![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
155 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Hematopoetic System |
Bone marrow and lymph |
|
|
|
Origin of all blood cells
|
stem cells/hemacytoblast |
|
|
|
Causes stem cells to differentiate into familial parenteral cells
|
Regulatory Mechanism |
|
|
|
Functions of blood
|
1 Transport of oxygen,nutrients,hormones and metab wastes |
|
|
|
Normal value Reticulocytes |
slides: 0.5-2.5% |
|
|
|
Increased RBC
|
Polycythemia |
|
|
|
Normal Value WBC
|
4000-11000/uL
|
|
|
|
Immature RBC's
|
Reticulocytes |
Suggests hemolysis or acute blood loss |
|
|
Oxygen Carrying capacity
|
Hgb
|
|
|
|
Transport medium
|
Plasma |
|
|
|
Hemostasis
|
Pct
|
|
|
|
Decreases first in acute blood loss
|
Rbc
|
Hgb and Hct stabilize in 4 hours
|
|
|
measures the average size of RBC
|
Mean Cell Volume(MCV) |
Hct + RBC |
|
|
Measures the amount or mass of Hgb
|
Mean Cell Hgb |
RBCs that are normochromic versus hypo hyperchromic
|
|
|
Manual differential
|
used to confirm microcytic cells, |
|
|
|
Abnormal RBCs
|
Anisocystosis-size, |
|
|
|
Abnormal WBCs
|
Bands vs Segs, |
|
|
|
Immature Netrophils
|
Bands : 3-5%
|
|
|
|
Granulocytes
|
Basophils: 0.4-1%, |
|
|
|
agranulocytes
|
Lymphocytes:25-35%, |
|
|
|
Left Shift
|
The immature bands increase or out number the segmented neutrophils |
|
|
|
RBC critical value
|
Hgb < 7, Hct < 21 |
|
|
|
Acute blood loss (Anemia)
|
Normochrocomic, Nomocytic
|
MCV & MCH is normal |
|
|
Iron Deficient,Inherited Anemia's
|
microcytic,hypochrcomic |
MCV low,MCH loW
|
|
|
Chronic Illness, sometimes thalasemia
|
Microcytic,Normochomic
|
MCV low; MCH normal |
|
|
B12 and Folate deficiency anemia
|
Macrocytic |
MCV high; MCH andMCHC Variable
|
|
|
Signs and Symptoms of anemia
|
can be asymptomatic
|
|
|
|
Laboratory for Microcytic Anemia
|
Serum Feritin, Iron, Total Ir0n Binding Capacity(TIBC),Homoglobin electrophoresis, |
|
|
|
Laboratory for Macrocytic (Megaloblastic Anemia)
|
B12 & folate
|
Shilling test
|
|
|
Laboratory forHemolytic Anemia
|
Reticulocyte, Direct coombs test |
|
|
|
Laboratory for Pancytopenia
|
Bone Marrow Biopsy |
|
|
|
findings in Acute Hemorrhagic Anemia
|
-fluid shift from interstitial to intravascular space |
|
|
|
Findings in chronic blood loss
|
Typically normal RBCs |
|
|
|
S&S of Iron Deficiency Anemia
|
-Mild to Moderate fatigue, weakness, activity intolerance, Dyspnea, Pica
-BRITTLE SPOON SHAPED NAILS, Cheilosis |
|
|
|
Treatment for Iron deficiency anemia
|
Diet, |
|
|
|
Causes of Iron Deficiency Anemia
|
Diet-Vegetarian, |
|
|
|
Dietary sources for Heme Iron
|
Beef, Chicken, Egg yolk, Clams, Oysters, Pork loin, Turkey and Veal |
|
|
|
Sources of non heme Iron
|
Bran flakes, Brown Rice, whole grain breads, Dried beans, Dried fruits, Greens, Oatmeal
|
|
|
|
Sources of folic acid
|
Green Leafy Veg, Brocoli,Organ meats, Eggs, wheat grain, asparagus, Liver, Milk, Yeast, Kidney beans
|
|
|
|
Sources of Vit B12
|
Liver, Fresh shrimp and oysters, Eggs, Milk, Kidneys, Meats(muscle), Cheese
|
|
|
|
What is deficient Megaloblastic Anemia? |
Folate and B12
