![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
About how many liters of blood are in the body?
|
4L
|
|
|
What are the main components of blood?
|
Cellular elements (10%) and plasma (90%)
|
|
|
What is blood suspended in?
|
Plasma
|
|
|
When blood is collected in a RED top tube, what layers form?
|
Red top has no anti-coagulant factor so:
Serum layer (liquid portion) Blood Clot layer (blood cells and clotting factors) |
|
|
When blood is collected in a PURPLE top tube, what layers form?
|
Anticoagulant factor present
Plasma layer: albumin, fibrinogen, immunoglobulins, lipoproteins, hormones, vitamins, salts (about 55%) Buffy coat: leukocytes and platelets (about 1%) Red blood cells: about 45% |
|
|
What is a hematocrit?
|
volume of RBC's (higher in men because of testosterone)
|
|
|
What does it mean when something is eosinophilic?
|
Loves eosin (pink)
Eosin is acidic so binds basic things Something eosinophilic must be basic! |
|
|
Why are red blood cells anucleated?
|
Makes room for hemoglobin
|
|
|
Why would a biconcave shape be favorable for RBC's?
|
RBC's main role is to transport O2
A biconcave shape increases the SA/Volume ratio which allows Hg to be closer to the surface of the cell Less distance to traverse for O2 difusion Also allows cells to be flexible when traveling through vessels |
|
|
Describe the subatomic structure of hemoglobin. How does nomenclature vary based on whether RBC's are in the lungs or in tissues?
|
Globular protein with 4 porphyrin rings with central iron atom = Heme groups (bind O2 in lungs-->oxyhemoglobin; binds CO2 in tissue-->carbaminohemoglobin)
4 globin chains: 2 alpha, 2 beta Hemoglobin = heme + globin chains |
|
|
How does the number of WBC's compare to the number of RBC's?
|
RBCs>>>>>>WBC's
~5 million ~5 thousand |
|
|
Why are WBC's considered transient?
|
Not meant to stay in vasculature like RBC's are
|
|
|
What are the two main categories of leukocytes? How would you differentiate between the two under a microscope?
|
Granulocytes: polymorphonuclear cells (multi-lobed nucleus, but appears multiple nuclei)
Agranulocytes (mononuclear): one nucleus |
|
|
What is the order of abundance of WBC's?
|
Neutrophils
Lymphocytes Monocytes Eosinophils Basophils |
|
|
What category of WBC do neutrophils fall under? How would you identify them under the microscope? What's their function?
|
Polymorphonuclear (granular)
AKA SEGS, POLYS Granules are "neutral" in color Hallmark feature = 2-5 lobes in nucleus with mixed granularity Function: phagocytosis and bacterial killing. Upon activation, enter tissues, ingest, destroy, die (1-2 day lifespan). AKA PUS |
|
|
When are neutrophils most useful?
|
For acute inflammation, ex; 48 hours after MI, polys flood into dead tissue to clean up mess
|
|
|
How would you identify an eosinophil under the microscope? How long are they in circulation? What function do eosinophils play in the body?
|
bi-lobed nucleus, eosin loving granules (pink) bc of MAJOR BASIC PROTEIN
Are in circulation for 2-8 hours before migrating to skin, lungs, GI tract Phagocytosis and killing of protozoa and paraistes Moderation of hypersensitivity allergy reactions (ex: dampening down allergic reaction in nasal mucosa or in response to adverse drug reaction) |
|
|
How would you identify a basophil under the microscope? What is their function?
|
Tons of granules, can't see nucleus.
Hallmark = large metachromatic granules (purplish) that obscure irregularly-lobed nucleus Function: exposure to allergen-->degranulation (anaphylaxis, bronchoconstriction, hives) |
|
|
What granules do basophils contain and what color do they stain?
|
Heparin sulfate
Histamine Leukotrine 3 Stain blue (basophilic, love base, blue) |
|
|
How would you identify lymphocytes under the microscope? What category of WBC do they fall under? How long are they in circulation?
|
Mononuclear cells with spherical nucleus (sometimes have an indentation)
Chromatin staining is INTENSE, very scant cytoplasm (thin rim) around nucleus Live hours to years |
|
|
How are lymphocytes different from all other WBC's?
|
It's the only type that will recirculate. Goes to tissue and back to blood stream.
|
|
|
What is the function of lymphocytes?
|
Increase in response to viral function;
Also responsible for generating specific immune responses to specific antigens they're the main functional cells of the immune system (B & T cells are main types) |
|
|
Briefly describe where lymphocytes are produced and mature.
