![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
Selective Serotonin Reuptake Inhibitors (SSRIs) |
Though to restore levels of 5-HT in synaptic cleft by binding to SERT protein prevent reuptake + degradation of 5-HT 1st line tx for depression side effect= decreased libido safe for most, rare side effect⇒ serotonin syndrome |
|
|
SNRIs: 5-HT + NA reuptake inhibitors |
both NA + 5-HT synapse affect but w/ more specificity than the TCAs minimal affinity thus minimal antagonism similar side effects as SSRI similar pharmacological actions as TCA evidence of BP elevation |
|
|
MAO= monoamine oxidase |
MAO-A⇒ metabolises NA + 5-HT in CNS MAO-B⇒ metabolises DA in CNS MAO-A inhibitors⇒ treat depression MAO-B inhibitors⇒ treat Parkinson's disease MAO-A inhibitors: prevent NT from being taken back up or from being broken down |
|
|
MAOI effects to GIT |
MAO-A in GIT tyrasine not broken down in GIT if MAO-A inhibited, therefore can enter bloodstream. Tyrasine cross BBB and displaces NA from synaptic terminal increase in BP |
|
|
Deficiency of NT in Depression |
must increase or supplement conc. of NT to compensate for shortage add NT or its precursor prevent NT from being taken up into the neuron or from being broken down |
|
|
Tricyclics (TCAs) |
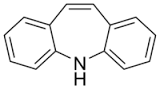
1st antidepressants have three ring structure inhibit reuptake of NA + 5-HT |
|
|
TCAs bind and antagonise |
Histamine H! receptors⇒ sedation alpha-adrenoreceptors⇒ postural hypotension mucarinic ACh receptors⇒ blurred vision, dry mouth, constipation |
|
|
Theories of Depression |
The Monoamine Hypothesis⇒ deficiency in brain of NA and 5-HT w/ peripheral involvement of DA Current Theory⇒ cortisol is usually elevated in depressed patients, balance between apoptosis and neurogenesis is gaining support within hippocampus. Glutamate levels also increased in depression |
|
|
NA and 5-HT Synpases |
NA is removed by reuptake through NET metabolised by MAO in neurons or COMT 5-HT has many receptor subtypes and is cleared form synaptic cleft by uptake transporter SERT and no COMT |
|
|
ADHD |
Symptoms in 3 main areas: → inattention → impulsiveness → hyperactivity begins in childhood, life time condition, effects decrease with time |
|
|
Ganglionic Blockers |
trimethaphan Blood pressure= peripheral resistance and rate rate force Sympathetic NS: vasodilation, decrease BP Parasympathetic NS: hear rate increase, tachycardia side effect due to predominant ANS branch blockage |
|
|
Neuromuscular Junction |
motor nerve (cholinergic) skeletal muscle nicotinic receptors at end plate when nACHR activated→ small depolarisation are summated to end plate potential→ action potentials develop + spread over muscle cell→ contraction occurs |
|
|
Nicotinic Acetylcholine Receptor Pharmacology |
Somatic Motor nerve presynaptic terminal → muscle relaxants: post synaptic muscle cell Pre-ganglionic presynaptic terminal → ganglionic blocker: postsynaptic post ganglionic cell |
|
|
Nicotine |
- non-selective agonist at nicotinic receptors - main alkaloid of tobacco plants - activate/paralyse para and/or sympathetic NS - usually activates predominant ANS in smokers - nicotine overdose cause nausea, abdominal cramp |
|
|
Nicotinic Cholinergic Receptors |
Acetyl choline: nicotinic ACH receptors, muscarinic ACH receptors Cation receptor: muscle [(ɑ1)2, β1], ganglion [(ɑ3)2, (β4)3], CNS (varies) |
|
|
Acetylcholinesterase Inhibitors |
"Agonistic" effects on neuromuscular junction: - greater muscle tension - treatment of myasthenia gravis "Agonistic" effects on muscarinic synapses: treamtent of glaucoma, GIT immobility Effect on CNS: treatment for Alzheimers |
|
|
High Dose of ACHE inhibitors or nerve gas |
Muscarinic Effects= pinpoint pupils, blurred vision, nausea, diarrhoea nicotinic effects= depolarisation block, skeletal muscle twitching, cramping followed by weakness and paralysis CNS: seizures, respiratory depression antidote= atropine |
|
|
Uses of Muscarinic Antagonists |