|
|
|
|
Paresthesia |
Only in B12 deficiency |
|
|
|
Labs for B12 Deficiency
|
shillings test-24 hours urine collection |
|
|
|
treatment for B12 deficiency |
Diet and suplements, |
|
|
|
Symptoms for Folic acid deficiency
|
Glositis and cheilosis, |
|
|
|
Premature Lysis of RBC
|
Hemolytic Anemia |
|
|
|
Hematopoetic Activity leads to
|
increased reticulocytes
|
|
|
|
initial manifestation of anemia |
tachypnea and tachycardia
|
|
|
|
Care for iron deficiency anemia
|
Iron rich food, |
|
|
|
care for vit b12 anemia |
Dietary intake, |
|
|
|
Care for folic acid anemia
|
Dietary intake, |
|
|
|
Care for sickle cell crises
|
Rest, |
|
|
|
Care for Vhest Syndrome
|
Hydration, |
|
|
|
Care for Thalasemia
|
Regular BT, |
|
|
|
Care for aplastic anemia
|
Withdrawal causative agent, |
|
|
|
HYDROXYUREA |
A drug that promotes fetal, hemoglobin production |
|
|
|
Aplastic anemia med mnmgt |
Immunosupressive therapy with antithymocyte globulin, Corticosteroids, and cyclosporines
|
|
|
|
Hypertension in polycethemia
|
Caused by increased blood, viscosity, |
|
|
|
2 types of hodgkin's dse virus |
Epstein-Barr Virus, |
|
|
|
MHCH
|
% of hgb in RBC |
|
|
|
Can indicate sepsis in BMT |
Left shift
|
|
|
|
in anemia heart rate increases upto 110-120 inducates
|
SHOCK
|
|
|
|
Nsg diagnosis in anemia
|
activity intolerance |
|
|
|
MCV and MCH normal
|
Normochromic Normocytic
Acute blood loss |
|
|
|
MCV low MCH low
|
Microcytic hypochromic, |
|
|
|
MCV high MCH and MCHC variable |
Macrocytic, B12 and folate deficiency, anemias |
|
|
|
Heart rate is increased up to about 110-120 in anemia |
SHOCK |
|
|
|
First CBC sign is lowered RBC |
Acute hemorrhagic Anemia |
|
|
|
Typically normal RBC count but Microcytic hypochromic |
Chronic hemorrhagic Anemia, May show signs and symptoms, of decreased iron |
|
|
|
Decreased RBC, H&H, Iron and increased TIBC |
Iron Deficiency anemia, Abnormal RBC shapes-teardrops |
|
|
|
Hydrops fatalis |
Alpha thalasemia trait |
|
|
|
Produces pacytopenia |
Aplastic anemia |
|
|
|
Diagnostic for aplastic anemia
|
BMA and biopsy, |
|
|
|
Donate in advance Donate right before surgery Salvaged Underuterilized
|
Autologous |
|
|
|
Use donate blood
|
Homologous
|
|
|
|
Use donate blood
|
Homologous
|
|
|
|
Blood donation between relatives
|
Directed
|
|
|
|
Can occur in PRBC
|
Hyperkalemia and fluid overload
|
|
|
|
watch out before plasma transfusion
|
PT and PTT >15 normal value
|
|
|
|
3 types of transfusion reaction
|
1. Allergic |
|
|
|
Tends to be high antigenic with reactions
Most likely to cause allergic reactions |
Granulocytes
|
|
|
|
Managent for hemolytic transfusion reaction
|
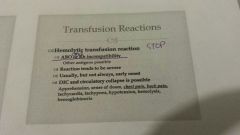
STOP
|
|
|
|
Antigen-antibody response to plasma and or WBC Usual history of previous Transfusion reaction |
Febrile non hemolytic reaction |
|
|
|
Management of reactions |
Stop infusion, keep vein open, Institute emergency protocol, Notify the physician, Careful assessment, send bag back to the bank |
|
|
|
What type of transfusion reaction would the patient who receive multiple transfusions over the course of his cancer treatment most likely experience? |