|
Produced in marrow
B cells mature in BM T cells mature in Thymus Once mature, they go to periphery |
|
|
What leukocyte would be present in chronic inflammation?
|
Lymphocytes
|
|
|
How would you identify a monocyte under the microscope? What is their function?
|
These are least easy to ID
They are BIG, have an indented, kidney shaped nucleus and eccentrically placed Cytoplasm is blue-grey and can have very fine granules (lysosomes) Fn: Monocytes enter CT where they become macrophages and phagocytose, produce cytokines, antigen presentation |
|
|
What is the medical term for platelets? Do they have a nucleus? What cells do they originate from? What is their function? Lifespan?
|
Thrombocytes
Anucleate Originate from megakaryocytes (giant polyploid cells) Fn: Promoting blood clotting Live 7-10 Days |
|
|
What platelet granules are necessary for clotting?
|
Alpha Granules
-Adhesive proteins (fibrinogen, vWF) -Growth modulators (PGDF, TGF) -Coagulation factors |
|
|
What changes do platelets undergo upon activation?
|
MT's contract to form pseudopods, granules release contents via open canalicular system
|
|
|
What is anemia? What does it results in?
|
Low RBC count, decreased capacity to carry O2 (decreased Hg)
|
|
|
What is polycythemia? What can cause it?Also known as?
|
High RBC; AKA erythrocytosis
Can be due to low O2 tension in high altitudes (increases RBC production) |
|
|
What is iron deficiency anemia? How would you identify this disorder under the microscope?
|
Decrease in number of RBC's because of low iron (due to bleeding or increased need)
RBC's become microcytic (small) and HYPOCHROMIC (RBCs are paler bc of decreased Hg) |
|
|
Describe the genetic mechanism behind sickle cell anemia.
|
Single point mutation in beta-globulin gene changes glutamate to valine.
This forms HbS which polymerizes and decreases cell's flexibility in navigating BV's. Last only 10-20 days. Marrow can't make new RBCs fast enough to replace them. |
|
|
How do the clinical manifestations of carbon monoxide poisoning come about?
|
CO binds to Hb 200x more tightly than oxygen
Patient presents with cherry-red skin because of color of CO-Hb complex |
|
|
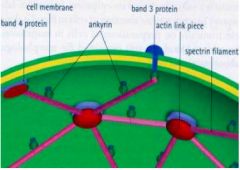
Draw the membrane proteins responsible to RBC shape.
|
|
|
|
What is the most common form of anemia?
|
Iron deficiency anemia
|
|
|
Describe the molecular mechanism and clinical manifestations of hereditary spherocytosis.
|
Defect or deficiency of spectrin protein
Causes spheroidal RBCs more vulnerable to destruction by spleen (get stuck in vasculature) Results in anemia! Some get splenectomy to tx |
|
|
What four blood antigen combinations give rise to blood types?
|
A antigen
A and B antigen B antigen No antigen (O) |
|
|
Where does erythropoiesis occur? What happens from here? How do RBCl precursors differ from mature RBC's?
|
bone marrow
mature for 5-7 days, enter periphery for 120 days, killed by reticuloendothelial cells of spleen precursors are nucleated |
|
|
What type of cell do all hematopoeitic cells originate from?
|
pluropotent hematopoietic stem cells in BM
|
|
|
Where is bone marrow found? What does it consist of?
|
Between trabeculae and in cavities
Consists of Hematopoietic cords (bunches) Stroma (reticular cells + fibers, matrix, sinusoids) |
|
|
What is yellow marrow?
|
Fat in marrow; when need less marrow, replace with fat
|
|
|
How do the sites of blood formation differ by age?
|
In embryo, BC's arise from yolk sac mesoderm
Mid-gestation: liver and spleen are hematopoietic organs, but some hematopoiesis occurs in BM From birth to old age, BM is primary hematopoietic organ with shift toward axial skeleton |
|
|
When looking at a bone marrow biopsy, how would you determine whether percent cellularity was abnormal?
|
Normal cellularity = 100-age
Babies about 100% cellular Old: ~20% cellular |
|
|
What do myeloid progentior cells give rise to?
|
Granulocytes, Monocytes/macophages, platelets, and erythrocytes.
|
|
|
What cells do lymphocytes arise from?
|
Lymphoid Progenitor Cell
|
|
|
What cell to lymphoid stem cells and myeloid stem cells arise from?
|
Hematopoietic Stem Cell
|
|
|
What role do stromal cells and GF's play in hematopoiesis? What are the clinical applications of this? Provide examples, include where GF's are manufactured.
|
Stromal cells and GF's facilitate differentiation and proliefation of hematopoietic lineages.
