![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
What is the function of the gall bladder?
|
Stores and concentrates bile (by removing water)
|
|
|
What is the function of the liver?
|
Nutrient storage (glycogen), release, and interconversion
Bile production Filtering: Receives blood from small intestine via Portal Vein |
|
|
What is meant by the liver's ability to interconvert?
|
Liver can change amino acid identities by swapping R groups
|
|
|
What are the two sphincters of the stomach? Where are they located?
Draw the regions of the stomach. |
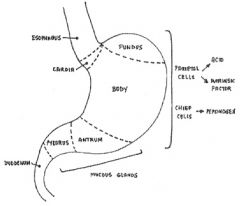
Cardiac Sphincter: between stomach and esophagus
Pyloric sphincter: between antrum and duodenum |
|
|
What is the fundus of the stomach? How does it appear on x-ray?
|
Most apical region of stomach
Seen as gas/air on x-rays |
|
|
What is the role of the stomach?
List all secretions. |
Stores food
Mixes, mechanical digestion Secretions: HCl, Gastrin, Pepsinogen (to become pepsin post-cleaving) |
|
|
What is the general mode of action of the pancreas? Provide examples.
|
Exocrine function; secretes lipase, bicarbonate (buffers chyme), other digestive enzymes
|
|
|
What is the function of the small intestine?
|
Very high surface area used for absorption of nutrients, digestion, mixing (chemical and mechanical digestion)
|
|
|
What is the coecum?
|
Region between ileum and ascending colon--appendix may hang off of it
|
|
|
What is the transverse colon?
|
Region of large intestine connecting ascending and descending colon
|
|
|
What is the role of the large intestine?
|
Resorbs water; forms feces
|
|
|
Define intraperitoneal. Provide examples.
|
Intraperitoneal--surrounded by visceral peritoneum; suspended by mesentary (similar to a ligament; connects on digestive part to another digestive part)
This includes most of the digestive tract (spleen included) |
|
|
Define retroperitoneal. Provide examples.
|
Covered on one surface by parietal peritoneum; superficial to the peritoneal cavity.
Includes the aorta, IVC, and genitourinary system |
|
|
Define secondary retroperitoneal. Provide examples.
|
began intraperitoneal, but fused to body wall and lost mesentary; thus becoming retroperitoneal.
Includes duodenum (stuck to posterior body wall), ascending and descending colon |
|
|
Do veins from the GI tract drain into the IVC?
|
No, they drain to the hepatic portal
|
|
|
What type of muscle comprises the GI tract? What properties allow coordinated contractions of such large sheets of muscle?
|
Unitary (visceral) smooth muscle--also lines reproductive tract--many gap junctions allow for coordinated contraction
|
|
|
How does the GI tract acquire an autorhythm? What is this used for (in terms of motility)?
|
Slow wave potentials, where slow waves are subthreshold potentials that result in weak tonic contractions
Used for mixing movements (segmentations) to mix food with digestive enzymes and EXPOSE TO MICROVILLI AP's that reach threshold result in stronger contractions which can contribute to transport (Peristalsis) |
|
|
What's the difference between peristalsis and segmentation?
|
Peristalsis is transport
Segmentation is mixing |
|
|
What are the descending controls on GI motility and secretion? Describe their effects and interactions with one another.
|
Autonomics:
Parasympathetic: vagus, splanchnic nerves; will increase motility and secretions via motor neurons based on sensory input from gut Sympathetic: Post-ganglionic sympathetic nerves from pre-vertebral ganglia; will DECREASE motility and secretion through motor neurons, have some sensory input from gut There is RECIPROCAL INHIBITION between descending controls, i.e., if parasympathetic is active, sympathetic is inhibited, and vice versa. |
|
|
What are the local controls on GI motility and secretion? Describe their effects and interactions with one another.
|
Enteric Nervous System = Intramural plexus
(enteric = general term for intestines) Myenteric (Auerbach's) Plexus and Submucosal (Meissner's) Plexus provide local reflexes. Work together and are sufficient to operate motility/secretion even post-vagotomy. Both have sensory and motor connections with gut |
|
|
What are the broad and local effects produced by the gut epithelium? Provide specific examples.
|
GI Hormones provide broad effects
Paracrines provide local effects Gastrin from antrum CCK from duodenum |
|
|
Describe secretion and motility of the foregut beginning with the Cephalic Phase and ending with chyme in the duodenum.
|
1) Cephalic Phase: anticipation, through, smell, taste of food. Triggers gastric secretions; controlled by vagus
2) Gastric Phase: food arrives in body of stomach; stretch receptors signal to brain, brain signals stomcha to relax} RECEPTIVE RELAXATION} VAGOVAGAL REFLEX (motor and sensory run through vagus) Food gets to antrum; feels stretch, results in MIXING movements 3) Chyme in duodenum: CCK Released |
|
|
What is receptive relaxation? What category of reflex does it fall under? Why?
|
Receptive Relaxation: stretch receptors in stomach send signal to brain, brain signals stomach to relax
Vagovagal reflex: sensory and motor info run through vagus each time |
|
|
What are the effects of CCK?
|
CCK contracts pyloric sphincter to slow stomach emptying
Contracts smooth muscle in gall bladder to release bile into duodenum Signals pancreas to release bicarbonate and enzymes to counteract acidic chyme in duodenum via SPHINCTER OF ODDI (which is relaxed by CCK) |
|
|
How is CCK release influenced?
|
Proportional to [lipids]; slower release of chyme means longer time to digest fat in small intestine with increased bile (emulsifier) present
|