Febrile non hemolytic |
|
|
|
indicated for symptomatic anemia in non-myeloid cancer patient |
Epogen |
|
|
|
Indicated for myelosuppression r/t HCST, chemo, HIV Goal is to reacch WBC count above 3500 |
Neupogen- STIMS |
|
|
|
In bone marrow aspiration what would you do if bleeding occurs? |
Apply direct pressure |
|
|
|
any increase in temperature is significant |
BMT/SCT |
|
|
|
last blood cell to recover |
Platelet |
|
|
|
first S/S of Graft versus host Disease |
Widespread rash, eventually leads to peeling may start in hands and feets |
|
|
|
Leukemia common in kids and young adults |
ALL |
|
|
|
Leukemia common in older adults |
AML |
|
|
|
Leukemia only seen in adults |
CLL and CML |
|
|
|
also called erythrocytosis |
Polycythemia vera |
|
|
|
Manifestations of polycythemia vera |
Hypertension, Plethora, Hypermetabolism, Hyperviscosity, |
|
|
|
Polycythemia vera management |
Recurrent phlebotomy of 300-500 ml |
|
|
|
Goal for leukemia treatment |
To prevent overwhelming infection and hemorrhage |
|
|
|
Nursing Diagnosis for patient with neutropenia |
Risk for infection |
|
|
|
Nurisng Diagnosis for patient with thrombocytopenia |
Risk for bleeding |
|
|
|
Treatment for Idiopathic thrombocytopenia |
1.GCSF 2.splenectomy |
|
|
|
similar to leukemia and lymphoma plasma cells multiply uncontrollably and infiltrate the bone marrow, lymph nodes, spleen and other tissues |
Multiple Myeloma |
|
|
|
There is destruction of of bones of skull and hips can lead to swiss cheese |
Multiple myeloma |
|
|
|
over production of plasma cells -high levels of cytokines and immunoglobulin |
Multiple Myeloma |
|
|
|
Treatment for multiple myeloma |
Fumilant or indolent, chemo, HSCT, THALIDOMIDE, localized RADIATION for BONE, LEsions
|
|
|
|
S/S for Hodgkin's lymphoma |
REED STEINBERG CELL, treated with raditaion and chemo therapy |
|
|
|
S/S for non hodgkin's lymphoma |
do not have reed steinberg cells, increasedrisk among, immunosuppressed, autoimmune dse, Treated with chemo, HSCT, Radiation + biotherapy |
|
|
|
Nursing Consideration before raditaion |
Sperm bank |
|
|
|
family members colorectal cancer |
increased surveillance colonoscopy q 3 yrs |
|
|
|
in breast cancer 90% of lumps are |
benign not cancerous |
|
|
|
Chemo for Colon cancer |
5-FU Leucovirin Camptosar |
|
|
|
Has spread into surrounding breast tissue but not other organs or structures |
Invasive ductal Ca |
|
|
|
Diagnostic test for Breast Ca |
Sentinel Lymph node biopsy hormone receptor status DNA ploidy status Cell proliferative indices Her-2/neu genetic marker |
|
|
|
Not always present Breast Ca Diagnosis |
Her-2/neu genetic marker |
|
|
|
Breast Ca Diagnosis ER or PR receptor tamoxifen-blocks these receptors
|
Hormone Receptor status -if no receptors tamoxifen is not indicated |
|
|
|
adjunctive therapy chemotherapy |
for non advanced Ca |
|
|
|
Adjunctive therapy for breast Ca |
Radiation therapy High dose Brachy therapy chemotherapy |
|
|
|
Given for Osteoprosis risk |
Biphosphonates |
|
|
|
Red Urine |
Adriamycin |
|
|
|