Can use these GF's in clinic: G-CSF (Granulocyte Colony Stimulating Factor): stimulates formation of granulocytes GM-CSF: stimulates production of granulocytes and macrophages M-CSF: macrophage formation IL-3 (Interleukin): ALL myeloid cells ALL ABOVE MADE BY STROMA EPO (erythropoeitin): stimulates RBC formation (made in kidney) |
|
|
Describe the stages (and location) of eryhtroctye maturation. How long does this take?
|
BM:
Proerthroblast Basophilic erythroblast (busy making Hg-->blue: lots of polyribs) Polychromatophilic erythroblast (multiple colors; losing polyribs) Orthochromatophilic erythroblast ("correct" color; have enough Hg, start to lose nucleus) LOSE NUCLEUS (macrophage eats extruded nuclei) ENTER CIRCULATION AS Reticulocyte (immature: lacks pallar) Erythrocyte (mature) Takes about a week. |
|
|
What is a Howell-Jolly body? When does it occur? Clinical effects?
|
Nuclear fragment
Occurs if RBC leaves BM and has nuclear remnant; spleen would destroy Most often seen post-splenectomy Causes no problems |
|
|
Describe the nucleation of reticulocytes. How long do they exist? What occurs over this period?
|
Anucleate
Mature over 2-3 days to become RBC's Lose mitochondria, ribosomes, cytoplasmic enzymes |
|
|
What's another term for erythroblast?
|
Normoblast
|
|
|
What is the overall trend in RBC maturation?
|
large, pale nucleus to dark, small nucleus to loss of nucleus
Increase in cytoplasm, gradual decrease in cytoplasm cytoplasm from intense blue (lots of RNA) to gray (mix of RNA and Hg) to red (full of Hg, no RNA) |
|
|
What are azurophilic granules?
|
Primary granules (lysosomes) that appear early in granulocyte development
THey're non-specific; have stuff that's found in lysosomes (lysozyme, myeolperoxidase, collegenase, acid phosphatase) Side note: Following are specific to neutrophils: lactoferrin lysozyme collagenase alkaline phosphatase antibacterial proteins |
|
|
Generally describe granulocyte stages of development.
|
Myeloblast-->Promyelocyte-->Myelocyte-->Specific dev't
|
|
|
Describe the stages of granulocytopoiesis.
|
Myeblast
Promyelocyte Myelocyte (speckled granules) NO MORE MITOSIS Metamyelocyte (kidney shaped nuc) Band (in blood) Seg (in blood) |
|
|
What is the overall trend of granulocytopoiesis?
|
dark, segmented nucleus, increasing cytoplasm
no granules to primary granules to specific granules |
|
|
Describe the stages of eospinophil development.
|
Eosinophilic myeloblast
Eosinophilic promyelocyte Eosinophilic myelocyte Eosinophilic metamyelocyte Mature eosinophil |
|
|
Describe the different pools of WBC's.
|
Precursor pool - progenitor and precursor cells
Storage pool - immature (band) and mature cells hanging around (released in times of stress) In periphery: Marginating pool (WBCs hanging around BV walls) Released into Circulating Pool Tissue pool (death by apoptosis) |
|
|
Describe the location and maturation of lymphocytes.
|
Produced in Marrow, originate from Lymphoid Stem cell (which came from hematopoietic stem cell)
Migrate to various areas: B cells to mature in marrow T cells to mature in thymus Once mature, migrate to peripheral lymphoid tissues ONLY TYPE OF WBC TO RECIRCULATE |
|
|
Describe the origin and development of platelets.
|
Megakaryocytes (largest cells in BM) produce platelets by cytoplasmic fragmentation
|
|
|
What is pancytopenia? How can it be caused? How would this be visible on a bone marrow aspirate?
|
Low blood cell counts (RBC, WBC, platelets, Hg)
Could lack hematopoietic cells (aplastic anemia) Could have acute leukemia (100% cellularity, i.e., 100% immature cells) If see blast cells on peripheral smear, BM is spitting out immature cells. BAD! Leukemia! |
|
|
In a WBC differential, what is a left shift?
|
Increase in bands (immaturity)
|