atropine + derivates - induce mydriasis - asthma - inhibits vagal reflexes during surgery |
|
|
Drugs Changing Cholinergic Transmission |
Botulincs toxin A- strongest poison, treatment for wrinkles and for flaccid paralysis of muscles Acetylcholinesterase inhibitors- enhanced ACh NT, skeletal muscle, postganglionic cell or effector organ inervated by parasympathetic NS |
|
|
Uses of muscarinic agonists |
philocarpine ↳ tx of glaucoma, dry mouth ↳ side effects: muscarinic side effects, seizures ↳ treat w/: agonist=atropine |
|
|
Glaucoma |
damage to optic disk loss of peripheral vision often due to increased intraocular pressure |
|
|
Muscarinic Acetylcholine Receptors |
particularly responsive to muscarine GPCR that act through 2nd messengers 5 subtypes- m1, m2, m3, m4, m5 m1,3 and 5⇒ IP3/DAG↑ (CNS, glands, Smooth muscle, GIT) m3, m4⇒ cAMP ↓ heart, CNS: k+ conductance↑, Ca2+ conductance ↓ |
|
|
Antidote to Atropine |
colinesterise inhibitors |
|
|
Nicotinic Receptors |
particularly responsive to nicotine also a NA+ and K+ ion channel form ligand-gated NA+, K+ ion channels N receptor: - found in autonomic ganglia
|
|
|
Cholinergic Transmission |
transmitters and receptors in the ANS NA/A→ adrenergic receptors GPCR (alpha 1,2) (beta 1,2) |
|
|
Changes in myometrium |
myometrium gets prepared for labour by - increase in blood oxytocin levels - rises in oestrogen which causes increase in # of OT receptors - progesterone an have opposite affect - more prostaglandin reuptake - more gap junctions - more ion channels |
|
|
Parturition |
=childbirth cervical ripening ↳ collagen broken down ↳ h20 + hyaluronic acid levels ↑ ↳ cervix no longer rigid ↳ cervix becomes thin (effacement) ↳ cervix opens (dilation |
|
|
Myometrium |
4 muscle layers containing smooth muscle cells in a matrix of collagen and ground substance around the smooth muscle bundles are fibroblasts, blood, lymph vessels and nerve cells surrounding uterus adrenergic and cholinergic play minor role in contraction prostaglandins + oxytocin play larger roles |
|
|
The Uterus |
supports growth and development of embryo and foetus upon childbirth→ from mostly inactive state to a strong synchronous, contractile state to expel foetus and placenta |
|
|
Molecular Mechanisms of Myometrial Contraction |
mostly like any other smooth muscle increase in Ca2+→ interact w/ calmodulin → forms Ca2+-calmodulin → activates myosin light chain kinase (MCKR) enzyme→ phosphorylates myosin→ phosphorylated myosin interacts w/ actin |
|
|
States of Childbirth in UTerus |
Phase 0- Quiescence (95% of pregnancy, quiet) Phase 1- Activation (oestrogen is key uterine awakening because ↑ CAPs) Phase 2- Stimulation (coordinated forceful contractions) Phase 4- involution (OT shrinks the uterus) |
|
|
Oxytocics |
Synthetic oxytocin - given by IV to induce/enhance uterine smooth muscle contractions - prevent postpartum uterine haemorrhage - nasal spray stimulates milk let down in nursing mothers - metabolised by an amino peptidase - enzyme in placenta, kidney liver |
|
|
Oxytocics MOA |
OT binds to OT receptor located on surface of smooth muscle cell G-Protein is activated- it is link to phospholipase C which produces IP3 an dDAG CA2+ mobilisation fro sarcoplasmic reticulum influx of Ca2+ through L type Ca2+ channels |
|
|
Prostaglandin Drugs |
Misoprostal is a prostaglandin analog it is an EP receptor Agonist → contraction used for induction of labour, pregnancy, preventing postpartum haemorrhages |
|
|
Dinoprostone |
prostaglandin drug naturally occurring PFE2 is a EP receptor agonist binds and activates → contraction applied intravaginally used for induction of labour, cervical ripening |
|
|
Dopaminergic Synpases |
one current theory is that there is an imbalance conc. within key brain circuits which modulate attention and interest ADHD subjects have higher than normal levels of DA transporters in the striatum fewer dopamine receptors present in ADHD patients |
|
|
ADD/ADHD treatment |
