![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
Where is the common passage of respiratory and digestive tracts?
|
Pharynx
|
|
|
Where is the voice box located?
|
Larynx
|
|
|
How does the design of the pleural cavitiy contribute to intrathoracic pressure?
|
The cavity is closed, allows a negative pressure to be maintained
|
|
|
How to the left and right lungs differ?
|
Left lung: two lobes (superior, inferior), heart presses against it
Right lung: Three lobes (Superior, middle, inferior); TRI to do RIGHT |
|
|
Where is the mediastinum in relation to the lungs?
|
Between them
|
|
|
What structures comprise the conducting zone?
|
Trachea, bronchi (primary, secondary, tertiary), bronchioles, terminal bronchiole
|
|
|
Where in the conducting zone does cartilage cease to exist?
|
Terminal bronchioles
|
|
|
Where do asthma drugs act?
|
on SM of terminal bronchioles
|
|
|
What embryonic germ layer does the conducting zone form from?
|
ENDODERM
|
|
|
About how many generations of branching do bronchioles undergo?
|
23
|
|
|
How many alveoli are in the lungs (total)?
|
300 million
|
|
|
How many primary bronchi are there?
Secondary? Tertiary? |
2
5 20 |
|
|
What is tidal volume?
|
~500mL: air moved in, and then out, of lungs in one breathing cycle
|
|
|
What is inspiratory reserve?
|
~3000mL: amount of air that can be inhaled after a normal inspiration
|
|
|
What is expiratory reserve?
|
~1200mL: Amount of air that can be exhaled after normal exhilation
|
|
|
What is residual volume?
|
~1200mL; amount of air that cannot be exhaled from lungs
|
|
|
What is inspiratory capacity?
|
~3500mL, tidal volume + inspiratory reserve volume
(Total fill of lungs) |
|
|
What is functional residual capacity?
|
~2400mL; expiratory reserve volume + residual volume
i.e., total amount of air in lungs after normal exhalation |
|
|
What is vital capacity?
|
~4700mL; inspiratory capacity + expiratory reserve
|
|
|
What is total lung capacity?
|
~6L; vital capacity + residual volume
|
|
|
Define compliance. What determines it in lung? In chest wall?
|
Distensibility of a system.
Elasticity of lung and surface tension in alveoli Bone, muscle, CT in wall |
|
|
How would a decrease in alveoli number affect compliance?
|
Decrease elastic fibers, increased compliance
|
|
|
When does FRC occur? How is it achieved (in terms of compliance)?
|
At rest; no movement of air
Compliance of lungs (wants to collapse) = compliance of chest wall (wants to expand) |
|
|
Describe the changes in pleural cavity and intraalveolar pressures during the following stages of respiration:
Rest Mid-inspiration End-inspiration Mid-expiration |
Rest: FRC! lungs want to collapse, chest wants to expand; IA: 0 atm (=Patm), Pleural space: -5
Mid-inspiration: diaphragm pulls down, increases volume of thorax, increases volume of pleural space IA: -1 Intrapleural: -6.5 End-inspiration: lungs stretch out IA: P=0 IP: P=-8 No air movm't, lungs want to pull back in Expiration: Diaphragm and muscles relax; lungs undergo elastic recoil, pulls diaphragm back up IA: P=+1 IP: P=-6.5 |
|
|
What is the effect of emphysema on respiratory system? Discuss compliance and FRC.
|
Lose alveoli, lose SA for gas exchange, lose elastic tissue, INCREASED COMPLIANCE
FRC increases, breathe at higher lung volumes, harder to push air out! |
|
|
What is hemothorax?
|
Liquid filling in PLEURAL CAVITY
|
|
|
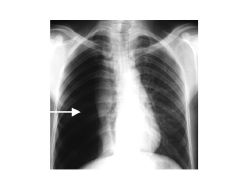
What is pneumothorax?
|
Collapsed lung; air fills in pleural space
|
|
|
What is tension pneumothorax?
|
Collapsed lung causes trapped air (in pleural space) to push heart to side
|
|

|
Pneumonia: fluid in lung
|
|

|
Hemothorax: fluid in pleural space (blood)
|
|
|
Pneumothorax: collapsed lung causes air to fill pleural space
|
|

|
Tension pneumothorax: collapsed lung causes air to enter, become trapped, and then push heart to side
|

