rarely causes ongoing disease. Treatment consists of oral antivirals C) Infection is short-lived and rarely causes ongoing disease. Treatment consists of oral and topical antivirals D) Infection is life-long and recrudescence can be stimulated by stress. Lysine is one therapeutic agent. |
D)
|
|
|
A 4 year old Quarter Horse mare is presented for a pre-purchase examination. On ophthalmic examination you detect cataracts, blunted corpora nigra, chorioretinal scarring and haab's striae. You advise the prospective owner:
A) That the horse likely suffers from herpesvirus keratitis B) That the horse will likely become blind eventually C) That the horse likely has Equine Recurrent Uveitis (ERU), but this is a common condition in horses and rarely causes ongoing problems D) That the horse should not be used for breeding |
B)- the horse is likely to become blind.
|
|
|
Which of the following is the incorrect order to complete an ophthalmic examination?
a) Corneal cytology, tonometry, fluorescein stain b)(STT, tonometry, pupil dilation, fluorescein stain c) Pupil dilation, STT, fluorescein stain, tonometry d) Indirect ophthalmoscopy, STT, fluorescein stain, tonometry |
c-- STT needs to be done early on.
|
|
|
A 3 year old male castrated German Shepherd dog presents for evaluation of dorsolateral corneal vascularization and melanosis. You diagnose Chronic Superficial Keratitis (pannus). Which of the following is not part of your treatment plan?
Topical latanoprost Topical cyclosporine ophthalmic ointment Topical glucocorticoid ophthalmic solution Reducing time spent outdoors during summer months |
Latanoprost is not indicated. (Latanoprost reduces IOP by increasing aqueous outflow.)
|
|
|
Glaucoma is a leading cause of blindness in dogs. Underlying mechanisms include:
A) Anterior lens luxation, uveitis, keratoconjunctivitis sicca B) Posterior lens luxation, trauma, indolent (Boxer) ulcers, herpesvirus C) Cataracts, anterior lens luxation, trauma, retinal detachment D) Proptosis, anterior lens luxation, ehrlichiosis, trauma |
C)... I guess. But I kinda suspect that these are associated, not underlying mechanisms necessarily.
|
|
|
Herpesvirus is the leading infectious agent causing conjunctivitis in cats. Which of the following statements is true of this pathogen?
A) Infection is life-long and treatment involves topical antibiotics, topical antivirals and topical prednisolone acetate (1%) ophthalmic solution B) Infection is short-lived and rarely causes ongoing disease. Treatment consists of oral antivirals C) Infection is short-lived and rarely causes ongoing disease. Treatment consists of oral and topical antivirals D) Infection is life-long and recrudescence can be stimulated by stress. Lysine is one therapeutic agent. |
D)
|
|
|
A 4 year old Quarter Horse mare is presented for a pre-purchase examination. On ophthalmic examination you detect cataracts, blunted corpora nigra, chorioretinal scarring and hobs striae. You advise the prospective owner:
A) That the horse likely suffers from herpesvirus keratitis B) That the horse will likely become blind eventually C) That the horse likely has Equine Recurrent Uveitis (ERU), but this is a common condition in horses and rarely causes ongoing problems D) That the horse should not be used for breeding |
B)- the horse is likely to become blind.
|
|

This is a Jersey; several are affected in the herd. You advise that:
A) This is likely due to trauma and the fences should be checked B) Calves will likely be spared as this condition mostly affects older cows C) The condition will likely resolve once the summer months begin, and that economic significance is negligible D) That fly control and segregation of affected animals are important parts of management of this condition |
D) This is IBK, caused by moraxella bovis, carried by flies and people.
|
|
|
Glaucoma is a painful, potentially vision-threatening ocular condition. The following are true of this disease:
A) It occurs most commonly in older pure-breed dogs, especially German Shepherds and Boxers B) It is caused by use of topical atropine C) It can be treated with mannitol, prostaglandin analogues and/or carbonic anhydrase inhibitors D) It is a symptom of early uveitis, which could be caused by a perforating injury |
C. Uveitis does NOT cause glaucoma. PG analogues decrease pressure.
|
|
|
Iris neoplasia differs between dogs and cats in the following ways:
1. A) Iris melanoma is the most common tumor in cats, while adenocarcinoma is most likely in dogs 2. B) Iris melanomas in cats rarely progress, while those in dogs frequently metastasize to distant organs early in the course of disease 3. C) Iris melanomas in cats do not typically respond as well to chemotherapy as do those in dogs 4. D) Iris melanomas in cats tend to more diffusely affect the iris than those in dogs |
D Iris melanomas in cats tend to more diffusley affect the iris in cats than in dogs.
|