tx can include medication training for parents and teachers and behaviour management programs for children medication for severe cases to help focus the child's attention dexamphetamine or methylphenidate most commonly prescribed drug |
|
|
Major NT in CNS |
Amino Acids GABA⇒ inhibitory Glycine⇒ inhibitory Glutamate⇒ excitatory Aspartate⇒ excitatory |
|
|
Dexamphetamine |
· can stabilise dopamine and NA transporters in channel configuration reverse low through intracellular transporters · effective |
|
|
Methylphenidate |
increases synaptic catecholamines by blocking the reuptake of both by their respective transporters effective short 1/2 life so sustained release forms are popular side effects- decreased appetite, insomnia, headaches, irritability, moodiness |
|
|
MOA of anti-epileptic Drugs |
1. blockade of NA+ channels which are required for impulse transmission to inhibit rapid firing of NA+ ion channel, ↓ AP 2. blockade of Ca2+ channels 3. Strengthening of GADAergic inhibitory input, bind to GABA induced hyperpolarisation increase inhibitory behaviour in CNS 4. blockade of excitatory glutamatergic input, reduce glutamatergic activity |
|
|
Anti-epileptic Drugs |
Carbamazepie valproic acid/valproate plenytoin lamotrigine gabapentin and pregabaline |
|
|
Glutamate Receptor as Drug Target |
penetration of BBB is a challenge difficult to selectively block funtion as glutamate is so generally used throughout hte CNS only 2 drugs are lipid soluble: - ketamine - memantine= noncompetitive antagonist on NMDA receptor, treats Alzheimers - PCP |
|
|
Life Cycle of GABA |
GABA is synthesised from glutamate by enzyme glutamic acid decarboxylase and only GABAergic neurons have glutamic acid decarboxylase degradation occurs by GABA transaminase |
|
|
PCP + Ketamine |
non-competitive antagonists of the NMDA receptor they bind at the same deep site within the ion channel of the NMDA receptor- blocking ion movement PCP used as anaesthetic agent but caused psychotic reactions + became recreational hallucinogenic drug |
|
|
GABAb Receptors |
modulates adenyl cyclase activity via G proteins that in addition increases outward let and reduces inward Ca2+ conductance, reduces post synaptic excitability BZP bind to g subunit at modulatory site and they cause a conformational change in GABA binding site, giving it a greater affinity for GABA |
|
|
Activation of GABAb Receptors |
modulates adenyl cyclase activity which increases outward k+ and inward ca2+ conductance |
|
|
GABAa Receptors |
inward movement of CL- ions results in hyperpolarization so AP is less likely to occur |
|
|
Tonic Seizure Phase |
strong contraction of whole musculature- all muscle stiffen initial strong contraction of whole musculature, cry or groan loss of consciousness, stop breathing |
|
|
Clonic Seizure Phase |
violent synchronous jerks that last several minutes injuries can occur from objects surrounding seizing patient |
|
|
Generalized Seizures |
induce whole brain immediate loss of consciouness tend to be genetic two types: tonic-clonic "grand-mal" or absence seizures "petite mal" |
|
|
Absence seizures "petite mal" |
typically in children of teens much less dramatic than tonic-clonic seizures sudden loss of consciousness usually short, recurs often no recollection of events symptoms= staring, flattering of eyes, 'check out' due to abnormalities in Ca2+ channels |
|
|
Ferbrile Seizures |
4% of children from 3 months-5yrs during high fever stay calm, observe child, place child on clear substance, don't hold or restrain, place on stomach to prevent choking, go to doctor afterwards |
|
|
Atypical antipsychotic medications |
⇒5-HT DA antagonists ⇒increased selectivity ⇒reduced EPS side effects ⇒clozapine treat both positive and negative symptoms- no EPS ⇒ muscarinic ACh etc. receptor brain blocked Agranulocytosis caused death so recalled |
|
|
Psychological Anorexic Symptoms include |
obsessive, rigid, showing emotional restraint, having high need for approval, w/ low self esteem, poor adaptability to change, disconnect between body image and reality |