Chemo protectant or enhance cancer treatment -Strong type of folic Acid |
Leucovorin it can be given with 5-FU always given with methotrexate |
|
|
|
secondary prevention C |
Changes in bowel and bladder habbits, A sore that does not heal, Unusual bleeding or discharge, Thickening lump on breast, Idigestion-difficulty swallowing, obvious changes in wart or mole, Nagging cough or horseness of voice |
|
|
|
ways to obtain tissue sample for biopsy |
Endoscopy, Needle core biopsy, Laparoscopy, Incisional Biopsy, Fine needle biopsy, Excisional biopsy |
|
|
|
Tertiary Care Cancer treatment
|
Surgery, Chemotherapy, Radiation therapy, Biologic therapy |
|
|
|
Protecting yourself from exposure to chemo drugs |
Mask-inhalation, gown,hat,gloves-skin contact, Minimize exposure through, ingestion
|
|
|
|
3 types of CVAD |
Portha cath, Hickmann or broviack, Groshong |
|
|
|
Cvad does not give HIT |
Groshong |
|
|
|
adverse effect of chemo |
Thrombocytopenia, hypersensitivity reaction, alopecia, Fatigue, Anorexia, Neutropenia, Mucositis, Anemia, N&V, |
|
|
|
Extravasation |
D/C Infusion, follow facility policy for re-extravasation, Notify physician, Carry out orders, Document S/S, Monitor closely |
|
|
|
May be curative, adjuvant or palliative |
Raditaion |
|
|
|
2 types of raditaion |
Brachytherapy, Teletherapy |
|
|
|
-High dose to small area -interstitial,oral, or intracavity -out patient or inpatient -complete in 5 days requires direct tumor access |
Brachytherapy |
|
|
|
-external beam radiation -usually 5x/week for 6 weeks -Actual radiation is just only a minute -variable dose based on goal of radiation |
Teletherapy |
|
|
|
Divers ever growing approach to cancer treatment(Biologic Response Modifier)(BRM) |
Biotherapy |
|
|
|
IL-2, Interferon, Vaccines |
Immunotherapy |
|
|
|
Most common targeted therapy |
Tamoxifen-blocks estrogen at receptor sites |
|
|
|
Is a life threathening emergency, rapid onset of metabolic derangemeents and acute renal failure |
Tumor Lysis Syndrome |
|
|
|
TLS Most frequent with |
bulky, high proliferative, chemo sensitive tumors |
|
|
|
TLS body is unable to excrete bi products leading to |
Hyperuricemia, hyperphosphatemia, hyperkalemia, and hypocalcemia |
|
|
|
TLS prevention |
Hydrate and Bicarb |
|
|
|
Diagnosis for TLS |
LDH(NV:100-300) |
|
|
|
TLS manifestations |
Hypocalcemia, Urinary symptoms, Hyperkalemia |
|
|
|
TLS treatment includes |
Identification of risk patients |
|
|
|
Nurisng care for TLS |
Review Labs |
|
|
|
Most common life threatening condition associated with maliganancy |
Hypercalcemia |
|
|
|
Uneven synthesis of alpha and beta chain |
Thalassemia |
|
|
|
diagnosed through hemoglobin electrophoresis |
hemoglobinopathies |
|
|
|
thalassemia is is characterized by |
lack or decreased globin chain |
|
|
|
synthesis of a normal globin chain proceeds at |
a normal rate |
|
|
|
heinz bodies |
G6PD |
|
|
|
Chemo diet |
No grapefruit or citrus juice |
|
|
|
oral care protocol, cryotherapy palifermiin |
Mucocytis |
|
|
|
Hct/RBCs |
MCV |
|
|
|
Hgb + RBCs |
MCH |
|
|
|
Hgb + Hct x 100 |
MHCH |
|
|
|
Normal Value RBC |
|
|

